Abstract
Introduction
The objective of this systematic review is to determine the benefits and harms of heel lifts to any comparator for lower limb musculoskeletal conditions.
Methods
Ovid MEDLINE, Ovid AMED, Ovid EMCARE, CINAHL Plus and SPORTDiscus were searched from inception to the end of May 2024. Randomised, quasi‐randomised or non‐randomised trials comparing heel lifts to any other intervention or no‐treatment were eligible for inclusion. Data was extracted for the outcomes of pain, disability/function, participation, participant rating of overall condition, quality of life, composite measures and adverse events. Two authors independently assessed risk of bias and certainty of evidence using the GRADE approach at the primary time point 12 weeks (or next closest).
Results
Eight trials (n = 903), investigating mid‐portion Achilles tendinopathy, calcaneal apophysitis and plantar heel pain were included. Heel lifts were compared to exercise, ultrasound, cryotherapy orthotics, stretching, footwear, activity modification, felt pads and analgesic medication. No outcome was at low risk of bias and few effects (2 out of 47) were clinically important. Low‐certainty evidence (1 trial, n = 199) indicates improved pain relief (55.7 points [95% CI: 50.3–61.1], on a 100 mm visual analogue scale) with custom orthotics compared to heel lifts at 12 weeks for calcaneal apophysitis. Very low‐certainty evidence (1 trial, n = 62) indicates improved pain and function with heel lifts over indomethacin (35.5 points [95% CI: 21.1–49.9], Foot Function Index) at 12 months for plantar heel pain.
Conclusions
Few trials have assessed the benefits and harms of heel lifts for lower limb musculoskeletal conditions. Only two outcomes out of 47 showed clinically meaningful between group differences. However, due to very low to low certainty evidence we are unable to be confident in the results and the true effect may be substantially different.
Registration
PROSPERO registration number CRD42022309644.
Keywords: musculoskeletal pain, orthotic devices, podiatry, rehabilitation, systematic review
1. INTRODUCTION
Non‐traumatic lower limb musculoskeletal conditions are common, reported to have an incidence of 19%–79% in the running population [1] and 16% in the sedentary population [2]. People with these lower limb conditions often report localised load‐related pain and disability, which affects sporting performance and promotes sedentary behaviors, with up to one third of all injured reported to not returning to their previous activity levels [2]. Considering that physical inactivity is a risk factor for multisystem disease [3], mental illness [4] and morbidity [5], injury to the lower limb can have a greater impact on individuals beyond sporting inconvenience.
First‐line treatments for non‐traumatic lower limb musculoskeletal conditions usually involve graduated exercise programs coupled with advice about managing occupational and sporting loads [6, 7, 8]; however, it is accepted that these treatments are not always successful and other interventions are sometimes needed [9]. One such option is heel lifts, which are shoe inserts designed to plantarflex the foot at the ankle joint [10]. Expert narratives and clinical guidelines support their use for a range of lower limb musculoskeletal conditions including, but not limited to, plantar heel pain [11], Achilles tendinopathy [12], calcaneal apophysitis [13] and anterior ankle impingement [14]. However, at present, there are no empirically proven guidelines to inform the recommended material (e.g., cork, polyurethane, EVA, etc.) or height of heel lift to use.
The speculated mechanisms by which heel lifts exert their effect are diverse and are yet to be fully understood [15]. Nonetheless, any clinically observed improvements in pain and function with heel lifts are often associated with alterations in various biomechanical variables, including temporospatial parameters [16], kinematics [17], dynamic plantar pressures [18], kinetics (e.g., joint moments [19]) and muscle function [20]. It is believed that these changes form the basis for the therapeutic effects of heel lifts. However, the biomechanical rationale for their application remains uncertain due to the limited and inconclusive evidence available in this field [15]. Despite the wide availability and use of heel lifts, no study has systematically reviewed research investigating the efficacy of heel lifts for lower limb musculoskeletal conditions. Summarising the musculoskeletal conditions that benefit or are at harm from heel lifts would serve as a valuable resource for clinicians to aid them in their decision‐making process.
1.1. Objectives
To determine the benefits and harms of heel lifts for lower limb musculoskeletal conditions compared to another intervention or a no treatment control (placebo, sham or wait‐and‐see).
2. METHODS
This systematic review was developed and reported according to the Preferred Reporting of Systematic Reviews and Meta‐Analysis (PRISMA) guidelines [21]. This systematic review was prospectively registered in the PROSPERO database; registration: CRD42022309644.
3. DEVIATIONS FROM STUDY REGISTRATION AND THE STUDY PROTOCOL
In our study registration, we also planned an analysis of biomechanical studies. Following peer‐review, we removed the biomechanical analysis, as it did not add anything to this systematic review. Instead, we have focussed on a high‐quality review of clinical outcomes.
4. CRITERIA FOR CONSIDERING STUDIES FOR THIS REVIEW
4.1. Types of studies
Randomised, quasi‐randomised and non‐randomised trials were included if one study arm used heel lifts (as an adjunct or primary intervention) compared to another intervention or a control (e.g., placebo, sham or wait‐and‐see) [22]. Trials that were unpublished, not peer reviewed or non‐English written studies were excluded.
4.2. Types of participants
We included all trials that recruited participants with a musculoskeletal condition, which may include but is not limited to conditions such as, Achilles tendinopathy and plantar heel pain. There were no restrictions on age or sex/gender. Trials including participants with neurological disorders, limb length discrepancies or a history of amputation were excluded.
4.3. Types of interventions
Heel lifts were defined as being removable (attached to the participant's barefoot or in the shoe) or a feature in‐built into a shoe intended to plantarflex the foot at the ankle joint [15]. Any comparisons were permitted and could include no treatment (placebo, sham or wait‐and‐see) or any intervention such as orthotics, exercise and education.
4.4. Types of outcome measures
Primary outcomes were pain, disability/function, participation, participant rating of overall condition, quality of life and composite measures, as they are recommended in the consensus statement for tendinopathy outcomes [23]. The number of participants reporting any adverse events (secondary outcome) were also extracted to provide a balanced perspective of harms.
4.5. Timing of outcome measures
The primary time point was 12 weeks (or the next closest time point) as it has commonly been used as a primary endpoint in clinical trials of interventions for musculoskeletal conditions [24, 25]. Outcome measures were obtained for the following time points: short term (0–6 weeks), medium term (>6–12 weeks), long term (>12 weeks) to comprehensively evaluate the benefits and harms of the interventions [26]. If two follow‐up assessments were reported within one of the defined time points, the results of the latter of the two assessments were selected [27].
5. SEARCH METHODS FOR IDENTIFICATION OF STUDIES
Database searching was performed across Ovid MEDLINE, Ovid AMED, Ovid EMCARE, CINAHL Plus and SPORTDiscus platforms from inception to the end of May 2024. The search strategy used a combination of key words pertinent to the research questions. The search syntax and related number of items found with each database can be found in Supporting Information S1. Forward and backward searches were conducted to identify other eligible trials (forward searches in Google Scholar and PubMed).
6. DATA COLLECTION AND ANALYSIS
6.1. Selection of studies
All trials identified from the search were downloaded into Endnote X9 (Thomson Reuters, Philadelphia, PA) and duplicates deleted by a single author (JB). Titles and abstracts of the trials were screened independently by two authors for inclusion (JB, EM) and any discrepancies were resolved by a third author (PM). If further information was required, the full‐text was obtained.
6.2. Data extraction and management
Relevant data were extracted and mapped to a characteristics table independently by two authors (JB, EM) and any discrepancies were resolved by a third author (PM). Additional data was retrieved from published protocols and trial registrations, where available. Any missing data was requested from the corresponding authors by a single author (JB) and considered unsuccessful if there was no reply after two attempts. The following was extracted from eligible trials:
trial characteristics: sample size, first author name, year of publication, type of trial (e.g., parallel, cross‐over);
participant characteristics: age, sex/gender, activity levels, adherence to the heel lifts, type of injury, duration of symptoms, type of footwear;
heel lift and comparator characteristics: height and material of the heel lifts and a description of the comparator intervention(s);
summary data for each outcome: number of events and number of participants per group for dichotomous outcomes, mean and standard deviation per group for continuous outcomes.
Definitions for the outcomes and our a priori decision rules for extracting data from multiple reported outcomes in trials can be found in the Supporting Information S2.
6.3. Assessment of risk of bias in included studies
Risk of bias assessment was performed using the revised Cochrane Collaboration tool for assessing risk of bias (RoB 2.0) [28, 29] independently by two authors (JB and SM). Disagreements were resolved by a third author (PM). An outcome was considered to have a high risk of bias if at least one of the criteria was rated high risk [30]. To be considered low risk of bias, all criteria had to be rated low risk [30]. Any outcomes not meeting these criteria were considered to be at some concern of risk of bias [30].
6.4. Measure of treatment effect
Measures of treatment effect were calculated as specified in the Cochrane Handbook for Systematic Reviews of Interventions [31]. For dichotomous outcomes, estimates were analyzed as risk ratios (RRs) with 95% confidence intervals (CIs). For continuous outcomes, estimates were analyzed as mean differences (MDs) with 95% CIs. We assumed a relative risk difference of 25% was a minimal clinically important difference (MCID) for dichotomous outcomes. Many different continuous outcome measures were included in this review; for example, pain was assessed using the visual analogue scale, subscale of the Foot Function Index, Faces Pain Scale and a 5‐point scale. Our assumed MCID for the different outcome measures is listed in Table 1. If we were unable to identify a suitable MCID, we used 10% of the maximum possible score of the outcome.
TABLE 1.
Minimal clinically important difference for the outcomes included in this review.
Two trials [36, 37] described their results in median and interquartile ranges; to calculate the MDs, the median was assumed as the mean and the interquartile range divided by 1.35 to identify the approximate standard deviations [38]. Where calculating MDs was not possible, a quote extracted from that trial was presented descriptively.
6.5. Assessment of the certainty of the evidence
Assessment of the certainty at the outcome level was undertaken using the GRADE approach for the primary time point (12 weeks) [39]. Two authors (JB, EM) independently assessed the quality of evidence, with a third author available to resolve any discrepancies (PM). The certainty of evidence for each outcome was graded as high, moderate, low or very low and presented in a Summary of Findings table [40]. We justified all decisions to downgrade the certainty of evidence using footnotes and made comments to aid the reader's understanding of the review where necessary. Our rules for determining the GRADE judgment for each outcome can be found in the Supporting Information S3, which were derived from the GRADE handbook [39] and consensus among authors (JB, PM, SM).
6.6. Data synthesis
Meta‐analysis was planned for trials with similar characteristics (e.g., participants, interventions, outcomes). Data was categorised according to the condition (e.g., plantar heel pain, Achilles tendinopathy, etc.). Different labels of conditions were grouped under a recommended label; for example, plantar fasciitis and ‘heel spur syndrome’ were grouped as plantar heel pain [11]. All MD calculations and quotes extracted from the trials can be found in Supporting Information S4.
7. RESULTS
7.1. Trial selection
Initially, 2109 records were retrieved and 880 deleted as duplicates and 256 removed by an automation tool to remove any records unrelated to humans. Of these, we assessed 14 in full‐text and excluded 6 after full‐text evaluation [41, 42, 43, 44, 45, 46], which yielded 8 [36, 37, 47, 48, 49, 50, 51, 52] trials eligible for inclusion (Figure 1).
FIGURE 1.
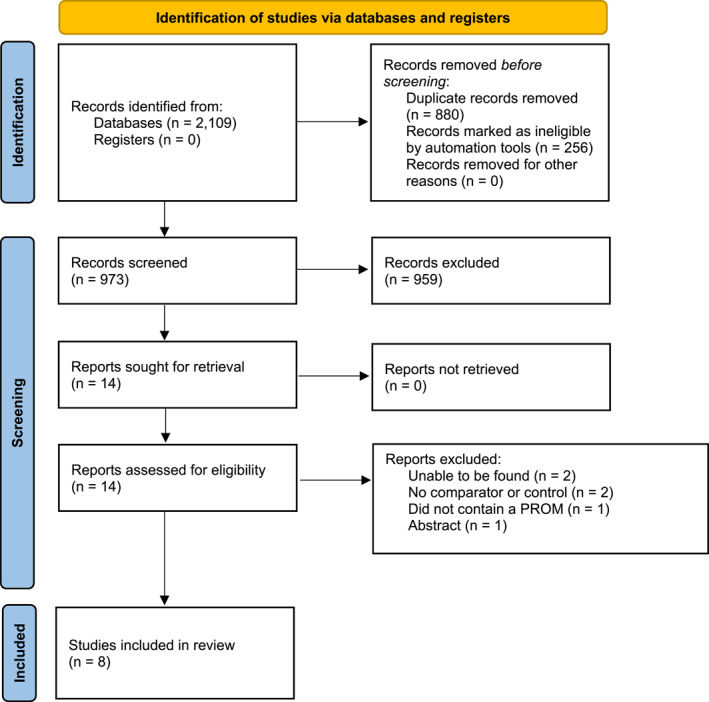
Flow of studies through the review process.
7.2. Trial characteristics
The characteristics of the included trials are shown in Supporting Information S4. All trials were randomised trials, seven were classified as parallel group superiority trials [36, 37, 47, 48, 50, 51, 52] and one used a 2 × 2 factorial design [49]. A total of 903 participants were included and sample sizes ranged from 23 to 208. The duration of the trials ranged from 8 to 52 weeks. Overall, participants were typically young adults (mean age = 31 years) and more than half were male (52%). The median height of heel lifts where reported was 8 mm (average = 9 mm, ranging from 6 to 12 mm) and they were manufactured from a variety of materials (e.g., ethyl vinyl acetate, silicone, proprietary products). The musculoskeletal conditions and interventions assessed were all single trial comparisons and were as follows.
7.2.1. Mid‐portion Achilles tendinopathy
heel lifts and activity modification versus eccentric calf exercises and activity modification [36];
heel lifts, therapeutic ultrasound, stretching and strengthening exercises for ‘posterior leg structures’ and activity modification versus therapeutic ultrasound, stretching and strengthening exercises for ‘posterior leg structures’ and activity modification [50].
7.2.2. Calcaneal apophysitis
heel lifts, cryotherapy, calf stretching and activity modification versus custom orthotics, cryotherapy, calf stretching and activity modification [47];
heel lifts, calf stretching and cryotherapy versus prefabricated orthotics, calf stretching and cryotherapy [49];
heel lifts, calf stretching and cryotherapy versus prefabricated orthotics, new Adidas runners, calf stretching and cryotherapy [49];
heel lifts versus activity modification [52];
heel lifts versus eccentric calf exercise [52].
7.2.3. Plantar heel pain
heel lifts, anti‐inflammatory medication and plantar fascia stretching versus custom orthotics, anti‐inflammatory medication and plantar fascia stretching [37];
heel lifts and a heat pack versus 75 mg of indomethacin [48].
heel lifts and a heat pack versus plantar fascia stretching and sham calf stretching [48];
heel lifts and a heat pack versus calf stretching and sham plantar fascia stretching [48];
heel lifts and ‘Achilles’ and plantar fascia stretching versus felt pads and ‘Achilles’ and plantar fascia stretching [51];
heel lifts and ‘Achilles’ and plantar fascia stretching versus custom orthotics and ‘Achilles’ and plantar fascia stretching [51];
heel lifts and ‘Achilles’ and plantar fascia stretching versus ‘Achilles’ and plantar fascia stretching [51].
7.3. Risk of bias assessment
The risk of bias for each included outcome is summarised in Figure 2. No outcome was judged to be at low risk of bias. Half of the outcomes were judged to have some concern of risk of bias (16 out of 31) and the other half at high risk of bias (15 out of 31). Most of the outcomes (94%) were downgraded due to being unable to blind the investigator, participant or both. Our rationale for the judgements can be found in the Supporting Information S5.
FIGURE 2.
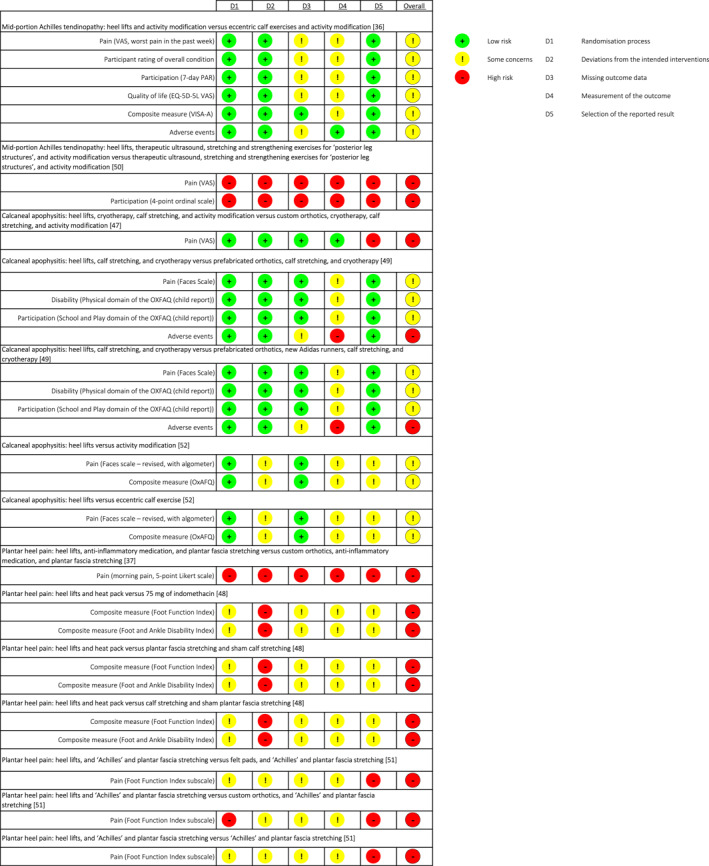
Risk of bias summary for each included outcome at the primary time point.
7.4. Effects of intervention
Results for the primary time point (12 weeks or next closest) are shown in the Summary of Findings table (Table 2) and for all time points in Figure 3. The full description of the interventions, outcomes assessed and time points extracted is located in Supporting Information S4. Meta‐analysis was not possible as there was significant heterogeneity in the comparator interventions between trials (no trial used the same heel lift and comparison). Instead, the findings were presented descriptively.
TABLE 2.
Summary of findings table for the primary time point (12 weeks).
| Outcomes | Mean difference (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments |
|---|---|---|---|---|
| Mid‐portion Achilles tendinopathy: Heel lifts and activity modification versus eccentric calf exercises and activity modification [36] | ||||
| Pain (VAS, worst pain in the past week) | −19.5 (−31.71 to −7.29) a | 80 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Participant/patient rating overall condition | Relative risk: 1.41 (1.02–1.95) a | 80 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Participation (7‐day PAR) | −51.5 (−512.88–409.88) | 80 (1 RCT) |
|
Downgraded due to some concerns of risk of bias. |
| Quality of life (EQ‐5D‐5 L VAS) | 2.1 (−3.39–7.59) | 80 (1 RCT) |
|
Downgraded due to some concerns of risk of bias. |
| Composite measure (VISA‐A) | 12.3 (3.52–21.08) a | 80 (1 RCT) |
|
Downgraded due to some concerns of risk of bias. |
| Adverse events | Relative risk: 1.05 (0.68–1.61) | 80 (1 RCT) |
|
Downgraded due to high risk of bias and group size < OIS. |
| Mid‐portion Achilles tendinopathy: Heel lifts, therapeutic ultrasound, stretching and strengthening exercises for ‘posterior leg structures’ and activity modification versus therapeutic ultrasound, stretching and strengthening exercises for ‘posterior leg structures’ and activity modification [50] | ||||
| Pain (VAS) | n/a | 33 (1 RCT) |
|
Downgraded due to high risk of bias, unable to calculate OIS and no description of how the condition was diagnosed. |
| Participation (4‐point ordinal scale) | n/a | 33 (1 RCT) |
|
Downgraded due to high risk of bias, unable to calculate OIS and no description of how the condition was diagnosed. |
| Calcaneal apophysitis: Heel lifts, cryotherapy, calf stretching and activity modification versus custom orthotics, cryotherapy, calf stretching and activity modification [47] | ||||
| Pain (VAS) | 55.7 (50.27–61.13) b | 199 (1 RCT) |
|
Downgraded due to a high risk of bias. |
| Calcaneal apophysitis: Heel lifts, calf stretching and cryotherapy versus prefabricated orthotics, calf stretching and cryotherapy [49] | ||||
| Pain (Faces scale) | 0 (−0.57 to 0.57) | 61 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Disability (physical domain of the OXFAQ (child report)) | −0.49 (−10.68–9.70) | 61 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Participation (school and play domain of the OXFAQ (child report)) | 3.32 (−3.75–10.39) | 61 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Adverse events | Relative risk: 0 (n/a) | 61 (1 RCT) |
|
Downgraded due to high risk of bias and group size < OIS. |
| Calcaneal apophysitis: Heel lifts, calf stretching and cryotherapy versus prefabricated orthotics, new Adidas runners, calf stretching and cryotherapy [49] | ||||
| Pain (faces scale) | 0.06 (−0.45–0.57) | 60 (1 RCT) |
|
Downgraded due to some concerns of risk of bias. |
| Disability (physical domain of the OXFAQ (child report)) | −4.96 (−13.90–3.98) | 60 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Participation (school and play domain of the OXFAQ (child report)) | −2.92 (−8.60–2.76) | 60 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and group size < OIS. |
| Adverse events | Relative risk: 0 (n/a) | 60 (1 RCT) |
|
Downgraded due to high risk of bias and group size < OIS. |
| Calcaneal apophysitis: Heel lifts versus activity modification [52] | ||||
| Pain (faces scale—revised, with algometer) | 0.4 (−1.01–1.81) | 63 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and compressing apophysis with algometer not reflective of clinical practice. |
| Composite measure (OXFAQ) | 4.8 (−0.11–9.71) | 63 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and having a wide confidence interval. |
| Calcaneal apophysitis: Heel lifts versus eccentric calf exercise [52] | ||||
| Pain (faces scale—revised, with algometer) | 0.5 (−0.95–1.95) | 65 (1 RCT) |
|
Downgraded due to some concerns of risk of bias and compressing apophysis with algometer not reflective of clinical practice. |
| Composite measure (OXFAQ) | 3 (−1.22–7.22) | 65 (1 RCT) |
|
Downgraded due to some concerns of risk of bias. |
| Plantar heel pain: Heel lifts, anti‐inflammatory medication and plantar fascia stretching versus custom orthotics, anti‐inflammatory medication and plantar fascia stretching [37] | ||||
| Pain (morning pain, 5‐point Likert scale) | 0.5 (−0.27–1.27) | 60 (1 RCT) |
|
Downgraded due to high risk of bias and group size < OIS. |
| Plantar heel pain: Heel lifts and heat pack versus 75 mg of indomethacin [48] | ||||
| Composite measure (foot function index) | −35.5 (−49.4 to −21.06) b | 62 (1 RCT) |
|
Downgraded due to high risk of bias and group size < OIS. |
| Composite measure (foot and ankle disability index) | 16.5 (6.56–26.44) a | 62 (1 RCT) |
|
Downgraded due to high risk of bias and group size < OIS. |
| Plantar heel pain: Heel lifts and heat pack versus plantar fascia stretching and sham calf stretching [48] | ||||
| Composite measure (foot function index) | 4.9 (−1.7–11.59) | 62 (1 RCT) |
|
Downgraded due to high risk of bias. |
| Composite measure (foot and ankle disability index) | −3.2 (−9.97–3.57) | 62 (1 RCT) |
|
Downgraded due to high risk of bias. |
| Plantar heel pain: Heel lifts and heat pack versus calf stretching and sham plantar fascia stretching [48] | ||||
| Composite measure (foot function index) | −3.8 (−13.22–5.62) | 60 (1 RCT) |
|
Downgraded due to high risk of bias and having a wide confidence interval. |
| Composite measure (foot and ankle disability index) | 4.2 (−3.90–12.30) | 60 (1 RCT) |
|
Downgraded due to high risk of bias and having a wide confidence interval. |
| Plantar heel pain: Heel lifts and ‘Achilles’ and plantar fascia stretching versus felt pads and ‘Achilles’ and plantar fascia stretching [51] | ||||
| Pain (foot function index subscale) | n/a | 98 (1 RCT) |
|
Downgraded due to high risk of bias, unable to calculate OIS and ‘felt pad’ not reflective of clinical practice. |
| Plantar heel pain: Heel lifts and ‘Achilles’ and plantar fascia stretching versus custom orthotics and ‘Achilles’ and plantar fascia stretching [51] | ||||
| Pain (foot function index subscale) | n/a | 93 (1 RCT) |
|
Downgraded due to high risk of bias and unable to calculate OIS. |
| Plantar heel pain: Heel lifts and ‘Achilles’ and plantar fascia stretching versus ‘Achilles’ and plantar fascia stretching [51] | ||||
| Pain (foot function index subscale) | n/a | 97 (1 RCT) |
|
Downgraded due to high risk of bias and unable to calculate OIS. |
Note: GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate.
Statistically significant.
Statistically significant and exceeds the MID.
FIGURE 3.
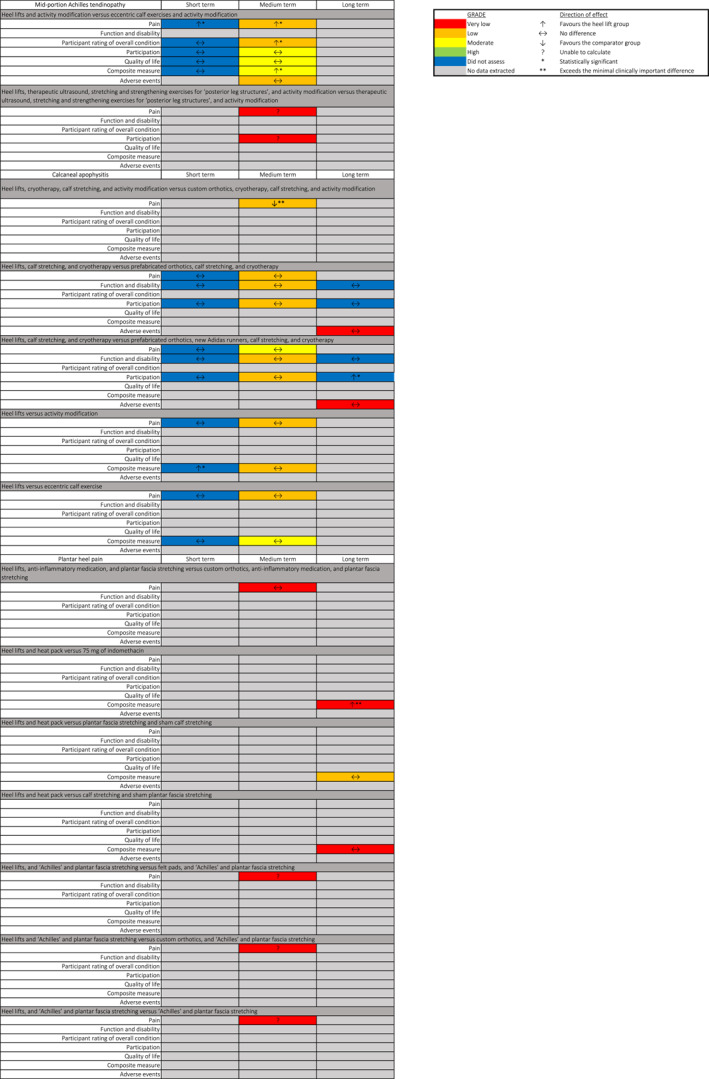
Summary of outcomes for all time points.
7.4.1. Mid‐portion Achilles tendinopathy
7.4.1.1. Heel lifts and activity modification versus eccentric calf exercises and activity modification [36]
At the primary timepoint (reported at 12 weeks), heel lifts were found to be superior to eccentric calf exercise in reducing pain severity by 19.5 points on a 100 mm visual analogue scale (VAS) (95% CI: 7.29–31.71), the VISA‐A questionnaire by 12.3 points (95% CI: 3.52–21.08) and participant rating of overall condition (relative risk: 1.41, 95% CI: 1.02–1.95) (low to moderate certainty evidence). The rate of adverse events was similar between groups (relative risk: 1.05, 95% CI: 0.71–1.54) and included developing areas of new pain (lower back, hips, knees, feet or ankles) and/or blisters (low certainty evidence). In the short‐term (reported at 6 weeks), heel lifts were found to be superior to eccentric calf exercise in reducing pain severity on a 100 mm VAS outcome by 15.1 points (95% CI: 2.75–27.45).
7.4.1.2. Heel lifts, therapeutic ultrasound, stretching and strengthening exercises for ‘posterior leg structures’ and activity modification versus therapeutic ultrasound, stretching and strengthening exercises for ‘posterior leg structures’ and activity modification [50]
At the primary time point (reported at 8 weeks), mean differences were unable to be calculated. The trial authors reported that the “benefit of viscoelastic pads widely used by athletes was not substantiated” (very low certainty evidence).
7.4.2. Calcaneal apophysitis
7.4.2.1. Heel lifts, cryotherapy, calf stretching and activity modification versus custom orthotics, cryotherapy, calf stretching and activity modification [47]
At the primary timepoint (reported at 12 weeks), heel lifts were found to be inferior to custom orthotics in reducing pain severity by 55.7 points on a 100 mm VAS (95% CI: 50.27–61.13, low certainty evidence).
7.4.2.2. Heel lifts, calf stretching and cryotherapy versus prefabricated orthotics, calf stretching and cryotherapy [49]
At the primary timepoint (reported at 8 weeks), there were no differences between groups for any outcome (low certainty evidence) and no participant reported any adverse reaction to the interventions (very low certainty evidence). In the short‐term (reported at 4 weeks) and long‐term (reported at 52 weeks), there were no differences between groups for any outcome.
7.4.2.3. Heel lifts, calf stretching and cryotherapy versus prefabricated, new Adidas runners, calf stretching and cryotherapy [49]
At the primary timepoint (reported at 8 weeks), there were no differences between groups for any outcome (low certainty evidence) and no participant reported any adverse reaction to the interventions (very low certainty evidence). In the short‐term (reported at 4 weeks), there were no differences between groups for any outcome. In the long‐term (reported at 52 weeks), heel lifts were found to be superior to the prefabricated orthotics and new Adidas runners in the Oxford Foot Ankle Questionnaire—School and Play domain by 6.7 points (95% CI: 0.84–12.56).
7.4.2.4. Heel lifts versus activity modification [52]
At the primary timepoint (reported at 12 weeks), there were no differences between groups for any outcome (low certainty evidence). In the short‐term (reported at 6 weeks), heel lifts were found to be superior to the activity modification group in the Oxford Foot and Ankle Questionnaire by 4.5 points (95% CI: 1.24–7.76).
7.4.2.5. Heel lifts versus eccentric calf exercise [52]
At the primary (reported at 12 weeks), there were no differences between groups for any outcome (low to moderate certainty evidence). In the short‐term (reported at 6 weeks), there were no differences between groups for any outcome.
7.4.3. Plantar heel pain
Heel lifts, anti‐inflammatory medication and plantar fascia stretching versus custom orthotics, anti‐inflammatory medication and plantar fascia stretching [37]
At the primary timepoint (reported at 12 weeks), there were no differences between groups (very low certainty evidence).
7.4.3.1. Heel lifts and heat pack versus 75 mg of indomethacin [48]
At the primary timepoint (reported at 52 weeks), heel lifts were found to be superior to 3 weeks of 75 mg of Indomethacin in the Foot Function Index (FFI) by 35.5 points (95% CI: 21.06–49.94) and Foot and Ankle disability Index (FADI) by 16.5 points (95% CI, 6.56–26.44) (very low certainty evidence).
7.4.3.2. Heel lifts and heat pack versus plantar fascia stretching and sham calf stretching [48]
At the primary timepoint (reported at 52 weeks), there were no differences between groups for any outcome (low certainty evidence).
7.4.3.3. Heel lifts and heat pack versus calf stretching and sham plantar fascia stretching [48]
At the primary timepoint (reported at 52 weeks), there were no differences between groups for any outcome (very low certainty evidence).
7.4.3.4. Heel lifts and ‘Achilles’ and plantar fascia stretching versus felt pads and ‘Achilles’ and plantar fascia stretching [51]
At the primary time point (reported at 8 weeks), mean differences were unable to be calculated. The trial authors reported that the silicone heel lift group improved by ‘95%’ compared to the felt pads ‘81%’ (very low certainty evidence).
7.4.3.5. Heel lifts and ‘Achilles’ and plantar fascia stretching versus custom orthotics and ‘Achilles’ and plantar fascia stretching [51]
At the primary time point (reported at 8 weeks), mean differences were unable to be calculated. The trial authors reported that the silicone heel lift group improved by ‘95%’ compared to the custom orthotics ‘68%’ (very low certainty evidence).
7.4.3.6. Heel lifts and ‘Achilles’ and plantar fascia stretching versus ‘Achilles’ and plantar fascia stretching [51]
At the primary time point (reported at 8 weeks), mean differences were unable to be calculated. The trial authors reported that the silicone heel lift group improved by ‘95%’ compared to the stretching group ‘72%’ (very low certainty evidence).
8. DISCUSSION
This is the first systematic review to investigate the benefits and harms of heel lifts for lower limb musculoskeletal conditions. Although heel lifts are recommended for numerous lower limb musculoskeletal conditions, such as posterior leg muscle strains [42], the existing evidence is limited to eight trials and three musculoskeletal conditions (mid‐portion Achilles tendinopathy, plantar heel pain and calcaneal apophysitis). Overall, the current evidence indicates that heel lifts may be effective for mid‐portion Achilles tendinopathy [36] and plantar heel pain [48] when compared to eccentric exercise and 75 mg of Indomethacin, respectively; but not for calcaneal apophysitis [47] when compared to custom orthotics. The harms of heel lifts are uncertain.
The benefit of heel lifts over exercise for mid‐portion Achilles tendinopathy in perception of treatment effect, reducing pain severity and improving VISA‐A scores, is a noteworthy finding given that the latest clinical practice guidelines recommend exercise, but they do not mention heel lifts [53]. Heel lifts are inexpensive, widely available and do not have to contend with the same behavioral change demands of a complex intervention such as exercise [54]. However, it is worthwhile noting the between group difference for the trial reporting favourable effects of heel lifts over eccentric calf muscle exercise, did not exceed the threshold of the minimal clinically important difference, which means it is unclear whether patients would be able to discern an appreciable difference if they were prescribed either intervention [55]. The benefit of heel lifts over Indomethacin for plantar heel pain, reflected in the FFI and FADI scores, is less surprising given the equivocal findings regarding oral anti‐inflammatory medications compared to sham treatments for this condition [56]. Although, any observed benefits of heel lifts may have been overestimated by 17 participants (out of 35) having their treatment terminated in the Indomethacin group after three weeks. Finally, there was a large effect favoring custom orthotics when compared to heel lifts for reducing pain severity in calcaneal apophysitis, presenting an interesting contrast to the lack of difference observed when comparing heel lifts to prefabricated orthotics for the same condition. Differences in the materials (soft vs. hard) and processes for supply (custom vs. prefabricated) leading to non‐intervention effects are plausible explanations for the discrepancy in outcomes; however, further investigation is required to elucidate these findings.
An important consideration when interpreting the findings of this review relates to the quality of the trials that investigated the effectiveness of heel lifts. Using GRADE, the certainty of evidence of the findings reported in these trials was judged to be very low (39%), low (45%) and moderate (16%), which means we have limited confidence in the estimates of effect and they are likely to change when future trials are conducted [39]. Importantly, half of the outcomes (15/31) were at high risk of bias, mainly due to an absence of measures to blind the investigator, participant and/or both. Although we acknowledge the inherent difficulty in blinding participants to any physical interventions of any kind in clinical trials [57], performance bias is a risk across the included trials.
9. CLINICAL RESEARCH IMPLICATIONS
Comparisons were made between heel lifts and various comparator interventions, including eccentric calf exercise, ultrasound, stretching, prefabricated and custom orthotics, new shoes, education regarding activity modification, felt pads and analgesic medication. However, no trial compared heel lifts to a no treatment control (placebo, wait‐and‐see or sham), which is an understandable omission if the aim was to assess superiority between treatments instead of efficacy. However, the absence of no treatment‐based trials leaves uncertainty as to whether any observed effects of heel lifts are due to specific treatment effects, non‐specific factors such as placebo, the natural progression of the condition(s) or expectancy effects [58, 59]. Further high‐quality randomised controlled trials (comparing heel lifts to a no treatment control) are required to determine the efficacy of heel lifts for lower limb musculoskeletal conditions for which they are recommended.
10. STRENGTHS AND LIMITATIONS
The strengths of this review include the inclusion of only randomised trials and an appraisal of the evidence using RoB2 and GRADE, which are both recommended tools. This was performed by two independent people to reduce the risk of assessment bias. However, there are limitations requiring acknowledgment. First, analyses were from single trials as we were unable to perform a meta‐analysis due to the significant heterogeneity, which lowers our confidence in the estimates of effect. Second, this review omitted non‐English‐language trials. Systematic bias is unlikely to have been introduced by the English language restriction, but inclusion of more studies may have improved precision [60].
11. CONCLUSION
This systematic review of eight trials demonstrates that the current evidence for the efficacy and safety of heel lifts for lower limb musculoskeletal conditions is limited to mid‐portion Achilles tendinopathy, calcaneal apophysitis and plantar heel pain. There is very low certainty evidence for the benefit of heel lifts compared to indomethacin (analgesic medication) for plantar heel pain at 12 months; but not calcaneal apophysitis when compared to custom orthotics (low certainty evidence) at 12 weeks. The remaining (45 out of 47) outcomes of various comparators including eccentric calf exercise, ultrasound, cryotherapy, stretching, prefabricated orthotics, new shoes, activity modification education and felt pads found no clinically important differences between groups for the conditions assessed. Most of the evidence these findings are drawn from is of very low to low certainty, so there is a distinct possibility that future trials of high quality may change some of the findings of this review. Rigorous trials are needed to assess the clinical efficacy and safety of heel lifts for conditions for which they are currently recommended.
AUTHOR CONTRIBUTIONS
Jaryd Bourke: Conceptualization; methodology; data curation; formal analysis; writing—original draft; writing—review and editing. Shannon Munteanu: Conceptualization; methodology; formal analysis; writing—review and editing; supervision. Eman Merza: Formal analysis; writing—review and editing. Alessandro Garofolini: Conceptualization; writing—review and editing; supervision. Simon Taylor: Conceptualization; writing—review and editing; supervision. Peter Malliaras: Conceptualization; methodology; formal analysis; writing—review and editing; supervision.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
ETHICS STATEMENT
Not applicable.
CONSENT TO PARTICIPATE
Not applicable.
SYSTEMATIC REVIEW PROTOCOL
A protocol was not prepared.
CONSENT FOR PUBLICATION
Not applicable.
Supporting information
Supporting Information S1
Supporting Information S2
Supporting Information S3
Supporting Information S4
Supporting Information S5
ACKNOWLEDGEMENTS
Not applicable.
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
DATA AVAILABILITY STATEMENT
The data presented in this review are included in the article and supplementary data files. Any additional data will be shared on reasonable request to the corresponding author (JB).
REFERENCES
- 1. van Gent, R. N. , Siem D., van Middelkoop M., van Os A. G., Bierma‐Zeinstra S. M. A., and Koes B. W.. 2007. “Incidence and Determinants of Lower Extremity Running Injuries in Long Distance Runners: A Systematic Review.” British Journal of Sports Medicine 41(8): 469–480. 10.1136/bjsm.2006.033548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hootman, Jennifer M. , Macera Carol A., Ainsworth Barbara E., Addy Cheryl L., Martin Malissa, and Blair Steven N.. 2002. “Epidemiology of Musculoskeletal Injuries Among Sedentary and Physically Active Adults.” Medicine & Science in Sports & Exercise 34(5): 838–844. 10.1097/00005768-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 3. Booth, Frank W. , Gordon Scott E., Carlson Christian J., and Hamilton Marc T.. 2000. “Waging War on Modern Chronic Diseases: Primary Prevention through Exercise Biology.” Journal of Applied Physiology 88(2): 774–787. 10.1152/jappl.2000.88.2.774. [DOI] [PubMed] [Google Scholar]
- 4. Huang, Yuchai , Li Liqing, Gan Yong, Wang Chao, Jiang Heng, Cao Shiyi, and Lu Zuxun. 2020. “Sedentary Behaviors and Risk of Depression: A Meta‐Analysis of Prospective Studies.” Translational Psychiatry 10(1): 26. 10.1038/s41398-020-0715-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chau, Josephine Y. , Grunseit Anne, Midthjell Kristian, Holmen Jostein, Holmen Turid Lingaas, Bauman Adrian E., and Van der Ploeg Hidde P.. 2015. “Sedentary Behaviour and Risk of Mortality from All‐Causes and Cardiometabolic Diseases in Adults: Evidence from the HUNT3 Population Cohort.” British Journal of Sports Medicine 49(11): 737–742. 10.1136/bjsports-2012-091974. [DOI] [PubMed] [Google Scholar]
- 6. Roddy, Edward , and Menz Hylton B.. 2018. “Foot Osteoarthritis: Latest Evidence and Developments.” Ther Adv Musculoskelet Dis 10(4): 91–103. 10.1177/1759720X17753337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Silbernagel, Karin Grävare , Hanlon Shawn, and Sprague Andrew. 2020. “Current Clinical Concepts: Conservative Management of Achilles Tendinopathy.” Journal of Athletic Training 55(5): 438–447. 10.4085/1062-6050-356-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Willy, Richard W. , Hoglund Lisa T., Barton Christian J., Bolgla Lori A., Scalzitti David A., Logerstedt David S., Lynch Andrew D., Snyder‐Mackler Lynn, and McDonough Christine M.. 2019. “Patellofemoral Pain.” Journal of Orthopaedic & Sports Physical Therapy 49(9): 1–95. 10.2519/jospt.2019.0302. [DOI] [PubMed] [Google Scholar]
- 9. van der Plas, A. , de Jonge S., de Vos R. J., van der Heide H. J. L., Verhaar J. A. N., Weir A., and Tol J. L.. 2012. “A 5‐year Follow‐Up Study of Alfredson's Heel‐Drop Exercise Programme in Chronic Midportion Achilles Tendinopathy.” British Journal of Sports Medicine 46(3): 214–218. 10.1136/bjsports-2011-090035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johanson, M. , Cooksey A., Hillier C., Kobbeman H., and Stambaugh A.. 2006. “Heel Lifts and the Stance Phase of Gait in Subjects with Limited Ankle Dorsiflexion.” Journal of Athletic Training 41: 159–165. [PMC free article] [PubMed] [Google Scholar]
- 11. Martin, Robroy L. , Davenport Todd E., Reischl Stephen F., McPoil Thomas G., Matheson James W., Wukich Dane K., McDonough Christine M., et al. 2014. “Heel Pain—Plantar Fasciitis: Revision 2014.” Journal of Orthopaedic & Sports Physical Therapy 44(11): 1–33. 10.2519/jospt.2014.0303. [DOI] [PubMed] [Google Scholar]
- 12. Chimenti, Ruth L. , Cychosz Chris C., Hall Mederic M., and Phisitkul Phinit. 2017. “Current Concepts Review Update: Insertional Achilles Tendinopathy.” Foot & Ankle International 38(10): 1160–1169. 10.1177/1071100717723127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Micheli, Lyle J. , and Ireland M. Lloyd. 1987. “Prevention and Management of Calcaneal Apophysitis in Children: An Overuse Syndrome.” Journal of Pediatric Orthopaedics 7(1): 34–38. 10.1097/01241398-198701000-00007. [DOI] [PubMed] [Google Scholar]
- 14. Lavery, Kyle P. , McHale Kevin J., Rossy William H., and Theodore George. 2016. “Ankle Impingement.” Journal of Orthopaedic Surgery and Research 11(1): 97. 10.1186/s13018-016-0430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rabusin, Chantel L. , Menz Hylton B., McClelland Jodie A., Tan Jade M., Whittaker Glen A., Evans Angela M., and Munteanu Shannon E.. 2019. “Effects of Heel Lifts on Lower Limb Biomechanics and Muscle Function: A Systematic Review.” Gait & Posture 69: 224–234. 10.1016/j.gaitpost.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 16. Hessas, S. , Behr M., Rachedi M., and Belaidi I.. 2018. “Heel Lifts Stiffness of Sports Shoes Could Influence Posture and Gait Patterns.” Science & Sports 33(2): 43–50. 10.1016/j.scispo.2017.04.015. [DOI] [Google Scholar]
- 17. Lee, Kawin K. W. , Ling Samuel K. K., and Yung Patrick S. H.. 2019. “Controlled Trial to Compare the Achilles Tendon Load during Running in Flatfeet Participants Using a Customized Arch Support Orthoses vs an Orthotic Heel Lift.” BMC Musculoskeletal Disorders 20(1): 535. 10.1186/s12891-019-2898-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang, Xianyi , and Li Bo. 2014. “Influence of In‐Shoe Heel Lifts on Plantar Pressure and Center of Pressure in the Medial‐Lateral Direction during Walking.” Gait & Posture 39(4): 1012–1016. 10.1016/j.gaitpost.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 19. Katoh, Y. , Chao E. Y. S., Morrey B. F., and Laughman R. K.. 1983. “Objective Technique for Evaluating Painful Heel Syndrome and its Treatment.” Foot and Ankle 3(4): 227–237. 10.1177/107110078300300410. [DOI] [PubMed] [Google Scholar]
- 20. Weinert‐Aplin, Robert A. , Bull Anthony M. J., and McGregor Alison H.. 2016. “Orthotic Heel Wedges Do Not Alter Hindfoot Kinematics and Achilles Tendon Force during Level and Inclined Walking in Healthy Individuals.” Journal of Applied Biomechanics 32(2): 160–170. 10.1123/jab.2015-0107. [DOI] [PubMed] [Google Scholar]
- 21. Moher, D. , Liberati A., Tetzlaff J., and Altman D. G.. 2009. “Preferred Reporting Items for Systematic Reviews and Meta‐Anyalyses: The PRISMA Statement.” BMJ 339(jul21 1): 2535. 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Merlin, Tracy , Weston Adele, and Tooher Rebecca. 2009. “Extending an Evidence Hierarchy to Include Topics Other Than Treatment: Revising the Australian 'levels of Evidence.” BMC Medical Research Methodology 9(1): 34. 10.1186/1471-2288-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vicenzino, Bill , de Vos R.‐Jan, Alfredson Hakan, Bahr Roald, Cook Jill L., Coombes Brooke K., Fu Siu Ngor, et al. 2020. “ICON 2019—International Scientific Tendinopathy Symposium Consensus: There Are Nine Core Health‐Related Domains for Tendinopathy (CORE DOMAINS): Delphi Study of Healthcare Professionals and Patients.” British Journal of Sports Medicine 54(8): 444–451. 10.1136/bjsports-2019-100894. [DOI] [PubMed] [Google Scholar]
- 24. Landorf, Karl B. , Keenan A.‐Maree, and Herbert Robert D.. 2006. “Effectiveness of Foot Orthoses to Treat Plantar Fasciitis: A Randomized Controlled Trial.” Archives of Internal Medicine 166(12): 1305–1310. 10.1001/archinte.166.12.1305. [DOI] [PubMed] [Google Scholar]
- 25. Munteanu, Shannon E. , Scott Lisa A., Bonanno Daniel R., Landorf Karl B., Pizzari Tania, Cook Jill L., and Menz Hylton B.. 2015. “Effectiveness of Customised Foot Orthoses for Achilles Tendinopathy: A Randomised Controlled Trial.” British Journal of Sports Medicine 49(15): 989–994. 10.1136/bjsports-2014-093845. [DOI] [PubMed] [Google Scholar]
- 26. Whittaker, Glen A. , Munteanu Shannon E., Menz Hylton B., Bonanno Daniel R., Gerrard James M., and Landorf Karl B.. 2019. “Corticosteroid Injection for Plantar Heel Pain: A Systematic Review and Meta‐Analysis.” BMC Musculoskeletal Disorders 20(1): 378. 10.1186/s12891-019-2749-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lim, Polly Q. X. , Lithgow Merridy J., Kaminski Michelle R., Landorf Karl B., Menz Hylton B., and Munteanu Shannon E.. 2023. “Efficacy of Non‐surgical Interventions for Midfoot Osteoarthritis: A Systematic Review.” Rheumatology International 43(8): 1409–1422. 10.1007/s00296-023-05324-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Higgins, J. , Savović J., Page M., Elbers R., and Sterne J.. 2023. “Chapter 8: Assessing Risk of Bias in a Randomized Trial.” version 6.4 In Cochrane Handbook for Systematic Reviews of Interventions, edited by Higgins J., Thomas J., Chandler J., Cumpston M., Li T., Page M. and Welch V.. Cochrane: (updated August 2023). [Google Scholar]
- 29. Sterne, Jonathan A. C. , Savović Jelena, Page Matthew J., Elbers Roy G., Blencowe Natalie S., Boutron Isabelle, Cates Christopher J., et al. 2019. “A Revised Tool for Assessing Risk of Bias in Randomized Trials.” BMJ 366: 4898. 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 30. Whittaker, Glen A. , Munteanu Shannon E., Menz Hylton B., Tan Jade M., Rabusin Chantel L., and Landorf Karl B.. 2018. “Foot Orthoses for Plantar Heel Pain: A Systematic Review and Meta‐Analysis.” British Journal of Sports Medicine 52(5): 322–328. 10.1136/bjsports-2016-097355. [DOI] [PubMed] [Google Scholar]
- 31. Higgins, J. , Li T., and Deeks J.. 2023. “Chapter 6: Choosing Effect Measures and Computing Estimates of Effect.” version 6.4 In Cochrane Handbook for Systematic Reviews of Interventions, edited by Higgins J., Thomas J., Chandler J., Cumpston M., Li T., Page M. and Welch V.. Cochrane: (updated August 2023). [Google Scholar]
- 32. Landorf, Karl B. , Radford Joel A., and Hudson Susie. 2010. “Minimal Important Difference (MID) of Two Commonly Used Outcome Measures for Foot Problems.” Journal of Foot and Ankle Research 3(1): 7. 10.1186/1757-1146-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lagas, Iris F. , van der Vlist Arco C., van Oosterom Robert F., van Veldhoven Peter L. J., Reijman Max, Verhaar Jan A. N., and de Vos R.‐Jan. 2021. “Victorian Institute of Sport Assessment‐Achilles (VISA‐A) Questionnaire‐Minimal Clinically Important Difference for Active People with Midportion Achilles Tendinopathy: A Prospective Cohort Study.” Journal of Orthopaedic & Sports Physical Therapy 51(10): 510–516. 10.2519/jospt.2021.10040. [DOI] [PubMed] [Google Scholar]
- 34. Landorf, Karl B. , and Radford Joel A.. 2008. “Minimal Important Difference: Values for the Foot Health Status Questionnaire, Foot Function Index and Visual Analogue Scale.” The Foot 18(1): 15–19. 10.1016/j.foot.2007.06.006. [DOI] [Google Scholar]
- 35. Tsze, Daniel S. , Hirschfeld Gerrit, von Baeyer Carl L., Bulloch Blake, and Dayan Peter S.. 2015. “Clinically Significant Differences in Acute Pain Measured on Self‐Report Pain Scales in Children.” Academic Emergency Medicine 22(4): 415–422. 10.1111/acem.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rabusin, Chantel L. , Menz Hylton B., McClelland Jodie A., Evans Angela M., Malliaras Peter, Docking Sean I., Landorf Karl B., Gerrard James M., and Munteanu Shannon E.. 2021. “Efficacy of Heel Lifts versus Calf Muscle Eccentric Exercise for Mid‐portion Achilles Tendinopathy (HEALTHY): A Randomised Trial.” British Journal of Sports Medicine 55(9): 486–492. 10.1186/s13047-019-0325-2. [DOI] [PubMed] [Google Scholar]
- 37. Turlik, Ma , Donatelli Tj, and Veremis Mg. 1999. “A Comparison of Shoe Inserts in Relieving Mechanical Heel Pain.” The Foot 9(2): 84–87. 10.1054/foot.1999.0522. [DOI] [Google Scholar]
- 38. Higgins, J. , Thomas J., Chandler J., Cumpston M., Li T., Page M., and Welch V.. 2019. Cochrane Handbook for Systematic Reviews of Interventions. (2nd ed.). Chichester, UK: John Wiley and Sons. [Google Scholar]
- 39. Schünemann, H. , Brożek J., Guyatt G. and Oxman A.. 2013. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. The GRADE Working Group: Updated October 2013 Available from www.guidelinedevelopment.org/handbook. [Google Scholar]
- 40. GRADEpro GDT . 2023. GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime. Available from www.gradepro.org.. [Google Scholar]
- 41. Clark, J. , and Percivall A.. 2000. “A Preliminary Investigation into the Effectiveness of the Homoeopathic Remedy, Ruta Graveolens, in the Treatment of Pain in Plantar Fasciitis.” Br J Pod 3: 81–85. [Google Scholar]
- 42. Lipton, J. , Flowers‐Johnson J., Bunnell M., and Carter L.. 2009. “The Use of Heel Lifts and Custom Orthotics in Reducing Self‐Reported Chronic Musculoskeletal Pain Scores.” AAOHN Journal 19: 15–21. [Google Scholar]
- 43. Perhamre, S. , Lundin F., Klassbo M., and Norlin R.. 2012. “A Heel Cup Improves the Function of the Heel Pad in Sever's Injury: Effects on Heel Pad Thickness, Peak Pressure and Pain.” Scandinavian Journal of Medicine & Science in Sports 22(4): 516–522. 10.1111/j.1600-0838.2010.01266.x. [DOI] [PubMed] [Google Scholar]
- 44. Shields, Nora . 2016. “Wait and See, Heel Raise and Eccentric Exercise May Be Equally Effective Treatments for Children with Calcaneal Apophysitis.” Journal of Physiotherapy 62(2): 112. 10.1016/j.jphys.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 45. Taylor, G. , and Pratt D.. 1997. “Viscolas Heel Orthoses in the Treatment of the Painful First Metatarsophalangeal Joint.” British Journal of Podiatric Medicine 9: 20–23. [Google Scholar]
- 46. Wibowo, Dwi Basuki , Harahap Rudiansyah, Widodo Achmad, Haryadi Gunawan Dwi, and Ariyanto Mochammad. 2017. “The Effectiveness of Raising the Heel Height of Shoes to Reduce Heel Pain in Patients with Calcaneal Spurs.” Journal of Physical Therapy Science 29(12): 2068–2074. 10.1589/jpts.29.2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alfaro‐Santafé, Javier , Gómez‐Bernal Antonio, Lanuza‐Cerzócimo Carla, Alfaro‐Santafé J.‐Víctor, Pérez‐Morcillo Aitor, and Almenar‐Arasanz A.‐Jesús. 2021. “Effectiveness of Custom‐Made Foot Orthoses vs. Heel‐Lifts in Children with Calcaneal Apophysitis (Sever’s Disease): A CONSORT‐Compliant Randomized Trial.” Children 8(11): 1–10. 10.3390/children8110963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gupta, Ravi , Malhotra Anubhav, Masih Gladson David, Khanna Tanu, Kaur Harsimranjit, Gupta Parmanand, and Kashyap Shweta. 2020. “Comparing the Role of Different Treatment Modalities for Plantar Fasciitis: A Double Blind Randomized Controlled Trial.” Indian Journal of Orthopaedics 54(1): 31–37. 10.1007/s43465-019-00038-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. James, Alicia M. , Williams Cylie M., and Haines Terry P.. 2016. “Effectiveness of Footwear and Foot Orthoses for Calcaneal Apophysitis: A 12‐month Factorial Randomised Trial.” British Journal of Sports Medicine 50(20): 1268–1275. 10.1136/bjsports-2015-094986. [DOI] [PubMed] [Google Scholar]
- 50. Lowdon, Alison , Bader Daniel L., and Mowat Alastair G.. 1984. “The Effect of Heel Pads on the Treatment of Achilles Tendinitis: A Double Blind Trial.” The American Journal of Sports Medicine 12(6): 431–435. 10.1177/036354658401200605. [DOI] [PubMed] [Google Scholar]
- 51. Pfeffer, Glenn , Bacchetti Peter, Deland Johnathan, Lewis Ai, Anderson Robert, Davis William, Alvarez Richard, et al. 1999. “Comparison of Custom and Prefabricated Orthoses in the Initial Treatment of Proximal Plantar Fasciitis.” Foot & Ankle International 20(4): 214–221. 10.1177/107110079902000402. [DOI] [PubMed] [Google Scholar]
- 52. Wiegerinck, Johannes I. , Zwiers Ruben, Sierevelt Inger N., van Weert Henk C. P. M., van Dijk C. Niek, and Struijs Peter A. A.. 2016. “Treatment of Calcaneal Apophysitis: Wait and See versus Orthotic Device versus Physical Therapy: A Pragmatic Therapeutic Randomized Clinical Trial.” Journal of Pediatric Orthopaedics 36(2): 152–157. 10.1097/BPO.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 53. de Vos, R.‐Jan , van der Vlist Arco C., Zwerver Johannes, Meuffels Duncan Edward, Smithuis Frank, van Ingen Ronald, van der Giesen Florus, et al. 2021. “Dutch Multidisciplinary Guideline on Achilles Tendinopathy.” British Journal of Sports Medicine 55(20): 1125–1134. 10.1136/bjsports-2020-103867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Michie, Susan , van Stralen Maartje M., and West Robert. 2011. “The Behaviour Change Wheel: A New Method for Characterising and Designing Behaviour Change Interventions.” Implementation Science 6(1): 42. 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Johnston, Bradley C. , Ebrahim Shanil, Carrasco‐Labra Alonso, Furukawa Toshi A., Patrick Donald L., Crawford Mark W., Hemmelgarn Brenda R., Schunemann Holger J., Guyatt Gordon H., and Nesrallah Gihad. 2015. “Minimally Important Difference Estimates and Methods: A Protocol.” BMJ Open 5(10): e007953. 10.1136/bmjopen-2015-007953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Donley, Brian G. , Moore Tim, Sferra James, Gozdanovic Jon, and Smith Richard. 2007. “The Efficacy of Oral Nonsteroidal Anti‐inflammatory Medication (NSAID) in the Treatment of Plantar Fasciitis: A Randomized, Prospective, Placebo‐Controlled Study.” Foot & Ankle International 28(1): 20–23. 10.3113/FAI.2007.0004. [DOI] [PubMed] [Google Scholar]
- 57. Boutron, Isabelle , Tubach Florence, Giraudeau Bruno, and Ravaud Philippe. 2004. “Blinding Was Judged More Difficult to Achieve and Maintain in Nonpharmacologic Than Pharmacologic Trials.” Journal of Clinical Epidemiology 57(6): 543–550. 10.1016/j.jclinepi.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 58. Blasi, Zelda Di , Harkness Elaine, Ernst Edzard, Georgiou Amanda, and Kleijnen Jos. 2001. “Influence of Context Effects on Health Outcomes: A Systematic Review.” Lancet 357(9258): 757–762. 10.1016/S0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- 59. Zhang, Weiya , and Doherty Michael. 2018. “Efficacy Paradox and Proportional Contextual Effect (PCE).” Clinical Immunology 186: 82–86. 10.1016/J.CLIM.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 60. Morrison, Andra , Polisena Julie, Husereau Don, Moulton Kristen, Clark Michelle, Fiander Michelle, Mierzwinski‐Urban Monika, Clifford Tammy, Hutton Brian, and Rabb Danielle. 2012. “The Effect of English‐language Restriction on Systematic Review‐Based Meta‐Analyses: A Systematic Review of Empirical Studies.” International Journal of Technology Assessment in Health Care 28(2): 138–144. 10.1017/S0266462312000086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Supporting Information S2
Supporting Information S3
Supporting Information S4
Supporting Information S5
Data Availability Statement
The data presented in this review are included in the article and supplementary data files. Any additional data will be shared on reasonable request to the corresponding author (JB).


