Abstract
Background:
The diagnosis, etiology, and optimal management of fibromyalgia remains contentious. This uncertainty may result in variability in clinical management. We conducted a systematic review and meta-analysis of cross-sectional studies examining physicians’ knowledge, attitudes, and practices regarding fibromyalgia.
Methods:
We searched MEDLINE, Embase, and PubMed from inception to February 2023 for cross-sectional surveys evaluating physicians’ attitudes toward, and management of, fibromyalgia. Pairs of independent reviewers conducted article screening, data extraction, and risk of bias assessment in duplicate. We used random-effects meta-analysis to pool proportions for items reported by more than one study and the Grading of Recommendations Assessment, Development, and Evaluation approach to summarize the certainty of evidence.
Results:
Of 864 citations, 21 studies (8904 participants) were eligible for review. Most physicians endorsed fibromyalgia as a distinct clinical entity (84%; 95% confidence interval [CI], 74–92), and half (51%; 95% CI, 40–62) considered fibromyalgia a psychosocial condition. Knowledge of formal diagnostic criteria for fibromyalgia was more likely among rheumatologists (69%, 95% CI, 45–89) versus general practitioners (38%, 95% CI, 24–54) (P = .04). Symptom relief was endorsed as the primary management goal by most physicians (73%, 95% CI, 52–90). Exercise, physiotherapy, antidepressants, nonsteroidal anti-inflammatory drugs, and non-opioid analgesics were most endorsed for management of fibromyalgia, but with wide variability between surveys. Opioids and most complementary and alternative interventions (e.g., homeopathy, chiropractic, and massage) received limited endorsement.
Conclusion:
There is moderate certainty evidence to suggest that physicians are divided regarding whether fibromyalgia is a biomedical or psychosocial disorder. Physicians typically prioritize symptom relief as the primary goal of management, and often endorse management with exercise, non-opioid analgesics, nonsteroidal anti-inflammatory drugs, antidepressants, and physiotherapy (moderate to high certainty evidence); however, important practice variation exists.
Keywords: attitudes, fibromyalgia, general practitioners, management, practice variation, rheumatologists
1. Introduction
Fibromyalgia is a syndrome without pathognomonic findings characterized by widespread and persistent pain, often accompanied by sleep disturbance, fatigue, and co-morbid mood disorders.[1] The 1990 American College of Rheumatology (ACR) fibromyalgia classification criteria identified a prevalence of 1.7% (95% confidence interval [CI], 0.7–2.8) among the general public,[2] which is similar to a 1.8% (95% CI, 1.7–1.9) prevalence rate for fibromyalgia in the general population reported in a 2017 systematic review.[3]
The modified 2010 ACR criteria were based on use of the Widespread Pain Index and the Symptom Severity Scale and increased the prevalence of fibromyalgia among the public more than 3-fold to 5.4% (95% CI, 4.7–6.1).[2] The ACR criteria for diagnosing fibromyalgia were further revised in 2016, and now require widespread, persistent pain (≥3 months), and scores of ≥7 on the Widespread Pain Index and ≥5 on the Symptom Severity Scale (or a score of 4–6 on the Widespread Pain Index and a score of ≥9 on the Symptom Severity Scale).[4] A survey of 3276 primary care patients attending 25 practices in Kansas, United States, classified 5.5% (95% CI, 4.8–6.3) of patients as meeting 2016 ACR criteria for fibromyalgia.[5]
Fibromyalgia is associated with reduced quality of life and unemployment, and considerable socioeconomic burden.[6] Despite extensive investigation, the diagnosis, underlying pathophysiology, and optimal management of fibromyalgia remains contentious.[1] Moreover, patients often report limited improvement in pain and function, even in specialized clinics.[7–9] Prior qualitative and mixed-methods studies indicate that inadequate pain management and provider stigma are common sources of frustration for patients with fibromyalgia,[10,11] while physicians often report insufficient knowledge or skill in diagnosing and caring for these patients.[10,12] To date, no systematic review or meta-analysis has examined the level of knowledge of the medical community about the quality of the care process, or attitudes towards the patient with fibromyalgia and the perception of its basic etiological aspects. We conducted a systematic review and meta-analysis of cross-sectional studies exploring physicians’ knowledge, attitudes, and practices regarding fibromyalgia.
2. Methods
We completed our systematic review in accordance with the Meta-analysis Of Observational Studies in Epidemiology and Preferred Reporting Items for Systematic Reviews and Meta-Analyses statements.[13,14] We did not prepare a protocol or register our review.
2.1. Data sources and searches
We searched Ovid MEDLINE, Ovid Embase, and PubMed from inception to February 1, 2023, using search strategies developed with the help of an experienced academic librarian (R.J.C.). (Appendix 1, Supplemental Digital Content, http://links.lww.com/MD/N278). We employed a combination of subject headings (MeSH in MEDLINE and Emtree in Embase) and keyword searches. We screened the reference lists of all eligible studies for additional citations. We included English-language cross-sectional surveys that explored physicians’ attitudes toward fibromyalgia and its management. We excluded conference abstracts, other gray literature (e.g., dissertations), and studies with mixed physician and nonphysician respondents where the physician sample could not be enumerated.
2.2. Study selection
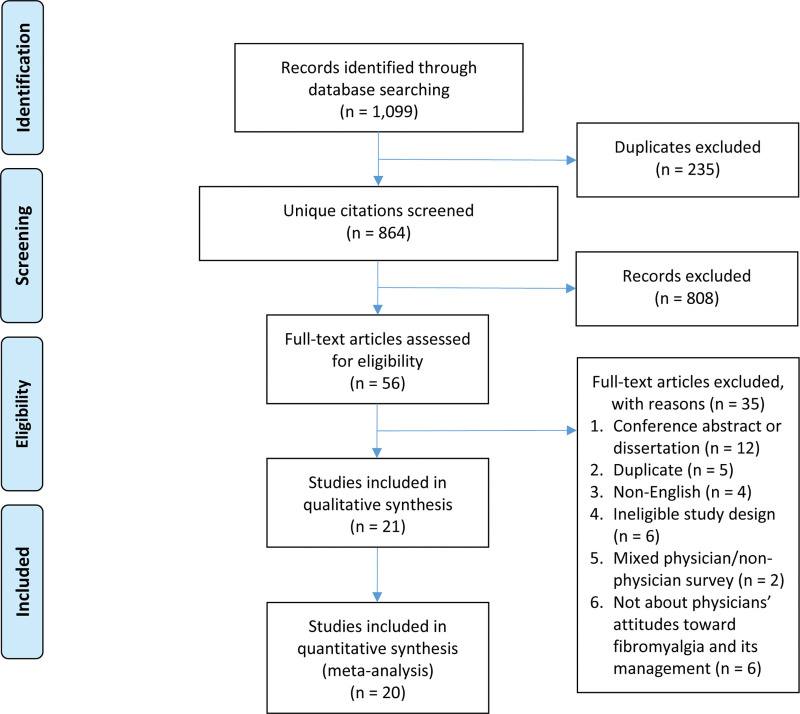
Pairs of reviewers (P.C.E., L.G., S.H.S., and A.R.) independently screened each title and abstract retrieved from the database searches, and full texts of all potentially eligible studies. Consensus was reached on decisions to include or exclude potentially eligible studies, with discrepancies resolved by discussion or adjudication by a third reviewer (A.A.). We used online systematic review software (DistillerSR, Evidence Partners, Ottawa, Canada; https://www.distillersr.com/) to facilitate literature screening. A flowchart illustrating our literature screening and study selection process is shown in Figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
2.3. Data abstraction
Using standardized, pretested data extraction forms, pairs of reviewers (P.C.E., L.G., Y.O., and A.R.) extracted data and appraised risk of bias of included studies, independently and in duplicate. Abstracted information included study characteristics (i.e., first author, year of publication, year of survey administration, country of study, study population, number of respondents, and response rate), data on physicians’ knowledge and attitudes toward fibromyalgia, and physicians’ endorsement of management options for fibromyalgia. For surveys administered to multiple medical specialties, we extracted information separately for rheumatologists versus non-rheumatologists if possible.
2.4. Risk of bias assessment
We used the following 5 criteria from the Users’ Guides to the Medical Literature[15] to assess risk of bias: (1) sample representativeness; (2) adequacy of response rate (˂50% was considered high risk of bias); (3) missing data for individual items within completed questionnaires (≥20% was considered high risk of bias); (4) pilot testing of surveys prior to administration; and (5) whether authors provided any evidence of instrument validity/reliability. Studies were evaluated on an item-by-item basis, with reviewers rating each item as being at a low or high risk of bias[16] (Appendix 2, Supplemental Digital Content, http://links.lww.com/MD/N278).
2.5. Data synthesis
We used the kappa statistic (κ) to measure inter-rater agreement of full-text screening and interpreted the strength of agreement as: poor (κ ≤ 0.2), fair (0.21 ≤ κ ≤ 0.4), moderate (0.41 ≤ κ ≤ 0.6), substantial (0.61 ≤ κ ≤ 0.8), or almost perfect (κ > 0.8).[17] We used random-effects models to pool data on proportions for items that were reported by 2 or more studies. We used the Freeman–Tukey double arcsine transformation to stabilize the variance to ensure that estimates of precision associated with point estimates contained only admissible values (between 0% and 100%).[18,19] We used the DerSimonian and Laird method[20] to compute the pooled estimate based on the transformed values and their variances, and the harmonic mean of sample sizes for the back-transformation to the original units of proportions.[21] We used the Grading of Recommendations Assessment, Development, and Evaluation approach to summarize the certainty of evidence for all meta-analyses as high, moderate, low, or very low.[22] When there were ≥10 studies in a meta-analysis,[23] we explored for small-study effects by visual inspection of funnel plots for asymmetry and calculation of Egger test. We performed a qualitative synthesis when data could not be pooled.
2.6. Subgroup, meta-regression and sensitivity analyses
We used tau-squared (τ2) and visual assessment of forest plots to examine heterogeneity.[24] We considered heterogeneity of a pooled estimate to be problematic if point estimates varied widely across studies, CIs showed minimal to no overlap, and the τ2 was large (≥0.1 was considered high heterogeneity).[25] Sources of between-study variability were explored using the following subgroups: (1) rheumatologists versus non-rheumatologists; (2) later versus earlier years of survey administration; (3) studies conducted in more versus less developed countries, according to the United Nations classification[26]; and (4) lower versus higher risk of bias, evaluated on a criterion-by-criterion basis. We used univariable meta-regression to determine a cutoff value for year of survey administration (i.e., 2013 and later vs pre-2013). Tests for interaction were performed to establish whether subgroups differed significantly from one another, and we assessed the credibility of significant subgroup effects (test for interaction, P < .05) using modified Instrument for assessing the Credibility of Effect Modification Analyses criteria[27] (Appendix 3.1, Supplemental Digital Content, http://links.lww.com/MD/N278). We also performed a sensitivity analysis to examine the impact of logit transformation versus Freeman–Tukey double arcsine transformation on our results. All data and comparative analyses were performed using Stata V.18 (StataCorp, College Station, TX), and the 2-sided statistical significance level was 5%.
2.7. Ethical considerations
Ethics approval was not required because this was a systematic literature review of previously published studies.
3. Results
Of 864 unique citations, 21 surveys reporting on 8904 physicians met our eligibility criteria (Fig. 1).[12,28–47] Agreement between reviewers at the full-text screening stage was almost perfect (κ = 0.96).
3.1. Study characteristics
Of the 21 eligible studies, 3 (14%) were multi-national,[28,35,37] 5 (24%) were conducted in the US,[31–33,39,40] 4 (19%) in Canada,[12,34,43,44] 2 (10%) in Israel,[28,36] and individual surveys administered in France,[29] China,[38] Iran,[41] Peru,[42] Spain,[45] Pakistan,[46] and Turkey.[47] Among 14 studies which reported the year of survey administration, all were administered from the year 2003 onwards.[12,29,31–33,35,37–44,47] Eight (38%) studies involved a broad physician population with explicit inclusion of rheumatologists as part of the sample,[12,29,32,35,37,40,44,47] 4 (19%) studies involved rheumatologists only,[30,34,38,43] 5 (24%) included physicians-in-training,[28,31,36,39,46] 3 (14%) involved general practitioners (GPs),[41,42,45] and 1 (5%) a mixed population of GPs and internists[32] (Table 1).
Table 1.
Characteristics of included studies.
| First author, year of publication | Year of survey administration | Study location(s) | Study population | Number of respondents | Response rate (%) |
|---|---|---|---|---|---|
| Buskila,[28] 1997 | NR | Israel | GPs, family medicine residents | 172 | 100% |
| Blotman,[29] 2005 | 2003 | France | GPs, rheumatologists | 1560 | 12% |
| Arshad,[30] 2007 | NR | Malaysia, Singapore, Thailand, Brunei, Indonesia | Rheumatologists | 118* | 91% |
| Lu,[31] 2007 | NR | United States | Medical students | 43 | NR |
| Hayes,[12] 2010 | 2007 | Canada | GPs, specialists (including rheumatologists)† | 328 | NR |
| Silverman,[32] 2010 | 2008 | United States | GPs, specialists (including rheumatologists)† | 102 | NR |
| Hadker,[33] 2011 | 2009 | United States | Internists, GPs | 94 | 3% |
| Ghazan-Shahi,[34] 2012 | NR | Canada | Rheumatologists | 80 | 53% |
| Perrot,[35] 2012 | 2008 | Europe, South Korea, Mexico | GPs, specialists (including rheumatologists)‡ | 1622 | NR |
| Bloom,[36] 2013 | NR | Israel | Orthopedic surgeons (including residents) | 219 | 100% |
| Clark,[37] 2013 | 2008–2010 | Latin America, Europe | Internists, GPs, other specialists (including rheumatologists)‡ | 1824 | NR |
| Mu,[38] 2013 | 2010 | China | Rheumatologists | 707 | 60% |
| Amber,[39] 2014 | 2011 | United States | Internists, GPs, medical students | 283 | 44% |
| Able,[40] 2016 | 2008–2010 | United States, Puerto Rico | GPs, specialists (including rheumatologists)§ | 91 | NR |
| Kianmehr,[41] 2017 | 2013 | Iran | GPs | 190 | NR |
| Ortiz,[42] 2017 | 2016 | Peru | GPs | 145 | 84% |
| Agarwal,[43] 2018 | 2016 | Canada | Rheumatologists | 140 | 42% |
| Kumbhare,[44] 2018 | 2015–2016 | Canada | GPs, specialists (including rheumatologists)ǁ | 284 | 50% |
| Torres,[45] 2020 | NR | Spain | GPs | 392 | 38% |
| Hyder Zaidi,[46] 2022 | NR | Pakistan | GPs (including residents) | 104 | NR |
| Ketenci,[47] 2022 | 2021 | Turkey | Specialists (including rheumatologists)ǁ | 406 | 26% |
GP = general practitioner, NR = not reported.
The number of responses received was reported as 108 by Arshad et al; however, 118 responses were received in total.
Other specialties included: anesthesiologists, neurologists, pain specialists, and psychiatrists.
Other specialties included: neurologists, psychiatrists, and pain specialists.
Other specialties included: pain medicine, psychiatrists, neurologists, an obstetrician/gynecologist, and an osteopath.
Other specialties included: physical medicine and rehabilitation, anesthesiologists, and neurologists.
3.2. Risk of bias
All studies were at high risk of bias for at least one criterion (Appendix 3.2, Supplemental Digital Content, http://links.lww.com/MD/N278). Of the 21 studies, 20 (95%) were rated as having a low risk of bias for missing data within completed questionnaires, and 17 (81%) were at low risk of bias for sample representativeness. Among 14 studies which reported the proportion of respondents, response rates ranged from 3% to 100% (median 50%) (Table 1). Six studies (29%) were at low risk of bias for adequacy of response rate, 5 studies (24%) reported pilot testing their questionnaire prior to administration, and only 1 (5%) provided support for instrument reliability and validity (Appendix 3.2, Supplemental Digital Content, http://links.lww.com/MD/N278).
3.3. Etiology and diagnosis of fibromyalgia
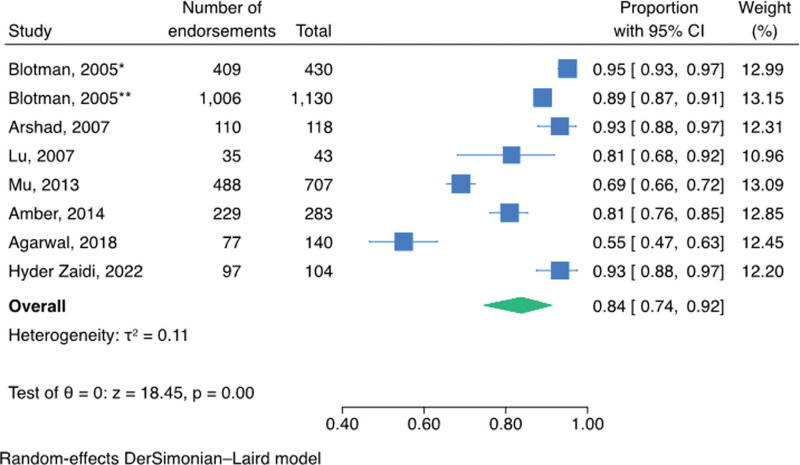
Seven surveys (2955 participants) inquired whether fibromyalgia is perceived as a distinct clinical entity, 3 involving rheumatologists only,[30,38,43] 3 involving GPs and/or physicians-in-training,[31,39,46] and one involving a mix of rheumatologists and GPs[29] (Appendix 3.3, Supplemental Digital Content, http://links.lww.com/MD/N278). The pooled proportion of respondents endorsing fibromyalgia as a distinct clinical entity was 84% (95% CI, 74–92; moderate certainty evidence) (Table 2 and Fig. 2).
Table 2.
GRADE evidence profile and summary of findings of physicians’ knowledge, attitudes, and practices regarding fibromyalgia.
|
No. of studies (participants) |
Quality assessment* | Summary of findings | |||||
|---|---|---|---|---|---|---|---|
| Risk of bias | Inconsistency | Indirectness | Imprecision | Small-study effects | Overall certainty of evidence | Proportion (95% CI) | |
| Endorsement of fibromyalgia as a distinct clinical entity: | |||||||
| 7 (2955) | No serious risk of bias† | Serious inconsistency (τ2 = 0.11) | No serious indirectness | Serious imprecision‡ | NA (only 7 studies) | Moderate | 84% (74–92) |
| Endorsement of fibromyalgia as a psychosocial illness: | |||||||
| 8 (3384) | No serious risk of bias† | Serious inconsistency (τ2 = 0.11) | No serious indirectness | Serious imprecision‡ | NA (only 8 studies) | Moderate | 51% (40–62) |
| Endorsement of comprehensive knowledge of ACR diagnostic criteria§: | |||||||
| 12 (7331) | No serious risk of bias† | Serious inconsistency (τ2 = 0.24) | No serious indirectness | Serious imprecision‡ | Undetected; symmetrical funnel plot; Egger test, P = .57 |
Moderate | 49% (36–62) |
| Utilization of ACR criteria to diagnose patients with fibromyalgia: | |||||||
| 6 (4453) | No serious risk of bias† | Serious inconsistency (τ2 = 0.15) | No serious indirectness | Serious imprecision‡ | NA (only 6 studies) | Moderate | 65% (49–79) |
| Endorsement of pain relief as the primary management goal of fibromyalgia: | |||||||
| 4 (1043) | No serious risk of bias† | Serious inconsistency (τ2 = 0.20) | No serious indirectness | Serious imprecision‡ | NA (only 4 studies) | Moderate | 73% (52–90) |
| Endorsement of non-opioid analgesics for managing fibromyalgia: | |||||||
| 5 (2139) | No serious risk of bias† | Serious inconsistency (τ2 = 0.11) | No serious indirectness | Serious imprecision‡ | NA (only 5 studies) | Moderate | 67% (54–79) |
| Endorsement of NSAIDs for managing fibromyalgia: | |||||||
| 6 (1353) | No serious risk of bias† | No serious inconsistency (τ2 = 0.07) | No serious indirectness | Serious imprecision | NA (only 6 studies) | Moderate | 49% (38–60) |
| Endorsement of corticosteroids for managing fibromyalgia: | |||||||
| 3 (1001) | No serious risk of bias† | No serious inconsistency (τ2 = 0.01) | No serious indirectness | Serious imprecision | NA (only 3 studies) | Moderate | 22% (17–28) |
| Endorsement of opioids for managing fibromyalgia: | |||||||
| 4 (1994) | No serious risk of bias† | No serious inconsistency (τ2 = 0.03) | No serious indirectness | Serious imprecision | NA (only 4 studies) | Moderate | 7% (4–12) |
| Endorsement of antidepressant medications for managing fibromyalgiaǁ: | |||||||
| 5 (1272) | No serious risk of bias† | Serious inconsistency (τ2 = 0.13) | No serious indirectness | Serious imprecision‡ | NA (only 5 studies) | Moderate | 67% (50–81) |
| Endorsement of sedative-hypnotic agents for managing fibromyalgia: | |||||||
| 2 (1654) | No serious risk of bias† | No serious inconsistency (τ2 = 0.00) | No serious indirectness | No serious imprecision | NA (only 2 studies) | High | 32% (30–35) |
| Endorsement of muscle relaxants for managing fibromyalgia: | |||||||
| 3 (300) | No serious risk of bias† | No serious inconsistency (τ2 = 0.05) | No serious indirectness | Serious imprecision | NA (only 3 studies) | Moderate | 41% (28–55) |
| Endorsement of anticonvulsant medications for managing fibromyalgiaǁ: | |||||||
| 5 (630) | No serious risk of bias† | Serious inconsistency (τ2 = 0.28) | No serious indirectness | Serious imprecision‡ | NA (only 5 studies) | Moderate | 33% (13–56) |
ACR = American College of Rheumatology, CI = confidence interval, GP = general practitioner, GRADE = Grading of Recommendations Assessment, Development, and Evaluation, NA = not applicable, NSAID = nonsteroidal anti-inflammatory drug.
We did not rate down for study design as cross-sectional surveys are an appropriate design for evaluating knowledge, attitudes, and practices.
We did not rate down for risk of bias because our subgroup analyses found no credible subgroup effects between the pooled estimate and each risk of bias component.
We did not rate down twice for both imprecision and inconsistency when both were present, as these are not independent (i.e., pooled effects that show inconsistency will often also be imprecise because of the inconsistency).
We found a significant subgroup effect between rheumatologists versus GPs/other physicians (moderate credibility; interaction, P = .04).
We found a significant subgroup effect between studies conducted in more versus less developed countries (moderate credibility; interaction, P < .001).
Figure 2.
Pooled proportion of respondents endorsing fibromyalgia as a distinct clinical entity. CI = confidence interval; *rheumatologists; **general practitioners.
Eight surveys (3384 participants) inquired whether fibromyalgia is perceived as a psychosocial illness versus a biomedical disease, 4 involving rheumatologists only,[30,34,38,43] 2 involving GPs,[45,46] 1 involving rheumatologists and GPs,[29] and 1 involving physicians (i.e., GPs, internists) and medical students[39] (Appendix 3.3, Supplemental Digital Content, http://links.lww.com/MD/N278). The proportion of respondents’ endorsing fibromyalgia as a psychosocial illness ranged from 31% to 72%, and the pooled proportion was 51% (95% CI, 40–62; moderate certainty evidence) (Table 2 and Appendix 4.1, Supplemental Digital Content, http://links.lww.com/MD/N278).
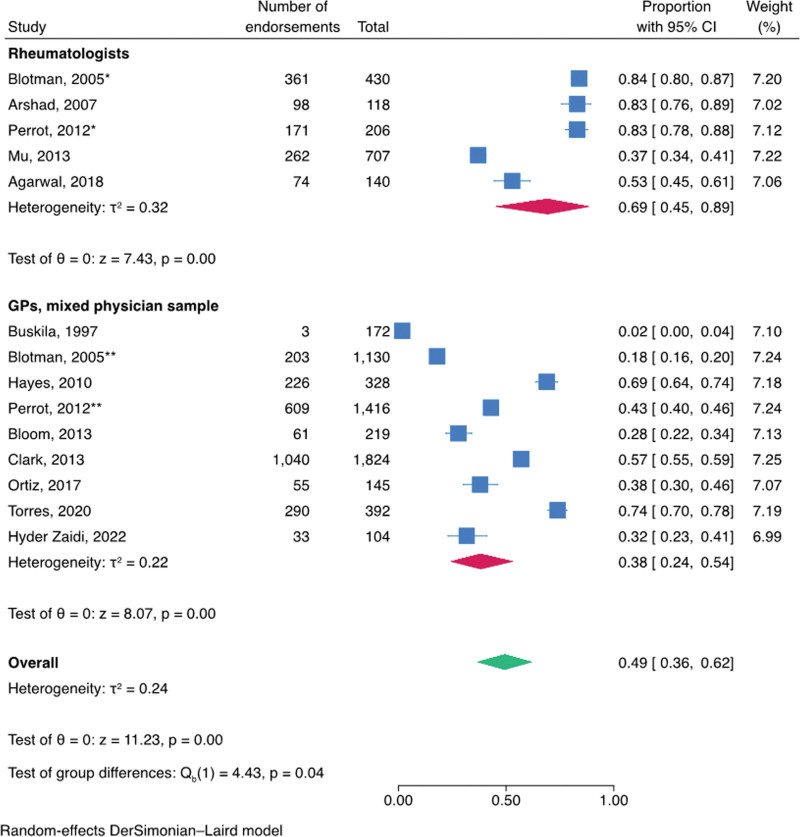
Twelve studies (7331 participants) examined knowledge and utilization of diagnostic criteria for fibromyalgia; 5 involving rheumatologists,[29,30,35,38,43] 5 involving GPs,[28,29,42,45,46] 3 involving a combination of generalists and specialists,[12,35,37] and 1 involving orthopedic surgeons[36] (Appendix 3.3, Supplemental Digital Content, http://links.lww.com/MD/N278). Across studies, there was moderate certainty evidence that 49% (95% CI, 36–62) of respondents endorsed comprehensive knowledge of the ACR diagnostic criteria (Table 2 and Appendix 4.2, Supplemental Digital Content, http://links.lww.com/MD/N278); however, this estimate was associated with high heterogeneity. We found a credible subgroup effect for physician type, with 69% (95% CI, 45–89) of rheumatologists endorsing knowledge of ACR criteria versus 38% (95% CI, 24–54) of GPs/mixed physician samples (test of interaction, P = .04; moderate credibility for subgroup effect) (Fig. 3 and Appendix 4.3, Supplemental Digital Content, http://links.lww.com/MD/N278). No small-study effects were detected (Appendix 4.4, Supplemental Digital Content, http://links.lww.com/MD/N278). Among 6[30,32,35,38,44,46] studies (4453 participants), the pooled proportion of physicians reporting use of the ACR criteria to diagnose patients with fibromyalgia in clinical practice was 65% (95% CI, 49–79; moderate certainty evidence) (Table 2 and Appendix 4.5, Supplemental Digital Content, http://links.lww.com/MD/N278).
Figure 3.
Subgroup analysis of rheumatologists’ versus GPs’/other physicians’ endorsement of comprehensive knowledge of the American College of Rheumatology diagnostic criteria (moderate credibility[27]; test of interaction, P = .04). CI = confidence interval; *rheumatologists; **general practitioners.
3.4. Treatment goal and oversight of fibromyalgia management
Four surveys (1043 participants) examined goals in the management of fibromyalgia, 2 involving rheumatologists,[38,43] and 1 each involving multiple specialties[32] and GPs[33] (Appendix 3.3, Supplemental Digital Content, http://links.lww.com/MD/N278). There was moderate certainty evidence that symptom relief was endorsed as a primary management goal by 73% (95% CI, 52–90) of respondents (Table 2 and Appendix 4.6, Supplemental Digital Content, http://links.lww.com/MD/N278).
Four studies (730 participants) evaluated perceptions regarding which type of medical provider should oversee management of fibromyalgia patients.[34,43,46,47] Ghazan-Shahi and colleagues conducted a survey of 80 rheumatologists and found that 89% endorsed that fibromyalgia should primarily be managed by GPs.[34] In 3 surveys involving a total of 626 specialists, including rheumatologists,[34,43,47] very low proportions (median 5%, range 4–6%) endorsed that rheumatologists should maintain primary ownership over fibromyalgia care (Appendix 3.3, Supplemental Digital Content, http://links.lww.com/MD/N278). Conversely, a survey of 104 physicians-in-training (63% residents and 33% house officers) found that 42% of respondents felt fibromyalgia should be managed by rheumatologists.[46]
3.5. Treatment modalities for managing fibromyalgia
Eleven studies (3720 participants) explored endorsement of pharmacological and non-pharmacological modalities for management of fibromyalgia[29,30,32–34,36,38,41,43,46,47] (Appendix 3.4, Supplemental Digital Content, http://links.lww.com/MD/N278).
3.5.1. Pharmacological
Among pharmacological agents, at least 1 class was highly endorsed across 10[29,30,32,33,36,38,41,43,46,47] of 11 studies (Appendix 3.4, Supplemental Digital Content, http://links.lww.com/MD/N278). Analgesics and/or anti-inflammatories were endorsed by most respondents across 9 studies (median 71% for analgesics in general, range 55–77%), with non-opioid analgesics (pooled estimate 67%; 95% CI, 54–79; moderate certainty evidence) (Table 2 and Appendix 4.7, Supplemental Digital Content, http://links.lww.com/MD/N278) and nonsteroidal anti-inflammatory drugs (NSAIDs) (pooled estimate 49%; 95% CI, 38–60; moderate certainty evidence) (Table 2 and Appendix 4.8, Supplemental Digital Content, http://links.lww.com/MD/N278) being most endorsed. Corticosteroids were less commonly endorsed[38,41,46] (pooled estimate 22%; 95% CI, 17–28; moderate certainty evidence) (Table 2 and Appendix 4.9, http://links.lww.com/MD/N278), and opioids were infrequently endorsed (pooled estimate 7%; 95% CI, 4–12; moderate certainty evidence)[29,41,43,46] (Table 2 and Appendix 4.10, Supplemental Digital Content, http://links.lww.com/MD/N278). Only 1 study reported on the use of medical marijuana and pharmaceutical cannabinoids for fibromyalgia management, and these modalities also received low endorsement (12% and 8%, respectively)[43] (Appendix 3.4, Supplemental Digital Content, http://links.lww.com/MD/N278).
While antidepressant medications in general received support as primary treatment modalities for fibromyalgia from the majority of respondents in 5 studies[32,36,38,43,46] (pooled estimate 67%; 95% CI, 50–81; moderate certainty evidence) (Table 2 and Appendix 4.11, Supplemental Digital Content, http://links.lww.com/MD/N278), endorsement was higher among responding physicians in more versus less developed countries (84% [95% CI, 73–93] vs 53% [95% CI, 36–69]; test of interaction, P < .001; moderate credibility for subgroup effect) (Appendices 4.12, Supplemental Digital Content, http://links.lww.com/MD/N278 and 4.13, Supplemental Digital Content, http://links.lww.com/MD/N278). Sedative-hypnotic agents were endorsed by a minority of respondents across 2 studies[29,33] (pooled estimate 32%; 95% CI, 30–35; high certainty evidence) (Table 2 and Appendix 4.14, Supplemental Digital Content, http://links.lww.com/MD/N278), as were muscle relaxants (pooled estimate 41%; 95% CI, 28–55; moderate certainty evidence) (see Table 2 and Appendix 4.15, Supplemental Digital Content, http://links.lww.com/MD/N278)[32,33,46] and anticonvulsant medications including pregabalin (pooled estimate 33%; 95% CI, 13–56; moderate certainty evidence) (see Table 2 and Appendix 4.16, Supplemental Digital Content, http://links.lww.com/MD/N278).[32,33,41,43,46] Endorsement of anticonvulsant medications was higher, however, among responding physicians from more versus less developed countries (50% [95% CI, 31–68] vs 12% [95% CI, 7–19]; test of interaction, P < .001; moderate credibility for subgroup effect) (Appendices 4.17, Supplemental Digital Content, http://links.lww.com/MD/N278 and 4.18, Supplemental Digital Content, http://links.lww.com/MD/N278).
3.5.2. Non-pharmacological
Five[29,36,38,43,46] of 6 studies (Appendix 3.4, Supplemental Digital Content, http://links.lww.com/MD/N278) that inquired about non-pharmacologic treatments (involving 2730 participants) found most respondents endorsed physical activity as a first-line management approach for fibromyalgia. Blotman and colleagues found that swimming and regular walking were endorsed by more than 2/3rds of respondents.[29] Two other studies[36,46] reported moderate endorsement (50%) of gymnastics/aerobic sports and low endorsement (22%) of aerobic exercise. Two studies reported that most respondents endorsed yoga, relaxation exercises, and/or cognitive behavioral therapy,[29,34] though 3 other studies reported only a minority of respondents endorsing yoga and/or cognitive behavioral therapy as primary treatment approaches[41,43,46] (Appendix 3.4, Supplemental Digital Content, http://links.lww.com/MD/N278).
Except for physical therapy (median endorsement 73%, range 56–93), little endorsement was reported for most practitioner-based non-pharmacological interventions.[29,36,38,41,43,46] A minority of respondents endorsed acupuncture across 2 studies (median 41%, range 25–42),[29,41] while 2 other studies reported low degrees of endorsement (median 16%, range 3–45) across other practitioner-based interventions, such as homeopathy, chiropractic, osteopathy, massage, hypnosis, and hydrotherapy/spa therapy[29,41] (Appendix 3.4, Supplemental Digital Content, http://links.lww.com/MD/N278).
3.6. Additional subgroup and sensitivity analyses
Aside from those already reported, no other subgroup analyses or meta-regression were significant (P-values ranged from 0.06–0.98). Sensitivity analyses of our findings using logit transformation versus Freeman–Tukey double arcsine transformation showed similar results (data not shown).
4. Discussion
4.1. Summary of main findings
This was the first systematic review to examine the literature on physicians’ knowledge, attitudes, and practices regarding fibromyalgia. Our findings suggest that most physicians endorse fibromyalgia as a distinct clinical entity; however, physicians were divided as to whether fibromyalgia is primarily a psychosocial or biomedical condition. Symptom relief was generally endorsed as the primary goal of management, particularly amongst rheumatologists. Most rheumatologists endorsed that oversight of fibromyalgia patient care belonged primarily to GPs. Views regarding management of fibromyalgia were highly divergent, with only non-opioid analgesics, relaxation exercises, and physical therapy consistently endorsed by most respondents.
4.2. Strengths and limitations
Our systematic review has several strengths. First, we used explicit eligibility criteria and conducted a comprehensive search to identify all eligible surveys. Second, we conducted article screening, data extraction, and risk of bias assessment in duplicate to improve reliability of subjective decisions. Further, we evaluated risk of bias of included studies using a tool specifically tailored for cross-sectional surveys,[15,16] and assessed the certainty of evidence using the Grading of Recommendations Assessment, Development, and Evaluation approach.
Our systematic review also has limitations. First, the search strategy was limited to English-language publications, which may limit the generalizability of our findings. Second, several of our pooled estimates suffered from serious inconsistency that we were often unable to explain, which impacts confidence in these findings.
4.3. Comparison with relevant literature
Consistent with Canadian 2012 fibromyalgia guidelines,[48,49] oversight of fibromyalgia management was largely perceived by rheumatologists in our review as belonging to primary care physicians. General practitioners were, however, more likely to perceive rheumatologists as having an oversight role. Our finding that many physicians feel that other specialities should be primary care providers for fibromyalgia may reflect that physicians in general find patients with fibromyalgia difficult to treat. A mixed-methods study of 189 GPs and 139 specialists (including rheumatologists) across Canada found that 76% endorsed fibromyalgia patients as time consuming and frustrating.[12]
A qualitative study of 26 Swedish physicians reported they found patients with fibromyalgia to be demanding, aggressive in collecting information on their illness, illness focused, and medicalizing.[50] The study authors opined that such perceptions are influenced by physicians’ inability to provide patients with a causal explanation of their condition, and that they find fibromyalgia difficult to treat.[50] The 2016 survey of 331 Canadian rheumatologists by Agarwal et al[43] found that 50% may refuse referrals for consultation of patients diagnosed with fibromyalgia, and a 2023 qualitative evidence synthesis[51] found that consultations for fibromyalgia were likely to result in dissatisfaction for both patients and physicians (e.g., patients with fibromyalgia often reported the need for greater moral support from physicians, whereas the latter often felt frustrated and of little help to patients[10,50,51]).
We found that respondents were divided with respect to whether fibromyalgia is primarily a psychosocial or a biomedical condition. Fibromyalgia is a condition with no currently validated biomarker,[52,53] pathognomonic imaging, or consistent examination findings, and diagnosis is subjective and dependent on patients’ reporting of symptoms.[54] This uncertainty likely contributes to the high variability in treatment that we found. One of the only interventions that was endorsed by most respondents across different surveys of physicians was “physical therapy”; however, this is a profession and not a distinct modality. Moreover, a survey of 100 physiotherapy and occupational therapy students in their final year of study found that only 13% disagreed with the statement that patients with fibromyalgia were difficult to manage, and less than half endorsed that they possessed the clinical skills to effectively manage fibromyalgia patients.[55]
The most recent evidence-based guidelines for management of fibromyalgia were published in 2017 by the European League Against Rheumatism (EULAR). These guidelines provided 10 recommendations regarding pharmacological and non-pharmacological management strategies for fibromyalgia.[56] The only strong recommendation in favor was for aerobic and strengthening exercise. We found that while exercise was often endorsed by physicians in their management of fibromyalgia, there remained high variability. For example, aerobic exercise was endorsed by 22% to 50% of survey respondents, and exercise in general was endorsed by 30% to 98% of respondents.
The EULAR guidelines did not make recommendations against any treatment approach,[56] and the remaining 9 recommendations were all weak in favor, including for tramadol (an opioid), whereas very few physicians surveyed in the studies we reviewed endorsed use of opioids (range 3–20%). The EULAR guidelines made no recommendations for most complementary and alternative therapies (except for acupuncture, meditative movement therapies, and mindfulness-based stress reduction); however, several physicians in the surveys we reviewed endorsed their use for fibromyalgia (e.g., osteopathy 12–33%, homeopathy 3–21%). Moreover, a 2020 survey of 670 people living with fibromyalgia found that 89% endorsed use of vitamin supplements, and 47% use of herbal medicines, with only about half endorsing aerobic exercise.[57] The EULAR guidelines made no recommendation for NSAIDs, and the most recent Cochrane review found very low certainty evidence that NSAIDs have no effect on pain or other symptoms in people with moderate or severe pain from fibromyalgia[58]; however, between 22% and 61% of physicians surveyed in the studies we reviewed endorsed their use.
5. Conclusions
Our review suggests that physicians are divided as to whether fibromyalgia is primarily a biomedical or psychosocial disorder. Management of fibromyalgia by physicians appears diverse and highly variable and updated, evidence-based, clinical practice guidelines are urgently needed to help improve the concordance between evidence and practice.
Author contributions
Conceptualization: Arnav Agarwal, Jason W. Busse.
Data curation: Peter C. Emary, Arnav Agarwal, Lucas Gallo, Yvgeniy Oparin, Arjun Rai.
Formal analysis: Peter C. Emary, Arnav Agarwal, Jason W. Busse.
Methodology: Li Wang, Jason W. Busse.
Project administration: Rachel J. Couban.
Supervision: Jason W. Busse.
Writing – original draft: Peter C. Emary, Arnav Agarwal.
Writing – review & editing: Peter C. Emary, Arnav Agarwal, Lucas Gallo, Yvgeniy Oparin, Sae Ha Shin, Mary-Ann Fitzcharles, Jonathan D. Adachi, Matthew D. Cooper, Samantha Craigie, Arjun Rai, Li Wang, Rachel J. Couban, Jason W. Busse.
Supplementary Material
Abbreviations:
- ACR
- American College of Rheumatology
- CI
- confidence interval
- EULAR
- European League Against Rheumatism
- GP
- general practitioner
- NSAIDs
- nonsteroidal anti-inflammatory drugs
No funds were received for the preparation of this manuscript. P.C.E. is supported by a post-doctoral award from the Michael G. DeGroote Institute for Pain Research and Care at McMaster University and research grants from the Canadian Institutes of Health Research (CIHR), the NCMIC Foundation, and the Canadian Chiropractic Research Foundation outside of the submitted work. J.W.B. is supported, in part, by a CIHR Canada Research Chair in the prevention and management of chronic pain. The authors have no other competing interests to declare.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental Digital Content is available for this article.
How to cite this article: Agarwal A, Emary PC, Gallo L, Oparin Y, Shin SH, Fitzcharles M-A, Adachi JD, Cooper MD, Craigie S, Rai A, Wang L, Couban RJ, Busse JW. Physicians’ knowledge, attitudes, and practices regarding fibromyalgia: A systematic review and meta-analysis of cross-sectional studies. Medicine 2024;103:31(e39109).
A.A. and P.C.E. contributed equally to the organization and writing of this manuscript.
Contributor Information
Arnav Agarwal, Email: arnav.agarwal@medportal.ca.
Lucas Gallo, Email: gallol@mcmaster.ca.
Yvgeniy Oparin, Email: opariny@mcmaster.ca.
Sae Ha Shin, Email: sshin2025@meds.uwo.ca.
Mary-Ann Fitzcharles, Email: mfitzcharles@sympatico.ca.
Jonathan D. Adachi, Email: jd.adachi@sympatico.ca.
Matthew D. Cooper, Email: matthew.daniel.cooper@gmail.com.
Samantha Craigie, Email: sam.craigie@gmail.com.
Arjun Rai, Email: raia10@dyc.edu.
Li Wang, Email: wangli1@mcmaster.ca.
Rachel J. Couban, Email: rcouban@mcmaster.ca.
References
- [1].Siracusa R, Paola RD, Cuzzocrea S, Impellizzeri D. Fibromyalgia: pathogenesis, mechanisms, diagnosis and treatment options update. Int J Mol Sci . 2021;22:3891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Jones GT, Atzeni F, Beasley M, Flüß E, Sarzi-Puttini P, Macfarlane GJ. The prevalence of fibromyalgia in the general population: a comparison of the American College of Rheumatology 1990, 2010, and modified 2010 classification criteria. Arthritis rheumatol (Hoboken, N.J.). 2015;67:568–75. [DOI] [PubMed] [Google Scholar]
- [3].Heidari F, Afshari M, Moosazadeh M. Prevalence of fibromyalgia in general population and patients, a systematic review and meta-analysis. Rheumatol Int. 2017;37:1527–39. [DOI] [PubMed] [Google Scholar]
- [4].Wolfe F, Clauw DJ, Fitzcharles MA, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46:319–29. [DOI] [PubMed] [Google Scholar]
- [5].Srinivasan S, Maloney E, Wright B, et al. The problematic nature of fibromyalgia diagnosis in the community. ACR Open Rheumatol. 2019;1:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Robinson RL, Kroenke K, Mease P, et al. Burden of illness and treatment patterns for patients with fibromyalgia. Pain Med. 2012;13:1366–76. [DOI] [PubMed] [Google Scholar]
- [7].Fitzcharles MA, Da Costa D, Pöyhiä R. A study of standard care in fibromyalgia syndrome: a favorable outcome. J Rheumatol. 2003;30:154–9. [PubMed] [Google Scholar]
- [8].Wolfe F, Anderson J, Harkness D, et al. Work and disability status of persons with fibromyalgia. J Rheumatol. 1997;24:1171–8. [PubMed] [Google Scholar]
- [9].Martinez JE, Ferraz MB, Sato EI, Atra E. Fibromyalgia versus rheumatoid arthritis: a longitudinal comparison of the quality of life. J Rheumatol. 1995;22:270–4. [PubMed] [Google Scholar]
- [10].Briones-Vozmediano E, Vives-Cases C, Ronda-Pérez E, Gil-González D. Patients’ and professionals’ views on managing fibromyalgia. Pain Res Manag. 2013;18:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Climent-Sanz C, Hamilton KR, Martínez-Navarro O, et al. Fibromyalgia pain management effectiveness from the patient perspective: a qualitative evidence synthesis. Disabil Rehabil. 2023;1:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hayes SM, Myhal GC, Thornton JF, et al. Fibromyalgia and the therapeutic relationship: where uncertainty meets attitude. Pain Res Manag. 2010;15:385–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [14].Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Randolph AG, Cook DJ, Guyatt G. Chapter 20: prognosis. In: Guyatt G, Rennie D, Meade MO, Cook DJ, editors. Users’ Guides to the medical literature: a manual for evidence-based clinical practice. 3rd Ed. New York: McGraw-Hill; 2015. p. 421–429 [Google Scholar]
- [16].Agarwal A, Guyatt GH, Busse JW. Methods commentary: risk of bias in cross-sectional surveys of attitudes and practices. Ottawa, Canada: Evidence Partners, 2017. [Google Scholar]
- [17].Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- [18].Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Statist. 1950;21:607–11. [Google Scholar]
- [19].Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [21].Miller J. The inverse of the Freeman-Tukey double arcsine transformation. Am Stat. 1978;32:138. [Google Scholar]
- [22].Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94. [DOI] [PubMed] [Google Scholar]
- [23].Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023). Cochrane, 2023. www.training.cochrane.org/handbook. Accessed July 22 2024. [Google Scholar]
- [24].Rucker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I2 in assessing heterogeneity may mislead. BMC Med Res Methodol. 2008;8:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Guyatt GH, Oxman AD, Kunz R, et al. GRADE Working Group. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011;64:1294–302. [DOI] [PubMed] [Google Scholar]
- [26].United Nations, Department of Economic and Social Affairs, Population Division. 2022. World Population Prospects 2022, Online Edition. https://population.un.org/wpp/Download/Documentation/Documentation/. Accessed July 22, 2024. [Google Scholar]
- [27].Schandelmaier S, Briel M, Varadhan R, et al. Development of the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN) in randomized controlled trials and meta-analyses. CMAJ. 2020;192:E901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Buskila D, Neumann L, Sibirski D, Shvartzman P. Awareness of diagnostic and clinical features of fibromyalgia among family physicians. Fam Pract. 1997;14:238–41. [DOI] [PubMed] [Google Scholar]
- [29].Blotman F, Thomas E, Myon E, Andre E, Caubere JP, Taïeb C. Awareness and knowledge of fibromyalgia among French rheumatologists and general practitioners. Clin Exp Rheumatol. 2005;23:697–700. [PubMed] [Google Scholar]
- [30].Arshad A, Ooi KK. Awareness and perceptions of fibromyalgia syndrome: a survey of Southeast Asian rheumatologists. JCR. 2007;13:59–62. [DOI] [PubMed] [Google Scholar]
- [31].Lu TV, Torres-Harding SR, Jason LA. The effectiveness of early educational intervention in improving future physicians’ attitudes regarding CFS/fibromyalgia. J Chronic Fatigue Syndr. 2007;14:25–30. [Google Scholar]
- [32].Silverman SL, Harnett J, Zlateva G, Mardekian J. Identifying fibromyalgia-associated symptoms and conditions from a clinical perspective: a step toward evaluating healthcare resource utilization in fibromyalgia. Pain Pract. 2010;10:520–9. [DOI] [PubMed] [Google Scholar]
- [33].Hadker N, Garg S, Chandran AB, Crean SM, McNett MM, Silverman SL. Primary care physicians’ perceptions of the challenges and barriers in the timely diagnosis, treatment and management of fibromyalgia. Pain Res Manag. 2011;16:440–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ghazan-Shahi S, Towheed T, Hopman W. Should rheumatologists retain ownership of fibromyalgia? A survey of Ontario rheumatologists. Clin Rheumatol. 2012;31:1177–81. [DOI] [PubMed] [Google Scholar]
- [35].Perrot S, Choy E, Petersel D, Ginovker A, Kramer E. Survey of physician experiences and perceptions about the diagnosis and treatment of fibromyalgia. BMC Health Serv Res. 2012;12:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bloom S, Ablin JN, Lebel D, et al. Awareness of diagnostic and clinical features of fibromyalgia among orthopedic surgeons. Rheumatol Int. 2013;33:927–31. [DOI] [PubMed] [Google Scholar]
- [37].Clark P, Paiva ES, Ginovker A, Salomon PA. A patient and physician survey of fibromyalgia across Latin America and Europe. BMC Musculoskelet Disord. 2013;14:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Mu R, Li C, Zhu JX, et al. National survey of knowledge, attitude and practice of fibromyalgia among rheumatologists in China. Int J Rheum Dis. 2013;16:258–63. [DOI] [PubMed] [Google Scholar]
- [39].Amber KT, Brooks L, Chee J, Ference TS. Assessing the perceptions of fibromyalgia syndrome in United States among academic physicians and medical students: where are we and where are we headed? J Musculoskeletal Pain. 2014;22:13–9. [Google Scholar]
- [40].Able SL, Robinson RL, Kroenke K, et al. Variations in the management of fibromyalgia by physician specialty: rheumatology versus primary care. Pragmat Obs Res. 2016;7:11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kianmehr N, Haghighi A, Bidari A, Sharafian Ardekani Y, Karimi MA. Are general practitioners well informed about fibromyalgia? Int J Rheum Dis. 2017;20:1917–21. [DOI] [PubMed] [Google Scholar]
- [42].Ortiz FE, Capitán de la Cruz VA, León Jiménez FE. Knowledge on fibromyalgia among general practitioners, from Chiclayo-Peru, 2016. Reumatol Clin. 2017;13:326–30. [DOI] [PubMed] [Google Scholar]
- [43].Agarwal A, Oparin Y, Glick L, et al. Attitudes toward and management of fibromyalgia: a national survey of Canadian rheumatologists and critical appraisal of guidelines. J Clin Rheumatol. 2018;24:243–9. [DOI] [PubMed] [Google Scholar]
- [44].Kumbhare D, Ahmed S, Sander T, Grosman-Rimon L, Srbely J. A survey of physicians’ knowledge and adherence to the diagnostic criteria for fibromyalgia. Pain Med. 2018;19:1254–64. [DOI] [PubMed] [Google Scholar]
- [45].Torres X, Ojeda B, Collado A, et al. Characterization of burnout among Spanish family physicians treating fibromyalgia patients: the EPIFFAC study. J Am Board Fam Med. 2020;33:386–96. [DOI] [PubMed] [Google Scholar]
- [46].Hyder Zaidi ST, Ashraf H, Javaid SS, et al. Survey of knowledge and attitude towards fibromyalgia among physicians in Karachi, Pakistan. Br J Pain. 2022;16:593–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Ketenci S, Gölboyu BE, Salbaş E, Uzuner B, Çiftçi B. The attitudes of Turkish physicians in the treatment of fibromyalgia; is “Pregabalinophobia” the new reality of pain medicine? Agri. 2022;34:200–9. [DOI] [PubMed] [Google Scholar]
- [48].Fitzcharles MA, Ste-Marie PA, Goldenberg DL, et al. 2012 Canadian guidelines for the diagnosis and management of fibromyalgia syndrome: executive summary. Pain Res Manag. 2013;18:119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Fitzcharles MA, Ste-Marie PA, Goldenberg DL, et al. 2012. Canadian guidelines for the diagnosis and management of fibromyalgia syndrome. Montreal, Quebec: Canadian Rheumatology Association and Canadian Pain Society, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Asbring P, Närvänen AL. Ideal versus reality: physicians perspectives on patients with chronic fatigue syndrome (CFS) and fibromyalgia. Soc Sci Med. 2003;57:711–20. [DOI] [PubMed] [Google Scholar]
- [51].Byrne A, Jones K, Backhouse M, Rose F, Moatt E, van der Feltz-Cornelis C. Patient and primary care practitioners’ perspectives on consultations for fibromyalgia: a qualitative evidence synthesis. Prim Health Care Res Dev. 2023;24:e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].D’Agnelli S, Arendt-Nielsen L, Gerra MC, et al. Fibromyalgia: Genetics and epigenetics insights may provide the basis for the development of diagnostic biomarkers. Mol Pain. 2019;15:1744806918819944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Huang C, Zhang N, Wei M, et al. Methylation factors as biomarkers of fibromyalgia. Ann Transl Med. 2023;11:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Häuser W, Fitzcharles MA. Adherence to clinical guidelines for fibromyalgia: help or hindrance? Can J Pain. 2023;7:2255070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Busse JW, Kulkarni AV, Badwall P, Guyatt GH. Attitudes towards fibromyalgia: a survey of Canadian chiropractic, naturopathic, physical therapy and occupational therapy students. BMC Complement Altern Med. 2008;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76:318–28. [DOI] [PubMed] [Google Scholar]
- [57].Pfalzgraf AR, Lobo CP, Giannetti V, Jones KD. Use of complementary and alternative medicine in fibromyalgia: results of an online survey. Pain Manag Nurs. 2020;21:516–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Derry S, Wiffen PJ, Häuser W, et al. Oral nonsteroidal anti-inflammatory drugs for fibromyalgia in adults. Cochrane Database Syst Rev. 2017;3:CD012332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.