Abstract
Background
Limitations exist with current ACLR functional testing assessments that may be mitigated by including single-leg multi-directional testing.
Hypothesis/Purpose
To compare Anterior Cruciate Ligament-Return to Sport after Injury Scale (ACL-RSI) scores, limb symmetry index (LSI) of the single-leg vertical jump (SLVJ), single-leg medial rotation hop (SLMRH), single-leg lateral hop (SLLH), and isokinetic quadriceps strength between participants with an ACLR and healthy controls and assess predictors of quadriceps strength asymmetry. It was hypothesized that ACL-RSI scores and LSIs for all tests would differ between ACLR and healthy control groups and within the ACLR group a strong correlation would exist between all outcome measures and quadriceps strength.
Study Design
Cross-Sectional Study
Methods
Twenty-six participants with an ACLR (median 13 months after surgery) and twenty-six matched healthy controls were recruited to participate in this study. Performance was assessed via SLVJ, SLMRH, SLLH, and isokinetic quadriceps strength. Between-group comparisons were made with independent t-tests and Mann-Whitney U test. Within the ACLR group, bivariate correlation and multivariate regression analysis were performed to assess the relationship between the outcome measures and quadriceps strength asymmetry.
Results
Significant between-limb differences were only identified in the ACLR group (p< 0.05): SLVJ LSI: 88.5%, SLMRH LSI: 93.6%, SLLH LSI: 92.7%, quadriceps strength LSI 80.9% - 83.9%, which were significantly lower (p <0.05) than the healthy control group. Within the ACLR group, a moderate-strong significant (p < 0.05) correlations existed with quadriceps strength and SLVJ (r=0.44-0.65), SLMRH (r =0.43-0.83), and SLLH (r=0.54-0.63); while ACL-RSI had a weak non-significant (p > 0.05) correlation with quadriceps strength (r= 0.12-0.30).
Conclusion
Single-leg multidirectional test LSIs were less in ACLR participants than matched healthy controls and all were directly related to quadriceps strength. Psychological readiness to return to sport was not related to quadriceps strength.
Keywords: Anterior Cruciate Ligament Reconstruction, Hop Tests, Psychological Readiness, Quadriceps Strength
INTRODUCTION
Anterior cruciate ligament (ACL) tears are devastating injuries to both civilian athletes and military service members.1 Due to the physical occupation demands military service members have a ten times greater incidence of ACL injuries than the general population.2 Most athletes and military service members with ACL tears elect to undergo anterior cruciate ligament reconstruction (ACLR).3 Despite evolving surgical procedures and post-operative rehabilitation, 2 -38% of athletes rupture their ACLR graft,4–6 up to 19% have a contralateral ACL rupture,7 and only 55% return to competitive sport.8 Military personnel have similar challenges as only 47% of service members return to full duty status after an ACLR.9
A crucial decision point during ACLR rehabilitation is determining when to return the athlete to sport or the service member to full military duty. Numerous factors are incorporated into this decision including type of sport/military occupation, prior medical history, and time from surgery, as well as psychological readiness, strength, and functional objective assessments.10 These assessments are essential as post-ACLR patients may have neuromuscular deficits for years11,12 and up to 24% of athletes do not return to sports due to fear of re-injury.13
Quadriceps strength is a standard post-ACLR assessment with isokinetic dynamometer being the gold standard for assessing quadriceps strength.14 Athletes with symmetric quadriceps strength after ACLR have a decreased injury risk.15 As isokinetic dynamometers are expensive, clinicians frequently utilize field expedient single-leg sagittal hops (SLSH) solely or in addition to quadriceps strength assessments to quantify lower extremity strength and functional asymmetry.16,17 Test results are typically displayed as a ratio of the operated limb to the non-operated limb, referred to as a limb symmetry index (LSI). A commonly employed LSI cutoff is ≥ 90% before an athlete may be cleared to return to sports,15,18 Nine months after ACLR surgery quadriceps strength LSI can range from 37% to 93%.19–22 and SLSH LSI can range from 52% to 98%.19,22,23
Clinicians commonly utilize patient-reported outcomes such as the Anterior Cruciate Ligament-Return to Sport After Injury (ACL-RSI) to assess psychological return to sport readiness after ACLR.24 The ACL-RSI has been explicitly designed for and validated within an ACLR population24 with scores ≥65 indicating a favorable prognosis to return to the same level of sports two years after ACLR.25
Several limitations exist with the current ACLR functional assessments. Only 23-43% of athletes pass the test batteries post-ACLR and passing may not be associated with lower re-injury rates.17 Furthermore, Webster et al. reported an increased risk of a contralateral ACL injury for those who passed return to sport testing.16 The commonly utilized SLSH may overestimate quadriceps strength and lower extremity symmetry.19–21,26,27 Due to high re-injury rates, ambiguous validity of return to sport test batteries, and individual test limitations, additional research is needed to optimize ACLR functional assessments.
Recent research has suggested that multidirectional single-leg testing such as the single-leg vertical jump (SLVJ), single-leg medial rotation hop (SLMRH), and single-leg lateral hop (SLLH) warrant inclusion in ACLR return to sport assessments. The SLVJ has a greater association with quadriceps strength than the SLSH,19,23 identifies functional impairments in ACLR patients one year from surgery,28 and correlates with the ACL-RSI.29 The SLMRH can identify asymmetry in ACLR patients six months after surgery.30 The SLLH can identify asymmetry in ACLR patients twelve months from surgery,31 and is associated with quadriceps strength.32 It remains unknown whether all of these single-leg multidirectional tests are associated with validated confidence or quadriceps strength measures.
The purpose of this study was to compare ACL-RSI scores and LSIs of the SLVJ, SLMRH, SLLH, and quadriceps strength between two groups of United States Military Academy (USMA) Cadets: those with an ACLR within 10 to 38 months and a healthy control group. The time from ACLR was chosen to be consistent with previous research conducted at our institute. The second aim was to examine if relationships exist among quadriceps strength LSI and ACL-RSI, and LSIs of the SLVJ, SLMRH, and SLLH in USMA cadets with a recent ACLR. It was hypothesized that ACL-RSI scores and LSIs for all tests would differ between the ACLR and healthy control groups. It was also hypothesized that within the ACLR group, a strong correlation would exist between quadriceps strength LSI and SLVJ LSI, SLMRH LSI, SLLH LSI, and ACL-RSI.
METHODS
Study Design
This was a case-control study among United States Military Academy (USMA) Cadets. A-priori power analysis using G power software (Heinrich-Heine Universität, Düsseldorf, Germany) indicated a necessary sample size of twenty-six participants in both groups for the first aim (effect size = 0.7 from prior research conducted by the researchers’ institute,33 α = 0.05, power= 0.8, two-tailed). For the second aim, twenty-six ACLR participants were required (effect size = 0.39 from prior research conducted by the researchers’ institute,33 α = 0.05, four predictors, power = 0.8, two-tailed). The Naval Medical Center Portsmouth Institutional Review Board approved this study. All participants provided written informed consent before data collection.
Participants
USMA Cadets with an ACLR prior to or after matriculation to USMA were invited to participate. All participants in the ACLR group had completed or were finishing their rehabilitation and were cleared for testing. ACLR group inclusion criteria consisted of ages 18-27 years (17 years if an emancipated Cadet), fluent in English, a history of a unilateral ACLR within 10 to 38 months to be consistent with prior research conducted at the researachers’ institute,33 and cleared by a medical provider to perform jump, hop, and strength testing. Potential participants were excluded if they had: a history of bilateral ACLR, any lower extremity surgery other than concomitant ACLR procedures (i.e. meniscal repair), a lower extremity injury within the prior six months, were currently pregnant, or had a medical condition that would preclude them from participating.
Healthy control group members were matched based on biological sex, height, weight, and collegiate athletic skill level to the ACLR participants. Healthy control group inclusion criteria consisted of ages 18-27 years (17 if an emancipated Cadet) and fluent in English. Participants were excluded if they had: a history of a lower extremity injury within six months, any lower extremity surgery, were currently pregnant, or had a medical condition that would preclude them from participating.
Procedure
Participants wore their own athletic clothes and athletic shoes. All data were collected on a single visit. After consenting, all participants completed intake documentation: demographic information, collegiate athletic skill level, surgical information, and the ACL-RSI. Before testing, all participants performed a warm-up on a stationary bicycle for five minutes at a low, self-determined intensity.34 They were also offered an optional non-standardized stretching or foam rolling period of five minutes.34 Participants completed testing in a standardized order ([1] SLVJ, [2] SLMRH, [3] SLLH, and [4] isokinetic quadriceps strength testing). Before performing the SLVJ, SLMRH, and SLLH, the examiner provided verbal instructions on how to perform the task. Alternating between limbs, each participant performed three practice repetitions per limb, and then three successful trials per limb. Each test commenced with the non-operated or non-dominant limb. The participant’s dominant limb was defined by their preferred limb to kick a ball.35 For the SLVJ, SLLH, and SLMRH a thirty-second rest period was provided between test repetitions.36
Anterior Cruciate Ligament-Return to Sport After Injury (ACL-RSI)
The ACL-RSI is a twelve-question questionnaire scored from 0 to 100.37 Greater scores indicate a positive psychological response for sport resumption following ACLR.24 Nine months after surgery, ACLR patients typically have an ACL-RSI score of 50-7229,38 and scores <47 indicate a decreased likelihood of returning to sports.24,38
Single-leg vertical jump (SLVJ)23
The SLVJ was performed on the commercially available Just Jump System (JPS, Probotics Inc, Huntsville, AL, USA). The Just Jump system is a portable, inexpensive, valid, and reliable tool (intrasession intraclass correlation coefficient [ICC]reliability of 0.90-0.92 compared to a three-camera motion analysis system)39 that calculates jump height from flight time between foot contacts.40 Participants were instructed to stand on a single-leg, perform a maximum countermovement single-leg vertical jump, use their arms when jumping, and land on the jumping leg. Tests were excluded and reperformed if the participant excessively flexed their hips, any part of their foot landed off the mat, lost their balance, or their hands or the contralateral limb touched the floor.
Single-leg medial rotation hop (SLMRH)30
The SLMRH is a reliable assessment (ICC reliability of 0.93- 0.95) of functional performance following ACLR.30 Participants were instructed to stand on a single-leg with the medial aspect of their foot perpendicular to the direction of travel, perform a maximum hop while rotating 90° in the medial direction, allowing use of their arms when performing the hop, and land on the jumping leg. The distance was measured from the medial aspect of the foot on the starting line to the participant’s toes at landing. The test was excluded and reperformed if the participant lost their balance, their hands or the contralateral limb touched the floor, or > 10° difference in the direction the participant’s foot should be pointing.
Single-leg lateral hop (SLLH)31
The SLLH is also a reliable assessment (ICC reliability of 0.91-0.95)41 of functional performance after ACLR.31 Participants were instructed to stand on a single-leg with the lateral aspect of their foot perpendicular to the hop direction, perform a maximum single-leg lateral hop, use their arms when performing the hop, and land on the jumping leg. The distance was measured from the lateral aspect of the foot on the starting line to the lateral aspect of the participant’s foot at landing. The test was excluded and reperformed if the participants lost their balance, either of their hands or the contralateral limb touched the floor, or > 10° difference in the direction the participant’s foot should be pointing.
Quadriceps isokinetic strength testing
Maximum isokinetic strength testing was performed with the Cybex HUMAC dynamometer Model 502140 (CSMi, Stoughton, MA, USA) or Biodex dynamometer (Biodex Medical Systems, Shirley, NY, USA). Both provide reliable assessments of quadriceps strength and present similar values (ICC reliability 0.88-0.92).42 Participants were seated and secured with straps over their torso and thigh, hips flexed to approximately 90°, knees flexed to approximately 90°, femoral condyles of the tested limb aligned with the rotation axis of the torque meter, and straps over their legs. For familiarization, the participants performed three submaximal knee extension/flexion repetitions. Participants rested for one minute after familiarization and between each strength test which consisted of five maximum consecutive concentric contractions of knee extension and flexion. Isokinetic strength was tested at angular velocities of 60°, 180°, and 300° per second. Participants were provided with standardized vigorous verbal encouragement.
Statistical Analysis
The final analysis utilized the average score (height or distance) for each hop/jump test and the maximum peak quadriceps torque for each isokinetic angular velocity. Quadriceps torque was normalized to the participant’s body mass. For ACLR participants, an LSI was calculated for each test with the following formula43:
LSI was calculated for healthy participants with the following formula for each test44:
Normality was assessed using the Shapiro-Wilk test. The group differences in demographic data, single-leg multidirectional tests, ACL-RSI, and quadriceps strength were analyzed using chi-square, Fischer’s exact test, independent t-test, or Mann-Whitney U test with two tails. Pearson’s product correlation coefficients were calculated to investigate association between time from surgery and all LSIs for SLVJ, SLMRH, SLLH, and quadriceps strength. Spearman correlation was calculated to investigate association between the ACL-RSI and the strength and functional assessments. The strength of associations was determined as weak: < 0.3, moderate: ≥ 0.3 to < 0.5: and strong ≥ 0.5.45 A priori, it was determined to enter each independent variable (ACL-RSI, SLVJ LSI, SLMRH LSI, and SLLH LSI) with the dependent variable being quadriceps strength (for each angular velocity) into multivariable backward stepwise linear regression models. Multicollinearity and model diagnostics were assessed for each final model. α = 0.05 was used for all statistical tests. All statistical analyses were performed with SPSS software (version 28.0.1.1 for Windows; SPSS, Chicago, IL, USA).
RESULTS
Participant characteristics are presented in Table 1. No significant differences were found in biological sex, collegiate athletic skill, age, height, weight, and body mass index between the ACLR and healthy control groups. The median time from surgery for the ACLR group was 13.0 months.
Table 1. Participant characteristics.
| ACLR (n=26) |
Control (n =26) |
p value | |
|---|---|---|---|
| Sex (male/female) | 14/12 | 14/12 | 1.00 |
| Activity Level | |||
| Intramurals Athletes | 12 | 12 | 0.29 |
| Club Athletes | 3 | 7 | |
| NCAA Athletes | 11 | 7 | |
| Age, years (mean ± SD) | 20.7 ± 1.4 | 21.3 ± 1.6 | 0.23 |
| Height, m (mean ± SD) | 1.72 ± 0.07 | 1.73 ± 0.08 | 0.64 |
| Weight, kg (mean ± SD) | 74.6 ± 9.2 | 75.1 ± 9.9 | 0.84 |
| BMI (mean ± SD) | 25.2 ± 2.8 | 25.3 ± 1.7 | 0.96 |
| Time from Surgery, months (median, interquartile range) | 13.0 (9.8) | N/A | N/A |
| Injured dominant limb | 11 | N/A | N/A |
| Autograft Type | 16 QT, 8 BTB, 2 HS | N/A | N/A |
| Meniscus Repair (Yes) | 16 | N/A | N/A |
Abbreviations: ACLR, Anterior Cruciate Ligament Reconstruction; SD, standard deviation; BMI, body mass index; BTB, bone-patellar tendon-bone autograft; HS, hamstring autograft; NCAA, National Collegiate Athletic Association; QT quadriceps tendon autograft
Functional and isokinetic quadriceps testing outcomes for participants in both groups are presented in Table 2. For the ACLR group, the surgical limb scored significantly (p< 0.001) less than the non-surgical limb for all single-leg multidirectional and strength tests. No significant between-limb differences were identified within the healthy control group. The healthy control group had significantly greater ACL-RSI scores (p <0.001) and greater limb symmetry on the SLVJ (p < 0.001), SLMRH (p= 0.016), SLLH (p< 0.001), and quadricep strength (p<0.05) than the ACLR group. The non-surgical limb for the ACLR group was stronger compared to the non-dominant limb of the healthy control group but was not statistically significantly different (p> 0.05). Sub-group analysis within the ACLR group for time from surgery, athletic group, gender, graft type, and meniscal procedure did not identify a significant difference between sub-groups.
Table 2. Anterior cruciate ligament return to sport injury scale, single-leg multidirectional tests, and quadriceps strength results.
| ACLR (n= 26) (mean ± SD) |
≥90% LSI, ACLR n (%) | Control (n =26) (mean ± SD) |
p value | |
|---|---|---|---|---|
| ACL-RSI Score | 66.6 ± 17.0 | 97.9 ± 4.2 | < 0.001 | |
| SLVJ | ||||
| LSI (%) | 88.5 ± 11.6 | 13 (50%) | 98.4 ± 9.0 | < 0.001 |
| Surgical/Dominant Limb (cm) | 28.0 ± 6.7 | 30.6 ± 5.8 | ||
| Non-surgical/Non-Dominant Limb (cm) | 31.6 ± 6.9 | 30.2 ± 6.6 | ||
| SLMRH | ||||
| LSI (%) | 93.6 ± 9.0 | 20 (77%) | 98.9 ± 6.4 | 0.016 |
| Surgical/Dominant Limb (cm) | 153.6 ± 29.9 | 165.2 ± 30.7 | ||
| Non-surgical/Non-Dominant Limb (cm) | 164.4 ± 32.0 | 163.1 ± 29.6 | ||
| SLLH | ||||
| LSI (%) | 92.7 ± 10.6 | 17 (65%) | 101.8 ± 7.0 | <0.001 |
| Surgical/Dominant Limb (cm) | 116.4 ± 26.4 | 122.2 ± 29.6 | ||
| Non-surgical/Non-Dominant Limb (cm) | 125.7 ± 26.1 | 123.7 ± 28.3 | ||
| Extension 60º/sec | ||||
| LSI (%) | 80.9 ± 26.5 | 11 (42%) | 98.5 ± 15.8 | 0.006 |
| Surgical/Dominant Limb (Nm/kg) | 1.8 ± 0.5 | 2.2 ± 0.5 | ||
| Non-surgical/Non-Dominant Limb (Nm/kg) | 2.3 ± 0.5 | 2.2 ± 0.7 | ||
| Extension 180º/sec | ||||
| LSI (%) | 82.5 ± 17.8 | 9 (35%) | 93.7 ± 2.0 | 0.035 |
| Surgical/Dominant Limb (Nm/kg) | 1.3 ± 0.4 | 1.4 ± 0.4 | ||
| Non-surgical/Non-Dominant Limb (Nm/kg) | 1.5 ± 0.4 | 1.3 ± 0.4 | ||
| Extension 300º/sec | ||||
| LSI (%) | 83.9 ± 28.3 | 8 (31%) | 102.6 ± 23.9 | 0.002 |
| Surgical/Dominant Limb (Nm/kg) | 0.9 ± 0.4 | 1.0 ± 0.4 | ||
| Non-surgical/Non-Dominant Limb (Nm/kg) | 1.1 ± 0.4 | 0.9 ± 0.3 |
Abbreviations: ACL-RSI, Anterior Cruciate Ligament-Return to Sport after Injury; ACLR, anterior cruciate ligament reconstruction; LSI, limb symmetry index; SLLH, single-leg lateral hop; SLMRH, single-leg medial rotation hop; SLVJ, single-leg vertical jump
Correlation coefficients between the ACL-RSI, single-leg multidirectional test LSI, and quadriceps strength LSI for the ACLR group are shown in Table 3. The SLVJ LSI (r: 0.44-0.67) (Figure 1), SLMRH LSI (r values range from 0.43-0.83) (Figure 2), and SLLH LSI (r: 0.54-0.63) (Figure 3) all had a significant positive moderate-strong correlation with quadriceps strength LSI (p< 0.05). ACL-RSI did not have a significant correlation with quadriceps strength LSI. Time from surgery had a moderate-strong significant correlation with quadriceps strength LSI (r: 0.41-0.60) (p<0.05).
Table 3. Correlation coefficients (ACLR group).
| Time from Surgery | ACL-RSI | SLVJ | SLMRH | SLLH | Extension 60º/sec | Extension 180º/sec | Extension 300º/sec | ||
|---|---|---|---|---|---|---|---|---|---|
| Time from Surgery | 1 | ||||||||
| ACL-RSI | 0.10 | 1 | |||||||
| SLVJ | 0.25 | 0.20 | 1 | ||||||
| SLMRH | 0.37 | 0.07 | 0.86** | 1 | |||||
| SLLH | 0.25 | 0.08 | 0.81** | 0.73** | 1 | ||||
| Extension 60º/sec | 0.45* | 0.12 | 0.67** | 0.83** | 0.54* | 1 | |||
| Extension 180º/sec | 0.60** | 0.30 | 0.60** | 0.68** | 0.63** | 0.77** | 1 | ||
| Extension 300º/sec | 0.41* | 0.26 | 0.44* | 0.43* | 0.56* | 0.56* | 0.73** | 1 | |
Pearson correlation coefficients, except for ACL-RSI, which are Spearman correlations
Abbreviations: ACL-RSI, Anterior Cruciate-Ligament Return to Sport after Injury; LSI, limb symmetry index; SLLH, single-leg lateral hop; SLMRH, single-leg medial rotation hop; SLVJ, single-leg vertical jump
*Correlation is significant at the 0.05 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed)
Figure 1. Scatterplot between single-leg vertical jump (SLVJ) limb symmetry index (LSI) and quadriceps extension 60º/sec LSI (ACLR group).
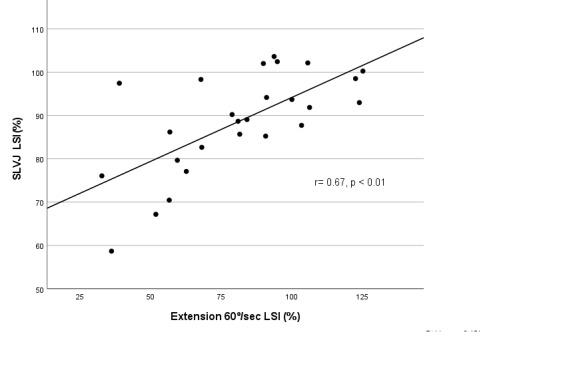
Figure 2. Scatterplot between single-leg medial rotation (SLMRH) limb symmetry index (LSI) and quadriceps extension 60º/sec LSI (ACLR group).
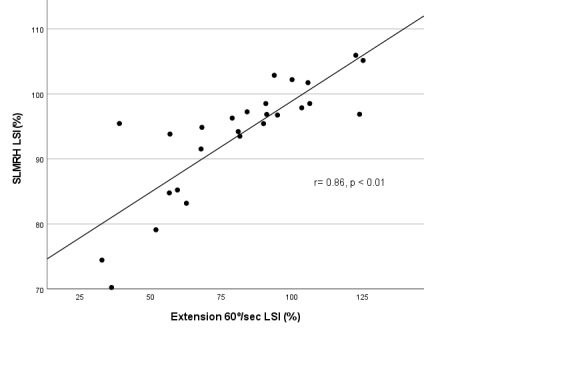
Figure 3. Scatterplot between single-leg lateral hop (SLLH) limb symmetry index (LSI) and quadriceps extension 60º/sec LSI (ACLR group).
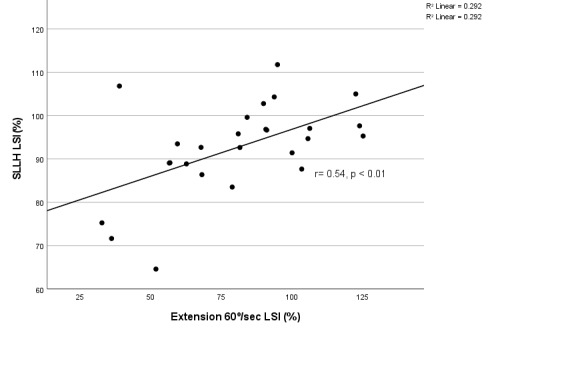
Table 4 displays the results of the multiple regression analysis. A priori (Model 1) only the ACL-RSI, SLVJ LSI, SLMRH LSI, and SLLH LSI were entered into the backwards regression analysis for each quadriceps isokinetic angular velocity LSI. As a significant correlation exists between time from surgery and quadriceps strength LSI, the analysis was repeated with time from surgery as an additional factor (Model 2). For Model 1, only one variable was retained (SLMRH LSI or SLLH LSI) for each isokinetic velocity LSI, accounting for 31.6% to 68.2% of the model variance. For Model 2 there was no change for extension 60º/sec LSI; however, for extension 180º/sec LSI and 300 º/sec LSI time since from surgery increased the explained variance from 46.7% to 57.7% and 31.6% to 62.9%.
Table 4. Backwards linear regression analysis to predict quadriceps strength limb symmetry index.
| Dependent Variable | Model | Retained Variable(s) | R2 | Beta | p value |
|---|---|---|---|---|---|
| Extension 60º/sec LSI | 1 | SLMRH LSI | 68.2% | 2.43 | < 0.001 |
| 2 | SLMRH LSI | 68.2% | 2.43 | < 0.001 | |
| Extension 180º/sec LSI | 1 | SLMRH LSI | 46.7% | 1.35 | < 0.001 |
| 2 | SLMRH LSI | 57.7% | 1.06 | < 0.001 | |
| Time From Surgery | 0.98 | ||||
| Extension 300º/sec LSI | 1 | SLLH LSI | 31.6% | 1.50 | 0.003 |
| 2 | SLLH LSI | 62.9% | 1.30 | < 0.001 | |
| Time From Surgery | 1.13 |
Model 1 variables: ACL-RSI, SLVJ, SLMRH, SLLH
Model 2 variables: Time from Surgery, ACL-RSI, SLVJ, SLMRH, SLLH
Abbreviations: ACL-RSI, Anterior Cruciate Ligament-Return to Sport after Injury; LSI, limb symmetry index; SLLH, single-leg lateral hop; SLMRH, single-leg medial rotation hop; SLVJ, single-leg vertical jump
Only four ACLR participants achieved ≥ 90% LSI on all tests. The proportion of ACLR participants who achieved the ≥ 90% LSI cutoff was greater for the single-leg multidirectional tests than for the quadriceps strength tests. Table 5 displays the results of the SLVJ LSI and SLMRH LSI compared to the reference standard of quadriceps extension 60º/sec with ≥ 90% LSI. Both tests over-estimated quadriceps strength symmetry; however, the SLVJ only had four false-negatives for quadriceps strength symmetry compared to nine for the SLRMH. This contributes to the greater sensitivity in detecting quadriceps strength asymmetry with the SLVJ (73.3%) compared to the SLMRH (40.0%) (Table 6).
Table 5. Relationship between quadriceps extension 60º/sec limb symmetry index (LSI), single-leg vertical jump, and single-leg medial rotation hop LSI with cutoff of 90% LSI.
| Extension 60º/sec LSI | Extension 180º/sec LSI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| < 90% | ≥ 90% | Sum | < 90% | ≥ 90% | Sum | |||||
| SLVJ LSI | < 90% | 11 | 2 | 13 | SLMRH LSI | < 90% | 6 | 0 | 6 | |
| ≥ 90% | 4 | 9 | 13 | ≥ 90% | 9 | 11 | 20 | |||
| Sum | 15 | 11 | 26 | Sum | 15 | 11 | 26 | |||
| p =0.015 | p=0.017 | |||||||||
Abbreviations: LSI, limb symmetry index; SLMRH, single-leg medial rotation hop; SLVJ, single-leg vertical jump
Table 6. Diagnostic accuracy of single-leg vertical jump and single-leg medial rotation hop to predict quadriceps strength at 60 deg/sec limb symmetry > 90%.
| Sensitivity | Specificity | |
|---|---|---|
| SLVJ LSI | 73.3% | 81.8% |
| SLMRH LSI | 40.0% | 100.0% |
Abbreviations: LSI, limb symmetry index; SLMRH, single-leg medial rotation hop; SLVJ, single-leg vertical jump
DISCUSSION
This study assessed the ability of the SLVJ, SLMRH, SLLH, and quadriceps strength to detect single-leg asymmetries between ACLR participants and healthy controls. The second aim examined the relationship between ACL-RSI, SLVJ LSI, SLMRH LSI, and SLLH LSI to quadriceps strength LSIs. The results partially confirmed the hypotheses. The ACL-RSI, SLVJ, SLMRH, SLLH, and quadriceps strength testing differentiated between ACLR participants and healthy controls; however, only the SLVJ LSI, SLMRH LSI, and SLLH LSI were associated with quadriceps strength asymmetry. Functional assessments consistently overestimate the strength present in the ACLR participants. In the regression analysis, time from surgery and the SLMRH LSI or SLLH LSI were the only retained factors to predict quadriceps strength asymmetry when accounting for the other variables. This is the first study to assess the association between the SLMRH and quadriceps strength asymmetry and identify single-leg multidirectional asymmetries in a military population after an ACLR. Additionally, these results contribute to the overall knowledge of single-leg multidirectional tests.
Single-leg hop and jump asymmetries were identified in the ACLR participants (median 13 months from surgery): SLVJ LSI of 88.5%, SLMRH LSI of 93.6%, and SLLH LSI of 92.7%. These results are consistent with prior ACLR research that identified an SLVJ LSI of 83.4%-90.4%,19,23,29,31 SLMRH LSI of 86.6%,30 and SLLH LSI of 82.2%-87.5%.31,46 Those results are similar to the current results despite several study design differences: most studies had ACLR participants only with HS autografts while only two (8%) of the ACLR participants in the current study had an HS autograft and most prior research had subjects six to nine months compared to the current study that had a median time of 13 months from surgery.19,29–31,46,47 The ability of the SLVJ, SLMRH, and SLLH to identify single-leg asymmetries in ACLR patients up to 38 months from surgery and with different graft types indicates that these tests warrant consideration as part of ACLR functional testing batteries.
Only four of the twenty-six ACLR participants (15%) achieved an LSI threshold of at least 90% for all strength and functional tests. A greater proportion of ACLR participants achieved a 90% LSI for the strength than the functional tests; however, the SLVJ had a greater diagnostic ability to rule out quadriceps asymmetry than the SLMRH (sensitivity of 73.3% vs 40.0%). The results of the current study are consistent with a meta-systematic review that identified that only 23% of individuals could pass the test batteries with similar LSI thresholds.16 The finding that ACLR participants have greater single-leg functional than quadriceps strength symmetry is consistent with prior research.46,48,49 This study is the first to investigate this for a greater range of isokinetic velocities and with three single-leg multi-directional movements.
Following ACLR, quadriceps muscle atrophy is common,50 therefore a goal of ACLR rehabilitation is to improve quadriceps strength which may reduce the risk of re-injury.15 As most clinicians do not possess expensive dynamometers51 they must rely upon other assessments such as single-leg hops to identify and quantify quadriceps strength asymmetry.16 Moderate -strong correlations (p > 0.05) were identified between quadriceps strength asymmetry and the single-leg multidirectional tests, which explain up to 68% of quadriceps strength asymmetry variance. When time from surgery was included in the regression analysis, the explained variance increased by another 10.0-31.3% for the faster quadriceps isokinetic velocities. The results are consistent with prior research identifying a moderate-strong correlation between SLVJ height and quadriceps strength19,29,48,52 and a significant correlation between SLLH and quadriceps strength.46 Within our study, ACLR participants with QT autographs tended to have weaker quadriceps strength compared to ACLR participants with BTB grafts (86.9% compared to 74.7% for quadriceps isokinetic velocity of 60 º/sec, p =0.351). This is consistent with observations from the authors’ clinic that patients with QT often have persistent quadriceps activation deficits. After ACLR, patients with QT autografts may have quadriceps neuromuscular inhibition compared to those with HS and BTB autografts,53 which may result in long-term muscle fiber type changes.50 A recent meta-analysis identified that patients with QT grafts may have similar strength outcomes to those with BTB grafts, but strength deficits persist for 24 months.54 Future research may better examine this relationship to better inform research strategies.
The results of this study indicated that despite the SLVJ, SLMRH, and SLLH possessing a moderate-strong correlation with quadriceps strength those assessments may overestimate quadriceps strength symmetry in ACLR patients. Despite the SLMRH possessing the largest correlation magnitude with quadriceps strength, the SLMRH has lower sensitivity than the SLVJ in detecting quadriceps strength asymmetry. Therefore, the SLVJ may be a more useful screening tool than the SLMRH to rule out quadriceps strength asymmetry. Similarly, researchers have identified the SLSH has a moderate-strong correlation with quadriceps strength but may overestimate quadriceps strength19,43 as SLSH improves faster than quadriceps strength.43,55 These findings have stimulated researchers to investigate the merit of including multidirectional single-leg tests in post-ACLR functional assessments.19 The SLVJ may be a better assessment of knee function which contributes to approximately a third of SLVJ height and only an eighth of SLSH distance.56 Limited biomechanical research specifically for the hip exists for the SLMRH and SLLH.41 As the current study illustrates the value of single-leg multidirectional tests in ACLR functional assessments, future biomechanical research should examine lower extremity muscle and joint kinetics for both the SLLH and SLMRH.
Interestingly, as the speed of quadriceps isokinetic contraction increased, the magnitude of the correlation between SLVJ LSI and quadriceps strength LSI decreased. This is counterintuitive as theoretically lower isokinetic quadriceps angular velocities are associated with maximal muscle strength, while higher velocities are associated with power movements such as a vertical jump.57 Previous research on ACLR participants has identified that as quadriceps isokinetic velocity increased the strength of the correlation between SLVJ jump height and peak quadriceps torque increased.19 Research studies with healthy individuals have revealed conflicting results. Faster isokinetic velocities increased the magnitude of correlation between jump height and quadriceps peak torque,58 as isokinetic speed increased to 300 º/sec the correlation magnitude between jump height and quadriceps peak torque decreases59 and a signification relationship did not exist between jump height and quadriceps peak torque.60 There are methodological differences between those studies; however, it appears a relationship between SLVJ jump height and quadriceps peak torque exists; however, how this relationship is related to isokinetic angular velocity (during testing) after ACLR is not clearly understood.
Clinicians typically include patient self-reported measures such as the ACL-RSI to determine an ACLR athlete’s psychological readiness to return to sport.61 Within the ACLR group, the mean ACL-RSI score was 67, which is consistent with previous studies25,60 and greater than the proposed ≥65 threshold to return an ACLR athlete to sport.25 Contrary to the stated hypothesis, results of this study identified a weak non-significant relationship between the ACL-RSI and the single-leg multidirectional tests and quadriceps strength assessments. Several researchers have identified a moderate-strong association between the ACL-RSI and functional hops29,33,46 while two large cohorts did not identify a significant relationship.37,47 These results indicate that patient-reported function is multifactorial and dependent upon factors other than just physical performance.
This study does have limitations. A larger sample size would have allowed additional sub-analysis according to athletic ability, time from surgery, and graft types. Second, these study data were collected cross-sectionally. A longitudinal study design could assess performance measurements at multiple time points and therefore ascertain the temporal relationship between single-leg multidirectional and quadriceps strength tests. Finally, the generalizability of these results may be limited as the participants were all current or recent graduates of the USMA and sixteen of the twenty-six participants in the ACLR group had a QT autograft.
CONCLUSION
Clinicians, especially those who do not own isokinetic dynamometers, may utilize the SLVJ, SLMRH, and SLLH to identify asymmetrical single-leg function in ACLR patients. Those tests have a strong-moderate direct correlation to quadriceps strength but may under-represent strength deficits. The ACL-RSI has a weak relationship with functional and strength testing and thus be interpreted with caution.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclaimer
The views expressed in this publication are those of the author(s) and do not reflect the official policy or position of William Beaumont Army Medical Center, Department of the Army, Defense Health Agency, or the US Government.
References
- Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Sanders T. L., Maradit Kremers H., Bryan A. J., et al. 2016Am J Sports Med. 44(6):1502–1507. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- The military ACL. Tennent D.J., Posner M.A. 2019J Knee Surg. 32(2):118–122. doi: 10.1055/s-0038-1676565. doi: 10.1055/s-0038-1676565. [DOI] [PubMed] [Google Scholar]
- Passing return-to-sport criteria and landing biomechanics in young athletes following anterior cruciate ligament reconstruction. Losciale J. M., Ithurburn M. P., Paterno M. V., Schmitt L. C. Jun 3;2021 J Orthop Res. doi: 10.1002/jor.25110. doi: 10.1002/jor.25110. [DOI] [PMC free article] [PubMed]
- Return to sport tests’ prognostic value for reinjury risk after anterior cruciate ligament reconstruction: A systematic review. Ashigbi E. Y. K., Banzer W., Niederer D. 2020Med Sci Sports Exerc. 52(6):1263–1271. doi: 10.1249/MSS.0000000000002246. doi: 10.1249/MSS.0000000000002246. [DOI] [PubMed] [Google Scholar]
- Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Hui C., Salmon L. J., Kok A., Maeno S., Linklater J., Pinczewski L. A. 2011Am J Sports Med. 39(1):89–98. doi: 10.1177/0363546510379975. doi: 10.1177/0363546510379975. [DOI] [PubMed] [Google Scholar]
- Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Wiggins A. J., Grandhi R. K., Schneider D. K., Stanfield D., Webster K. E., Myer G. D. 2016Am J Sports Med. 44(7):1861–1876. doi: 10.1177/0363546515621554. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Morgan M. D., Salmon L. J., Waller A., Roe J. P., Pinczewski L. A. 2016Am J Sports Med. 44(2):384–392. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Ardern C. L., Taylor N. F., Feller J. A., Webster K. E. 2014Br J Sports Med. 48(21):1543–1552. doi: 10.1136/bjsports-2013-093398. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- Return to military duty after anterior cruciate ligament reconstruction. Antosh I. J., Patzkowski J. C., Racusin A. W., Aden J. K., Waterman S. M. 2018Mil Med. 183(1-2):e83–e89. doi: 10.1093/milmed/usx007. doi: 10.1093/milmed/usx007. [DOI] [PubMed] [Google Scholar]
- Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making. Shrier I. 2015Br J Sports Med. 49(20):1311–1315. doi: 10.1136/bjsports-2014-094569. [DOI] [PubMed] [Google Scholar]
- Running biomechanics in individuals with anterior cruciate ligament reconstruction: A systematic review. Pairot-de-Fontenay B., Willy R. W., Elias A. R. C., Mizner R. L., Dubé M. O., Roy J. S. 2019Sports Med. 49(9):1411–1424. doi: 10.1007/s40279-019-01120-x. doi: 10.1007/s40279-019-01120-x. [DOI] [PubMed] [Google Scholar]
- Clinical measures associated with knee function over two years in young athletes after ACL reconstruction. Ithurburn M. P., Paterno M. V., Thomas S., et al. 2019The Knee. 26(2):355–363. doi: 10.1016/j.knee.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Kvist J., Ek A., Sporrstedt K., Good L. 2005Knee Surg Sports Traumatol Arthrosc. 13(5):393–397. doi: 10.1007/s00167-004-0591-8. doi: 10.1007/s00167-004-0591-8. [DOI] [PubMed] [Google Scholar]
- Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: is there an association? A systematic review and a protocol recommendation. Undheim M. B., Cosgrave C., King E., et al. 2015Br J Sports Med. 49(20):1305–1310. doi: 10.1136/bjsports-2014-093962. doi: 10.1136/bjsports-2014-093962. [DOI] [PubMed] [Google Scholar]
- Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Grindem H., Snyder-Mackler L., Moksnes H., Engebretsen L., Risberg M.A. 2016Br J Sports Med. 50(13):804–808. doi: 10.1136/bjsports-2016-096031. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Webster K.E., Hewett T.E. 2019Sports Med. 49(6):917–929. doi: 10.1007/s40279-019-01093-x. doi: 10.1007/s40279-019-01093-x. [DOI] [PubMed] [Google Scholar]
- The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: A systematic review with meta-analysis. Losciale J. M., Zdeb R. M., Ledbetter L., Reiman M. P., Sell T. C. 2019J Orthop Sports Phys Ther. 49(2):43–54. doi: 10.2519/jospt.2019.8190. doi: 10.2519/jospt.2019.8190. [DOI] [PubMed] [Google Scholar]
- Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Kyritsis P., Bahr R., Landreau P., Miladi R., Witvrouw E. 2016Br J Sports Med. 50(15):946–951. doi: 10.1136/bjsports-2015-095908. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- Single-leg hop can result in higher limb symmetry index than isokinetic strength and single-leg vertical jump following anterior cruciate ligament reconstruction. Ohji S., Aizawa J., Hirohata K., et al. 2021The Knee. 29:160–166. doi: 10.1016/j.knee.2021.01.030. doi: 10.1016/j.knee.2021.01.030. [DOI] [PubMed] [Google Scholar]
- Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Ebert J.R., Edwards P., Yi L., et al. 2018Knee Surg Sports Traumatol Arthrosc. 26(8):2353–2361. doi: 10.1007/s00167-017-4712-6. doi: 10.1007/s00167-017-4712-6. [DOI] [PubMed] [Google Scholar]
- Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: How many actually meet recommended return-to-sport criterion cutoffs? Toole A. R., Ithurburn M. P., Rauh M. J., Hewett T. E., Paterno M. V., Schmitt L. C. 2017J Orthop Sports Phys Ther. 47(11):825–833. doi: 10.2519/jospt.2017.7227. doi: 10.2519/jospt.2017.7227. [DOI] [PubMed] [Google Scholar]
- Who passes return-to-sport tests, and which tests are most strongly associated with return to play after anterior cruciate ligament reconstruction? Webster K.E., Feller J.A. 2020Orthop J Sports Med. 8(12):2325967120969425. doi: 10.1177/2325967120969425. doi: 10.1177/2325967120969425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Single-leg vertical hop test detects greater limb asymmetries than horizontal hop tests after anterior cruciate ligament reconstruction in NCAA Division 1 collegiate athletes. Zarro M.J., Stitzlein M.G., Lee J.S., et al. 2021Int J Sports Phys Ther. 16(6):1405–1414. doi: 10.26603/001c.29595. doi: 10.26603/001c.29595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Webster K.E., Feller J.A., Lambros C. 2008Phys Ther Sport. 9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Progression of the psychological ACL-RSI score and return to sport after anterior cruciate ligament reconstruction: A prospective 2-year follow-up study from the French prospective anterior cruciate ligament reconstruction cohort study (FAST) Sadeqi M., Klouche S., Bohu Y., Herman S., Lefevre N., Gerometta A. 2018Orthop J Sports Med. 6(12):2325967118812819. doi: 10.1177/2325967118812819. doi: 10.1177/2325967118812819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patellofemoral joint loads during running at the time of return to sport in elite athletes with ACL reconstruction. Herrington L., Alarifi S., Jones R. 2017Am J Sports Med. 45(12):2812–2816. doi: 10.1177/0363546517716632. [DOI] [PubMed] [Google Scholar]
- Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. Wellsandt E., Failla M. J., Snyder-Mackler L. 2017J Orthop Sports Phys Ther. 47(5):334–338. doi: 10.2519/jospt.2017.7285. doi: 10.2519/jospt.2017.7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. Petschnig R., Baron R., Albrecht M. 1998J Orthop Sports Phys Ther. 28(1):23–31. doi: 10.2519/jospt.1998.28.1.23. doi: 10.2519/jospt.1998.28.1.23. [DOI] [PubMed] [Google Scholar]
- Single-leg vertical jump test as a functional test after anterior cruciate ligament reconstruction. Lee D.W., Yang S.J., Cho S.I., Lee J.H., Kim J.G. 2018The Knee. 25(6):1016–1026. doi: 10.1016/j.knee.2018.07.014. doi: 10.1016/j.knee.2018.07.014. [DOI] [PubMed] [Google Scholar]
- Test-retest reliability and discriminative ability of forward, medial and rotational single-leg hop tests. Dingenen B., Truijen J., Bellemans J., Gokeler A. 2019The Knee. 26(5):978–987. doi: 10.1016/j.knee.2019.06.010. [DOI] [PubMed] [Google Scholar]
- Which hop tests can best identify functional limb asymmetry in patients 9-12 months after anterior cruciate ligament reconstruction employing a hamstrings tendon autograft? Ebert J. R., Du Preez L., Furzer B., Edwards P., Joss B. 2021Int J Sports Phys Ther. 16(2):393–403. doi: 10.26603/001c.21140. doi: 10.26603/001c.21140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correlations between isokinetic knee torques and single-leg hop distances in three directions in patients after ACL reconstruction. Aizawa J., Hirohata K., Ohji S., et al. 2021BMC Sports Sci Med Rehabil. 13(1):38. doi: 10.1186/s13102-021-00265-5. doi: 10.1186/s13102-021-00265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borawski J. Do psychological factors contribute to neuromuscular asymmetries following anterior cruciate ligament reconstruction?; APTA Combined Sections Meeting; San Antonio, TX: [Google Scholar]
- Knee extensor strength, hop performance, patient-reported outcome and inter-test correlation in patients 9-12 months after anterior cruciate ligament reconstruction. Ebert J. R., Edwards P., Preez L. D., Furzer B., Joss B. 2021The Knee. 30:176–184. doi: 10.1016/j.knee.2021.04.012. doi: 10.1016/j.knee.2021.04.012. [DOI] [PubMed] [Google Scholar]
- Bilateral alterations in running mechanics and quadriceps function following unilateral anterior cruciate ligament reconstruction. Pamukoff D. N., Montgomery M. M., Choe K. H., Moffit T. J., Garcia S. A., Vakula M. N. J Orthop Sports Phys Ther. 48(12):960–967. doi: 10.2519/jospt.2018.8170. doi: 10.2519/jospt.2018.8170. [DOI] [PubMed] [Google Scholar]
- Better reporting standards are needed to enhance the quality of hop testing in the setting of ACL return to sport decisions: a narrative review. Read P., Mc Auliffe S., Wilson M. G., Myer G. D. 2021Br J Sports Med. 55(1):23–29. doi: 10.1136/bjsports-2019-101245. doi: 10.1136/bjsports-2019-101245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- No relationship between strength and power scores and anterior cruciate ligament return to sport after injury scale 9 months after anterior cruciate ligament reconstruction. O’Connor R.F., King E., Richter C., Webster K.E., Falvey É.C. 2020Am J Sports Med. 48(1):78–84. doi: 10.1177/0363546519887952. doi: 10.1177/0363546519887952. [DOI] [PubMed] [Google Scholar]
- The role of psychological readiness in return to sport assessment after anterior cruciate ligament reconstruction. Faleide A.G.H., Magnussen L.H., Strand T., et al. 2021Am J Sports Med. 49(5):1236–1243. doi: 10.1177/0363546521991924. doi: 10.1177/0363546521991924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The reliability of three devices used for measuring vertical jump height. Nuzzo J. L., Anning J. H., Scharfenberg J. M. 2011J Strength Cond Res. 25(9):2580–2590. doi: 10.1519/JSC.0b013e3181fee650. doi: 10.1519/JSC.0b013e3181fee650. [DOI] [PubMed] [Google Scholar]
- Validity of two alternative systems for measuring vertical jump height. Leard J. S., Cirillo M. A., Katsnelson E.., et al. 2007J Strength Cond Res. 21(4):1296–1299. doi: 10.1519/R-21536.1. doi: 10.1519/R-21536.1. [DOI] [PubMed] [Google Scholar]
- Hip abduction-adduction strength and one-leg hop tests: test-retest reliability and relationship to function in elite ice hockey players. Kea J., Kramer J., Forwell L., Birmingham T. 2001J Orthop Sports Phys Ther. 31(8):446–455. doi: 10.2519/jospt.2001.31.8.446. doi: 10.2519/jospt.2001.31.8.446. [DOI] [PubMed] [Google Scholar]
- Inter-machine reliability of the Biodex and Cybex isokinetic dynamometers for knee flexor/extensor isometric, concentric and eccentric tests. de Araujo Ribeiro Alvares J. B., Rodrigues R., de Azevedo Franke R., et al. 2015Phys Ther Sport. 16(1):59–65. doi: 10.1016/j.ptsp.2014.04.004. doi: 10.1016/j.ptsp.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Knee extensor strength and hop test performance following anterior cruciate ligament reconstruction. Barfod K. W., Feller J. A., Hartwig T., Devitt B. M., Webster K. E. 2019The Knee. 26(1):149–154. doi: 10.1016/j.knee.2018.11.004. doi: 10.1016/j.knee.2018.11.004. [DOI] [PubMed] [Google Scholar]
- Leg asymmetry and muscle function recovery after anterior cruciate ligament reconstruction in elite athletes: a pilot study on slower recovery of the dominant leg. Souissi S., Chaouachi A., Burnett A., et al. 2020Biol Sport. 37(2):175–184. doi: 10.5114/biolsport.2020.94238. doi: 10.5114/biolsport.2020.94238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Lawrence Erlbaum; [Google Scholar]
- Correlations between isokinetic knee torques and single-leg hop distances in three directions in patients after ACL reconstruction. Aizawa J., Hirohata K., Ohji S., et al. 2021BMC Sports Sci Med Rehabil. 13(1):38. doi: 10.1186/s13102-021-00265-5. doi: 10.1186/s13102-021-00265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subjective knee apprehension is not associated to physical parameters 6-12 months after anterior cruciate ligament reconstruction. Gauthier M., Lê T. N., Wehn A., Joseph S., Tscholl P. M. 2022J Exp Orthop. 9(1):110. doi: 10.1186/s40634-022-00545-0. doi: 10.1186/s40634-022-00545-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isokinetic extension strength is associated with single-leg vertical jump height. Fischer F., Blank C., Dünnwald T., et al. 2017Orthop J Sports Med. 5(11):2325967117736766. doi: 10.1177/2325967117736766. doi: 10.1177/2325967117736766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relationship between isokinetic knee strength and jump characteristics following anterior cruciate ligament reconstruction. Laudner K., Evans D., Wong R., et al. 2015Int J Sports Phys Ther. 10(3):272–280. [PMC free article] [PubMed] [Google Scholar]
- Muscle atrophy after ACL injury: Implications for clinical practice. Lepley L.K., Davi S.M., Burland J.P., Lepley A.S. 2020Sports Health. 12(6):579–586. doi: 10.1177/1941738120944256. doi: 10.1177/1941738120944256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinician-friendly lower extremity physical performance measures in athletes: a systematic review of measurement properties and correlation with injury, Part 1. The tests for knee function including the hop tests. Hegedus E. J., McDonough S., Bleakley C., Cook C. E., Baxter G. D. 2015Br J Sports Med. 49(10):642–648. doi: 10.1136/bjsports-2014-094094. doi: 10.1136/bjsports-2014-094094. [DOI] [PubMed] [Google Scholar]
- Residual deficits in reactive strength indicate incomplete restoration of athletic qualities following anterior cruciate ligament reconstruction in professional soccer players. Read P. J., Davies W. T., Bishop C., Mc Auliffe S., Wilson M. G., Turner A. N. Nov 5;2020 J Athl Train. doi: 10.4085/169-20. doi: 10.4085/169-20. [DOI] [PubMed]
- Anterior cruciate ligament reconstruction: A systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Mouarbes D., Menetrey J., Marot V., Courtot L., Berard E., Cavaignac E. 2019Am J Sports Med. 47(14):3531–3540. doi: 10.1177/0363546518825340. doi: 10.1177/0363546518825340. [DOI] [PubMed] [Google Scholar]
- Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: systematic review and meta-analysis. Johnston P.T., McClelland J.A., Feller J.A., Webster K.E. 2021Knee Surg Sports Traumatol Arthrosc. 29(9):2918–2933. doi: 10.1007/s00167-020-06311-y. doi: 10.1007/s00167-020-06311-y. [DOI] [PubMed] [Google Scholar]
- Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Thomeé R., Neeter C., Gustavsson A., et al. 2012Knee Surg Sports Traumatol Arthrosc. 20(6):1143–1151. doi: 10.1007/s00167-012-1912-y. doi: 10.1007/s00167-012-1912-y. [DOI] [PubMed] [Google Scholar]
- Vertical and horizontal hop performance: Contributions of the hip, knee, and ankle. Kotsifaki A., Korakakis V., Graham-Smith P., Sideris V., Whiteley R. 2021Sports Health. 13(2):128–135. doi: 10.1177/1941738120976363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physiological significance of the force-velocity relation in skeletal muscle and muscle fibers. Sugi H., Ohno T. 2019Int J Mol Sci. 20(12):3075. doi: 10.3390/ijms20123075. doi: 10.3390/ijms20123075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relationship between isokinetic strength, vertical jump, spring speed, agility, and Yo-Yo intermittent recovery test in soccer players. Cerrah A.O., Bayram İ. 2022Eur J Phys Educ Sport Sci. 9(2) doi: 10.46827/ejpe.v9i2.4514. doi: 10.46827/ejpe.v9i2.4514. [DOI] [Google Scholar]
- Assessment of isokinetic knee strength in elite young female basketball players: correlation with vertical jump. Rouis M., Coudrat L., Jaafar H., et al. 2015J Sports Med Phys Fitness. 55(12):1502–1508. [PubMed] [Google Scholar]
- Relationship between force-velocity-power profiles and inter-limb asymmetries obtained during unilateral vertical jumping and singe-joint isokinetic tasks. Kozinc Ž., Marković G., Hadžić V., Šarabon N. 2021J Sports Sci. 39(3):248–258. doi: 10.1080/02640414.2020.1816271. doi: 10.1080/02640414.2020.1816271. [DOI] [PubMed] [Google Scholar]
- Quadriceps function, knee pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction. Lepley A.S., Pietrosimone B., Cormier M.L. 2018J Athl Train. 53(4):337–346. doi: 10.4085/1062-6050-245-16. doi: 10.4085/1062-6050-245-16. [DOI] [PMC free article] [PubMed] [Google Scholar]


