Abstract
A 56-year-old female diagnosed with hypertrophic obstructive cardiomyopathy and myocardial bridge (MB) of the left anterior descending (LAD) coronary artery underwent septal myectomy with resolution of her left ventricular outflow tract gradient. She had ongoing refractory symptoms of exertional angina and fatigue for over a decade and finally presented to our clinic to be re-evaluated for treatment. Provocative angiographic testing confirmed significant ischemia secondary to LAD MB. She underwent robotic totally endoscopic off pump unroofing of the LAD MB with complete relief of her symptoms and return to full activity. We conclude that patients undergoing septal myectomy for hypertrophic obstructive cardiomyopathy should be evaluated for MB and undergo unroofing of the bridge at the time of surgery.
Learning objective
A myocardial bridge (MB) is a condition in which a coronary artery, most often the left anterior descending, takes an intramuscular route and is covered by the myocardium leading to compression and potential ischemia. This case report adds to the growing body of evidence supporting the significance of considering MB in the overall management of hypertrophic obstructive cardiomyopathy, and the symptomatic relief that a patient can obtain from an unroofing procedure.
Keywords: Myocardial bridge, Hypertrophic obstructive cardiomyopathy, Left anterior descending coronary artery, Robotic surgery
Introduction
Myocardial bridge (MB) is a congenital anatomic variant that is often undiagnosed due to its asymptomatic nature. This occurs when part of a coronary artery, usually the left anterior descending (LAD), takes an intramuscular route through the myocardium, thereby allowing the myocardial fibers to form a “bridge” anterior to the burrowed artery. While this condition is usually benign, compression of the tunneled artery during systole can sometimes compromise distal blood flow and cause angina, arrhythmias, myocardial ischemia, and rarely death [1]. Both stenting and surgical procedures, such as coronary artery bypass grafting and myotomy, have been performed to resolve symptoms and hemodynamic abnormalities associated with MBs.
This case report describes a robotic beating-heart MB unroofing procedure on a patient, who previously underwent septal myectomy for hypertrophic obstructive cardiomyopathy (HOCM) via sternotomy, but continued experiencing refractory angina symptoms.
By presenting this case, we aim to highlight the symptomatic relief post-unroofing of an MB in a patient who experienced multiple surgeries to alleviate her symptoms, while acknowledging the benefits of robotic redo-beating heart surgery in select cases.
Case report
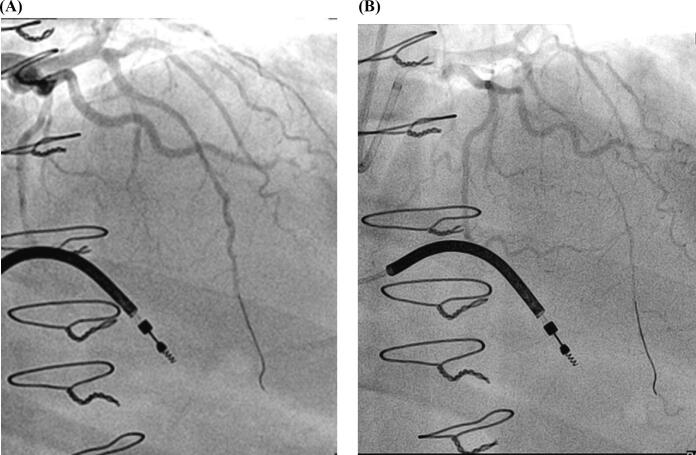
A 56-year-old woman presented to our clinic with a previously diagnosed LAD MB and a prolonged symptomatic history of unresolved angina and fatigue. This patient's medical history is notable for hypothyroidism, hyperlipemia, and HOCM. Following the diagnosis of HOCM with a significant left ventricular outflow tract (LVOT) gradient in 2005, the patient underwent ventricular septal ablation and had an implantable cardioverter defibrillator (ICD) placed. She was also noted to have a LAD MB at that time. Less than a year later, because of unresolved symptoms, she underwent a sternotomy and septal myectomy. Although recognized previously, the MB was not addressed during surgery as it was considered a normal variant. While a myectomy is considered the gold standard of treatment for HOCM [2], this patient experienced no significant symptomatic relief, despite the surgery achieving a normal pressure gradient across the LVOT. Due to persistent chest pain over the ensuing 5–6 years and failed medical therapy, the patient underwent a spinal stimulator placement (2011) which made the pain tolerable, but did not resolve it. The patient's symptoms began to interfere with daily activities, leading her to seek re-evaluation for further treatment at our clinic. She underwent provocative angiography with findings of significant LAD ischemia beyond the MB on stimulation with acetylcholine, dobutamine, and adenosine with a fractional flow reserve of 0.51, 0.79, 0.82 respectively (Fig. 1). Computed tomography angiography confirmed significant LAD bridging (Fig. 2). Transesophageal echocardiogram showed normal LV and valvular heart function, along with a normal gradient across the LVOT. After lack of efficacy of medical therapy for MB (including beta-blockers and calcium channel blockers), she was considered as a candidate for robotic redo surgery to unroof the bridge and increase coronary blood flow.
Fig. 1.
Pre-operative angiogram (A); pre-operative angiogram with provocative testing using adenosine (B).
Fig. 2.

Computed tomography angiography showing compression of the middle and distal portions of the left anterior descending coronary artery within the myocardium.
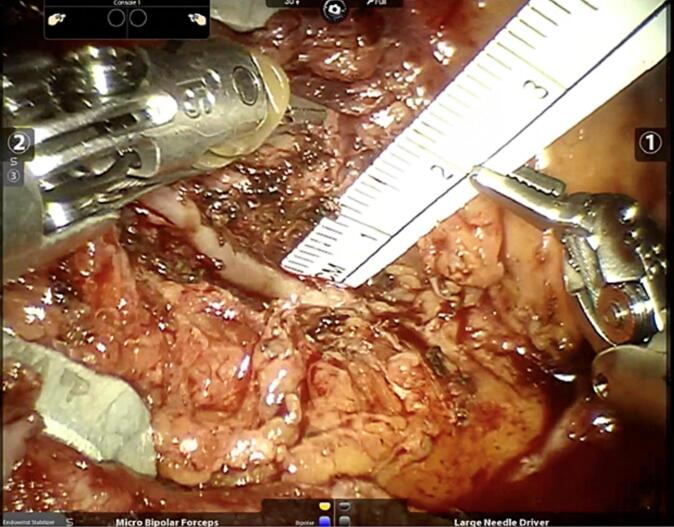
The patient underwent a totally endoscopic robotic-assisted off-pump unroofing of the LAD on the beating heart. This procedure was completed using the Da Vinci ™ SI surgical robot with the EndoWrist™ stabilizer (Intuitive Surgical Inc., Sunnyvale, CA, USA). Standard robotic endoscopic ports were placed and dissection of adhesions between the pericardium and the heart was performed. With the assistance of the EndoWrist stabilizer, the muscle and overlying adipose tissue were removed using low electrocautery monopolar energy (spatula) in the right hand and bipolar energy (micro bipolar) in the left hand along with sharp dissection (Potts scissors) in few areas. The MB, which was 5 cm in length and 1.5 cm in depth, was fully unroofed and the anterior surface of the LAD was completely exposed to show the total length of its intramyocardial course (Fig. 3). Papaverine solution was used topically to dilate the LAD and an intravenous vasodilator was administered to prevent spasm. The patient tolerated the procedure well and was discharged on postoperative day 1. At 1-month follow-up, she reported that her pre-operative symptoms had almost fully disappeared. Her only complaint was having some numbness around the incision and having a heart rate in the 90s. At 2 months post-operatively, she filled out a Seattle angina questionnaire and reported no angina or use of antianginal medications since surgery and significant improvement in daily activities. She noted feeling stronger and expressed interest in pursuing job opportunities previously hindered by pre-operative symptoms.
Fig. 3.
Left anterior descending myocardial bridge (unroofed).
Discussion
This case report describes a robotic totally endoscopic redo surgery on a beating heart to unroof a LAD MB in a patient with refractory symptoms. This patient previously had septal myectomy for HOCM via sternotomy but remained symptomatic despite multiple medical therapy regimens.
HOCM is a genetic cardiovascular disorder and is characterized by abnormal thickening of the myocardium, particularly in the interventricular septum. This hypertrophy can obstruct the outflow of blood from the left ventricle, resulting in impaired cardiac function. Symptoms of HOCM include dyspnea, angina, dizziness, and palpitations and can lead to complications such as arrhythmias, heart failure, and sudden cardiac death [3]. In patients with HOCM, these symptoms may be linked to the frequent component of concomitant intramural course of the LAD artery, otherwise known as MB [4]. In this condition, a coronary artery is covered by a band of muscle, causing significant compression of the artery during systole. Diagnostic evaluation of coronary angiography for a MB can display the “milking effect” - narrowing of the artery at systole and widening at diastole [5]. The clinical significance of MB has been more recently evaluated in symptomatic patients, with provocative angiographic testing performed in combination with physiologic assessment of the coronary microcirculation [6].
While our patient previously underwent a septal myectomy for HOCM, she continued to experience exertional chest pain and fatigue. Despite being known to have a MB, this was not addressed during her initial sternotomy. Given her ongoing symptoms, and the likely lack of experience with this entity, she underwent further interventions such as a spinal stimulator for severe chest pain after medical therapy was ineffective. However, it was clear that the unroofing of the MB should have been considered earlier in her course. While not a consistent practice, concomitant septal myectomy and MB unroofing would have been justified in this case due to the patient's severe symptoms interfering with her quality of life and lack of efficacy of medical therapy. This approach would have prevented subsequent surgical interventions. After failing medical therapy and undergoing provocative angiography, the correct diagnosis was made and redo-cardiac surgery with coronary unroofing was recommended.
An unroofing procedure entails dividing the myocardial muscle fibers that cover the bridged artery (LAD). Our patient's symptoms were completely resolved following the surgery, suggesting this to be the cause of her symptoms for over 15 years. Symptom relief is due to removal of the dynamic obstruction of the LAD secondary to the hypertrophied muscle that was covering it and causing ischemia. MB unroofing, although uncommon, has reasonably good data supporting it as a useful treatment for symptomatic patients who have failed medical therapy, and with good long-term outcomes [7].
We have previously described our operative technique for robotic totally endoscopic MB unroofing [8]. This arose from our experience with robotic beating heart totally endoscopic coronary artery bypass, where intramyocardial targets are routinely approached and not considered a contraindication [9]. We believe the enhanced visualization and magnification of the robotic scope provides a distinct advantage in visualizing the intramyocardial vessel's course. Furthermore, the robotic stabilizer's versatility in exposing the depths of the dissection is essential for this operation. When coupled with avoiding anticoagulation by eliminating cardiopulmonary bypass, we feel that complications of bleeding and right ventricular injury can be minimized.
Although prior sternotomy and thoracotomy can be considered relative contraindications for robotic surgery, advances in robotic-assisted techniques paired with an experienced team have enabled successful reoperations. Avoiding redo-sternotomy minimizes injury to vital structures upon re-entry. We have published our experience in redo robotic cardiac surgery [10] and showed excellent outcomes with redo robotic totally endoscopic approaches.
Our preference for beating heart surgery in this case aligns with the established benefits of preserving cardiac function and avoiding cardioplegic arrest. By integrating robotic technology, we aim to optimize outcomes and enhance safety in redo cardiac procedures.
In conclusion, the vast improvement in our patient's symptoms suggests that the MB was the cause of her symptoms. The unroofing procedure resolved her exertional angina and allowed her to return to normal physical activity. This report underscores the benefits of the robotic approach, including quick recovery and return to physical activity, particularly in a patient with prior sternotomy. This case report also highlights the association between HOCM and LAD MB. Provocative angiographic testing is warranted in all patients with an LAD MB who present with HOCM, and evaluation of possible LVOT obstruction secondary to a hypertrophic septum is necessary in patients with a symptomatic MB. Surgical management of both entities at the patient's initial presentation could have reduced unnecessary procedures and significant chronic symptoms. Evaluating the clinical significance of an MB remains challenging and requires a multidisciplinary team with experience in a wide variety of diagnostic and therapeutic options.
Consent statement
Informed consent was obtained from the patient for publication of this case report, including accompanying images and video.
Declaration of competing interest
Dr. Balkhy is a proctor for Intuitive Surgical. All other authors have nothing to disclose.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jccase.2024.01.001.
Appendix A. Supplementary data
The following is the supplementary data related to this article.
Robotic totally endoscopic off-pump unroofing of LAD myocardial bridge in a patient with previous sternotomy for ventricular septal myectomy.
References
- 1.Lee M.S., Chen C.H. Myocardial bridging: an up-to-date review. J Invasive Cardiol. 2015;27:521–528. [PMC free article] [PubMed] [Google Scholar]
- 2.Maron B.J., Desai M.Y., Nishimura R.A., Spirito P., Rakowski H., Towbin J.A., et al. Management of hypertrophic cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79:390–414. doi: 10.1016/j.jacc.2021.11.021. [DOI] [PubMed] [Google Scholar]
- 3.Stroumpoulis K.I., Pantazopoulos I.N., Xanthos T.T. Hypertrophic cardiomyopathy and sudden cardiac death. World J Cardiol. 2010;2:289–298. doi: 10.4330/wjc.v2.i9.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basso C., Thiene G., Mackey-Bojack S., Frigo A.C., Corrado D., Maron B.J. Myocardial bridging, a frequent component of the hypertrophic cardiomyopathy phenotype, lacks systematic association with sudden cardiac death. Eur Heart J. 2009;30:1627–1634. doi: 10.1093/eurheartj/ehp121. [DOI] [PubMed] [Google Scholar]
- 5.Juilliére Y., Berder V., Suty-Selton C., Buffet P., Danchin N., Cherrier F. Isolated myocardial bridges with angiographic milking of the left anterior descending coronary artery: a long-term follow-up study. Am Heart J. 1995;129:663–665. doi: 10.1016/0002-8703(95)90312-7. [DOI] [PubMed] [Google Scholar]
- 6.Rogers I.S., Tremmel J.A., Schnittger I. Myocardial bridges: overview of diagnosis and management. Congenit Heart Dis. 2017;12:619–623. doi: 10.1111/chd.12499. [DOI] [PubMed] [Google Scholar]
- 7.Wang S., Wang S., Lai Y., Song Y., Cui H., Song C., et al. Midterm results of different treatment methods for myocardial bridging in patients after septal myectomy. J Card Surg. 2021;36:501–508. doi: 10.1111/jocs.15226. [DOI] [PubMed] [Google Scholar]
- 8.Mirzai S., Patel B., Balkhy H.H. Robotic totally endoscopic off-pump unroofing of left anterior descending coronary artery myocardial bridge: a report of two cases. J Card Surg. 2019;34:735–737. doi: 10.1111/jocs.14094. [DOI] [PubMed] [Google Scholar]
- 9.Balkhy H.H., Nisivaco S., Kitahara H., Torregrossa G., Patel B., Grady K., et al. Robotic off-pump totally endoscopic coronary artery bypass in the current era: report of 544 patients. Eur J Cardiothorac Surg. 2022;61:439–446. doi: 10.1093/ejcts/ezab378. [DOI] [PubMed] [Google Scholar]
- 10.Kitahara H., Wehman B., Balkhy H.H. Can robotic-assisted surgery overcome the risk of mortality in cardiac reoperation? Innovations (Phila) 2018;13:438–444. doi: 10.1097/IMI.0000000000000567. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Robotic totally endoscopic off-pump unroofing of LAD myocardial bridge in a patient with previous sternotomy for ventricular septal myectomy.