Introduction
To better address population cancer burden, the National Cancer Institute (NCI) of the United States requires each NCI-designated cancer center to perform outreach and research relevant to a self-defined catchment area on the basis of the geographic area it serves.1 Many non-NCI cancer centers have also established geographic catchment areas inspired by NCI's mandate, reporting requirements under the Affordable Care Act, and new Commission on Cancer standards.2,3 As a result, efforts have increased among all cancer centers to use geospatial science to interrogate cancer health disparities and drive cancer prevention and control efforts among catchment area populations. Geospatial approaches in cancer research expedite tracking geographically associated cancer incidence and mortality trends, identifying places with cancer health disparities and increased social and environmental risks, and directing the implementation of evidence-based cancer control strategies.4-9 Cancer centers have also responded by developing online geospatial dashboard applications for internal and external users.10-13 Yet, despite having similar objectives, centers often engage in these efforts independent of one another. Continued growth in using geospatial approaches to cancer research in the catchment area requires developing new tools and methods for accessing, analyzing, and visualizing the increasing amounts of available geographic data. Creating a common space for researchers to share ideas and learn from each other is vital to accomplishing this. The Catchment Area Research and Data Science (CARDS) group formed to foster such growth.
We founded CARDS in the fall of 2022 to build a supportive and collaborative community for individuals involved in cancer center catchment area data collection, analysis, and utilization. Initial efforts to do this have included multiple webinars, an email listserv, and participation in the creation of a new national conference. Our vision is that building such a community could help streamline progress in geospatial science for cancer research and reduce parallel efforts across institutions. We seek to do this through (1) supporting the free exchange of ideas, (2) encouraging the use of open-source development, and (3) advancing the creation of new methods, models and measures that can be applied broadly across catchment areas. This article seeks to demonstrate the impact these ideas can have through two examples featured in previous CARDS webinars and to cast a vision for the future directions of CARDS work and advocacy among US cancer centers.
Synergy Through Open-Source Development
The first example features two open-source projects designed to make accessing data easier for researchers and the community, and a synergy that emerged through the CARDS collaboration.
The University of Kansas Cancer Center (KUCC) developed the Organize and Prioritize Trends to Inform KU Cancer Center (OPTIK) initiative in 2018.11 The goal of OPTIK was to ensure a more inclusive approach to cancer assessment in KUCC's diverse catchment area and to make data accessible for describing the population living within its boundaries. At present, OPTIK consists of a data warehouse and several visualization applications. Staff retrieve data from public websites, state health department partners, and internal sources for OPTIK yearly and compile it into a comprehensive data source repository. These data then get used in the visualization applications and are made available to KUCC researchers on request. The data visualizations produced by OPTIK allow users to evaluate trends in demographics, screening, risk factors, cancer incidence, and cancer mortality to inform strategic research and outreach initiatives. OPTIK uses a combination of Tableau dashboards and R Shiny for data visualization, generating interactive heat maps, bar graphs, and other graphical representations of cancer risk factors and mortality rates. The data contained within OPTIK are presented annually to the KUCC catchment area committee, community advisory board, and cancer center leadership to guide a better understanding of catchment area needs and facilitate outreach and research planning.
Although researchers at KUCC were developing and implementing OPTIK, researchers at the University of Kentucky Markey Cancer Center (UKMCC) created the Cancer InFocus (CIF) data gathering and visualization platform.12 CIF automates the collection of data on UKMCC's catchment area at various geographic levels through a series of Python programs. These programs access dozens of publicly available sources related to cancer rates, social determinants of health, behavioral risk factors, and other health outcome–related data, and curate the results into comma-separated values files. These data can stand-alone or be used in conjunction with web-based mapping applications built in R Shiny.14 Like with OPTIK, these applications make obtaining data and assessing patterns more accessible to researchers but are also designed to be placed on public-facing websites for dissemination within the community. Although initially developed as a resource for UKMCC, staff generalized the CIF software to work on any set of US counties and offer it to other cancer centers and state cancer registries for use through a no-cost licensing agreement. As of May 2024, 26 cancer centers (including five nondesignated centers) and one state cancer registry have licensed the use of CIF.
In the Spring of 2023, KUCC connected with UKMCC to obtain a license for using CIF. The data provided by CIF helped enhance what was included in OPTIK and reduce time spent by KUCC researchers in compiling updates. Moreover, since CIF and OPTIK use the same open-source platform for data visualization, researchers at KUCC can easily integrate the two products. Through the free exchange of ideas and use of open-source development, KUCC added functionality to OPTIK with less resource commitment than would have been necessary to see similar gains on their own.
Solving Common Problems Using New Methods
Our second case example looks at how a cancer registry partnered with multiple organizations to aid in the creation and dissemination of a new method for reporting cancer incidence rates.
In 2018, the Greater Bay Area Cancer Registry (GBACR) based at the University of California, San Francisco (UCSF), began planning an interactive mapping tool for exploring cancer incidence rates, social determinants of health, and cancer-related risk factors across the state. Typical cancer incidence reporting uses county-level data with strict suppression rules to protect privacy. For California, this meant that dense urban counties lacked a desired amount of nuance, although suppression hid the rates among many of the state's more rural areas. The GBACR hoped to overcome this barrier by creating subcounty geographies for cancer data reporting. When they learned that NCI and Westat were undertaking a similar project, GBACR reached out and the groups decided to partner. This partnership resulted in methodology to generate a set of zones, led by NCI and Westat.15 Zones are an aggregation of contiguous census tracts based on sociodemographic similarity, designed to minimize data suppression and allow for more granular reporting of cancer incidence than previously possible. UCSF incorporated cancer reporting zones incidence data into an interactive web platform, California Health Maps, with the help of data visualization experts at GreenInfo Network (Fig 1).16 The arrival of California Health Maps has corresponded with a reduction of almost 50% in the number of custom cancer rate and case count data requests being submitted to the GBACR—from 89 in 2017 to 45 in 2023.
FIG 1.
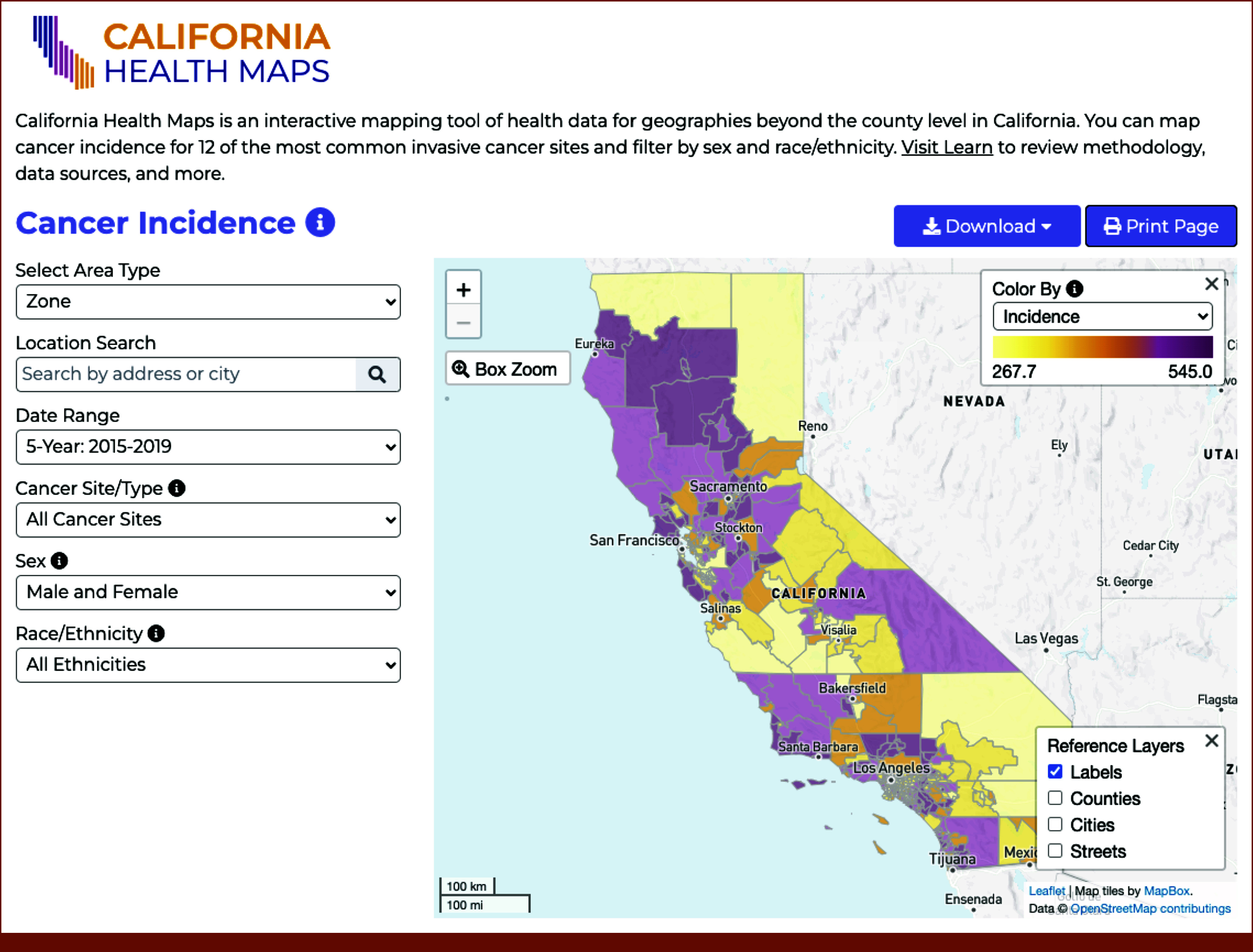
Example of state cancer surveillance dashboard using new statistical methodology. Screenshot of California Health Maps from the University of California, San Francisco.
NCI and Westat are currently using the automated zone design approach for generating cancer incidence rates with other cancer registries. They also provide open-source code developed by GreenInfo to disseminate these new rates through online mapping applications. To date, this platform has been adopted by three additional registries (Louisiana, Iowa, and Delaware). In the end, the focus on solving a common problem through common methods and tools resulted in a new and efficient way for cancer registries to provide data that better illustrate cancer's impact on the population to cancer centers and the communities they serve.
Future Directions
Informing Resource Utilization for Growth in Geospatial Sciences
Cancer centers must regularly make decisions about how to distribute time, money, and resources across a growing list of priorities. Responsible allocation of these is crucial to the growth of geospatial approaches to catchment area analysis. Internal and external collaboration should be used to minimize parallel efforts and redundancy. By freely sharing ideas and ongoing projects, CARDS has the potential to drive centers toward creating and evaluating products and processes that can be replicated by others. Helping cancer centers move away from the siloed approach that currently exists within the catchment area research and development space will lead to more efficient resource utilization. Federal agencies and nonprofit organizations incentivizing centers to work together to create reproducible, open-source platforms through funded opportunities would drive these collaborations further. CARDS can also create a learning space for geospatial science where new skills are presented in online workshops and networks for mentoring student and early career data professionals are established.
Advocating for Greater Data Access and the Development of New Metrics and Models
Cancer centers place significant time and effort into catchment area data retrieval, organization, normalization, and dissemination. Significant gains could be made by adopting a collaborative approach to this shared need. Since the majority of cancer centers use the same handful of publicly available sources for catchment area surveillance, developing a single, coordinated warehouse of US cancer rate and risk factor data would be of great benefit. Data within this warehouse could be curated to the specific catchment areas of cancer centers and accessible to them through an API or other automated download protocols. It could also be configured to allow cancer centers to submit previously unavailable data for the benefit of others, such as data collected through the Population Health Assessment in Cancer Center Catchment Areas supplemental funding initiative.17 Streamlining data gathering this way would offer an advantage over existing sources (eg, US Cancer Statistics Data Visualizations Tool, State Cancer Profiles), which often require manual downloads and are tailored to national- or state-level analysis rather than catchment areas.18,19 It would also ensure that researchers can spend more time developing new data sources, cancer surveillance metrics, and geospatial modeling techniques. Coordination between centers, registries, government agencies, and others will be required to create a data ecosystem that can both grow and be maintained for the future. Comprising data professionals from across US cancer centers, CARDS can advocate for the modern data infrastructure needed to combat our nation's cancer burden.
Determining Ways to Measure Impact
The most visible contribution of geospatial approaches to catchment area research to date is the development of numerous online dashboard applications. Although producing these dashboards is important for driving research that benefits the population, the research community must also find a way to measure their impact. Usage analytics products are available through many different sources and allow for varying degrees of tracking engagement and reach of online resources. Other methodologies more commonly found in the private sector, such as usability testing and user satisfaction surveys, could also be adopted. These metrics are vital to quantify the impact catchment area applications have on cancer-related information and health behaviors in the community. Furthermore, emphasis should be placed on researchers' appropriately crediting catchment area tools when they are used to obtain study data or perform analysis. The CARDS community can work to develop the methodologies and best practices to address this. Measuring impact of online dashboards may require new thinking among our cancer centers, and a closer engagement with the end users of our products, but will ensure that we gain the knowledge necessary to sustain and improve upon tool development into the future.
In conclusion, performing surveillance and doing research on the cancer burden of a specific geographic catchment area has become a common place in modern cancer centers. Rather than continuing to operate independently, a movement is underway for US cancer centers to share their catchment area tools and research knowledge and collaborate on the next generation of data resources. Building on the examples shared here—and with a commitment to the free exchange of ideas, the use of open-source development, and the creation of new geographic methods, models, and measures that can be applied broadly—cancer centers can chart a more efficient and effective path toward using data to fight the cancer burden within and beyond their catchment areas.
ACKNOWLEDGMENT
We acknowledge contributions from Scarlett Gomez of the University of California, San Francisco, and Greater Bay Area Cancer Registry, Zaria Tatalovich and David Stinchcomb of the National Cancer Institute, and Diane Ng of Westat.
SUPPORT
Supported by National Institutes of Health grants P30CA177558 (T.B.), 2P30CA082103-24 (D.L.O.), NCI5P30CA056036-17 (C.M.), and P30CA168524 (H.K., D.P.M.). D.L.O. also reports funding from California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention's (CDC) National Program of Cancer Registries, under cooperative agreement 1NU58DP007156; and the National Cancer Institute's Surveillance, Epidemiology, and End Results Program under contract HHSN261201800032I awarded to the University of California, San Francisco.
DATA SHARING STATEMENT
No data were analyzed in the preparation of this manuscript.
AUTHOR CONTRIBUTIONS
Conception and design: Todd Burus, Peter DelNero, Sam Pepper, Isuru Ratnayake, Debora L. Oh, Christopher McNair, Hope Krebill, Dinesh Pal Mudaranthakam
Financial support: Dinesh Pal Mudaranthakam
Administrative support: Dinesh Pal Mudaranthakam
Provision of study materials or patients: Dinesh Pal Mudaranthakam
Collection and assembly of data: Todd Burus, Josh Martinez, Peter DelNero, Sam Pepper, Isuru Ratnayake, Christopher McNair, Dinesh Pal Mudaranthakam
Data analysis and interpretation: Todd Burus, Sam Pepper, Christopher McNair, Dinesh Pal Mudaranthakam
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/cci/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Debora L. Oh
Employment: Amgen
Stock and Other Ownership Interests: Amgen
Hope Krebill
Employment: University of Kansas Medical Center, University of Kansas Medical Center
Honoraria: MJH Life Sciences
Consulting or Advisory Role: Locus Health (Inst), Locus Health (Inst)
Research Funding: National Cancer Institute, National Cancer Institute, National Institute of Health (NIH)
No other potential conflicts of interest were reported.
REFERENCES
- 1.Cancer Center Support Grants (CCSGs) for NCI-Designated Cancer Centers. https://grants.nih.gov/grants/guide/pa-files/PAR-21-321.html [Google Scholar]
- 2.Community Health Needs Assessment for Charitable Hospital Organizations—Section 501(r)(3). https://www.irs.gov/charities-non-profits/community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3 [Google Scholar]
- 3.Optimal Resources for Cancer Care: 2020 Standards. 2019. https://www.facs.org/quality-programs/cancer-programs/commission-on-cancer/standards-and-resources/2020/access/ [Google Scholar]
- 4.Xu Y, Fu C, Onega T, et al. : Disparities in geographic accessibility of National Cancer Institute cancer centers in the United States. J Med Syst 41:203, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrett NJ, Ingraham KL, Bethea K, et al. : Project PLACE: Enhancing community and academic partnerships to describe and address health disparities. Adv Cancer Res 146:167-188, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tai CG, Hiatt RA: The population burden of cancer: Research driven by the catchment area of a cancer center. Epidemiol Rev 39:108-122, 2017 [DOI] [PubMed] [Google Scholar]
- 7.Hiatt RA, Kobetz EN, Paskett ED, et al. : Community outreach and engagement revisited: The 2021 guidelines for cancer center support grants from the national cancer Institute. Cancer Prev Res 15:349-354, 2022 [DOI] [PubMed] [Google Scholar]
- 8.Finster LJ, Shirazipour CH, Escobedo LA, et al. : Addressing health disparities across the cancer continuum—a Los Angeles approach to achieving equity. Front Oncol 12:912832, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sahar L, Foster SL, Sherman RL, et al. : GIScience and cancer: State of the art and trends for cancer surveillance and epidemiology. Cancer 125:2544-2560, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paskett ED, Hiatt RA: Catchment areas and community outreach and engagement: The new mandate for NCI-designated cancer centers. Cancer Epidemiol Biomarkers Prev 27:517-519, 2018 [DOI] [PubMed] [Google Scholar]
- 11.Mudaranthakam DP, Harlan-Williams LM, Jensen RA, et al. : OPTIK: A database for understanding catchment areas to guide mobilization of cancer center assets. Database 2020:baaa054, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burus JT, Park L, McAfee CR, et al. : Cancer InFocus: Tools for cancer center catchment area geographic data collection and visualization. Cancer Epidemiol Biomarkers Prev 32:OF1-OF5, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manne SL, Knott CL, Berger A, et al. : Current approaches to serving catchment areas in cancer centers: Insights from the Big Ten Cancer Research Consortium Population Science Working Group. Cancer Epidemiol Biomarkers Prev 32:465-472, 2023 [DOI] [PubMed] [Google Scholar]
- 14.R Core Team : R: A Language and Environment for Statistical Computing, 2023. https://www.R-project.org/ [Google Scholar]
- 15.Tatalovich Z, Stinchcomb DG, Ng D, et al. : Developing geographic areas for cancer reporting using automated zone design. Am J Epidemiol 191:2109-2119, 2022 [DOI] [PubMed] [Google Scholar]
- 16.University of California, San Francisco School of Medicine Dean’s Office of Population Health and Health Equity. UCSF Health Atlas. 2022. www.healthatlas.ucsf.edu [Google Scholar]
- 17.Blake KD, Ciolino HP, Croyle RT: Population health assessment in NCI-designated cancer center catchment areas. Cancer Epidemiol Biomarkers Prev 28:428-430, 2019 [DOI] [PubMed] [Google Scholar]
- 18.US Cancer Statistics Working Group: US Cancer Statistics Data Visualizations Tool. US Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. 2024. https://www.cdc.gov/cancer/dataviz [Google Scholar]
- 19.National Cancer Institute, Centers for Disease Control and Prevention: State cancer Profiles. https://statecancerprofiles.cancer.gov/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data were analyzed in the preparation of this manuscript.


