Abstract
To estimate the 2009–2010 death rates, causes, and patterns of mortality in rural Cambodia, we conducted active, population-based death surveillance in 25 rural villages of Cambodia from March 2009 to August 2010. Among the population of 28 053 under surveillance, 280 deaths were reported and explored by physician-certified verbal autopsies, using the International Classification of Diseases 10, yielding an overall mortality rate (MR) of 6.7/1000 persons-year (95% CI 5.74–7.68). The MR was 39.1/1000 live births for those younger than 5 years old. Infants accounted for 5.4% of all deaths. In children younger than 5 years, infectious and parasitic diseases were the leading causes of death. In children 5 to 14 years, 3 out of 4 deaths were due to injuries. Adult deaths were mainly attributed to noncommunicable diseases (52%). We conclude that this rural population is facing a substantial burden of noncommunicable diseases while still struggling with infectious diseases, respiratory diseases in particular.
Keywords: mortality, rural health, Cambodia, verbal autopsy
Background
Policy makers need accurate and timely information on mortality to determine evidence-based public health priorities. Information on mortality and cause of death is available for 72% of the world’s population, providing global or regional data from countries with established reporting systems.1 While regional estimates may be useful for the observation of larger trends, those estimates cannot be deemed representative of all countries in an economically diverse region, nor can they be relied on for public health policy decisions at a national level. Detailed mortality data are lacking in Cambodia, a resource-poor Southeast Asian country2 with a largely rural (~80%) population of 13.4 million.3
There is no complete civil registration or vital statistics system in Cambodia.3 Deaths are recorded in village and district registries and not systematically reported to higher administrative levels. Cause of death certificates are not required prior to body cremation or burying. Due to the observance of religious rituals, as well as to economic barriers (including cost of hospitalization and of transportation of the corpses), most deaths occur at home. A 2005 study in rural Cambodia showed that up to 95% of deaths occur at home.4 Hospital-based mortality data provide scarce information, representing, by definition, deaths occurring at hospital only, and only 13 diseases and syndromes (acute flaccid paralysis, meningo-encephalitis, encephalitis, rabies, acute lower respiratory tract infection, diphtheria, measles, dengue fever, acute jaundice, acute watery diarrhea, bloody diarrhea, neonatal tetanus, and unknown diseases occurring in a cluster).
The only sources of information on mortality in Cambodia are estimates from the Demographic and Health Survey (DHS) conducted every 5 years since 20005,6 from the National Population Census3 and from international organizations.7 The successive DHS presented mortality rates (MR) estimates for early ages (neonatal, postneonatal, infant, child, and under-5 MR). Causes of deaths were only explored in 2005 and in children only.
This study is the first to provide estimates on age-specific mortality rates for all causes of death in both hospital and at-home settings in Cambodia. Observations in the differences in trends between at-home deaths and hospital deaths will allow the public health community to consider the representativeness of hospital-based reporting alone when establishing vital statistics systems and when interpreting data for policy decisions. Finally, data from a relatively wealthy rural area are used to provide an idea of what the future trends in mortality may be in rural Cambodia as the country’s economic development continues to mature.
Based on an existing community-based surveillance of febrile diseases in Kampong Cham, Cambodia’s largest rural province,8 we conducted a mortality study in the same area to estimate the 2009–2010 death rates, and causes and patterns of mortality in this population, with a particular attention to respiratory diseases. We also investigated if the distribution of deaths occurring at hospital were representative of those occurring at home.
Methods
We conducted active, population-based death surveillance in 25 villages of 4 districts of Kampong Cham province, Cambodia, from March 2009 to August 2010. The 25 villages are situated along the national road, within a 40-km radius around Kampong Cham city, where the main sources of income are agriculture, forestry, and fishing.
Health workers (HWs; N = 66) involved in the surveillance of febrile illnesses recorded all consecutive vital events (births and deaths). They collected preliminary information on each death (name, age, date, place, and cause of death according to the family). Mortality reports were then cross-checked with the village chiefs and monks by our study team to ensure information completeness. Monks and village authorities conduct funerals before cremation at the pagoda or burial on family land.
With family consent we investigated each mortality report using a verbal autopsy (VA) approach.9 Trained nonmedical interviewers conducted interviews with next of kin to ascertain symptoms, signs, and circumstances preceding death. The VA questionnaire comprised an open-narrative section and 100 close-ended questions adapted from the WHO VA tool. Questionnaires were administered in Khmer language. Medical charts were collected from health facilities for cases recently admitted at hospital. To avoid recall bias, VA was not conducted when the death had occurred more than 3 months earlier. VA was also not conducted for accidental or violent deaths when they were confirmed as such by the families, the HW, and the village chiefs. Maternal deaths were investigated through the ongoing National Maternal Deaths Audit (NMDA) program. Audit results were shared by the provincial program coordinator.
Two experienced physicians independently reviewed the VA reports and hospital medical charts to determine an underlying cause of death for each case using their clinical judgment. They manually coded their conclusions using the International Classification of Diseases, version 10 (ICD-10), at the level of chapters and subchapter headings. Discordant conclusions between the physicians were reviewed by the study medical coordinator and another physician to find a consensus on a cause of death. Once agreed on, that cause of death was considered final. The study coordinator assigned the relevant ICD-10 codes for the accidental and violent deaths.
The CDC, IVI, Pasteur Institute and Cambodian Ethics Committees approved the study. Informed consent was obtained from respondents before data collection.
Data Analysis
Maternal death was defined as death of a woman while pregnant or within 42 days of termination of pregnancy. Stillbirth or fetal death was defined as death prior to complete birth. Infants were children aged 0 to 11 months. The neonatal period began with birth and ended 27 days after birth. Early neonatal deaths were defined as deaths during the first 7 days of life. The postneonatal period was defined as 28 or more days to 1 year old.
Population denominators came from a village population census conducted in December 2009, the midterm of the study period. A small proportion (0.9%) of the population moved from the area during the course of an influenza-like illness (ILI) surveillance study indicating that the population was generally stable.8 This census, conducted by village chiefs, did not report the gender and ages of the population. Therefore, we derived the gender and age structures from those of the 2009 cohort for ILI surveillance which recruited 55% of the village population.8
The neonatal, infant, and under-5 MR were the number of deaths in these age groups divided by the number of live births during the study period, expressed per 1000 live births. MR for the population over 5 years were calculated by 1000 person-years (p-y). Age-specific MRs were calculated by dividing the number of deaths in each age group by the number of population-years in each age group. Cause-specific MR were the relevant number of deaths for a given cause per 1000 persons/year surveyed.
We determined that influenza was active in August-December 2009, as shown by the Cambodia’s National Influenza Center reports to FluNet (http://www.who.int/influenza/gisrs_laboratory/flunet/en/).
A multivariate logistic regression analysis was performed to identify factors associated with death in a health care facility. We explored the following factors: (1) age, gender, and occupation of the deceased; (2) wealth of the deceased’s family (characterized by household possessions) and education of the household head; and (3) cause of death and duration of final illness. Factors with a level of significance in bivariate analysis of P < .20 were included in the model which was run using a stepwise backward approach.
Analyses were performed using Stata 11.0 (StataCorp, College Station, TX). Statistical significance was defined at P < .05. Odds ratios (ORs) are given with their 95% confidence interval (95% CI).
Results
At midterm of the study period, in December 2009, 28 053 persons resided in the 25 villages under active surveillance, including 10 632 children younger than 15 years (Table 1). Median village population was 834 (range: 334–3954). A total of 280 deaths occurred during the study period, resulting in an overall MR of 6.7/1000 persons-years (95% CI 5.7–7.7). Of these, 50.3% were males and the median age at death was 59 (IQR 34.5–78 years). The highest MR occurred in the 65 and older group (Table 1). Gender-specific rates were 6.2/1000 p-y for females and 7.2 for males (P = .17). Male MR was significantly higher than female MR among 15- to 24-year-olds (3.4/1000 vs 0.5/1000 respectively; P = .007; results not shown).
Table 1.
Study Population and Deaths Reported From March 2009 to August 2010, in 25 Villages of Kampong Cham Province, Cambodia.
| Population Under Surveillance | Deaths Reported During the Study Period | Percentage of Overall Number of Deaths | Mortality Rates | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| Age Group | Male | Female | All | Male | Female | All | All | All | 95% CI | Unit |
| 0–11 months | 213 | 167 | 380 | 10 | 5 | 15 | 5.4 | 20.9 | 11.8–34.3 | Per 1000 live births |
| 12–59 months | 1523 | 1520 | 3043 | 5 | 8 | 13 | 4.6 | 18.1 | 9.7–30.8 | Per 1000 live births |
| 5–14 years | 3621 | 3589 | 7209 | 3 | 1 | 4 | 1.4 | 0.4 | 0.1–1.2 | Per 1000 p-y |
| 15–44 years | 5445 | 6572 | 12 017 | 38 | 25 | 63 | 22.5 | 3.5 | 2.5–4.7 | Per 1000 p-y |
| 45–64 years | 1563 | 2382 | 3945 | 30 | 34 | 64 | 22.9 | 10.8 | 7.9–14.6 | Per 1000 p-y |
| 65+ years | 632 | 826 | 1458 | 55 | 66 | 121 | 43.2 | 55.3 | 44.4–68.6 | Per 1000 p-y |
| Total under 5 years | 1736 | 1687 | 3423 | 15 | 13 | 28 | 10.0 | 39.1 | 26.1–56.0 | Per 1000 live births |
| Total | 12 997 | 15 056 | 28 053 | 141 | 139 | 280 | 100.0 | 6.7 | 5.7–7.7 | Per 1000 p-y |
Among the 7343 women aged 15 to 49, 716 live births and 125 deaths were reported during the study period, including 1 maternal death.
Of the 3423 children younger than 5 years, 28 died, accounting for 10.0% of all deaths during the study. The MR for children younger than 5 years was 39.1 per 1000 live births (95% CI 26.1–56.0). Infants deaths accounted for 15 (5.4%) of all deaths, yielding an infant death rate of 20.9/1000 live births (95% CI 11.8–34.3). Of 3 neonatal deaths, all occurred during the early neonatal period. The neonatal MR rate was 4.2/1000 live births. There were no recorded stillbirths or fetal deaths. There were no statistically significant differences between MR in males versus females for either infants or children.
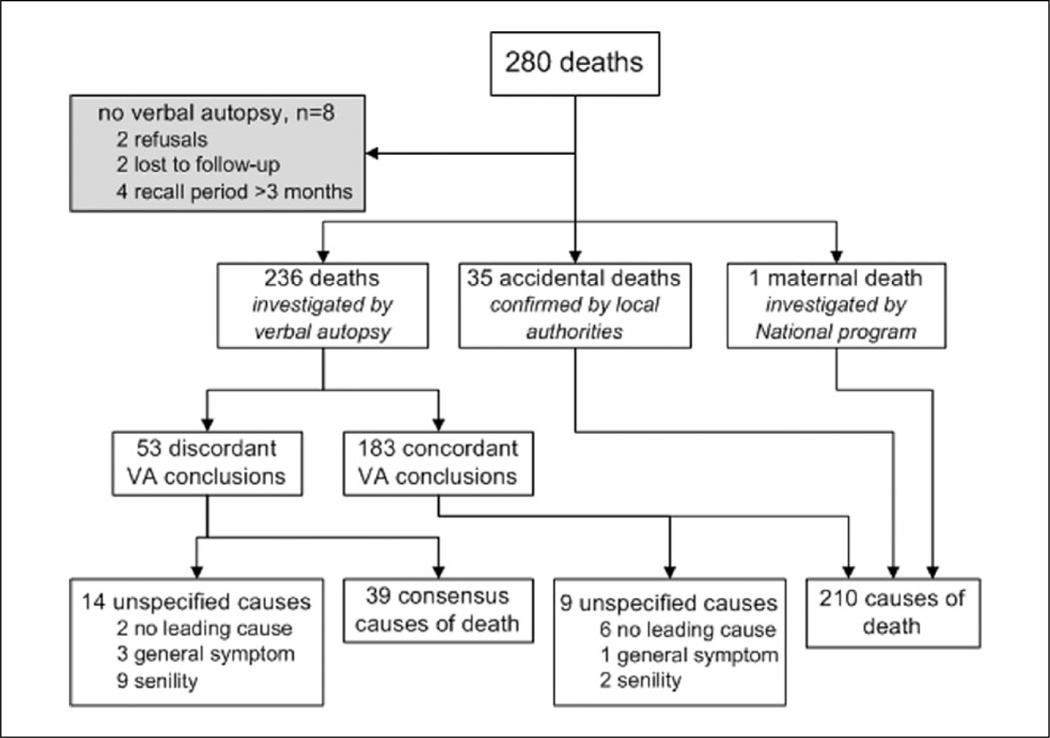
We investigated 236 cases by VA. The median time between death and VA was 17 days (IQR 12–23 days). Almost all (99%) respondents were living with the deceased at their time of death. The median interview duration was 30 minutes. The physicians assigned the same cause of death to 183 (77.5%) of VAs. Of the 53 initial VA discordances between the 2 physicians, 66% were related to infants and elderly deaths. The reviewers reached a consensus on cause for 39 of the discordant cases. Thirty-five cases were confirmed to be accidental, while 1 was a maternal death investigated by the NMDA program. In 8 cases, the VA was not conducted because the recall period exceeded 3 months (n = 4), the next of kin refused the investigation (n = 2) or the families were lost to follow-up (n = 2). Of all 272 coded deaths, 23 remained with an unspecified cause of death (Figure 1).
Figure 1.
Causes of death investigation, N = 280 deaths in 25 villages of Kampong Cham province, Cambodia, from March 2009 to August 2010.
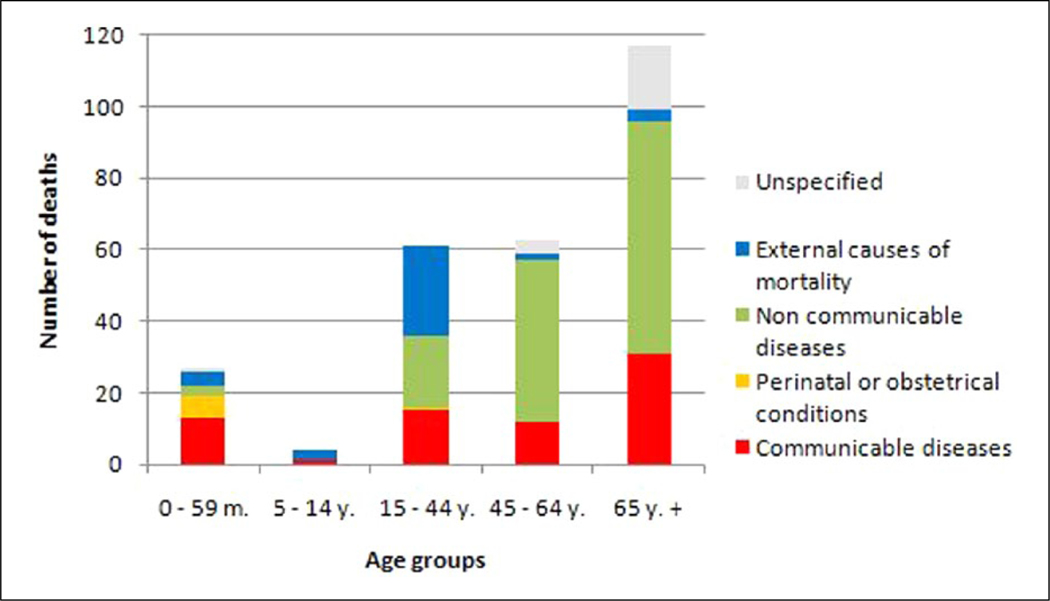
Causes of death in the population aged 0 to 15 years differed by age subgroup (Figure 2). In children younger than 5 years, communicable diseases (n = 13/28, 46%) were the leading cause with the highest cause-specific MR (2.53/1000; Table 2). Perinatal conditions were the second most frequent cause with 6 cases, including 3 newborns who died following delivery complications. Three of the 4 children aged 5 to 14 years died due to external causes (road accident and drowning), and the last due to tetanus in a partially vaccinated child. Cause of death could not be determined for 2 infants. In both cases, the family attributed the death to “throat infection.”
Figure 2.
Causes of death by age group in 25 villages of Kampong Cham province, Cambodia, from March 2009 to August 2010. N = 272 cases with coded cause of death.
Table 2.
Leading Causes of Death, by Age Group and Gender, Among 10 632 Children Younger Than 15 Years, in 25 Villages of Kampong Cham Province, Cambodia, From March 2009 to August 2010, N = 32 Death Cases.
| Children Younger Than 5 Years | 5–14 Years | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| 0–11 Months | 12–59 Months | Total Younger Than 5 Years | Total | |||||||
|
|
|
|
|
|||||||
| Leading Cause of Death | All | All | All | Female | All | All | ||||
|
|
|
|
|
|
|
|
||||
| Title (ICD10 Blocks) | n | Percentage | n | Percentage | n | Percentage | Percentage | MR (‰) | n | Percentage |
| Communicable diseases | 7 | 47 | 6 | 46 | 13 | 46 | 38 | 2.53 | 1 | 25 |
| Acute lower respiratory diseases (J09-J22) | 3 | 4 | 7 | 25 | 43 | 1.36 | 0 | |||
| Intestinal infectious diseases (A00-A09) | 2 | 0 | 2 | 7 | 50 | 0.39 | 0 | |||
| Arthropod-borne viral fevers (A90-A99) | 2 | 0 | 2 | 7 | 0 | 0.39 | 0 | |||
| Tetanus (A35) | 0 | 0 | 1 | 4 | 100 | 0.19 | 1 | |||
| Septicemia, unspecified (A41) | 0 | 1 | 1 | 4 | 100 | 0.19 | 0 | |||
| Varicella (B01) | 0 | 1 | 1 | 4 | 0 | 0.19 | 0 | |||
| Perinatal conditions | 6 | 40 | 0 | 0 | 6 | 21 | 67 | 1.17 | — | — |
| Complications of pregnancy, labor, and delivery (P00-P04) | 3 | 0 | 3 | 11 | 67 | 0.58 | 0 | |||
| Metabolic and digestive disorders (P70-P78) | 2 | 0 | 2 | 7 | 100 | 0.39 | 0 | |||
| Other disorders (P90-P96) | 1 | 0 | 1 | 4 | 0 | 0.19 | 0 | |||
| Noncommunicable diseases | 0 | 0 | 3 | 23 | 3 | 11 | 100 | 0.58 | 0 | 0 |
| Malignant neoplasms (C00-D48) | 0 | 1 | 1 | 4 | 100 | 0.19 | 0 | |||
| Diseases of the blood (D50-D89) | 0 | 1 | 1 | 4 | 100 | 0.19 | 0 | |||
| Congenital malformations (Q00-Q99) | 0 | 1 | 1 | 4 | 100 | 0.19 | 0 | |||
| External causes of mortality | 0 | 0 | 4 | 31 | 4 | 14 | 25 | 0.78 | 3 | 75 |
| Transport accidents (V01-V99) | 0 | 1 | 1 | 4 | 100 | 0.19 | 1 | |||
| Accidental drowning (W70) | 0 | 3 | 3 | 11 | 0 | 0.58 | 2 | |||
| Unknown or unspecified | 2 | 13 | 0 | 2 | 7 | 0 | 0.39 | 0 | ||
| No leading cause identified | 1 | 0 | 1 | 4 | 0 | 0.19 | 0 | |||
| No verbal autopsy conducted | 1 | 0 | 1 | 4 | 0 | 0.19 | 0 | |||
| Total | 15 | 13 | 28 | 100 | — | — | 4 | |||
MR: mortality rate per 1000 person-years of same age. Percentage: number of deaths by cause in the age group, divided by the number of deaths in the age group.
The main causes of 248 deaths among those 15 or older were noncommunicable diseases (NCDs; n = 130, 52%), followed by communicable diseases (CDs; n = 58, 23%) and violent/accidental causes (n = 30, 12%; Table 3). There were differences in rank for causes of death between age groups (Figure 2). In adults aged 15 to 44 years, 29% of deaths (n = 18) were caused by traffic accidents, classified under external cause of death. More men died from accidental causes than women in this group (sex ratio 4:1, P = .002; data not shown). CDs were the second most frequent leading causes of death (n = 15, 24%), with HIV disease and tuberculosis being the most frequent (Table 3). Among the persons aged 45 to 64 years, the most frequent cause of death was NCDs (n = 45/64, 70%), including malignant neoplasms (n = 19, 29%) and vascular diseases (n = 16, 25%; Table 3). Finally, among persons aged 65 or older years, circulatory diseases (n = 33, 27%), respiratory diseases (n = 18, 15%), and neoplasms (n = 18, 15%) caused the most deaths. Deaths due to unknown cause were more frequent in this group (n = 22, 18%; Table 3).
Table 3.
Leading Causes of Death by Gender Among 17 421 Subjects Aged 15 Years and Older, in 25 Villages of Kampong Cham Province, Cambodia, From March 2009 to August 2010, N = 248 Death Cases.
| Leading Cause of Death | 15 to 44 Years | 45 to 64 Years | 65+ Years | Total 15 Years and Older | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
||||
| Title (ICD10 blocks) | All | All | All | All | Female | P Value | Percentage | MR (‰) |
| Communicable diseases | 15 | 12 | 31 | 58 | 31 | .69 | 23 | 2.22 |
| Certain infectious and parasitic diseases | 13 | 5 | 13 | 31 | 20 | .11 | 13 | 1.19 |
| Intestinal infectious diseases (A00-A09) | 1 | 0 | 2 | 3 | 3 | |||
| Tuberculosis (A15-A19) | 3 | 1 | 6 | 10 | 8 | |||
| Tetanus (A35) | 0 | 0 | 0 | 0 | 0 | |||
| Septicemia, unspecified (A41) | 1 | 1 | 1 | 3 | 2 | |||
| Neurosyphillis (A52) | 0 | 0 | 1 | 1 | 0 | |||
| Viral infections of the central nervous system (A80-A89) | 2 | 0 | 0 | 2 | 0 | |||
| Herpes infection (B00) | 1 | 0 | 0 | 1 | 0 | |||
| Viral hepatitis (B15-B19) | 2 | 0 | 0 | 2 | 0 | |||
| HIV disease (B20-B24) | 3 | 3 | 0 | 6 | 4 | |||
| Others/unspecified inf. diseases (B34, B99, B82) | 0 | 0 | 3 | 3 | 2 | |||
| Diseases of the respiratory system | 2 | 7 | 18 | 27 | 11 | .34 | 11 | 1.03 |
| Acute lower respiratory diseases (J09-J22) | 1 | 6 | 13 | 20 | 9 | |||
| Chronic lower respiratory diseases (J40-J47) | 1 | 1 | 4 | 6 | 0 | |||
| Diseases of pleura (J90-J94) | 0 | 0 | 1 | 1 | 0 | |||
| Pregnancy, childbirth, and the puerperium | 1 | 0 | 0 | 1 | 1 | — | 0 | 0.04 |
| Complication of the puerperium (O90) | 1 | 0 | 0 | 1 | ||||
| Noncommunicable diseases | 20 | 45 | 65 | 130 | 70 | .38 | 52 | 4.97 |
| Diseases of the circulatory system | 5 | 16 | 33 | 54 | 31 | .27 | 22 | 2.07 |
| Cerebrovascular diseases (160-169) | 2 | 5 | 19 | 26 | 17 | |||
| Hypertensive diseases (110-115) | 0 | 4 | 6 | 10 | 6 | |||
| Ischaemic and pulmonary heart diseases (120-128) | 3 | 3 | 4 | 10 | 4 | |||
| Other forms of heart diseases (130-152) | 0 | 4 | 2 | 6 | 4 | |||
| Others diseases of the circulatory system (171, 199) | 0 | 0 | 2 | 2 | 0 | |||
| Malignant neoplasms | 3 | 19 | 18 | 40 | 18 | .53 | 16 | 1.53 |
| Of breast or female genital organs (C50-C58) | 0 | 8 | 0 | 8 | 8 | |||
| Of digestive organs (C15-C26) | 1 | 5 | 5 | 11 | 6 | |||
| Of respiratory system (C30-C39) | 0 | 1 | 2 | 3 | 1 | |||
| Others or unspecified | 2 | 5 | 11 | 18 | 3 | |||
| Diseases of the digestive system | 7 | 6 | 13 | 26 | 15 | .43 | 10 | 0.99 |
| Diseases of liver (K70-K77) | 5 | 5 | 5 | 15 | 7 | |||
| Diseases of intestines (K55-K63) | 0 | 0 | 7 | 7 | 6 | |||
| Others (K65,K90, K92) | 2 | 1 | 1 | 4 | 2 | |||
| Diseases of the blood (D50-D89) | 0 | 1 | 0 | 1 | 1 | — | 0 | 0.04 |
| Diseases of the nervous system (G00-G99) | 3 | 2 | 0 | 5 | 2 | — | 2 | 0.19 |
| Renal failure (N17-N19) | 2 | 1 | 1 | 4 | 3 | — | 2 | 0.15 |
| External causes of mortality | 25 | 2 | 3 | 30 | 7 | <.001 | 12 | 1.15 |
| Transport accident (V01-V99) | 18 | 2 | 0 | 20 | 4 | <.001 | 8 | 0.77 |
| Accidental drowning (W70) | 1 | 0 | 1 | 2 | 3 | |||
| Falls (W00-W19) | 2 | 0 | 2 | 4 | 0 | |||
| Intentional self-harm (X60-X84) | 2 | 0 | 0 | 2 | 0 | |||
| Assault (X85-Y09) | 1 | 0 | 0 | 1 | 0 | |||
| Complications of surgical care (Y40) | 1 | 0 | 0 | 1 | 0 | |||
| Unknown or unspecified | 2 | 5 | 22 | 29 | 17 | .35 | 12 | 1.11 |
| Senility (R54) | 0 | 1 | 10 | 11 | 10 | |||
| Other general symptoms (T51,M80,R10,F32 ) | 0 | 1 | 3 | 4 | 0 | |||
| No leading cause identified | 0 | 2 | 5 | 7 | 4 | |||
| No verbal autopsy | 2 | 1 | 4 | 7 | 3 | |||
| Total | 63 | 64 | 121 | 248 | 55 | 100 | 9.49 | |
MR: mortality rate per 1000 person-years of same age. Proportion: n of deaths by cause divided by total number of deaths among persons aged ≥15 years. P value: tests female vs male rates.
Among all ages, respiratory infections caused 34 (12%) of the 271 documented deaths (respiratory infections—MR of 0.81/1000 p-y), with no noticeable increase during the influenza season.
Among the 236 cases investigated by VA, 34 (14.4%) died in hospital, although 153 of them (65.1%) sought medical care during their final illness. Multivariate analysis of these 236 cases (Table 4) showed that dying at hospital was more frequent for children younger than 5 years (OR: 10.4 [2.8–37.9]), when the final illness lasted less than 1 week (OR: 2.8 [1.2–6.7]) and when the family was wealthy enough to own a motorbike (OR: 3.6 [1.4–9.3]).
Table 4.
Univariate and Multivariate Analysis of Factors Associated With a Death at Home Versus a Death in at Hospital, in 25 Villages of Kampong Cham Province, Cambodia, From March 2009 to August 2010, N = 236 Verbal Autopsies.
| Death at Hospital, n = 34 | Death at Home, n = 202 | Univariate | Multivariate | |||
|---|---|---|---|---|---|---|
|
|
|
|
|
|||
| Factors | n (%) | n (%) | Odds Ratio (95% CI) | P Value | Odds Ratio (95% CI) | P Value |
| Age of deceased younger than 5 years | 13 (38.2) | 10 (4.9) | 11.8 (4.2–33.1) | <.001 | 10.36 (2.8–37.9) | <.001 |
| Gender of deceased: male | 19 (55.9) | 90 (44.6) | 1.6 (0.7–3.3) | .22 | NK | |
| Head of family attended school in childhood | 25 (73.5) | 123 (60.9) | 1.8 (0.8–4.0) | .15 | NS | |
| Occupation of the deceased | ||||||
| Farmer | 15 (44.1) | 111 (54.9) | 0.64 (0.3–1.3) | .24 | NK | |
| Seller | 7 (20.6) | 39 (19.3) | 1.1 (0.4–2.6) | .86 | NK | |
| Factory worker | 1 (2.9) | 2 (0.9) | 3.0 (0.3–34.7) | .34 | NK | |
| Other (students) | 11 (32.3) | 50 (24.8) | 1.4 (0.6–3.2) | .35 | NK | |
| Cause of death by verbal autopsy | ||||||
| Communicable disease | 17 (50.0) | 55 (27.2) | 2.7 (1.3–5.7) | .008 | NS | |
| Noncommunicable disease | 13 (38.2) | 120 (59.4) | 0.4 (0.2–0.9) | .021 | NS | |
| External cause | 0 (0) | 2 (0.9) | — | NK | ||
| Perinatal conditions | 4 (11.8) | 2 (0.9) | 13.3 (2.2–80.4) | <.001 | NS | |
| Unknown, unspecified | 0 (0) | 23 (11.4) | — | NK | ||
| Final illness duration <1 week | 19 (55.9) | 58 (28.7) | 3.1 (1.5–6.7) | .002 | 2.8 (1.2–6.7) | .019 |
| Wealth of the deceased’s family | ||||||
| Owns a TV | 26 (76.5) | 144 (72.0) | 1.3 (0.5–2.9) | .589 | NK | |
| Owns a mobile phone | 21 (61.8) | 113 (56.5) | 1.2 (0.6–2.6) | .567 | NK | |
| Owns a motorbike | 20 (58.8) | 87 (43.1) | 1.8 (0.9–4.1) | .088 | 3.6 (1.4–9.3) | .009 |
| Owns a car | 3 (8.8) | 4 (1.9) | 4.7 (1.0–22.8) | .029 | NK |
95% CI: 95% confidence interval. NK: not kept in the multivariate logistic regression model.
Discussion
Our study provides some insights on mortality in rural Cambodia, suggesting that this population is facing a substantial burden of NCDs while still struggling with infectious diseases.
Our estimate of overall crude MR is comparable to 2004 estimates from the Ministry of Health.10 Our observed crude birth rate was also comparable to 2008 national crude birth rate estimates for rural areas. In our study, death rates in children were low, which is not discordant with the continuous and remarkable decline in child mortality reported by successive DHS since 2000. However, we believe that our death reports were exhaustive in this population since we closely monitored death reports through civil and religious institutions. Stillbirths and fetal deaths may have been underreported.
Our low MRs may be due to several factors, including improved conditions prevailing in this area: health centers have clinical staff available on call at night; several health programs on maternal and child health, detection and prevention of infectious diseases or focusing on improving living conditions of the poorest are implemented by national/international organizations; people have reasonably easy access to the provincial referral hospital; financial schemes facilitate access to medical care for the poor;11 in most (19/25) villages, micro-finance institutions and nongovernmental organizations have made micro-loans available for groups and individuals with a positive impact on income and food security security.12 All these conditions and interventions have a positive impact on population health.
Among children younger than 5 years, CD (including acute lower respiratory infections, infection of the gastro-intestinal system and arboviral fevers) were the leading cause of death. Perinatal conditions were the second most frequent cause, followed by accidents (mainly drowning). In 2005, the Cambodian DHS listed the same leading causes of mortality in children, adding malnutrition and measles which were not observed in our study. Many factors can explain the high prevalence of waterborne and vector-borne diseases in rural Cambodia. Sanitation is improving but remains poor: the proportion of rural Cambodian households with access to improved water sources (pipes, protected wells and tanks) increased from 17% to 40% between 1998 and 2008 while only 23% of rural households have toilets.3 Open water tanks, artificial ponds, and rice paddies surrounding houses provide large vector-breeding sites. Humans also live close to animals in rural Cambodia resulting in potential exposure to zoonotic diseases.
Among adults, NCD caused half the deaths. A national survey conducted after our study showed that almost 10% of the rural population present 3 or more risk factors for NCD.13 Among those risk factors are a high intake of salt and cheap saturated cooking oil and decreasing physical activity due to increasingly motorized transportation, and finally, Cambodians have become a target for tobacco, alcohol, and sweetened beverage companies.14
Infectious diseases were the second most frequently attributed cause of death in those 15 or older, which is typical of countries in epidemiological transition.15 Nationwide, the prevalence of some potentially severe CDs has been decreasing. It is estimated that the HIV/AIDS prevalence in the general population declined from 2% during the peak of the epidemic in 1998 to 0.5% in 2009.16 The tuberculosis burden is still heavy in Cambodia, with an incidence at 442/100 000 in 2009.17 However, the number of prevalent cases decreased by 29% between 1990 and 2008, with a measurable impact on mortality.18
Respiratory infectious diseases remained a major cause of death in adults, causing 15% of the elderly (65 y. and more) deaths and 11% of deaths in the 45 to 64 age group.
Finally, we show that accident-related deaths were frequent among young men.19 Cambodia has seen great improvements in road infrastructure and the number of motor vehicles has increased significantly. However, traffic regulations are not effectively implemented and road safety practices are not widely followed.20
Our findings have some limitations. First, as the population in the study area enjoys comparatively good living conditions for rural areas, the conclusions should be extrapolated to the rest of the country’s population with caution. Cambodia is considered to be the Asian country with the highest rate of health inequalities21 and substantial health systems variations within the country (ie, health staffing, access to health facilities, etc).
Second, our study methods did not allow us to estimate the infant- and children younger than 5 years- MRs as defined in the national DHS, preventing comparisons. We estimated the incidence of infant and younger than 5 years deaths during the study period while the DHS MRs measure the probability of dying between birth and the first birthday (infant- MR) or the fifth birthday (younger than 5 years MR) Our limited sample size did not allow us to estimate the maternal mortality ratio (206 deaths per 100 000 live births, with a 95% CI at 124–288, according to the 2010 DHS).5 Rare, fatal events and diseases can be reliably documented only through large-scale or prolonged cohort studies. Our limited sample size was not expected to capture any pandemic- or seasonal influenza-related deaths, as recent studies estimated the upper bound of influenza-related mortality rates in the tropics at ~4/100 000 in those under 5 years old22 and 3/100 000 in adults.23 Also, our study being conducted over an 18-month period, we may have overestimated MRs related to CD with annual incidence peaks between March and August (period covered twice during the study).
Third, we used the age profile of the survey population as denominator data to estimate the age-specific MR. This derives from the study census and differs slightly from the 2008 national data, showing an under-representation of young male adults (20–24 years) probably absent to work in the capital. This may have led to an overestimation of the male adult mortality rate, as people come back to die at home even if they do not permanently reside with their family.
VA tools had been developed and successfully implemented elsewhere, and are recommended in the absence of vital event registration systems.1 We chose the standard and commonly used “physician-certified VA” method (PCVA) to interpret VA data.24 This method is considered as costly, time consuming and physician diagnostic performance dependant.24 However, it was the best option for this study since 2 experienced French physicians working in Cambodian hospitals for several months volunteered to review the cases. Besides PCVA, computer coding systems are being developed, aiming to provide consistently accurate VA interpretations, at low-cost, in a timely manner, and facilitating comparisons between studies. The most commonly discussed are the InterVA,25 the Tariff,26 the Simplified Symptom Pattern,27 the King-Lu method28 and the Flaxman et al’s Random Forest method.29 The latest seemed promising in terms of validity, reliability and timeliness in 2011, but still has to be proven the best-performing method.30 In further studies, we would recommend the use of such a computer coding method.
As mortality trends continue to change, reliable and timely health statistics are an essential tool to be used in the development of strategies and policies to promote and protect health. We showed that in-hospital deaths are not representative of the total population. We believe Cambodia should extend its civil registration system to also document deaths and their medically certified cause, rather than relying on estimates from national surveys or on surveillance of in-hospital deaths. Vital statistics data are irreplaceable tools for health system activities planning and measuring progress and are one of the few ways to ensure that interventions reflect current health needs.
Conclusion
Our findings corroborate the WHO and the Cambodian Ministry of Health observations for Cambodia in 2010; we found that trends in mortality have begun to show a shift toward a greater burden of NCDs, while infectious diseases still account for a significant portion of deaths in our study area. Interventions, then, should focus on tackling the newly documented NCD burden while reinforcing prevention and cure of acute respiratory infections in children and in the elderly and sustaining infectious diseases surveillance programs. Premature mortality would also be avoided by preventing accidental deaths.
Acknowledgments
We acknowledge the villagers for their participation to this study, Ms Savy Sean who supervised the field work. We also acknowledge Dr Fabienne Plouvier for the case reviews and Dr Arnaud Tarantola for the proofreading.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The present study was funded by the US Centers for Disease Control and Prevention (grant 1U01IP000148-01). The study benefited from the surveillance site that was funded by the Pediatric Dengue Vaccine Initiative, Seoul, Republic of Korea, which received funding from the Bill & Melinda Gates Foundation (grant 23197).
Footnotes
Authors’ Note
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. Br Med Bull. 2009;92:7–32. [DOI] [PubMed] [Google Scholar]
- 2.Summerskill W, Horton R. Health in southeast Asia. Lancet. 2011;377(9763):355–356. [DOI] [PubMed] [Google Scholar]
- 3.ECLAC.Cambodia General Population Census. 2008. Available at: http://celade.cepal.org/khmnis/census/khm2008/. Accessed February 10, 2012.
- 4.Oum S, Chandramohan D, Cairncross S. Community-based surveillance: a pilot study from rural Cambodia. Trop Med Int Health. 2005;10(7):689–697. [DOI] [PubMed] [Google Scholar]
- 5.Cambodian Demographic and Health Survey.2010. Available at: http://measuresdhs.com. Accessed August 8, 2012.
- 6.Cambodia Demographic and Health Survey. 2005. Available at: http://www.measuredhs.com. Accessed August 8, 2012.
- 7.World Health Organization. Estimated causes of death among children aged <5 years, 2008. Geneva, Switzerland: World Health Organization, 2010. [Google Scholar]
- 8.Vong S, Khieu V, Glass O, et al. Dengue incidence in urban and rural Cambodia: results from population-based active fever surveillance, 2006–2008. PLOS Negl Trop Dis. 2010;4(11):e903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Verbal Autopsy Standards, Ascertaining and Attributing Cause of Death. Available at: http://whqlibdoc.who.int/publications/2007/9789241547215_eng.pdf. Accessed February 10, 2012.
- 10.Ministry of Planning, Department of Demographic Statistics, Censuses and Survey. Cambodia Inter-Censal Population Survey. 2004. General Report, 2004
- 11.Ir P, Horemans D, Souk N, Van Damme W. Using targeted vouchers and health equity funds to improve access to skilled birth attendants for poor women: a case study in three rural health districts in Cambodia. BMC Pregnancy Childbirth. 2010;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandararot K, Dannet L. Impact of micro finance services in Cambodia. Available at: http://cma-network.org/drupal/CMAPublications. Accessed August 31, 2013. [Google Scholar]
- 13.Oum S, Prak P. Non-communicable diseases prevalence and risk factors in Cambodia. STEPS survey. Available at: http://www.univ-sante.edu.kh/mekong_sante_2011/download/ncd/2-001.pdf. Accessed February 10, 2012. [Google Scholar]
- 14.Dans A, Ng N, Varghese C, Tai ES, Firestone R, Bonita R. The rise of chronic non-communicable diseases in southeast Asia: time for action. Lancet. 2011;377(9766):680–689. [DOI] [PubMed] [Google Scholar]
- 15.Lau RS, Johnson S, Kamalanabhan TJ. Healthy life expectancy in the context of population health and ageing in India. Asia Pac J Public Health. 2012;24(1):195–207. [DOI] [PubMed] [Google Scholar]
- 16.USAID. Global Aids—Cambodia Profile. Available at: http://www.usaid.gov/our_work/global_health/aids/Countries/asia/cambodia_profile.pdf. Accessed February 10, 2012.
- 17.World Health Organization. Cambodia: Tuberculosis Profile. Available at: https://extranet.who.int/sree/Reports?op=Replet&name=%2FWHO_HQ_Reports%2FG2%2FPROD%2FEXT%2FTBCountryProfile&ISO2=KH&outtype=html. Accessed February 10, 2012.
- 18.Tuberculosis Morbidity—Cambodia Health. Available at: http://www.indexmundi.com/cambodia/tuberculosis-morbidity.html. Accessed February 10, 2012.
- 19.Tong SF, Low WY. Public health strategies to address Asian men’s health needs. Asia Pac J Public Health. 2012;24(4):543–555. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. Road Safety in Cambodia. Available at: http://www.who.int/violence_injury_prevention/road_traffic/countrywork/khm/en/index.html. Accessed August. 26, 2013.
- 21.Chongsuvivatwong V, Phua KH, Yap MT, et al. Health and health-care systems in southeast Asia: diversity and transitions. Lancet. 2011;377(9763):429–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nair H, Brooks WA, Katz M, et al. Global burden of respiratory infections due to seasonal influenza in young children: a systematic review and meta-analysis. Lancet. 2011;378(9807):1917–1930. [DOI] [PubMed] [Google Scholar]
- 23.Wu JT, Ma ES, Lee CK, et al. The infection attack rate and severity of. 2009 pandemic H1N1 influenza in Hong Kong. Clin Infect Dis. 2010;51(10):1184–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lozano R, Lopez AD, Atkinson C, Naghavi M, Flaxman AD, Murray CJ. Performance of physician-certified verbal autopsies: multisite validation study using clinical diagnostic gold standards. Popul Health Metr. 2011;9:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lozano R, Freeman MK, James SL, et al. Performance of InterVA for assigning causes of death to verbal autopsies: multisite validation study using clinical diagnostic gold standards. Popul Health Metr. 2011;9:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.James SL, Flaxman AD, Murray CJ. Performance of the Tariff Method: validation of a simple additive algorithm for analysis of verbal autopsies. Popul Health Metr. 2011;9:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray CJ, James SL, Birnbaum JK, Freeman MK, Lozano R, Lopez AD. Simplified Symptom Pattern Method for verbal autopsy analysis: multisite validation study using clinical diagnostic gold standards. Popul Health Metr. 2011;9:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.King G, Lu Y, Shibuya K. Designing verbal autopsy studies. Popul Health Metr. 2010;8:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flaxman AD, Vahdatpour A, Green S, James SL, Murray CJ. Random forests for verbal autopsy analysis: multisite validation study using clinical diagnostic gold standards. Popul Health Metr. 2011;9:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chandramohan D. Validation and validity of verbal autopsy procedures. Popul Health Metr. 2011;9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]