Abstract
An attenuated Plasmodium falciparum (Pf) sporozoite (SPZ) vaccine, PfSPZ Vaccine, is highly protective against controlled human malaria infection (CHMI) 3 weeks after immunization, but the durability of protection is unknown. We assessed how vaccine dose, regimen, and route of administration affected durable protection in malaria-naïve adults. After 4 intravenous immunizations with 2.7 × 105 PfSPZ, 6/11 (55%) vaccinated subjects remained without parasitemia following CHMI 21 weeks after immunization. Five non-parasitemic subjects from this dose group underwent repeat CHMI at 59 weeks and none developed parasitemia. Although Pf-specific serum antibody levels correlated with protection up to 21–25 weeks after immunization, antibody levels waned substantially by 59 weeks. Pf-specific T cell responses also declined in blood by 59 weeks. To determine whether T cell responses in blood reflected responses in liver, we vaccinated non-human primates (NHP) with PfSPZ Vaccine. Pf-specific interferon-γ-producing CD8 T cells were present at ~100-fold higher frequencies in liver than in blood. Our findings suggest that PfSPZ Vaccine conferred durable protection to malaria through long-lived tissue-resident T cells and that administration of higher doses may further enhance protection.
INTRODUCTION
In 2015 there were an estimated 214 million clinical cases and 438,000 deaths due to malaria1, primarily caused by Plasmodium falciparum (Pf) in children in Sub-Saharan Africa. A highly effective vaccine is urgently needed to prevent malaria in individuals and facilitate elimination of malaria from defined geographic areas. To achieve these goals, we have set an interim target of >80% sterilizing protection against Pf infection for >6 months2.
There is currently no malaria subunit vaccine that approaches this level of protection. The most extensively studied candidate malaria vaccine, RTS,S, a subunit vaccine based on the Pf circumsporozoite protein (PfCSP), confers sterilizing protection against controlled human malaria infection (CHMI) in about 22% of healthy malaria-naïve adults 5 months after vaccination3. In a phase 3 field study, efficacy of RTS,S against clinical malaria was 26% and 36% in young infants and children age 5-17 months, respectfully, through 38-48 months of follow-up following a four dose regimen on a 0, 1, 2, and 20 month schedule.4 Therefore, it is necessary to investigate alternative vaccination strategies that confer long-lived sterilizing protection5,6.
Sustained sterilizing immunity against the pre-erythrocytic stages has been observed in humans immunized by whole parasite approaches using mosquitoes for vaccination7,8. In a study of malaria-naïve adults, 5/6 subjects exposed to >1000 irradiated mosquitoes carrying attenuated PfSPZ were protected when CHMI occurred 23–42 weeks after immunization8. To advance from using mosquitoes for inoculation of attenuated PfSPZ towards a clinical product, we previously reported that immunization by intravenous (IV) injection of radiation-attenuated, aseptic, purified, cryopreserved PfSPZ, a product called Sanaria® PfSPZ Vaccine9, was well tolerated and immunogenic (the VRC 312 study)10,11. PfSPZ Vaccine induced a dose-dependent increase in PfSPZ-specific antibodies and frequencies of multi-functional THI cytokine-producing CD4 T cells and γδ T cells in the blood. When vaccine recipients underwent CHMI 3 weeks after final immunization, Pf parasitemia was observed in 3/9 and 0/6 subjects who received 4 or 5 doses of 1.35 × 105 PfSPZ, respectively, but in 5/6 unvaccinated controls, demonstrating that PfSPZ Vaccine confers high-level, short-term protection. The next critical milestones for PfSPZ Vaccine were to assess the durability of vaccine efficacy and investigate immune correlates and mechanisms of protection.
RESULTS
PfSPZ Vaccine efficacy at 21 weeks
To assess durability of protection, subjects from the VRC 312 study were re-enrolled for repeat CHMI with the homologous Pf clone 3D7. Because vaccine efficacy is assessed at multiple time points in the same vaccinated subjects, we defined vaccine efficacy as first VE (VE at 1st CHMI), subgroup VE (VE among the subgroup of subjects that were not parasitemic after the 1st CHMI), and cumulative VE (first VE multiplied by subgroup VE). VE is calculated as 1 – relative risk, where relative risk is the ratio of the infection rate among the vaccinated subjects divided by the infection rate among the controls. Thus, VE is always adjusted to account for those cases in which the infection rate in the controls is not 100%.
Six subjects who had received 4 or 5 IV doses of 1.35 × 105 PfSPZ and had not develop parasitemia following CHMI at 3 weeks14 underwent repeat CHMI 21 weeks after final vaccination. Four of 6 subjects developed parasitemia compared to 6/6 unvaccinated controls (Supplementary Fig. 1a,b), for a subgroup VE of 33% (P = 0.23) and cumulative VE of 25%. Thus, 1.35 × 105 PfSPZ administered 4 or 5 times did not confer adequate protection at 21 weeks.
Additionally, 8 subjects in the VRC 312 study who were parasitemic at a prior CHMI (6 immunized subjects and 2 unvaccinated controls) underwent repeat CHMI, and all developed parasitemia (Supplementary Fig. 1c,d). Thus, a single previous episode of Pf parasitemia followed by drug treatment did not confer protection against a subsequent CHMI. Therefore, only vaccinated subjects who did not develop parasitemia following their first CHMI underwent repeat CHMI in the following studies.
Study design
We assessed in a new study (VRC 314) whether increasing the dose of PfSPZ Vaccine from 1.35 × 105 to 2.7 × 105 PfSPZ per dose affected VE. With this higher dose, we tested three-dose (group 1) and four-dose (groups 4 and 5) regimens. A fourth group of subjects received 1.35 × 105 PfSPZ four times followed by a fifth dose of 4.5 × 105 PfSPZ (group 3) to determine if a higher final dose improved VE compared to 5 doses of 1.35 × 105 PfSPZ (Fig. 1a). In each of these groups, PfSPZ Vaccine was administered by rapid IV injection.
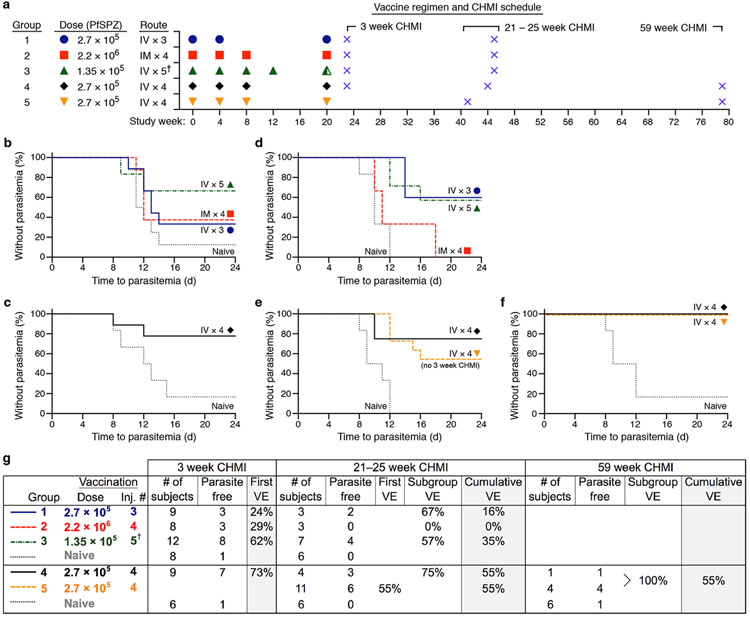
Figure 1. Sterile protection following CHMI at 59 weeks after immunization with PfSPZ Vaccine.
(a) Timing of immunizations and CHMIs. Vaccinated subjects underwent CHMI 3, 21–25, and/or 59 weeks after final immunization. Half-filled green triangle denotes 4.5 × 105 PfSPZ IV. †Group 3 received four doses of 1.35 × 105 PfSPZ and a fifth dose of 4.5 × 105 PfSPZ.
(b–f) Kaplan-Meier curves showing the percent of volunteers who did not develop parasitemia after each of 5 separate CHMIs at 3 weeks (b,c), 21-25 weeks (d,e), or 59 weeks (f) after final immunization. New unvaccinated control subjects were enrolled for each CHMI. Day 0 indicates the time of exposure to infected mosquitoes. Monitoring for parasitemia was by once daily PCR.
(g) Vaccine efficacy for each group after each CHMI. VE = 1 – relative risk, where relative risk is the infection rate in the vaccine group divided by the infection rate in the naive control group. First VE = VE at first CHMI; subgroup VE = VE among the subgroup of subjects that were not parasitemic at first CHMI; cumulative VE = first VE multiplied by subgroup VE. Subjects in group 5 underwent CHMI for the first time 21 weeks after final immunization and first VE was 55% (95% c.i. 0.13-0.76); P = 0.037, one-sided Fisher’s exact test. Five subjects from groups 4 and 5 underwent repeat CHMI 59 weeks after last immunization, and all were without parasitemia (P = 0.013).
The trial also assessed route of administration. Studies in non-human primates (NHP) and humans show that IV administration of PfSPZ Vaccine is substantially more immunogenic and protective than subcutaneous (SC) or intradermal (ID) administration at a dose of 1.35 × 105 PfSPZ10,11. However, studies in rodents show that intramuscular (IM) administration of radiation-attenuated SPZ is more protective than SC or ID administration, albeit considerably less than by IV administration12,13. As there may be instances in which IV administration is logistically complex, we compared protective efficacy of 2.7 × 105 PfSPZ administered IV with 2.2 × 106 PfSPZ administered IM (an 8.1-fold higher dose) with the same four-dose regimen (group 2) (Fig. 1a).
For the primary efficacy analysis, the results are presented for the first CHMI for each vaccine group as compared to controls. To account for multiple comparisons, P-values < 0.01 were taken as evidence of an effect and P-values between 0.01–0.05 as suggestive. This threshold for significance of the primary analysis was specified in the protocol to balance the potential for type 1 error with the conservative Bonferroni approach (see Online methods). Secondary analyses compare the results from the different groups as well as describe the results of repeated challenges among those who remained parasite free in each group. No formal multiple comparison adjustment were employed for secondary endpoints.
Daily monitoring by PCR was used for diagnosis of parasitemia and treatment rather than thick blood smear. In VRC 312, PCR allowed detection of parasitemia one to two days earlier than blood smear (Supplementary Table 1), which enabled clinical monitoring criteria to be changed from overnight stays after day 7 to once daily outpatient visits.
Study population
101 subjects were enrolled: 57 vaccine recipients, 32 CHMI controls, and 12 backup controls (Supplementary Fig. 2). Baseline demographic characteristics are shown in Supplementary Table 2. Fifty-five of 57 (96%) subjects completed all scheduled vaccinations and, cumulatively, 224 vaccinations were administered. In total, 52/55 subjects (95%) who completed their vaccinations underwent at least one CHMI. At CHMI occurring 3 weeks, 21–25 weeks, and 59 weeks after final vaccination, there were 39, 31, and 5 participating vaccine recipients, respectively (Supplementary Table 3).
Adverse events
Vaccinations were well tolerated. Of 57 vaccine recipients, 41 (72%) had no solicited adverse events at the injection site after any vaccination, 15 (26%) had mild symptoms, and one (2%) had moderate symptoms (Supplementary Table 4). Solicited systemic symptoms were none for 32 (56%) vaccine recipients, mild for 19 (33%), and moderate for six (11%; Supplementary Table 5). There were no serious adverse events attributed to vaccination. Alanine aminotransferase levels measured 14 days after each vaccination were not elevated in any dose group compared to pre-vaccine levels (Supplementary Fig. 3).
Vaccine efficacy over 1 year
VE at 3 weeks, IV administration.
Four of 12 subjects in group 3 (4 doses of 1.35 × 105 PfSPZ and a fifth dose of 4.5 × 105 PfSPZ) and 6/9 subjects in group 1 (3 doses of 2.7 × 105 PfSPZ) developed parasitemia after CHMI compared to 7/8 controls (Fig. 1b). In group 4 (4 doses of 2.7 × 105 PfSPZ), 2/9 vaccinated subjects developed parasitemia, compared to 5/6 controls (Fig. 1c). First VE was estimated to be 62% for group 3 (P = 0.025), 24% for group 1 (P = 0.34) and 73% for group 4 (P = 0.035).
VE at 21-25 weeks, IV administration.
Only vaccine recipients who did not develop parasitemia after their first CHMI underwent repeat CHMI. Seven subjects from group 3 (4 doses of 1.35 × 105 PfSPZ and a fifth dose of 4.5 × 105 PfSPZ) underwent repeat CHMI at 25 weeks after final vaccination, and 3/7 developed parasitemia compared to 6/6 controls. Subgroup VE was 57%, and cumulative VE was 35% (Fig. 1d). These results were similar to the results from the VRC 312 study when CHMI was performed at 21 weeks (Supplementary Fig. 1). Thus, increasing the final dose 3.3-fold did not improve short- or long-term protection compared to the five-dose regimen of 1.35 × 105 PfSPZ11. Three subjects in group 1 (3 doses of 2.7 × 105 PfSPZ) underwent repeat CHMI at 25 weeks, and 1/3 developed parasitemia (Fig. 1d); subgroup VE was estimated at 67% and cumulative VE was 16%.
Four subjects in group 4 (4 doses of 2.7 × 105 PfSPZ) underwent repeat CHMI at 24 weeks. One of 4 vaccinated subjects and 6/6 controls developed parasitemia (Fig. 1e), resulting in a subgroup VE of 75% and cumulative VE of 55%. A second group of subjects that received 4 doses of 2.7 × 105 PfSPZ (group 5) underwent their first CHMI at 21 weeks. Five of these 11 vaccinated subjects developed parasitemia resulting in a first VE of 55% (P = 0.037; Fig. 1e).
VE at 59 weeks, IV administration.
Five subjects who received 4 doses of 2.7 × 105 PfSPZ, who had each undergone a single prior CHMI and not developed parasitemia, underwent a second CHMI 59 weeks after final immunization. None of the 5 vaccine recipients and 5/6 controls developed parasitemia (P = 0.013; Fig. 1f). Subgroup VE was 100% and estimated cumulative VE was 55% at 59 weeks (Fig. 1g).
VE at 3 and 25 weeks, IM administration.
Five of 8 subjects from group 2 (IM vaccination with 2.2 × 106 PfSPZ) developed parasitemia following CHMI 3 weeks after vaccination; first VE of 29% (Fig. 1b). The 3 subjects that did not develop parasitemia at 3 weeks underwent repeat CHMI at 25 weeks, and all developed parasitemia (Fig. 1d). Thus, PfSPZ administered IM at 8.1-fold higher dose was less efficient in inducing protection than IV administration (8/8 parasitemic in group 2 through 21–25 week CHMI vs. 5/11 in group 5; P = 0.018).
Immunogenicity
Antibody responses.
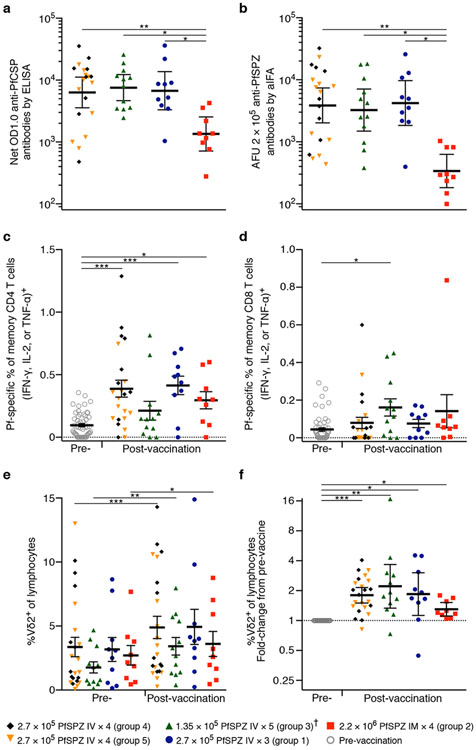
Antibodies induced by attenuated SPZ vaccination can limit parasites from infecting hepatocytes in animals14-16. Therefore, antibodies against PfCSP and whole PfSPZ were assessed by enzyme-linked immunosorbent assay (ELISA) and automated immunofluorescence assay (aIFA), respectively, two weeks after final vaccination. There were no differences in antibody levels among the groups that received the different IV regimens. However, subjects immunized IM had lower antibody responses than did subjects immunized IV (Fig. 2a,b)
Figure 2. Pf-specific antibody and cellular immune responses two weeks after final immunization.
(a) Antibodies to PfCSP were measured by ELISA.
(b) Antibodies to PfSPZ were measured by automated immunofluorescence assay (aIFA).
(c) Pf-specific memory CD4 T cells secreting IFN-γ, IL-2, and/or TNF-α were measured by intracellular cytokine staining (ICS). Results are the percent of cytokine-producing cells after incubation with PfSPZ minus percent of cytokine-producing cells after incubation with vaccine diluent (medium with 1% HSA).
(d) Pf-specific memory CD8 T cells secreting IFN-γ, IL-2, and/or TNF-α by ICS after incubation with Pf-infected red blood cells (PfRBCs) or uninfected RBCs as control. Results calculated as in c.
(e) Frequency of Vδ9+Vδ2+ (hereafter Vδ2+) γδ T cells among total lymphocytes.
(f) Fold change from pre- to post-vaccination in the frequency of Vδ2+ T cells as a percentage of total lymphocytes.
For a–b, between group differences were assessed by Kruskal-Wallis test with Dunn’s correction for multiple comparisons. For c–e, there were no differences between vaccine groups in the post-vaccination responses by Kruskal-Wallis test. Difference from pre-vaccine was assessed by Wilcoxon signed rank test (c–e) or one-sample t-test (f). For c–f, P-values were corrected by the Bonferroni method. * P < 0.05, ** P < 0.01, *** P < 0.001. Geometric mean ± 95% c.i. (a, b, f) or mean ± s.e.m. (c–e). Each dot represents one subject.
†See Fig. 1 for doses.
Cellular responses.
Cellular immunity is critical for protective efficacy of live-attenuated SPZ vaccination in rodent and NHP models10,17-19. While interferon (IFN)-γ-producing CD8 T cells are necessary and sufficient in the majority of mouse and NHP studies20, NK, γδ, and CD4 T cells also influence protection19,21. Pf-specificity was determined by stimulating peripheral blood mononuclear cells (PBMCs) with PfSPZ Vaccine (for CD4 T cell responses) or Pf-infected erythrocytes (for CD8 T cell responses) (Supplementary Figs. 4-5 and Supplementary Table 6). There is considerable overlap in the proteomes of PfSPZ and PfRBC. While there was an increase in PfSPZ-specific CD4 T cell cytokine responses after final immunization in groups 1, 2, 4, and 5, there were no differences between the vaccine groups (including the IM group) in the magnitude (Fig. 2c) or quality of PfSPZ-specific CD4 cytokine responses (Supplementary Fig. 6). The PfRBC-specific CD8 T cells in blood two weeks after the final immunization were no different from background (pre-vaccine) in most vaccine groups (Fig. 2d). Last, there was a vaccine-induced increase in the frequency of total γδ T cells, but no differences between the groups (Fig. 2e,f). The expansion was restricted to the Vγ9+Vδ2+ family (hereafter Vδ2+), which comprises ~75% of γδ T cells in blood (Supplementary Fig. 7a-f). A higher percentage of γδ T cells expressed the activation markers CD38, the cytotoxic molecule perforin, and the liver-homing chemokine receptor CXCR622 after vaccination (Supplementary Fig. 7g-l). Of note, γδ T cells from PBMC analyzed prior to vaccination expressed IFN-γ when stimulated ex vivo with live-attenuated PfSPZ (Supplementary Fig. 7m).
Immune correlates
To identify potential immune correlates of protection23, we assessed whether there were associations between immune responses measured two weeks after last immunization and outcome after each CHMI (parasitemia vs. no parasitemia).
Antibody correlates.
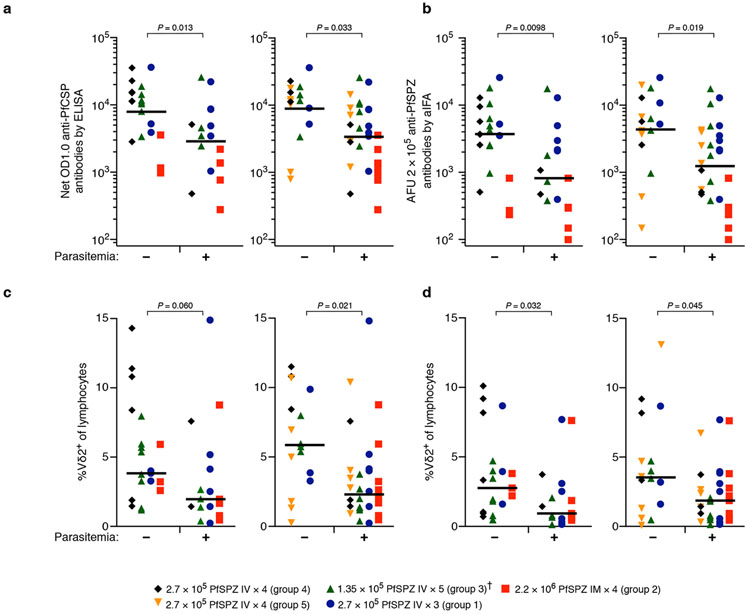
PfCSP and PfSPZ-specific antibody levels correlated with outcome when CHMI occurred 3 weeks and 21–25 weeks after final immunization (Fig. 3a,b). For this analysis, we assumed that subjects who developed parasitemia after the 3 week CHMI would also develop parasitemia after the 21–25 week CHMI, which is based on our earlier findings (Supplementary Fig. 1).
Figure 3. Correlation between immune responses and CHMI outcome.
(a) Antibodies to PfCSP were measured by ELISA (net OD1.0) 2 weeks after final immunization in subjects who did (+) and did not (−) develop parasitemia at 3 (left) and 21–25 (right) week CHMIs.
(b) Antibodies to PfSPZ were measured by aIFA (AFU 2 × 105) 2 weeks after final immunization in subjects who did (+) and did not (−) develop parasitemia at 3 (left) and 21–25 (right) week CHMIs.
(c) Frequency of Vδ2+ T cell subset among total lymphocytes 2 weeks after final immunization in subjects who did (+) and did not (−) develop parasitemia at 3 (left) and 21–25 (right) week CHMIs.
(d) Frequency of Vδ2+ T cells among total lymphocytes prior to immunization in subjects who did (+) and did not (−) develop parasitemia at 3 (left) and 21–25 (right) week CHMIs.
For a–d, since we expected subjects who were parasitemic at 3 weeks to again be parasitemic at 21–25 weeks, the immune data from individuals who were parasitemic at 3 weeks were included in the analysis for 21–25 week CHMI.
Statistical significance for all correlations was determined by stratified Wilcoxon test with vaccine regimen as co-variate. Bar denotes geometric mean (a,b) or median (c,d). Each dot represents one subject.
†See Fig. 1 for doses.
Cellular correlates.
The percentage of Pf-specific CD4 and CD8 T cells in the blood that produced IFN-γ, IL-2 and/or TNF-α did not correlate with outcome at the 3 or 21–25 week CHMIs (Supplementary Fig. 8). However, the absolute frequency of unstimulated Vδ2+ T cells as a percentage of total lymphocytes correlated with outcome at the 21–25 week CHMI (Fig. 3c). Interestingly, the frequency of the Vδ2+ T cell subset measured before the first vaccination also correlated with outcome at the 3 and 21–25 week CHMIs (Fig. 3d).
Role of PfSPZ antibodies in protection
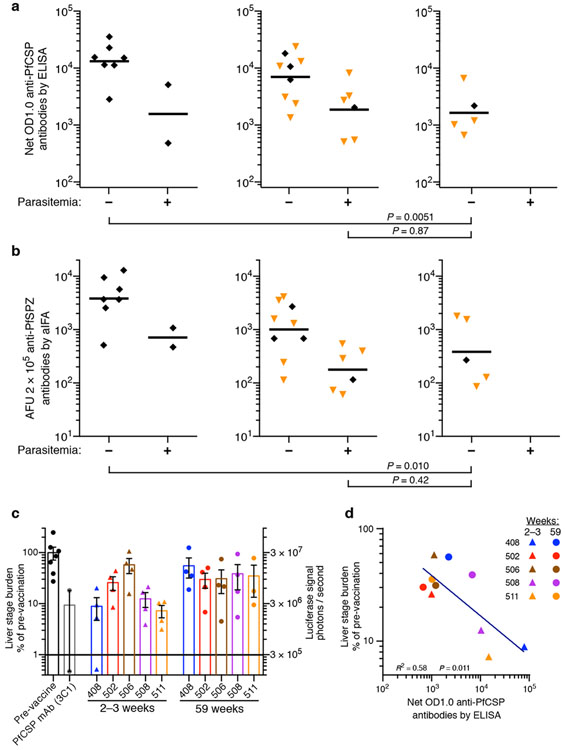
The finding that PfCSP- and PfSPZ-specific antibody levels two weeks after final immunization correlated with outcome of the 3 and 21–25 week CHMIs suggested that antibodies were a biomarker of a successful vaccine response; however, antibodies could also have a functional role in mediating protection14-16. To investigate this we assessed the magnitude of antibodies at the time of the 21–25 and 59 week CHMIs. At 59 weeks, PfCSP antibody responses in the five subjects who did not develop parasitemia were 8.0-fold lower (PfCSP geometric mean (GM) = 1640) than the responses among subjects who did not develop parasitemia at 3 weeks (PfCSP GM = 13200; P = 0.0051; Fig. 4a). Of note, the magnitude of PfCSP antibody responses in the 5 subjects at 59 weeks (PfCSP GM = 1640) was no different than antibody responses in subjects immunized with the same regimen who developed parasitemia at CHMI at 21–24 weeks (PfCSP GM = 1860; P = 0.87; Fig. 4a). Assessment of antibody responses against whole PfSPZ (Fig. 4b) also revealed a decline in Pf-specific antibodies over time.
Figure 4. Functional role of PfSPZ-specific antibodies.
(a) Antibodies to PfCSP (net OD1.0) measured by ELISA at the time of CHMI in subjects who received 4 doses of 2.7 × 105 PfSPZ IV and subsequently did (+) or did not (−) develop parasitemia at 3 (left), 21–24 (middle), or 59 (right) week CHMIs.
(b) Antibodies to PfSPZ (AFU = 2 × 105) measured by aIFA at the time of each CHMI in subjects who received 4 doses of 2.7 × 105 PfSPZ IV and subsequently did (+) or did not (−) develop parasitemia at 3 (left), 21–24 (middle), or 59 (right) week CHMIs.
(c) Effect of passive transfer of purified IgG on liver stage burden assessed by IVIS. The experiment was done once. Right Y-axis shows the raw luciferase signal. Left Y-axis shows percent signal in mice that received the IgG from each of the 5 subjects at each of the two time points as compared to the signal in the mice that received pre-vaccination IgG, which was set to be 100%.
(d) Correlation between PfCSP antibody abundance (net OD1.0) and liver-stage burden measured by luciferase expression in the FRG-huHep mice.
For a–b, comparison between groups was assessed by Mann-Whitney U test. Bar denotes geometric mean. Each dot represents one subject. For c, data are mean ± s.e.m.
To assess the in vivo functional activity of Pf-specific antibodies, we used immune deficient FRG mice reconstituted with human hepatocytes (FRG-huHep mice) capable of supporting liver stage development of Pf24. Total IgG from the five vaccine recipients that did not develop parasitemia following CHMI at 59 weeks was purified from plasma and serum. The IgG was passively transferred to FRG-huHep mice, and they were challenged by exposure to 50 mosquitoes infected with luciferase-expressing PfSPZ. Liver stage burden was quantified by whole animal imaging. The negative control was pooled IgG from the five subjects from before vaccination. Passive transfer of the positive control, 150 μg of the anti-PfCSP monoclonal antibody 3C1, reduced liver stage burden as compared to the negative control by ~90%. Purified IgG from the five vaccinated subjects taken 2–3 weeks after vaccination reduced liver stage burden by 88% (median), and IgG from 59 weeks after final immunization reduced liver stage burden by 65% (median) (Fig. 4c). There was higher inhibitory activity in IgG from 4/5 subjects at 2–3 weeks compared to 59 weeks, but the difference did not reach the level of statistical significance (P > 0.05 by Wilcoxon signed rank test). However, liver stage burden did correlate inversely with PfCSP antibody level (Fig. 4d).
PfSPZ-specific T cell activation is dependent on timing of CHMI
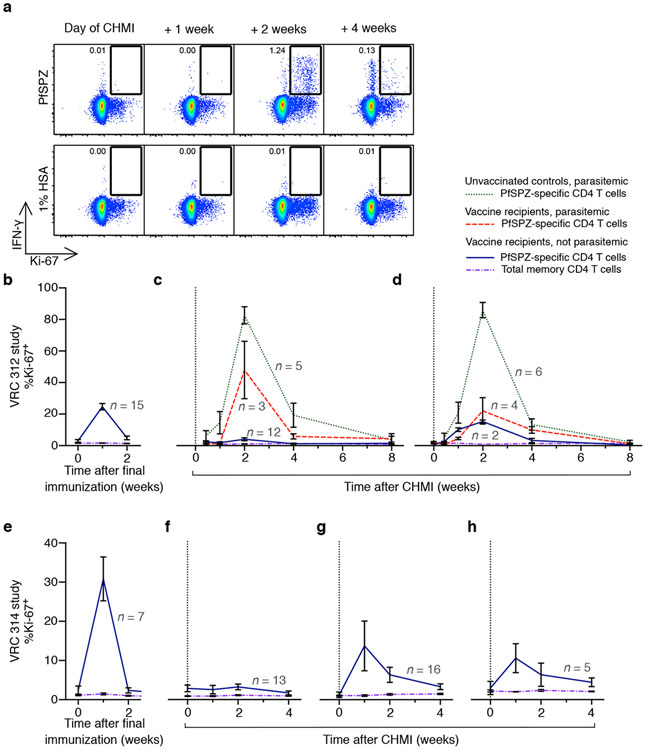
To provide additional insight into the potential mechanisms of protection, we assessed how CHMI affected PfSPZ-specific T cell responses in vivo after each CHMI. For this analysis, we identified PfSPZ-specific T cells by IFN-γ, IL-2, and TNF-α expression induced by ex vivo stimulation with PfSPZ antigens, and simultaneously measured the expression of Ki-67 (a marker used to detect recent lymphocyte cell division25; Fig. 5a). One week after final immunization in the VRC 312 (Fig. 5b) and VRC 314 (Fig. 5e) clinical trials, ~20–30% of PfSPZ-specific CD4 T cells were Ki-67+, demonstrating that vaccination induced T cell division. Ki-67 was only detected in PfSPZ-specific CD4 T cells, not in total memory CD4 T cells (Fig. 5b-h), providing evidence for PfSPZ-specificity. One to two weeks following the 3 week CHMI, Ki-67 was detected in ~40–60% of PfSPZ-specific CD4 T cells from parasitemic subjects (both vaccinated and unvaccinated subjects), showing that malaria infection was associated with activation of a high proportion of PfSPZ-specific CD4 T cells (Fig. 5c,d); in contrast, there were low to undetectable Ki-67+ PfSPZ-specific CD4 T cells in PBMCs from the 25 subjects who did not develop parasitemia from VRC 312 (n = 12; Fig. 5c) and VRC 314 (n = 13; Fig. 5f) studies after the 3 week CHMI. In contrast, one to two weeks after the 21–25 and 59 week CHMIs, ~10–20% of PfSPZ-specific CD4 T cells from subjects who did not develop parasitemia were Ki-67+ (Fig. 5d and Fig. 5g,h), compared to 0–1% on the day of the CHMI. These data suggest that there was differential antigen exposure in vivo when CHMI was done at 3 weeks compared to 21–25 or 59 weeks among subjects who remained without parasitemia. The percentage of Pf-specific CD4, CD8, or γδ T cells in blood did not change after CHMI at any time in non-parasitemic subjects (Supplementary Fig. 9a-f), nor did PfCSP-specific antibody levels (Supplementary Fig. 9g).
Figure 5. Activation of PfSPZ-specific CD4 T cells following CHMI.
PBMCs were isolated before and after the final vaccination and each CHMI from vaccinated subjects and unvaccinated controls in the VRC 312 and VRC 314 studies. Cells were incubated with PfSPZ or vaccine diluent (1% HSA), and IFN-γ, IL-2, TNF-α, and Ki-67 expression were assessed by flow cytometry.
(a) Gating example showing memory CD4 T cells at 0, 1, 2, and 4 weeks following CHMI in an unvaccinated control who developed parasitemia. PfSPZ-specific cells are identified by expression of IFN-γ following PfSPZ stimulation, and cells undergoing replication are identified by Ki-67.
(b) Percentage of either total memory CD4 T cells (purple, dot-dash) expressing Ki-67 or PfSPZ-specific CD4 T cells (blue, solid) expressing Ki-67 after final immunization in vaccine recipients who received 1.35 × 105 PfSPZ IV in the VRC 312 study.
(c–d) Frequency of cells (see key) expressing Ki-67 in vaccine recipients who did or did not develop parasitemia following CHMI at 3 (c) and 21 (d) weeks after final vaccination. Unvaccinated controls are also shown. Subjects were from the VRC 312 study.
(e) Same analysis as in b, for IV-vaccinated subjects in the VRC 314 study.
(f–h) Same analysis as in c–d, except subjects are IV-vaccinated subjects from the VRC 314 study, and CHMIs occurred 3 (f), 21–25 (g), and 59 (h) weeks after final vaccination.
For b–h, PfSPZ-specific cells are identified by any combination of IFN-γ, IL-2, or TNF-α. Data are mean ± s.e.m. Gray numbers on graph denote number of subjects in each group.
Tissue distribution of Pf-specific T cells
The low level of Pf-specific antibody at 59 weeks when all five vaccinated subjects were not parasitemic after CHMI (Fig. 4a,b) suggested that antibodies were unlikely to have had a major role in mediating protection at this time point. Therefore, PfSPZ-specific T cell responses were assessed in blood through the course of vaccination and following each CHMI.
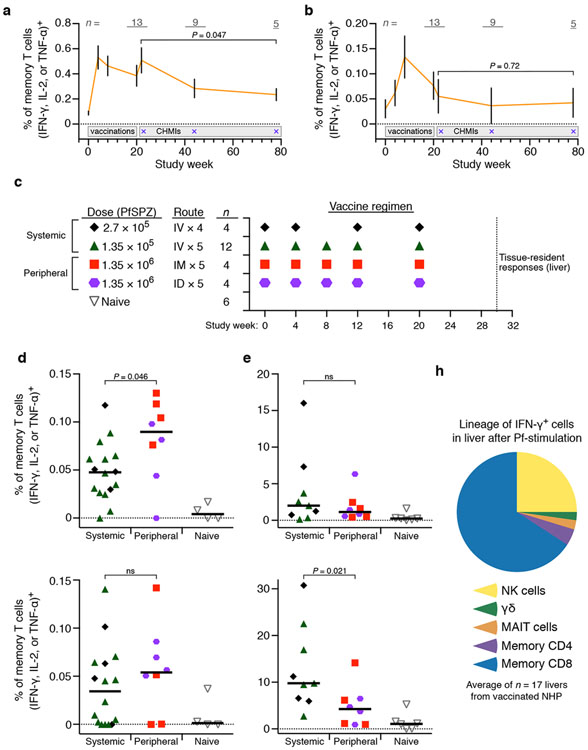
Longitudinal cellular responses in humans.
In PBMCs, cytokine-producing PfSPZ-specific CD4 T cell responses declined significantly over the course of 59 weeks in vaccinated subjects who remained without parasitemia (P = 0.047; Fig. 6a), and cytokine-producing PfRBC-specific CD8 T cell responses appeared during the vaccination series but returned to pre-vaccine levels shortly after final vaccination (Fig. 6b). Thus, neither antibodies nor Pf-specific T cells were readily detected in blood of the 5 vaccinated subjects that were not parasitemic after CHMI at 59 weeks. We hypothesized that the T cells resident in the liver were playing a critical role in protection10,26.
Figure 6. Circulating and liver-resident Pf-specific T cells in humans and NHPs.
(a–b) Longitudinal assessment of PfSPZ-specific CD4 T cell responses (a) and PfRBC-specific CD8 T cell responses (b) in subjects who received 4 doses of 2.7 × 105 PfSPZ IV and did not develop parasitemia at the 3, 21–24 and 59 week CHMIs. Gray numbers on graph denote number of subjects included at each time point. Data are mean ± s.e.m. P-values are for comparisons between immune responses at 2 and 59 weeks after the final immunization by Mann-Whitney U test.
(c) NHP study design.
(d) PfSPZ-specific CD4 (top) and PfRBC-specific CD8 (bottom) T cell responses in PBMCs of NHPs 2 weeks after final vaccination.
(e) PfSPZ-specific CD4 (top) and PfRBC-specific CD8 (bottom) T cell responses in livers of NHPs 10 weeks after final vaccination.
(f) Lineage of liver-resident lymphocytes in vaccinated NHP expressing IFN-γ following stimulation with PfRBC.
For d–e, bar denotes median, and between group comparisons were determined by Mann-Whitney U test. ns, non-significant (P > 0.05).
Tissue-resident T cell responses in NHP.
As liver-resident cellular immunity could not be directly assessed in the human subjects, such responses were assessed in NHPs following immunization with PfSPZ (Supplementary Fig. 10 and Supplementary Table 6). Immunogenicity studies with PfSPZ Vaccine in NHP previously provided immune data that guided successful translation to humans10,11. As we had previously shown that 1.35 × 105 PfSPZ administered SC did not induce detectable T cell responses in the blood or liver of NHPs10, we administered ten-fold more PfSPZ in each of five doses by the IM or ID routes and compared the T cell responses to five IV doses of 1.35 × 105 PfSPZ and four IV doses of 2.7 × 105 PfSPZ (Fig. 6c). PfSPZ-specific CD4 T cell responses in PBMCs were modestly higher in NHPs vaccinated by the peripheral (IM or ID) routes as compared to the systemic (IV) route (P = 0.046), and there were no differences in PfRBC-specific CD8 T cell responses in PBMCs (Fig. 6d). In contrast, IV administration induced two-fold higher frequencies of PfRBC-specific CD8 T cells in the liver compared to 6–10 fold higher total doses of PfSPZ administered IM or ID (Fig. 6e). Importantly, the frequency of PfRBC-specific CD8 T cell responses in the liver were ~100-fold higher than in PBMCs. Moreover, while multiple populations of IFN-γ-producing lymphocytes including NK, γδ, and CD4 T cells were identified in the liver of NHP, the majority (~60%) were CD8 T cells (Fig. 6f and Supplementary Fig. 11). The composition and differentiation state (i.e., memory phenotype) of lymphocytes in NHP liver largely reflect that of unvaccinated human liver samples, underscoring the biological relevance of the NHP model (Supplementary Fig. 11).
DISCUSSION
This was the first clinical trial of a malaria vaccine in which the first CHMI in one of the vaccine groups was done more than four weeks after final immunization, representing a shift beyond a search for short-term protection towards trials that focus on dose and regimen optimization for durable sterilizing protection. At 59 weeks after four doses of 2.7 × 105 PfSPZ, cumulative VE against CHMI was estimated to be 55%, the most durable efficacy against CHMI reported to date with an injectable malaria vaccine. In the vaccination regimens tested here, efficacy of PfSPZ Vaccine depended on both dose per vaccination and number of vaccinations. The estimated VE against CHMI done 3 weeks after immunization with 3 doses of 2.7 × 105 PfSPZ was 24% compared to 73% with 4 doses of 2.7 × 105 PfSPZ. Similarly, 4 or 5 doses of 1.35 × 105 PfSPZ conferred an estimated 25% efficacy against CHMI at 21 weeks compared to 55% with 4 doses of 2.7 × 105 PfSPZ. On the basis of these data, we hypothesize that additional increases in dose of PfSPZ Vaccine will further increase the magnitude and durability of protective efficacy. Ongoing studies using 4.5 × 105 to 2.7 × 106 PfSPZ per dose are assessing this against homologous CHMI, heterologous CHMI, and natural exposure in all age groups.
Route of administration influenced VE, further underscoring the importance of PfSPZ administration by the IV route in achieving protection with this vaccine. Completed studies in Mali, Tanzania, and Equatorial Guinea have provided the first data for the feasibility of direct venous inoculation (DVI) of PfSPZ Vaccine to adults in Africa27, and field studies in Africa have begun to determine the safety, efficacy, and feasibility of DVI administration in young children and infants.
An unexpected immunological finding was that the pre-vaccination frequency of circulating Vδ2+ T cells correlated with outcome of CHMI. Vδ2+ T cells recognize intracellular lipid metabolites (i.e., HMBPP) from Plasmodium28,29. It is possible that these cells play a role in the initial priming of adaptive immune responses through rapid Pf recognition, IFNγ production (Supplementary Fig. 7m), and/or by serving as antigen presenting cells30 at the time of immunization, leading to enhanced CD8 T cell priming31, γδ T cells have been shown to provide help to dendritic cells to facilitate protective responses to blood stage malaria32 and IFN-γ-secreting γδ T cells are a correlate of protection against blood stage malaria33. It is possible Vδ2+ T cells also mediate direct effector functions in the liver. A high frequency of circulating γδ T cells express CXCR6, a chemokine receptor that facilitates surveillance of the liver sinusoids22, and produce IFN-γ and perforin (Supplementary Fig. 7i-m), two potent effector molecules shown to mediate killing of intracellular Pf. γδ T cells have been shown to contribute to protection against pre-erythrocytic malaria in mouse models21 and expand in humans following whole SPZ immunization34. The correlation between γδ T cell frequency and CHMI outcome described herein suggests that PfSPZ Vaccine induces protective immunity not only through induction of conventional CD8 and CD4 T cell responses, but also γδ T cells. Such broad based T cell responses induced by live-attenuated vaccines may not occur after immunization with the most commonly used protein and viral vectored subunit vaccines, highlighting one of many important differences between these approaches.
We previously showed a dose-dependent increase in Pf-specific antibodies and multi-functional cytokine producing CD4 T cells with IV doses between 7.5 × 103 and 1.35 × 105 PfSPZ, but could not assess correlates of protection based on the high-level of protection at the 3 week CHMI11. The clear dose-response in the prior study likely reflects the wider range (18-fold) of doses given. In this present study, there was a smaller range of doses given IV, which likely accounts for the narrower range of antibody and T cell responses. The correlates of protection described herein are hypothesis-generating and require validation in large prospective studies. Moreover, correlates of protection may differ depending on the dose per vaccination, the number of vaccinations, the time of sampling, and history of malaria exposure.
The data presented here are consistent with the following role for antibodies: at the time of early CHMIs (3 weeks), antibody responses were highest and may have reduced the numbers of PfSPZ that successfully invaded hepatocytes (Fig. 4c,d)14-16, allowing for rapid elimination of the remaining parasites in the liver by cellular responses35,36, and thus low Ki-67 expression by PfSPZ-specific CD4 T cells in protected subjects. At the time of the later CHMIs (21-25 and 59 weeks), antibodies were considerably lower, resulting in more parasites reaching the liver after CHMI, and thus, greater activation (Ki-67 expression) of PfSPZ-specific CD4 T cells during liver stage parasite clearance (Fig. 5d,g,h).
Circulating Pf-specific T cell responses were low in blood at 59 weeks in all subjects that were not parasitemic after CHMI (Fig. 6a,b). Thus, if T cells are contributing to protection it may be due to an unmeasured aspect of the response in blood or differential responses in the liver. Indeed, tissue-resident Pf-specific CD8 T cell responses in the liver of PfSPZ-vaccinated NHP were highest after IV administration despite using 6–10 fold higher doses with the IM or ID routes. Infectivity studies in mice show that >90% of SPZ administered IM or ID fail to reach the liver12, and the parasite antigens are limited to muscle- or skin-draining lymph nodes37. IV administration, in contrast, results in the efficient delivery of attenuated PfSPZ to the liver, where they likely mediate priming of T cells that are programmed to remain as non-recirculating, liver-resident cells26. For this vaccine, efficacy is critically dependent on the route of vaccination. The data in NHP indicate this is likely because IV administration induces robust tissue-resident responses in the liver, whereas peripheral (IM or ID) administration results in T cell responses in blood, but more limited responses in the liver. Thus, for vaccines seeking to induce protective T cells, vaccine development efforts may be misled by focusing solely on maximizing T cell responses in the blood without considering how the vaccination strategy affects T cell responses at the infection site. In summary, the immune data presented herein support the conclusion that - while antibodies may have some contribution to protection early after final immunization - tissue-resident CD8 T cells are likely necessary for durable sterile protection10,17-20,26,38,39.
ONLINE METHODS
VRC 312 study.
VRC 312 (ClinicalTrials.gov #NCT01441167) was a phase 1, open-label, dose-escalation trial with CHMI to assess the safety, immunogenicity, and protective efficacy of PfSPZ Vaccine9,10 administered by intravenous (IV) injection. The VRC 312 clinical trial protocol, funding, study oversight, and data reporting have been previously described11. Subjects from the VRC 312 study were re-enrolled for repeat CHMI. PCR and thick blood smear (TBS) for detection of parasitemia were assessed in parallel. The criteria for initiation of treatment for malaria were: (a) a positive TBS, (b) two consecutive positive PCRs, or (c) one positive PCR with symptoms or signs consistent with malaria. Upon diagnosis of parasitemia, a 3-day course of atovaquone and proguanil (Malarone) was used for treatment.
VRC 314 study.
VRC 314 (ClinicalTrials.gov #NCT02015091) was a multi-institution, phase 1, open-label, dose escalation trial with CHMI, designed to assess the safety, immunogenicity, and protective efficacy of PfSPZ Vaccine administered by IV or intramuscular (IM) injection.
Complete inclusion and exclusion criteria are available at ClinicalTrials.gov. Briefly, malaria-naïve, healthy US adults, 18–45 years of age, were screened for good health, including laboratory testing for hepatitis B and C, HIV, and for pregnancy testing for women of childbearing potential. Baseline complete blood counts, creatinine, and alanine aminotransferase (ALT) were screened and only volunteers with normal values were enrolled. Volunteers with significant cardiovascular risk were excluded (i.e., 5 year risk of >10%)40. Exclusion criteria included known history of malaria infection or vaccination, the presence of hemoglobin S by electrophoresis, and splenectomy._The Vaccine Research Center (VRC) Clinical Trials Core at the National Institutes of Health (NIH) Clinical Center (CC) developed the protocol. The University of Maryland, Baltimore (UMB), Center for Vaccine Development (CVD) assisted with protocol development and study design. VRC and UMB CVD performed clinical duties. Sanaria produced, characterized, and prepared the syringes of PfSPZ Vaccine. The Walter Reed Army Institute of Research raised and infected mosquitoes, and assisted with the conduct of the CHMIs.
Study oversight and safety surveillance.
Study Oversight and Safety Surveillance was approved by the Intramural Institutional Review Board (IRB) of the National Institute of Allergy and Infectious Diseases (NIAID). U.S. Department of Health and Human Services guidelines for conducting clinical research were followed. Each step was reviewed and approved by a Safety Monitoring Committee and submitted to the Food and Drug Administration (FDA). The protocol was reviewed by FDA and conducted under IND 14826. Oral and written informed consent was obtained from all subjects.
Local injection site and systemic reactogenicity parameters were recorded through 7 days after vaccination as solicited adverse events (AEs). Unsolicited AEs were recorded until day 28 post-CHMI. Serious AEs and new chronic medical conditions were recorded through 24 weeks following last vaccination. AEs were graded using a Toxicity Grading Scale for Adults, adapted from FDA Guidance for Industry 2007. Malaria infection was recorded as a separate study endpoint. Therefore, associated signs and symptoms were not included in unsolicited AE listings.
Vaccine and vaccination.
PfSPZ Vaccine, composed of aseptic, purified, cryopreserved, metabolically active, radiation-attenuated P. falciparum sporozoites, was manufactured as described9 using Pf NF54 parasites and met all quality control release and stability assay specifications. Cryovials containing PfSPZ Vaccine were thawed and formulated using phosphate buffered saline (PBS) and human serum albumin (HSA) as diluent. Vaccines were administered by rapid intravenous injection of 1 mL volume into an antecubital vein or by intramuscular injection in two divided doses of 0.25 mL in the deltoid muscle.
CHMI.
CHMI was achieved by the bites of 5 PfSPZ-infected Anopheles stephensi mosquitoes that met standard infectivity criteria41-43. All challenges were performed with the 3D7 clone. Subjects were monitored from days 7–28 after CHMI until diagnosis and cure of parasitemia was documented. Blood draws for PCR were performed and analyzed daily as previously described11. Treatment with atovaquone and proguanil (Malarone) was initiated when two PCR results were positive for Pf parasitemia. For the week 3 CHMI for groups 1–3, based on the large number of vaccinated subjects and controls, half of the subjects in each vaccine group were equally randomized and 4 unvaccinated controls underwent CHMI on two consecutive days (total of 8 controls).
Efficacy analysis.
For the primary efficacy analysis, the results of the first CHMI for each vaccine group were compared to controls who underwent CHMI concurrently. To account for multiple comparisons, P-values < 0.01 were taken as evidence of an effect and P-values between 0.01–0.05 as suggestive. This threshold for significance of the primary analysis was specified in the protocol, to partially address the potential for type 1 error rate inflation. A strict Bonferroni adjustment would have been overly conservative as the study design has several features, including the sequential and dependent nature of the groups and the use of new controls for each CHMI that resembles a sequence of small trials rather than a traditional parallel multi-arm trial. A fixed threshold that did not depend on the final number of groups was preferable in this case where results of some CHMI were available before the next arm had been finalized. Secondary efficacy analyses compare the results from the different groups as well as describe the results of repeated challenges among those who remained parasite free in each group. No formal multiple comparison adjustment were employed for secondary endpoints.
When determining vaccine efficacy (VE), first VE was the VE (VE = 1 – relative risk) for the first CHMI. In instances in which a group underwent two CHMIs, vaccine recipients that developed parasitemia during the first CHMI did not undergo repeat CHMI. This was based on data in Supplementary Fig. 1 showing that vaccinated subjects that were parasitemic following CHMI and treated remained parasitemic following a second CHMI. Subgroup VE was VE among the subgroup of subjects that were not parasitemic at the prior CHMI. Cumulative VE is first VE multiplied by subgroup VE.
PfCSP ELISA.
For ELISA measurement of IgG against PfCSP, a recombinant Pf circumsporozoite protein (rPfCSPv2) was used. The rPfCSP (3D7 strain) is a 48 kDa protein with an N-terminal sequence SLGEND, with the first amino acid being residue 50 at the N-terminus and comprising the rest of the N- and C-termini with 22 NANP and 4 NVDP intervening repeats. 96-well plates (Nunc MaxiSorp Immuno Plate) were coated overnight at 4°C with 2.0 μg rPfCSP/mL in 50 μL per well in coating buffer (KPL). Plates were then washed three times with 1× imidazole-based wash solution containing 2 mM imidazole, 160 mM NaCl, 0.02% Tween-20, 0.5 mM EDTA and blocked with 1% Bovine Serum Albumin (BSA) blocking buffer (KPL) containing 1% non-fat dry milk for 1 hour at 37°C. Plates were washed three times and serially diluted samples (in triplicates) were added and incubated at 37°C for 1 hour. After washing three times, peroxidase-labeled goat anti-human IgG (KPL) was added at a dilution of 0.1 μg/mL and incubated at 37°C for 1 hour. After washing three times, ABTS peroxidase substrate was added for plate development, and the plates were incubated for 75 minutes at 22°C. The plates were read with a Spectramax Plus384 microplate reader (Molecular Devices) at 405 nm. The data were collected using Softmax Pro GXP v5. Data were fit to a 4-parameter sigmoidal curve, and the reciprocal serum dilution at which the optical density was 1.0 (OD1.0) calculated. To serve as assay controls, a negative control (pooled serum from non-immune individuals from a malaria-free area) and a positive control (serum from an individual with anti-PfCSP antibodies) were always included. The results are reported as net OD1.0, which was the OD1.0 of the post-immunization serum minus the OD1.0 of the pre-immunization serum. Samples were considered positive if the difference between the post-immunization OD1.0 and the pre-immunization OD1.0 (net OD1.0) was >50 and the ratio of post-immunization OD1.0 to pre-immunization OD1.0 (ratio) was >2.5.
Supplementary Table 7 lists all PfCSP antibody levels 2 weeks after final vaccination.
PfSPZ aIFA.
Purified PfSPZ (NF54 strain) from aseptic A. stephensi mosquitoes produced by Sanaria were resuspended in PBS (pH 7.4). 0.5 × 104 PfSPZ in 40 μL were added to each well of Greiner CELLSTAR clear-bottom black 96-well plates (Sigma-Aldrich). After addition of the suspension, plates were left at room temperature for 12–18 hour for air-drying. 50 μL of sera diluted in PBS with 2% BSA were added to each well containing air-dried PfSPZ. Sera samples were added at 2-fold dilutions. Plates were incubated at 37°C for 1 hour. Plates were washed in PBS three times. Alexa Fluor 488-conjugated goat anti-human IgG (Molecular Probes) was diluted to 1:250 in PBS with 2% BSA and 40 μL was added to each well. The plates were then incubated for 1 hour at 37°C. Plates were washed three times with PBS. 100 μL PBS was added to each well. Samples were assessed by scanning the entire surface of each well using an Acumen eX3 laser scanning imaging cytometer. The positive control was pooled human serum taken 2 weeks after the last immunization from 12 protected volunteers immunized 4 or 5 times with PfSPZ Vaccine in the VRC 312 clinical trial11. The data was plotted to fit a 4-parameter sigmoidal curve. Sera from malaria-naïve volunteers in the USA and Europe, including pre-immune sera, always register an AFU value less than 2.0 × 105 even at the highest concentration used in this assay (1:50 dilution). For sera that do bind to PfSPZ, 2.0 × 105 AFU falls in the exponential portion of the sigmoidal curves. Therefore 2.0 × 105 was chosen as the threshold in the aIFA assay, and the level of anti-PfSPZ antibodies for each volunteer is reported as the reciprocal serum dilution at which fluorescence intensity was equal to 2.0 × 105 AFU.
Supplementary Table 7 lists all PfSPZ antibody levels 2 weeks after final vaccination.
T cell assays.
Assessment of cellular immune responses using multi-parameter flow cytometry was done from PBMCs on cryopreserved samples at the completion of the study. After thawing, PBMCs were rested for 8 hours in complete RPMI (RPMI-1640 containing 2 mM L-glutamine, 10% v/v heat-inactivated FCS, 100 U/mL penicillin, 100 μg streptomycin, 25 mM HEPES buffer, 0.1% v/v 2-mercapto-ethanol) containing 25 U/mL Benzonase, and plated in 200 μL of media at 1.5 × 106 cells per well in a 96-well V-bottom plate and stimulated for 17 hours with: (a) PfSPZ Vaccine diluent (1% Human Serum Albumin, CSL Behring); (b) 1.5 × 105 viable, irradiated, aseptic, purified, cryopreserved PfSPZ from a single production lot; (c) 2 × 105 lysed, infected RBC consisting of >90% parasitemic late-stage schizonts (PfRBC) from a single production lot; or (d) a single lot of donor-matched uninfected erythrocytes (uRBC). PfSPZ and PfRBC were titrated for optimal sensitivity and specificity of detection of Pf-specific responses. For the last 5 hours of the stimulation, 10 μg/mL Brefeldin A (BD) was added to the culture. A positive control sample from a subject vaccinated with 5 doses of 1.35 × 105 PfSPZ IV and negative malaria-naïve control were included for each day subjects were analyzed to determine the reproducibility of antigen stimulation.
After stimulation, cells were stained as previously described44. The staining panels are shown in Supplementary Table 6, the gating tree is shown in Supplementary Fig. 4 and 5, and the antibody clones and manufacturers are shown in Supplementary Table 6. Briefly, cells were surface stained with CCR7 at 37°C for 20 min. Dead cells were identified by Aqua Live/Dead dye (Invitrogen) per manufacturer’s instructions. This was followed by 15 min surface staining at room temperature for CD4, CD8, CD14, CD20, CD38, CD45RA, CD56, TCR Vα7.2, CD161, TCRγδ, TCR Vδ1, TCR Vδ2, TCR Vγ9, or CXCR6. Cells were washed, fixed, and permeabilized using Cytofix/Cytoperm kit (BD) and stained intracellularly for CD3, IFN-γ, IL-2, TNF-α, Perforin, or Ki-67. Cells were washed, fixed in 0.5% paraformaldehyde, and acquired on a modified LSR II (BD Biosciences). All antigen-specific cytokine frequencies are reported after background subtraction of identical gates from the same sample incubated with the control antigen stimulation (HSA or uRBC).
Human liver samples.
Human liver samples were obtained under a clinical protocol unrelated to the PfSPZ vaccination protocol. The regional Ethical Review Board in Stockholm, Sweden, approved the study. Oral and written informed consent was obtained from all subjects. Livers were obtained during partial hepatectomy from living donors undergoing therapeutic tumor excision where only tumor-free unaffected tissue was used for isolation of immune cells. Immune cells were isolated using a previously described protocol45.
Functional assessment of vaccine-induced IgG.
Total IgG serum antibodies were purified from serum or plasma by affinity chromatography using Pierce Protein G Plus Agarose (Thermo Scientific) according to manufacturer’s instructions. Column eluted IgG was concentrated and buffer-exchanged into phosphate-buffered saline (pH 7.4) using Amicon Ultra 30,000 MWCO centrifugal filters (EMD Millipore). Protein concentration of the purified IgG was calculated by BCA assay (Thermo Scientific).
Human hepatocyte donor-matched FRG-huHep mice (male and female, age 5–9 months) were purchased from Yecuris, Inc. All animals were cared for in accordance with the NIH Guide for the Care and Use of Laboratory Animals. The Institutional Animal Care and Use Committee approved all animal procedures. Animals were randomly allocated to experimental and control groups.
Mice were intravenously injected with 8 mg/mouse of total IgG purified from vaccinated subjects or 150 μg of anti-PfCSP mouse monoclonal antibody (IgG3, clone 3C1) 16 hours before challenge. For mosquito bite challenge, Anopheles mosquitoes infected with P. falciparum expressing GFP-luciferase were generated as previously described46. Mosquito infection was quantified at day 10 post-blood meal and were used only if infection was >50% prevalence with an average of >10 oocysts/midgut. All qualifying mosquitoes were then pooled and distributed into cages with ~50 mosquitoes/mouse, up to 250 mosquitoes. Mice, in groups of up to 5, were then anesthetized with isoflurane and placed on a mesh screen covering the container of mosquitoes while under isoflurane anesthesia. Mosquitoes were then allowed to feed for 10 minutes with lifting of mice every minute to encourage probing and injection of sporozoites rather than blood feeding. After 10 minutes mice were returned to normal activity.
At day 6 post-infection (peak of liver burden), mice were imaged for liver stage burden using bioluminescence and IVIS imaging as previously described47,48. Briefly, mice were intraperitoneally injected with 100 μL of RediJect D-Luciferin (PerkinElmer) and, after 5 minutes, imaged with a 5-minute exposure. Liver stage burden was assessed by placing a region of interest (ROI) around the liver of each mouse and measuring total flux in photons/second. An identical ROI was placed over the thorax, which was used to subtract background signal. Liver stage burden of all mice was normalized to the mean of the negative control group, which received pre-immune IgG. Sample size was based on prior passive transfer experiments and calculated using Prism (GraphPad) and JMP Design of Experiment functionality (SAS). Pearson correlation coefficient was used to determine the relationship between Pf liver stage burden and PfCSP level. Investigators were blinded to treatment group during passive transfer of IgG, Pf infection, and measurement of luminescence.
NHP vaccinations.
Thirty healthy male and female Indian origin rhesus macaques (Macaca mulatta) with a mean (s.d.) age and weight of 6.1 (1.5) years and 8.7 (3.1) kg were singly housed in animal biosafety level 2 facilities and were monitored throughout the study for physical health, food consumption, body weight, and temperature. All animals were cared for in accordance with the NIH Guide for the Care and Use of Laboratory Animals. The Institutional Animal Care and Use Committee approved all animal procedures.
Study groups were balanced with respect to age, weight, and gender (equal numbers of males and females in each group). Sample size was based on prior NHP immunogenicity studies and calculated using Prism (GraphPad) and JMP Design of Experiment functionality (SAS). PfSPZ Vaccine was formulated and administered as for human injection with the following exceptions. For IV groups, PfSPZ in 500 μL was administered by direct venous inoculation into the saphenous vein. For the IM group, PfSPZ was administered to the left and right deltoid, and each injection was 500 μL in volume. For the ID group, PfSPZ was administered in the skin over the left and right deltoid, and each injection was 100 μL in volume. Immunizations and blood sampling occurred with the animal under anesthesia (10 mg/kg ketamine HCl).
NHP T cell assays.
Immune assays on PBMCs were batch-analyzed on cryopreserved samples at the completion of the study. PBMCs were isolated by density-gradient centrifugation from ACD anti-coagulated whole blood. Ten weeks after final immunization, animals were euthanized and liver tissue was processed as previously described10. For immune analysis, samples were thawed, rested, stimulated, stained, and analyzed using identical reagents, stimulation antigens, and protocol as the intracellular cytokine staining assay used for human PBMC samples (described above). The staining panel is shown in Supplementary Table 6, the gating tree is shown in Supplementary Fig. 10, and the antibody clones and manufacturers are shown in Supplementary Table 6. Investigators were blinded to treatment group during lymphocyte stimulations and flow cytometry gating. All antigen-specific cytokine frequencies are reported after background subtraction of identical gates from the same sample incubated with the control antigen stimulation (HSA or uRBC).
Statistical analyses.
Flow cytometry data was analyzed using FlowJo v9.8.5 (Tree Star). Statistical analyses were performed with Pestle v1.7 and SPICE v5.3 (M. Roederer)49, JMP 11 (SAS), and Prism 6 (GraphPad), and R v3.2.2 with RStudio v0.99.483.
For vaccine immunogenicity, comparisons between groups were performed using Kruskal-Wallis with Dunn’s post-test correction for multiple comparisons. If no differences between vaccines groups were identified by Kruskal-Wallis, then difference from pre-vaccination was assessed by Wilcoxon matched-pairs signed rank test with Bonferroni correction for multiple comparisons, as specified in the figure legends.
Immune responses were assessed 2 weeks after final immunization or pre-vaccination (as specified in the figure legends) and compared to outcome at either 3 week CHMI or 21-25 week CHMI. Assessment of immune responses that correlate with outcome at CHMI (parasitemia or no parasitemia) was made using a stratified Wilcoxon test controlling for vaccine regimen as a co-variate.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the vaccine trials participants for their contribution and commitment to vaccine research. We acknowledge the contributions of: our U.S. National Institutes of Health (NIH) Clinical Center (CC) and National Institute of Allergy and Infectious Diseases (NIAID) colleagues, especially J. Stein, J. Pierson, R. Eckes, P. Driscoll, L. Ediger, and the nursing staff of the 5NW, SCSU, 5SE-S, and 5SE-N units; our VRC colleagues, especially A. Mittelman, H. Harvey, M. Young, C. Artis, R. Hicks, P. Darrah, and T. Abram; our Sanaria and Protein Potential colleagues, especially Y. Abebe, J. Jackson, A. Awe, M. King, H. Huang, A. Patil, S. Matheny, J. Overby, Y. Wen, K. Nelson, V. Pich, M. Orozco, D. Padilla, E. Saverino, B. Jiang, L. Gao, R. Xu, E. Fomumbod, M. Laskowski, T.T. Wai, F. Beams, R. Thompson, and A. Hoffman for administrative, operations, and legal support, and T. Luke for insight and inspiration; the EMMES Corporation; the NIAID Institutional Review Board; the NIAID Office of Communications and Government Relations; the NIH CC Department of Laboratory Medicine; the NIH CC IND Pharmacy, and the NIH CC Patient Recruitment and Public Liaison Office. We appreciate the expert reviews of the Safety Monitoring Committee (A. Durbin, K. Kester, and A. Cross) and the assistance from the U.S. Military Malaria Vaccine Program, the Walter Reed Army Institute of Research Entomology Branch, and the Naval Medical Research Center, especially A. Reyes, Y. Alcorta, G. Banania, C. Fedders, M. Dowler, T. Savransky, D. Patel, C. Brando, K. Kobylinski, and K. Walker.
This work was supported by the intramural research program of the VRC, NIAID, NIH. Production and characterization of the PfSPZ Vaccine were supported in part by NIAID Small Business Innovation Research grants 5R44AI055229-11, 5R44AI058499-08, and 5R44AI058375-08 awarded to S.L.H. (Sanaria).
The findings and conclusions in this report are those of the authors and do not necessarily reflect the views of the funding agency or collaborators. The views expressed in this article are those of the author and do not necessarily reflect the official policy or position of the Department of the Navy, the Department of the Army, Department of Defense, nor the U.S. Government. This work was supported in part by work unit number 6000.RADI.F.A0309. J. Epstein, S. Davidson, and L. Garver are military service members. This work was prepared as part of their official duties. Title 17 U.S.C. §101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
Footnotes
COMPETING FINANCIAL INTERESTS
The authors declare competing financial interests:
T.L.R., E.R.J., P.F.B., A.G., S.C., A.M., M.L., A.J.R., T.L., A.G.E., R.E.S., N.K., T.M., B.K.L.S., and S.L.H. are salaried employees of Sanaria Inc., the developer and owner of PfSPZ Vaccine and the sponsor of the clinical trials. In addition, S.L.H. and B.K.L.S. have a financial interest in Sanaria Inc.
All other authors declare no competing financial interests.
REFERENCES FOR MAIN TEXT
- 1.World Malaria Report 2015. (World Health Organization, 2015). [Google Scholar]
- 2.Richie TL, et al. Progress with Plasmodium falciparum sporozoite (PfSPZ)-based malaria vaccines. Vaccine 33, 7452–7461 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kester KE, et al. Randomized, double-blind, phase 2a trial of falciparum malaria vaccines RTS,S/AS01B and RTS,S/AS02A in malaria-naive adults: safety, efficacy, and immunologic associates of protection. The Journal of infectious diseases 200, 337–346 (2009). [DOI] [PubMed] [Google Scholar]
- 4.Rts SCTP Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet 386, 31–45 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Plowe CV, Alonso P & Hoffman SL The potential role of vaccines in the elimination of falciparum malaria and the eventual eradication of malaria. J Infect Dis 200, 1646–1649 (2009). [DOI] [PubMed] [Google Scholar]
- 6.mal E.R.A.C.G.o.V. A research agenda for malaria eradication: vaccines. PLoS Med 8, e1000398 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roestenberg M, et al. Long-term protection against malaria after experimental sporozoite inoculation: an open-label follow-up study. Lancet 377, 1770–1776 (2011). [DOI] [PubMed] [Google Scholar]
- 8.Hoffman SL, et al. Protection of humans against malaria by immunization with radiation-attenuated Plasmodium falciparum sporozoites. J Infect Dis 185, 1155–1164 (2002). [DOI] [PubMed] [Google Scholar]
- 9.Hoffman SL, et al. Development of a metabolically active, non-replicating sporozoite vaccine to prevent Plasmodium falciparum malaria. Human vaccines 6, 97–106 (2010). [DOI] [PubMed] [Google Scholar]
- 10.Epstein JE, et al. Live attenuated malaria vaccine designed to protect through hepatic CD8(+) T cell immunity. Science 334, 475–480 (2011). [DOI] [PubMed] [Google Scholar]
- 11.Seder RA, et al. Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science 341, 1359–1365 (2013). [DOI] [PubMed] [Google Scholar]
- 12.Nganou-Makamdop K, et al. Reduced Plasmodium berghei sporozoite liver load associates with low protective efficacy after intradermal immunization. Parasite Immunol 34, 562–569 (2012). [DOI] [PubMed] [Google Scholar]
- 13.Kramer LD & Vanderberg JP Intramuscular immunization of mice with irradiated Plasmodium berghei sporozoites. Enhancement of protection with albumin. Am J Trop Med Hyg 24, 913–916 (1975). [DOI] [PubMed] [Google Scholar]
- 14.Potocnjak P, Yoshida N, Nussenzweig RS & Nussenzweig V Monovalent fragments (Fab) of monoclonal antibodies to a sporozoite surface antigen (Pb44) protect mice against malarial infection. J Exp Med 151, 1504–1513 (1980). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charoenvit Y, et al. Monoclonal, but not polyclonal, antibodies protect against Plasmodium yoelii sporozoites. J Immunol 146, 1020–1025 (1991). [PubMed] [Google Scholar]
- 16.Charoenvit Y, et al. Inability of malaria vaccine to induce antibodies to a protective epitope within its sequence. Science (New York, N.Y.) 251, 668–671 (1991). [DOI] [PubMed] [Google Scholar]
- 17.Schofield L, et al. Gamma interferon, CD8+ T cells and antibodies required for immunity to malaria sporozoites. Nature 330, 664–666 (1987). [DOI] [PubMed] [Google Scholar]
- 18.Weiss WR, Sedegah M, Beaudoin RL, Miller LH & Good MF CD8+ T cells (cytotoxic/suppressors) are required for protection in mice immunized with malaria sporozoites. Proc Natl Acad Sci U S A 85, 573–576 (1988). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doolan DL & Hoffman SL The complexity of protective immunity against liver-stage malaria. J Immunol 165, 1453–1462 (2000). [DOI] [PubMed] [Google Scholar]
- 20.Weiss WR & Jiang CG Protective CD8+ T lymphocytes in primates immunized with malaria sporozoites. PLoS One 7, e31247 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsuji M, et al. Gamma delta T cells contribute to immunity against the liver stages of malaria in alpha beta T-cell-deficient mice. Proc Natl Acad Sci U S A 91, 345–349 (1994). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tse SW, Radtke AJ, Espinosa DA, Cockburn IA & Zavala F The chemokine receptor CXCR6 is required for the maintenance of liver memory CD8(+) T cells specific for infectious pathogens. J Infect Dis 210, 1508–1516 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Plotkin SA Immunologic correlates of protection induced by vaccination. Pediatr Infect Dis J 20, 63–75 (2001). [DOI] [PubMed] [Google Scholar]
- 24.Sack BK, et al. Model for in vivo assessment of humoral protection against malaria sporozoite challenge by passive transfer of monoclonal antibodies and immune serum. Infection and immunity 82, 808–817 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McElroy AK, et al. Human Ebola virus infection results in substantial immune activation. Proc Natl Acad Sci U S A 112, 4719–4724 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tse SW, Cockburn IA, Zhang H, Scott AL & Zavala F Unique transcriptional profile of liver-resident memory CD8+ T cells induced by immunization with malaria sporozoites. Genes Immun 14, 302–309 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sissoko M, H. S, Shekalaghe S, and Olutu A. Submitted for publication January. (2016).
- 28.Chen ZW Multifunctional immune responses of HMBPP-specific Vgamma2Vdelta2 T cells in M. tuberculosis and other infections. Cell Mol Immunol 10, 58–64 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morita CT, Jin C, Sarikonda G & Wang H Nonpeptide antigens, presentation mechanisms, and immunological memory of human Vgamma2Vdelta2 T cells: discriminating friend from foe through the recognition of prenyl pyrophosphate antigens. Immunol Rev 215, 59–76 (2007). [DOI] [PubMed] [Google Scholar]
- 30.Brandes M, Willimann K & Moser B Professional antigen-presentation function by human gammadelta T Cells. Science (New York, N.Y.) 309, 264–268 (2005). [DOI] [PubMed] [Google Scholar]
- 31.Brandes M, et al. Cross-presenting human gammadelta T cells induce robust CD8+ alphabeta T cell responses. Proc Natl Acad Sci U S A 106, 2307–2312 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Inoue S, et al. Enhancement of dendritic cell activation via CD40 ligand-expressing gammadelta T cells is responsible for protective immunity to Plasmodium parasites. Proc Natl Acad Sci U S A 109, 12129–12134 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.D'Ombrain MC, et al. Association of early interferon-gamma production with immunity to clinical malaria: a longitudinal study among Papua New Guinean children. Clin Infect Dis 47, 1380–1387 (2008). [DOI] [PubMed] [Google Scholar]
- 34.Teirlinck AC, et al. Longevity and composition of cellular immune responses following experimental Plasmodium falciparum malaria infection in humans. PLoS Pathog 7, e1002389 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoffman SL, et al. Sporozoite vaccine induces genetically restricted T cell elimination of malaria from hepatocytes. Science (New York, N.Y.) 244, 1078–1081 (1989). [DOI] [PubMed] [Google Scholar]
- 36.Weiss WR, et al. A T cell clone directed at the circumsporozoite protein which protects mice against both Plasmodium yoelii and Plasmodium berghei. J Immunol 149, 2103–2109 (1992). [PubMed] [Google Scholar]
- 37.Amino R, et al. Quantitative imaging of Plasmodium transmission from mosquito to mammal. Nat Med 12, 220–224 (2006). [DOI] [PubMed] [Google Scholar]
- 38.Cockburn IA, et al. In vivo imaging of CD8+ T cell-mediated elimination of malaria liver stages. Proc Natl Acad Sci U S A 110, 9090–9095 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schmidt NW, Butler NS, Badovinac VP & Harty JT Extreme CD8 T cell requirements for anti-malarial liver-stage immunity following immunization with radiation attenuated sporozoites. PLoS Pathog 6, e1000998 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
METHODS-ONLY REFERENCES
- 40.Gaziano TA, Young CR, Fitzmaurice G, Atwood S & Gaziano JM Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk: the NHANES I Follow-up Study cohort. Lancet 371, 923–931 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lyke KE, et al. Plasmodium falciparum malaria challenge by the bite of aseptic Anopheles stephensi mosquitoes: results of a randomized infectivity trial. PLoS One 5, e13490 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chulay JD, et al. Malaria transmitted to humans by mosquitoes infected from cultured Plasmodium falciparum. Am J Trop Med Hyg 35, 66–68 (1986). [DOI] [PubMed] [Google Scholar]
- 43.Rickman LS, et al. Plasmodium falciparum-infected Anopheles stephensi inconsistently transmit malaria to humans. Am J Trop Med Hyg 43, 441–445 (1990). [DOI] [PubMed] [Google Scholar]
- 44.Lamoreaux L, Roederer M & Koup R Intracellular cytokine optimization and standard operating procedure. Nat Protoc 1, 1507–1516 (2006). [DOI] [PubMed] [Google Scholar]
- 45.Lecluyse EL & Alexandre E Isolation and culture of primary hepatocytes from resected human liver tissue. Methods Mol Biol 640, 57–82 (2010). [DOI] [PubMed] [Google Scholar]
- 46.Vaughan AM, et al. A transgenic Plasmodium falciparum NF54 strain that expresses GFP-luciferase throughout the parasite life cycle. Molecular and biochemical parasitology 186, 143–147 (2012). [DOI] [PubMed] [Google Scholar]
- 47.Miller JL, et al. Quantitative Bioluminescent Imaging of Pre-Erythrocytic Malaria Parasite Infection Using Luciferase-Expressing Plasmodium yoelii. PloS one 8, e60820 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sack BK, et al. Model for In Vivo Assessment of Humoral Protection against Malaria Sporozoite Challenge by Passive Transfer of Monoclonal Antibodies and Immune Serum. Infection and immunity 82, 808–817 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roederer M, Nozzi JL & Nason MC SPICE: exploration and analysis of post-cytometric complex multivariate datasets. Cytometry A 79, 167–174 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.