Dear Editor
The escalating impact of alphaviruses, particularly Ross River Virus (RRV), represents a growing public health challenge, especially in Australia and the broader Southern Pacific region. Initially identified in the 1950s in Ross River, Townsville, Queensland, RRV has not only remained the predominant mosquito-borne disease in Australia but has also extended its reach to Papua New Guinea and even as far as Indonesia, Fiji, Samoa, the Moluccas, Vietnam and New Caledonia during a major outbreak in the 1980s [1]. The urgency to intensify efforts against RRV is driven by heightened risks from climate change, urbanization, and global travel, which continue to increase transmission risks beyond the peak season.
In the first half of 2024, Australia's National Notifiable Disease Surveillance System (NNDSS) recorded a significant increase in RRV cases, with totals surging to 2942—a 73 % rise from 1705 cases in the previous year. Queensland reported most cases with 2,278, followed by a slight increase in New South Wales from 355 to 372 cases. In contrast, Western Australia and Victoria saw substantial decreases, with cases dropping to 157 from 317 and to 63 from 173, respectively. Tasmania experienced the largest proportional increase, rising from 3 to 8 cases, while South Australia's cases dramatically decreased from 95 to 16. The data also shows an increase in other vector-borne diseases like dengue fever and malaria, emphasizing the need for improved public health measures and surveillance. This data highlights the persistent spread of such viruses, exacerbated by climate change, urban expansion, and global mobility [2]. Table 1 provides an overview of Notifications of RRV cases by jurisdiction in Australia for 2023-24 (as of June 24) [Insert Table 1]
Table 1.
Notifications of Ross River Virus Cases by Jurisdiction in Australia for 2023-24 (as of June 24). Data sourced from the National Notifiable Disease Surveillance System (NNDSS) Dashboard, Australia Government.
| States and territories | RRV Cases in 2024 | RRV Cases in 2023 |
|---|---|---|
| Queensland (QLD) | 2278 | 695 |
| New South Wales (NSW) | 372 | 355 |
| Western Australia (WA) | 157 | 317 |
| Victoria (VIC) | 63 | 173 |
| Northern Territory (NT) | 47 | 66 |
| South Australia (SA) | 16 | 95 |
| Tasmania (TAS) | 8 | 3 |
| Australian Capital Territory (ACT) | 1 | 2 |
| Total | 2942 | 1705 |
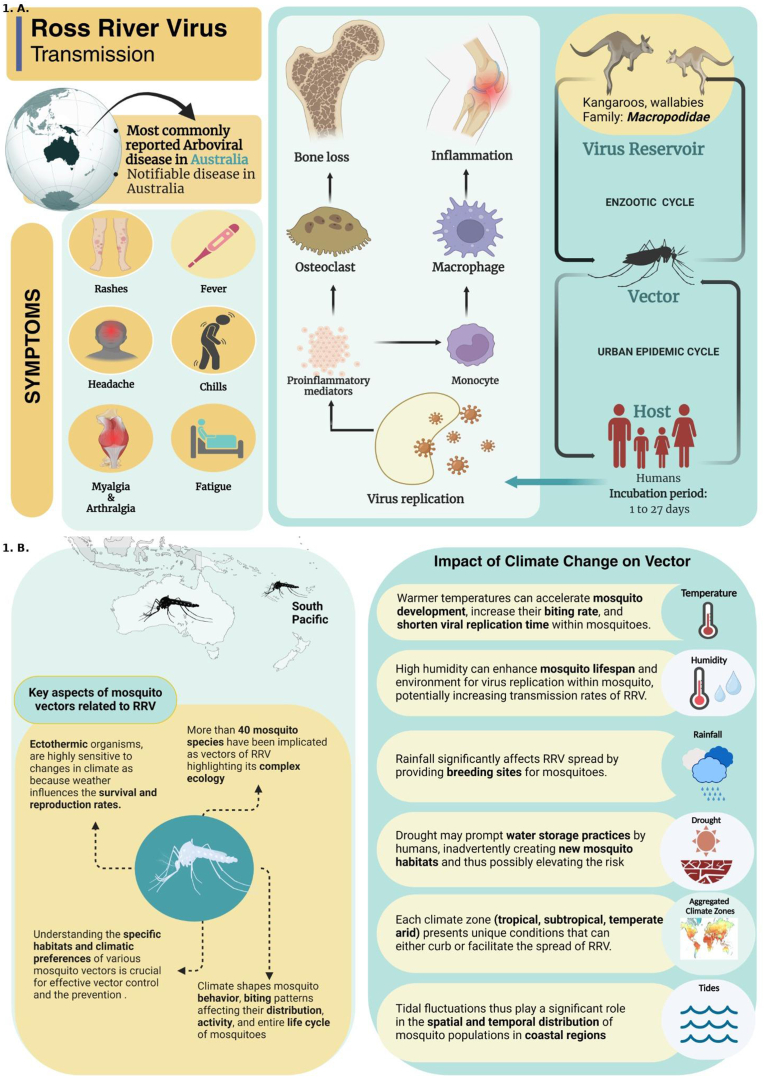
The transmission of RRV occurs through the bites of over 40 mosquito species, such as Culex annulirostris, Aedes vigilax, and A. notoscriptus, with marsupials, particularly kangaroos and wallabies, acting as reservoir hosts, sustaining the virus within natural ecosystems. Originally known as epidemic polyarthritis, RRV leads to severe joint inflammation, markedly reducing the quality of life in affected individuals. RRV infection typically results in symptoms like polyarthritis, rash, fever, and fatigue. While most individuals recover, some may experience prolonged symptoms affecting their quality of life [1]. [Insert Fig. 1].
Fig. 1.A.
illustrates the transmission cycle of the Ross River virus, highlighting the interactions between the mosquito vector and host, clinical symptoms in affected individuals, and the virus's lifecycle. Fig. 1B depicts the influence of climate on mosquito ecology, demonstrating how environmental factors, such as temperature and rainfall, affect mosquito breeding and virus transmission dynamics.
Climate change significantly impacts RRV transmission by influencing mosquito vector behaviors and expanding their geographical range. Warmer temperatures accelerate mosquito life cycles and viral replication, increasing numbers and transmission speed. Rainfall fluctuations, from floods to droughts, alter water accumulation crucial for mosquito breeding [3]. This can create new breeding sites or encourage water storage practices that inadvertently provide ideal breeding conditions. Extended breeding seasons and warmer climates allow mosquitoes to colonize new areas, exposing populations with low immunity or awareness to RRV, increasing outbreak risks. Moreover, climate shifts affect the movements and interactions of reservoir hosts like kangaroos and wallabies with mosquitoes, altering the virus's transmission cycle. Climate variations also prompt more outdoor activities and water storage during droughts, further elevating the risk of mosquito bites and RRV transmission [4].
The One-Health approach marks a significant shift in managing diseases like RRV, highlighting the interconnectedness of human, animal, and environmental health. This strategy promotes cross-disciplinary collaboration among public health, veterinary science, environmental science, and entomology to effectively tackle the ecosystem dynamics of RRV transmission [3]. It includes comprehensive surveillance and monitoring for early RRV detection, habitat and vector control to reduce mosquito breeding, community engagement to lower risk, policy integration for climate impacts, and enhanced research for better disease management. This strategy addresses RRV challenges and supports sustainable health practices amid climate change [1,5].
There are no vaccines or specific treatments for RRV; management focuses on symptomatic relief and supportive care. Preventive strategies are crucial for controlling RRV Individuals can reduce risk using insect repellents, wearing light-colored clothing, and securing living spaces against mosquitoes. Integrated Mosquito Management (IMM) is vital [5]. At the community level, adopting climate change adaptation and a One-Health approach enhances these efforts through cross-disciplinary collaboration for mosquito management, public health initiatives, and veterinary surveillance to monitor the virus in animal hosts [3]. Local health departments play a key role in deploying mosquito control programs tailored to local ecological and climate conditions [1].
The rise in RRV cases in Australia highlights the urgent need for comprehensive prevention strategies that blend individual protective actions with community-level public health initiatives. A coordinated One Health approach, addressing human, animal, and environmental health, is essential for effective RRV management and protecting public health against mosquito-borne diseases.
CRediT authorship contribution statement
Pawan Kumar: Conceptualization, Visualization, Writing – original draft. Yashreet Kaur: Data curation, Visualization. Vasso Apostolopoulos: Supervision, Visualization, Writing – review & editing. Manu Pant: Data curation, Supervision, Writing – review & editing. Abhay M. Gaidhane: Visualization, Writing – review & editing. Quazi Syed Zahiruddin: Supervision, Writing – review & editing. Mahendra Pratap Singh: Visualization. Sanjit Sah: Conceptualization, Supervision, Visualization, Writing – original draft.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling Editor: Patricia Schlagenhauf
Contributor Information
Pawan Kumar, Email: pawankumar705c@gmail.com.
Yashreet Kaur, Email: yashreetsaini@gmail.com.
Vasso Apostolopoulos, Email: Vasso.Apostolopoulos@vu.edu.au.
Manu Pant, Email: manupant@geu.ac.in.
Abhay M. Gaidhane, Email: abhaygaidhane@gmail.com.
Quazi Syed Zahiruddin, Email: zahirquazi@gmail.com.
Mahendra Pratap Singh, Email: msingh.gces@gmail.com.
Sanjit Sah, Email: sanjitsahnepal561@gmail.com.
References
- 1.Yuen K.Y., Bielefeldt-Ohmann H. Ross River virus infection: a cross-disciplinary review with a veterinary perspective. Pathogens. 2021;10(3) doi: 10.3390/pathogens10030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NNDSS . Department Of Health and Aged Care; 2024. National communicable disease surveillance dashboard: national notifiable disease surveillance System | Australian government.https://nindss.health.gov.au/pbi-dashboard/ [updated 24-06-2024. Available from: [Google Scholar]
- 3.Mackenzie J.S., Lindsay M.D.A., Smith D.W., Imrie A. The ecology and epidemiology of Ross River and murray valley encephalitis viruses in western Australia: examples of One health in action. Trans R Soc Trop Med Hyg. 2017;111(6):248–254. doi: 10.1093/trstmh/trx045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hime N.J., Wickens M., Doggett S.L., Rahman K., Toi C., Webb C., et al. Weather extremes associated with increased Ross River virus and Barmah Forest virus notifications in NSW: learnings for public health response. Aust N Z J Public Health. 2022;46(6):842–849. doi: 10.1111/1753-6405.13283. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal K., Srivastava S., Singh V., Rohilla R., Zaman K., Rukadikar A., et al. One health concept and its applications in clinical practice: a comprehensive review. The Evidence. 2023;2(1) [Google Scholar]