Abstract
Adolescent idiopathic scoliosis (AIS) is an abnormal coronal curvature of the spine that most commonly presents in adolescence.
While it may be asymptomatic, AIS can cause pain, cosmetic deformity, and physical and psychological disability with curve progression.
As adolescents with AIS enter adulthood, condition outcomes vary with some experiencing curve stabilization and others noting further curve progression, chronic pain, osteoporosis/fractures, declines in pulmonary and functional capacity, among others.
Regular monitoring and individualized management by healthcare professionals are crucial to address the diverse challenges and provide appropriate support for a fulfilling adult life with AIS.
This review examines the prevalence, risk factors, presenting symptoms, diagnosis, management, and complications of AIS in the adult population, informing targeted interventions by clinicians caring for adult patients with AIS.
Keywords: adolescent idiopathic scoliosis, adults, progression, quality of life, management
Introduction
Adolescent idiopathic scoliosis (AIS) is the abnormal coronal curvature of the spine (Cobb angle ≥10º) that affects 0.5–5.2% of children ages 10–18 years (1, 2, 3, 4, 5). It is disproportionately seen in females, with a female-to-male prevalence ratio ranging from 1.5:1 to 3:1. While de novo scoliosis has a mean age of onset of 70.5 years, AIS often begins in late childhood or adolescence. Although the cause of AIS is unknown, a multitude of genetic and environmental factors are thought to play a role (6, 7, 8, 9, 10, 11, 12). As mild disease can be asymptomatic, diagnosis often requires early and frequent school screenings followed by radiographic confirmation (1). Management is subsequently dependent on the extent of the curvature, with simple observation and bracing for mild cases and surgical management for severe cases (13, 14).
Despite optimal management, AIS can continue into adulthood and result in chronic pain, disability, and cosmetic deformity (3, 4, 15, 16). Failure to diagnose AIS at its earlier stages or to recognize AIS as a debilitating lifelong condition can occur among clinicians and even delay treatment (17). This review aims to summarize data regarding AIS in adulthood, including prevalence, risk factors, presentation, diagnosis, management, and complications, such that clinicians can better understand and treat patients with this condition.
Epidemiology
Prevalence
Scoliosis affects roughly 8% of adults over the age of 25 years and its prevalence rises to 68% in those over 60 years with the development of degenerative changes in the spine (5, 18). While it is known that AIS affects 0.5–5.2% of children ages 10–18 years, it is not known what proportion of these patients continue to have symptomatic AIS in adulthood (2, 3, 4, 5). The natural history of AIS is curve progression, mainly in curves that reach a cobb angle >40° at the end of growth; thus, an adolescent with AIS will eventually become an adult with AIS.
Risk factors
Female sex is a well-known risk factor of AIS regardless of age (4, 16). Family history of AIS has also been associated in several twin/single-family studies and is likely a result of a complex interplay of multiple genes, including in the rs6570507 locus within GPR126 and in genes associated with the calmodulin pathway (11, 19, 20, 21). Radiographic features, in particular greater Cobb angle, cranially located apical vertebrae, and tilting of the L3 vertebrae, can also give insight into the development and progression of AIS (15, 22). Others including asymmetry of the body, muscular imbalances or weaknesses, and abnormal puberty have also been associated, though these factors are likely not causative but rather manifestations of associated genetic and soft tissue-related conditions (12).
Presentation
In adolescence, AIS often presents with progressive deformity manifesting as asymmetric shoulder or hip height, body tilt, or unusual body prominence (1). Back pain is also commonly seen (3, 16). In adults, these symptoms may persist and progressively worsen, with correlation between AIS-associated back pain and need for surgery in adulthood (16). Chronically untreated patients may further develop respiratory and cardiac abnormalities due to their growing curvature affecting the contour of the thoracic cavity, thereby reducing its diameter and thus vital capacity (3, 23).
Diagnosis
Diagnosis of AIS involves a thorough patient history, including personal growth and family history, followed by physical assessment for upright posture, unequal leg length, shoulder height discrepancies, truncal shift, and pelvic tilt. Early and routine screening has shown many benefits in preventing the severe physical and psychological sequelae of AIS in adults (1, 4, 15, 23). However, the evidence for the benefit of routine scoliosis screening is debated, with the U.S. Preventive Services Task Force and American Academy of Family Physicians (USPSTF) recommending against routine scoliosis screening in asymptomatic adolescents and the Scoliosis Research Society (SRS), American Academy of Orthopaedic Surgeons (AAOS), American Academy of Pediatrics (AAP), and Pediatric Orthopaedic Society of North America (POSNA) recommending for routine screening in all adolescents (1). Despite this debate, routine screenings with the Adams’ forward bend test and scoliometers continue to be performed at regular wellness visits, with delays in diagnosis often stemming from a paucity of medical knowledge or a lack of awareness regarding the condition as opposed to a failure of screening (17).
Physical exam
The Adams’ forward bend test, which involves the patient bending forward at the waist with the knees straight and the examiner assessing for ribcage asymmetry and spinal deformity, is perhaps the most widely used screening test for scoliosis (Fig. 1) (1, 24). Scoliometers can also provide an additional quantitative assessment of truncal rotation, with >5–7º considered abnormal, but are generally considered to be less sensitive (Fig. 1) (1, 25, 26). Right thoracic curvature is most commonly observed; left thoracic curvature is atypical and can be associated with cysts or syrinx, warranting further workup with MRI spine screen (27).
Figure 1.

Lateral view of the Adams’ forward bend test (right) and use of a scoliometer during the test (left).
Imaging
Full-length 36-inch, or EOS imaging, can be used to visualize the spinal curvature in patients with suspected AIS (13, 28). Images are taken from posteroanterior (PA) and lateral views to assess for coronal and sagittal plane abnormalities, respectively. The coronal films are especially useful for the measurement of Cobb angle. This indirect angle is a measure of scoliosis curvature calculated by identifying the superior and inferior endplates of the two vertebrae with the greatest tilt, drawing lines in parallel with the endplates, and measuring the angle at the intersection (29). Scoliosis can, then, be quantified and categorized as mild (10º–20º), moderate (21º–40º), and severe (>40º) (Table 1). The lateral films can provide further information about the associated changes in key sagittal parameters, including sagittal vertical axis, lumbar lordosis, pelvic incidence, pelvic tilt, and sacral slope.
Table 1.
Severity and treatment recommendations for AIS based on Cobb angle.
| Cobb angle magnitude | Severity and treatment |
|---|---|
| 0°–10° | Normal curvature; no treatment necessary |
| 10°–25° | Mild scoliosis; follow progression of curvature, re-evaluate after set period |
| 25°–40° | Moderate scoliosis; bracing |
| 40° and over | Severe scoliosis; surgical treatment may be necessary |
In addition to upright imaging, fulcrum bending films and traction radiographs may be performed to determine the flexibility of curvature. Magnetic resonance imaging (MRI) may also be necessary for patients with neuromuscular symptoms, left thoracic curvature, or other atypical abnormalities to rule out malignancy, developmental abnormalities (e.g. syringomyelia), and structural issues (30, 31, 32, 33).
Classification
Several classification systems have been devised to guide management of adult spinal deformity. The Aebi classification initially characterized spinal deformity by etiology, including primary degenerative (type I), progressive idiopathic (type II), and secondary (type III) scoliosis (34). The Scoliosis Research Society (SRS)–Schwab classification was later developed and incorporated coronal curve type and sagittal parameters, including pelvic incidence–lumbar lordosis mismatch, sagittal vertical axis, and pelvic tilt (35). In parallel, the Roussouly classification was refined and identified ‘current’ and ‘theoretical’ sagittal profiles based on pelvic incidence (36). Now, concurrent consideration of both the SRS-Schwab and the Roussouly classification system is made to define the severity of deformity and optimal realignment goals (37).
Management of AIS in adults
Management of AIS is primarily dependent on the risk of progression. Once skeletal maturity is reached, the likelihood of progression of AIS is lower (38). Non-operative interventions, such as physical therapy and bracing, generally slow the progression of the spinal curve during adulthood. Operative interventions, such as spinal instrumentation and fusion, on the other hand, attempt to restore spinal curvature and improve coronal and sagittal spinopelvic alignment. Both, ultimately, hope to improve presenting symptoms and long-term outcomes.
Non-operative techniques
Exercise and physical therapy
Physiotherapy scoliosis-specific exercises (PSSEs) are considered as the first step in the management of mild scoliosis (4, 34, 39, 40). The Schroth method, the Scientific Exercise Approach to Scoliosis (SEAS), the Dobosiewicz technique, and the side-shift program, in particular, are the most frequently prescribed types of PSSE (41, 42, 43, 44, 45, 46). These techniques generally focus on enhancing posture control, muscle endurance, spinal stability, and overall balance.
Bracing
Few studies have addressed initiating bracing in adult cases of AIS. Bracing is not common among adults due to barriers precluding its effective implementation including limited mobility, discomfort in high temperatures, and cosmetic displeasure (47). Modest evidence, however, indicates that bracing can slow down curve progression, reduce pain, and improve disability scores when worn for just 6 h daily (48, 49, 50).
Indications for operative management
Chronic back pain
Chronic back pain due to early AIS can develop or persist in adulthood and is generally more severe than that observed in the normal population (51, 52). A study by Ersen et al. has further shown an association with weight using data from the SRS-22, a questionnaire specifically designed to assess health-related quality of life in patients with AIS, noting that increased BMI is associated with chronic low back pain in both normal and scoliotic individuals (53). This can result in restrictions in daily activities, such as difficulties in walking, exercising, and socializing. Surgery tends to be more painful for adult patients compared to adolescents, but long-term outcomes show a significant reduction in pain regardless (54).
Poor physical function
Although AIS patients score similar to their peers in health-related quality of life (HRQoL) measures in mild disease, they may note a significant decline in HRQoL and physical functioning measures in adulthood in more severe disease (55). In one longitudinal study, Danielsson et al. found that patients with mild AIS had comparable HRQoL as the general population 20 years after treatment with bracing or surgery (3). The degree of curvature after treatment, total treatment time, or age at the completion of treatment played no apparent role. On the other hand, patients with severe AIS, particularly with curves greater than 50°, note significant limitations in activities of daily living and physical functioning. Surgical treatment in this population can prevent and alleviate these conditions, with treated adults showing significant improvements in their physical functioning (54). Such restoration in functional mobility can also improve performance at work, reducing absenteeism and increasing productivity by 18.1% post-surgical intervention (56).
Low self-image
AIS patients have also been shown to consistently suffer from decreased self-esteem and poor psychological health due to negative body image, regardless of disease severity (57, 58, 59, 60). In particular, longer bracing durations, older age at initial bracing, and higher Cobb angles have been associated with greater depression symptoms and more deformed physical appearance, particularly in older patients who may be more conscious of their body image (61, 62). This decline in self-image is typically worse in surgically treated patients, likely due to spinal fusion-related stiffness and scarring, and awareness of implants and surgical incisions (63, 64).
Osteopenia/osteoporosis
Continued AIS in adulthood is associated with reduced bone mineral density (BMD), leading to osteopenia and osteoporosis (65). Studies have shown that 20–38% of adults with a history of AIS develop osteoporosis later in life, often at an earlier age than the general pediatric and adolescent population (66, 67). Moreover, even with early treatment of AIS, these patients may still lose BMD and develop significant intervertebral disc degeneration in adulthood than matched controls (68, 69). The loss of bone density could be due to abnormal mechanical loading in scoliotic patients, resulting in localized areas of increased or decreased resorption. Serial imaging and DEXA screening is, thus, warranted in patients with AIS (9).
Respiratory decline
Eventually, adults with untreated or severe (Cobb angle ≥40º) AIS may develop respiratory function decline, including reduced vital capacity and frequent shortness of breath (70). This may further exacerbate chronic back pain, emotional distress, and reduced quality of life. However, such severe cardiopulmonary compromise is rare and the associated impact on morbidity and mortality may, in fact, be similar between patients with and without AIS (70). Further longitudinal studies would need to be conducted to confirm this relationship.
Pregnancy-related implications
Although concerns have been raised about the impact of AIS on pregnancy and vice versa, studies have shown that spinal curves do not affect fetal growth or significantly worsen during pregnancy (71, 72). Likewise, complication rates following surgical intervention for severe curvature during pregnancy and/or delivery do not significantly differ between patients with and without AIS (73). However, the additional weight of the fetus does place eccentric mechanical load on the scoliotic spine, possibly exacerbating chronic pain in AIS. This may subsequently explain the higher rates of C-section in women with AIS than those without AIS (74).
Operative techniques
Surgical intervention in adults with AIS is primarily indicated for focal painful deformities, compressive neurological conditions, and global spinal imbalance. The mainstay of surgical treatment is spinal instrumentation and fusion. During spinal fusion, anchors connected to longitudinal rods spanning the desired length of fusion are fixed to the vertebrae with screws inserted into the pedicles. Bone grafting can then be used to promote fusion between the individual vertebrae (75). Most spinal fusions are performed using posterior approach. However, in some cases, a combined approach can be used (i.e. minimally invasive lateral (XLIF (extreme lateral interbody fusion)) or retroperitoneal anterior (ALIF (anterior lumbar interbody fusion) or OLIF (oblique lateral interbody fusion))) (76, 77).
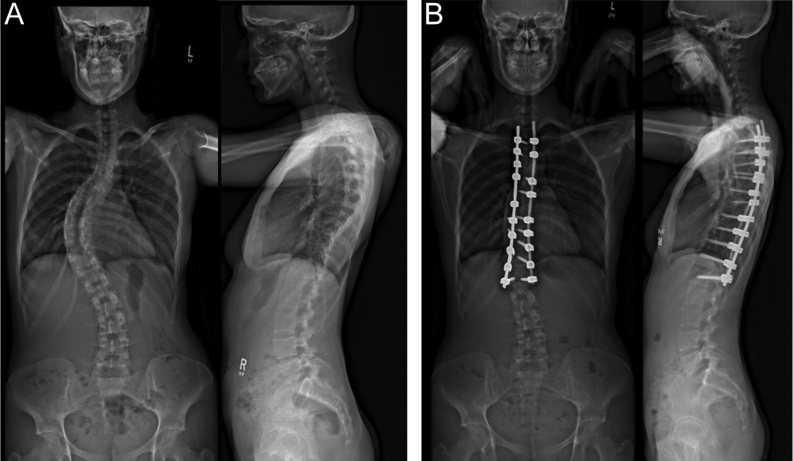
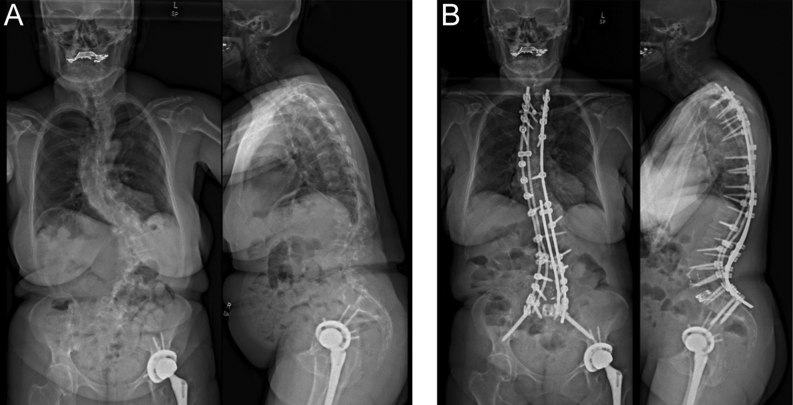
Figure 2 demonstrates pre-/post-operative radiographs for a 43-year-old female with untreated AIS who underwent T3–L2 fusion. Figure 3 similarly illustrates pre-/post-operative radiographs for a 64-year-old female with progressive AIS in both the coronal and sagittal plane who underwent an upper thoracic to pelvis fusion after failing conservative management. Anterior spinal fusion (ASF) is often saved for the correction of lumbar hypolordosis and thoracic hypokyphosis, as it allows for a greater degree of sagittal curve correction and improved postoperative mobility of the spine (78). Combined anterior and posterior spinal fusion may, ultimately, be necessary in cases of large curvature as it allows for a greater degree of curve correction, decreased stress on the construct, and improved overall fusion.
Figure 2.
A 43-year-old patient who underwent a selected T3–L2 fusion for untreated AIS presenting with back pain (A: pre-operation and B: 2 months post operation).
Figure 3.
A 64-year-old patient who underwent a T2–pelvis spinal fusion for untreated scoliotic deformity presenting with lower back pain and worsening of posture (A: pre-operation and B: post operation).
Complications
Acute complications
Coe at al. performed an analysis of the surgeon-reported SRS morbidity and mortality database, which included 6334 patients who underwent spinal fusion surgeries for AIS, and found an overall complication rate of 5.7%, with higher rate for combined anterior/posterior procedures (10.2%) compared to posterior (5.1%) and anterior (5.2%) procedures alone (79). Early or late infection, implant failure (pseudarthrosis), and recurrence have all been estimated to be approximately 1–2%; neurological complications occur even more infrequently, at less than 1% (80). Furthermore, when comparing young adults to adolescents after AIS surgery, Lavelle et al. showed that young adults had more levels fused, more intra-operative blood loss, and a lower percentage of correction at 21 months follow-up (80).
Chronic complications
Adjacent segment disease, proximal junctional kyphosis, and flatback syndrome can occur as a consequence of a multi-level fusion (81, 82, 83, 84, 85, 86). Although patients with these conditions may not always present with any specific complaints, they still need to be examined by deformity specialists because they may develop neurologic deficits due to compression or injury to the spinal cord or nerve roots (86, 87, 88, 89, 90). Presence of pain, on the other hand, may be an indication of hardware failure and potential neurologic injury. In particular, postoperative weakness, gait abnormalities, and pain at the top or bottom of the fusion may be suggestive of a neurologic injury and warrant emergent imaging and evaluation by a deformity specialist.
Conclusion
AIS in adulthood is a common but underrecognized disorder with a multifactorial etiology. Early detection of AIS is crucial for the development of an effective and patient-specific management plan. Both non-surgical and surgical interventions are available, with treatment depending on various factors including severity of spinal curvature and risk of curve progression. While non-surgical approaches such as observation and bracing are generally considered the first line of treatment, surgery and orthopedic referral is recommended for severe cases, especially among those with rapid curve progression, pain, disability, or associated neurological compression syndromes. Adult treatment of AIS requires critical evaluation of clinical data as well as consideration of individual alignment parameters and should be reserved for spinal deformity specialists in lieu of the general spine surgeon.
ICMJE Conflict of Interest Statement
KA, MS, JRM, JAG, MBC, MD, and CLM declare no competing interests. BGD declares consulting fees for Clariance and Spinevision. However, none of them is relevant to this manuscript. AHD declares grants from Stryker and Medtronic, royalties from Stryker and Spineart, consulting fees from Stryker, Spineart, and Medtronic, receiving payment for expert testimony from multiple law firms. However, none of them is relevant to this article.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
References
- 1.Horne JP Flannery R & Usman S. Adolescent idiopathic scoliosis: diagnosis and management. American Family Physician 201489193–198. [PubMed] [Google Scholar]
- 2.Asher MA & Burton DC. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis 200612. ( 10.1186/1748-7161-1-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Danielsson AJ. Natural history of adolescent idiopathic scoliosis: a tool for guidance in decision of surgery of curves above 50°. Journal of Children’s Orthopaedics 2013737–41. ( 10.1007/s11832-012-0462-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erwin J Carlson BB Bunch J Jackson RS & Burton D. Impact of unoperated adolescent idiopathic scoliosis in adulthood: a 10-year analysis. Spine Deformity 202081009–1016. ( 10.1007/s43390-020-00142-0) [DOI] [PubMed] [Google Scholar]
- 5.Konieczny MR Senyurt H & Krauspe R. Epidemiology of adolescent idiopathic scoliosis. Journal of Children’s Orthopaedics 201373–9. ( 10.1007/s11832-012-0457-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grubb SA Lipscomb HJ & Coonrad RW. Degenerative adult onset scoliosis. Spine 198813241–245. ( 10.1097/00007632-198803000-00004) [DOI] [PubMed] [Google Scholar]
- 7.Diebo BG Shah NV Boachie-Adjei O Zhu F Rothenfluh DA Paulino CB Schwab FJ & Lafage V. Adult spinal deformity. Lancet 2019394160–172. ( 10.1016/S0140-6736(1931125-0) [DOI] [PubMed] [Google Scholar]
- 8.Vanderpool DW James JI & Wynne-Davies R. Scoliosis in the elderly. Journal of Bone and Joint Surgery 196951446–455. ( 10.2106/00004623-196951030-00002) [DOI] [PubMed] [Google Scholar]
- 9.Wu Z, Zhu X, Xu L, Liu Z, Feng Z, Hung VWY, Cheng JCY, Qiu Y, Lee WYW, Lam TP, et al.More prevalent and severe low bone-mineral density in boys with severe adolescent idiopathic scoliosis than girls: a retrospective study of 798 surgical patients. Journal of Clinical Medicine 2023122991. ( 10.3390/jcm12082991) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu JZ Wu WH He LJ Ke QF Huang L Dai ZS & Chen Y. Effect of melatonin and calmodulin in an idiopathic scoliosis model. BioMed Research International 201620168460291. ( 10.1155/2016/8460291) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li W, Li Y, Zhang L, Guo H, Tian D, Li Y, Peng Y, Zheng Y, Dai Y, Xia K, et al.AKAP2 identified as a novel gene mutated in a Chinese family with adolescent idiopathic scoliosis. Journal of Medical Genetics 201653488–493. ( 10.1136/jmedgenet-2015-103684) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kikanloo SR Tarpada SP & Cho W. Etiology of adolescent idiopathic scoliosis: a literature review. Asian Spine Journal 201913519–526. ( 10.31616/asj.2018.0096) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lonstein JE. Scoliosis: surgical versus nonsurgical treatment. Clinical Orthopaedics and Related Research 2006443248–259. ( 10.1097/01.blo.0000198725.54891.73) [DOI] [PubMed] [Google Scholar]
- 14.Farshad M Kutschke L Laux CJ Kabelitz M Schüpbach R Böni T & Jentzsch T. Extreme long-term outcome of operatively versus conservatively treated patients with adolescent idiopathic scoliosis. European Spine Journal 2020292084–2090. ( 10.1007/s00586-020-06509-1) [DOI] [PubMed] [Google Scholar]
- 15.Ascani E Bartolozzi P Logroscino CA Marchetti PG Ponte A Savini R Travaglini F Binazzi R & Di Silvestre M. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine 198611784–789. ( 10.1097/00007632-198610000-00007) [DOI] [PubMed] [Google Scholar]
- 16.Larson AN Baky F Ashraf A Baghdadi YM Treder V Polly DW & Yaszemski MJ. Minimum 20-year health-related quality of life and surgical rates after the treatment of adolescent idiopathic scoliosis. Spine Deformity 20197417–427. ( 10.1016/j.jspd.2018.09.003) [DOI] [PubMed] [Google Scholar]
- 17.Kenner P McGrath S & Woodland P. What factors influence delayed referral to spinal surgeon in adolescent idiopathic scoliosis? Spine 2019441578–1584. ( 10.1097/BRS.0000000000003146) [DOI] [PubMed] [Google Scholar]
- 18.Carter OD & Haynes SG. Prevalence rates for scoliosis in US adults: results from the first National Health and Nutrition Examination Survey. International Journal of Epidemiology 198716537–544. ( 10.1093/ije/16.4.537) [DOI] [PubMed] [Google Scholar]
- 19.Simony A Carreon LY Jmark KH Kyvik KO & Andersen MØ. Concordance rates of adolescent idiopathic scoliosis in a Danish twin population. Spine 2016411503–1507. ( 10.1097/BRS.0000000000001681) [DOI] [PubMed] [Google Scholar]
- 20.Kou I, Watanabe K, Takahashi Y, Momozawa Y, Khanshour A, Grauers A, Zhou H, Liu G, Fan YH, Takeda K, et al.A multi-ethnic meta-analysis confirms the association of rs6570507 with adolescent idiopathic scoliosis. Scientific Reports 2018811575. ( 10.1038/s41598-018-29011-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Y Gu Z & Qiu G. The association study of calmodulin 1 gene polymorphisms with susceptibility to adolescent idiopathic scoliosis. BioMed Research International 20142014168106. ( 10.1155/2014/168106) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohashi M Watanabe K Hirano T Hasegawa K Katsumi K Shoji H Mizouchi T & Endo N. Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves: a mean 25-year follow-up. Spine 201843E1403–E1411. ( 10.1097/BRS.0000000000002716) [DOI] [PubMed] [Google Scholar]
- 23.Xue X Shen J Zhang J Zhao H Li S Wang Y Liang J Weng X & Qiu G. An analysis of thoracic cage deformities and pulmonary function tests in congenital scoliosis. European Spine Journal 2015241415–1421. ( 10.1007/s00586-014-3327-6) [DOI] [PubMed] [Google Scholar]
- 24.Altaf F Gibson A Dannawi Z & Noordeen H. Adolescent idiopathic scoliosis. BMJ 2013346f2508. ( 10.1136/bmj.f2508) [DOI] [PubMed] [Google Scholar]
- 25.Ashworth MA Hancock JA Ashworth L & Tessier KA. Scoliosis screening: an approach to cost/benefit analysis. Spine 1988131187–1188. ( 10.1097/00007632-198810000-00024) [DOI] [PubMed] [Google Scholar]
- 26.Kuznia AL Hernandez AK & Lee LU. Adolescent idiopathic scoliosis: common questions and answers. American Family Physician 202010119–23. [PubMed] [Google Scholar]
- 27.Yeom JS Lee CK Park KW Lee JH Lee DH Wang KC & Chang BS. Scoliosis associated with syringomyelia: analysis of MRI and curve progression. European Spine Journal 2007161629–1635. ( 10.1007/s00586-007-0472-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bunch JT Glassman SD Underwood HR Metcalfe LN Ondra S Vasilyev I & Carreon LY. Preoperative full-length standing radiographs and revision rates in lumbar degenerative scoliosis. Journal of Neurosurgery 201828581–585. ( 10.3171/2017.10.SPINE17638) [DOI] [PubMed] [Google Scholar]
- 29.Horng MH Kuok CP Fu MJ Lin CJ & Sun YN. Cobb angle measurement of spine from X-ray images using convolutional neural network. Computational and Mathematical Methods in Medicine 201920196357171. ( 10.1155/2019/6357171) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnes PD Brody JD Jaramillo D Akbar JU & Emans JB. Atypical idiopathic scoliosis: MR imaging evaluation. Radiology 1993186247–253. ( 10.1148/radiology.186.1.8416573) [DOI] [PubMed] [Google Scholar]
- 31.Choudhry MN Ahmad Z & Verma R. Adolescent idiopathic scoliosis. Open Orthopaedics Journal 201610143–154. ( 10.2174/1874325001610010143) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oestreich AE Young LW & Young Poussaint T. Scoliosis circa 2000: radiologic imaging perspective. I. Diagnosis and pretreatment evaluation. Skeletal Radiology 199827591–605. ( 10.1007/s002560050445) [DOI] [PubMed] [Google Scholar]
- 33.Reamy BV & Slakey JB. Adolescent idiopathic scoliosis: review and current concepts. American Family Physician 200164111–116. [PubMed] [Google Scholar]
- 34.Aebi M. The adult scoliosis. European Spine Journal 200514925–948. ( 10.1007/s00586-005-1053-9) [DOI] [PubMed] [Google Scholar]
- 35.Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, Ryan DJ, Hostin R, Hart R, Burton D, et al.TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. Journal of Bone and Joint Surgery 2014961631–1640. ( 10.2106/JBJS.M.01459) [DOI] [PubMed] [Google Scholar]
- 36.Roussouly P Gollogly S Berthonnaud E & Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 200530346–353. ( 10.1097/01.brs.0000152379.54463.65) [DOI] [PubMed] [Google Scholar]
- 37.Passias PG, Bortz C, Pierce KE, Passfall L, Kummer NA, Krol O, Lafage R, Diebo BG, Lafage V, Ames CP, et al.Comparing and contrasting the clinical utility of sagittal spine alignment classification frameworks: Roussouly versus SRS-Schwab. Spine 202247455–462. ( 10.1097/BRS.0000000000004300) [DOI] [PubMed] [Google Scholar]
- 38.Rowe DE. The Scoliosis Res earch Society Brace Manual. https://www.srs.org/Files/Research/Manuals-and-Publications/SRS_Bracking_Manual.pdf. Accessed May 11, 2024. [Google Scholar]
- 39.Rafferty A Fleming N Kiely P Mockler D & Dockrell S. Does exercise therapy improve pulmonary function in patients with Adolescent Idiopathic Scoliosis? Physiotherapy Theory and Practice 2023391095–1105. ( 10.1080/09593985.2022.2034198) [DOI] [PubMed] [Google Scholar]
- 40.Walker CT Agarwal N Eastlack RK Mundis GM Alan N Iannacone T Akbarnia BA & Okonkwo DO. Surgical treatment of young adults with idiopathic scoliosis. Journal of Neurosurgery 20233884–90. ( 10.3171/2022.7.SPINE2298) [DOI] [PubMed] [Google Scholar]
- 41.Berdishevsky H, Lebel VA, Bettany-Saltikov J, Rigo M, Lebel A, Hennes A, Romano M, Białek M, M’hango A, Betts T, et al.Physiotherapy scoliosis-specific exercises: a comprehensive review of seven major schools. Scoliosis and Spinal Disorders 20161120. ( 10.1186/s13013-016-0076-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Day JM Fletcher J Coghlan M & Ravine T. Review of scoliosis-specific exercise methods used to correct adolescent idiopathic scoliosis. Arch Physiother 201998. ( 10.1186/s40945-019-0060-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dobosiewicz K Durmala J Czernicki K & Jendrzejek H. Pathomechanic basics of conservative treatment of progressive idiopathic scoliosis according to Dobosiewicz method based upon radiologic evaluation. Studies in Health Technology and Informatics 200291336–341. [PubMed] [Google Scholar]
- 44.Karavidas N & Tzatzaliaris D. Brace and physiotherapeutic scoliosis specific exercises (PSSE) for adolescent idiopathic scoliosis (AIS) treatment: a prospective study following scoliosis research society (SRS) criteria. Arch Physiother 20221222. ( 10.1186/s40945-022-00150-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lehnert-Schroth C. Introduction to the three-dimensional scoliosis treatment according to Schroth. Physiotherapy 199278810–815. ( 10.1016/S0031-9406(1060451-8) [DOI] [Google Scholar]
- 46.Romano M Negrini A Parzini S Tavernaro M Zaina F Donzelli S & Negrini S. SEAS (Scientific Exercises Approach to Scoliosis): a modern and effective evidence based approach to physiotherapic specific scoliosis exercises. Scoliosis 2015103. ( 10.1186/s13013-014-0027-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dureigne F Chagnas MO Roren A Couzi E Lefèvre-Colau MM Moreau S Nicol V Rannou F Daste C & Nguyen C. Barriers and facilitators to bracing in adults with painful degenerative scoliosis: a single-centred mixed-method feasibility study. BMC Musculoskeletal Disorders 20232432. ( 10.1186/s12891-022-06111-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palazzo C Montigny JP Barbot F Bussel B Vaugier I Fort D Courtois I & Marty-Poumarat C. Effects of bracing in adult with scoliosis: a retrospective study. Archives of Physical Medicine and Rehabilitation 201798187–190. ( 10.1016/j.apmr.2016.05.019) [DOI] [PubMed] [Google Scholar]
- 49.Zaina F Poggio M Di Felice F Donzelli S & Negrini S. Bracing adults with chronic low back pain secondary to severe scoliosis: six months results of a prospective pilot study. European Spine Journal 2021302962–2966. ( 10.1007/s00586-021-06808-1) [DOI] [PubMed] [Google Scholar]
- 50.McAviney J Mee J Fazalbhoy A Du Plessis J & Brown BT. A systematic literature review of spinal brace/orthosis treatment for adults with scoliosis between 1967 and 2018: clinical outcomes and harms data. BMC Musculoskeletal Disorders 20202187. ( 10.1186/s12891-020-3095-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mayo NE Goldberg MS Poitras B Scott S & Hanley J. The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study. Part III: back pain. Spine 1994191573–1581. ( 10.1097/00007632-199407001-00005) [DOI] [PubMed] [Google Scholar]
- 52.Weinstein SL Dolan LA Spratt KF Peterson KK Spoonamore MJ & Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003289559–567. ( 10.1001/jama.289.5.559) [DOI] [PubMed] [Google Scholar]
- 53.Erşen Ö Yüzügüldü U Başak AM Güveli R & Ege T. Effect of clinical and radiological parameters on the quality of life in adult patients with untreated adolescent idiopathic scoliosis: a cross-sectional study. European Spine Journal 2023321196–1203. ( 10.1007/s00586-023-07571-1) [DOI] [PubMed] [Google Scholar]
- 54.Pan X Qiao J Liu Z Shi B Mao S Li S Sun X Zhu Z & Qiu Y. Posterior-only correction surgery for idiopathic scoliosis Lenke type 5c: differences of strategies and outcomes between adult patients and adolescent patients. Spine Deformity 202311665–670. ( 10.1007/s43390-023-00647-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dolan L & Weinstein S. Health, function, quality of life and self-esteem in AIS; preliminary results from BrAIST. Scoliosis 20149(Supplement 1) O80. ( 10.1186/1748-7161-9-S1-O80) [DOI] [Google Scholar]
- 56.Durand WM, Babu JM, Hamilton DK, Passias PG, Kim HJ, Protopsaltis T, Lafage V, Lafage R, Smith JS, Shaffrey C, et al.Adult spinal deformity surgery is associated with increased productivity and decreased absenteeism from work and school. Spine 202247287–294. ( 10.1097/BRS.0000000000004271) [DOI] [PubMed] [Google Scholar]
- 57.Belli G Toselli S Latessa PM & Mauro M. Evaluation of self-perceived body image in adolescents with mild idiopathic scoliosis. European Journal of Investigation in Health, Psychology and Education 202212319–333. ( 10.3390/ejihpe12030023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Danielsson AJ Wiklund I Pehrsson K & Nachemson AL. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. European Spine Journal 200110278–288. ( 10.1007/s005860100309) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Payne WK Ogilvie JW Resnick MD Kane RL Transfeldt EE & Blum RW. Does scoliosis have a psychological impact and does gender make a difference? Spine 1997221380–1384. ( 10.1097/00007632-199706150-00017) [DOI] [PubMed] [Google Scholar]
- 60.Tones M Moss N & Polly DW. A review of quality of life and psychosocial issues in scoliosis. Spine 2006313027–3038. ( 10.1097/01.brs.0000249555.87601.fc) [DOI] [PubMed] [Google Scholar]
- 61.Lin T Meng Y Ji Z Jiang H Shao W Gao R & Zhou X. Extent of depression in juvenile and adolescent patients with idiopathic scoliosis during treatment with braces. World Neurosurgery 2019126e27–e32. ( 10.1016/j.wneu.2019.01.095) [DOI] [PubMed] [Google Scholar]
- 62.Noonan KJ Dolan LA Jacobson WC & Weinstein SL. Long-term psychosocial characteristics of patients treated for idiopathic scoliosis. Journal of Pediatric Orthopedics 199717712–717. ( 10.1097/01241398-199711000-00004) [DOI] [PubMed] [Google Scholar]
- 63.Sucato DJ. Long-term outcome for scoliosis is dependent on several factors: commentary on an article by Elias Diarbakerli, PT, MSc, et al.: “health-related quality of life in adulthood in untreated and treated individuals with adolescent or juvenile idiopathic scoliosis”. Journal of Bone and Joint Surgery 2018100e71. ( 10.2106/JBJS.18.00180) [DOI] [PubMed] [Google Scholar]
- 64.Bess S, Boachie-Adjei O, Burton D, Cunningham M, Shaffrey C, Shelokov A, Hostin R, Schwab F, Wood K, Akbarnia B, et al.Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 2009342186–2190. ( 10.1097/BRS.0b013e3181b05146) [DOI] [PubMed] [Google Scholar]
- 65.Cheng JC Qin L Cheung CS Sher AH Lee KM Ng SW & Guo X. Generalized low areal and volumetric bone mineral density in adolescent idiopathic scoliosis. Journal of Bone and Mineral Research 2000151587–1595. ( 10.1359/jbmr.2000.15.8.1587) [DOI] [PubMed] [Google Scholar]
- 66.Cheng JCY Hung VWY Lee WTK Yeung HY Lam TP Ng BKW Guo X & Qin L. Persistent osteopenia in adolescent idiopathic scoliosis: longitudinal monitoring of bone mineral density until skeletal maturity. Studies in Health Technology and Informatics 200612347–51. [PubMed] [Google Scholar]
- 67.Li XF Li H Liu ZD & Dai LY. Low bone mineral status in adolescent idiopathic scoliosis. European Spine Journal 2008171431–1440. ( 10.1007/s00586-008-0757-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Courtois I Collet P Mouilleseaux B & Alexandre C. Bone mineral density at the femur and lumbar spine in a population of young women treated for scoliosis in adolescence. Revue du Rhumatisme 199966705–710. [PubMed] [Google Scholar]
- 69.Suzuki S, Fujiwara H, Nori S, Tsuji O, Nagoshi N, Okada E, Fujita N, Yagi M, Nohara A, Kawakami N, et al.Residual lumbar curvature that developed during adolescence accelerates intervertebral disc degeneration in adulthood. Spine Deformity 20219711–720. ( 10.1007/s43390-020-00252-9) [DOI] [PubMed] [Google Scholar]
- 70.Pehrsson K Larsson S Oden A & Nachemson A. Long-term follow-up of patients with untreated scoliosis a study of mortality, causes of death, and symptoms. Spine 1992171091–1096. ( 10.1097/00007632-199209000-00014) [DOI] [PubMed] [Google Scholar]
- 71.Blount WP & Mellencamp D. The effect of pregnancy on idiopathic scoliosis. Journal of Bone and Joint Surgery 1980621083–1087. ( 10.2106/00004623-198062070-00005) [DOI] [PubMed] [Google Scholar]
- 72.Danielsson AJ & Nachemson AL. Childbearing, curve progression, and sexual function in women 22 years after treatment for adolescent idiopathic scoliosis: a case–control study. Spine 2001261449–1456. ( 10.1097/00007632-200107010-00015) [DOI] [PubMed] [Google Scholar]
- 73.Orvomaa E Hiilesmaa V Poussa M Snellman O & Tallroth K. Pregnancy and delivery in patients operated by the Harrington method for idiopathic scoliosis. European Spine Journal 19976304–307. ( 10.1007/BF01142675) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Swany L Larson AN Shah SA Grabala P Milbrandt T & Yaszemski MJ. Outcomes of pregnancy in operative vs. nonoperative adolescent idiopathic scoliosis patients at mean 30-year follow-up. Spine Deformity 202081169–1174. ( 10.1007/s43390-020-00158-6) [DOI] [PubMed] [Google Scholar]
- 75.Geck MJ Rinella A Hawthorne D Macagno A Koester L Sides B Bridwell K Lenke L & Shufflebarger H. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine 2009341942–1951. ( 10.1097/BRS.0b013e3181a3c777) [DOI] [PubMed] [Google Scholar]
- 76.Vigneswaran HT Grabel ZJ Eberson CP Palumbo MA & Daniels AH. Surgical treatment of adolescent idiopathic scoliosis in the United States from 1997 to 2012: an analysis of 20, 346 patients. Journal of Neurosurgery 201516322–328. ( 10.3171/2015.3.PEDS14649) [DOI] [PubMed] [Google Scholar]
- 77.Von Heideken J Iversen MD & Gerdhem P. Rapidly increasing incidence in scoliosis surgery over 14 years in a nationwide sample. European Spine Journal 201827286–292. ( 10.1007/s00586-017-5346-6) [DOI] [PubMed] [Google Scholar]
- 78.Lin Y Chen W Chen A Li F & Xiong W. Anterior versus posterior selective fusion in treating adolescent idiopathic scoliosis: a systematic review and meta-analysis of radiologic parameters. World Neurosurgery 2018111e830–e844. ( 10.1016/j.wneu.2017.12.161) [DOI] [PubMed] [Google Scholar]
- 79.Coe JD Arlet V Donaldson W Berven S Hanson DS Mudiyam R Perra JH & Shaffrey CI. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium: a report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine 200631345–349. ( 10.1097/01.brs.0000197188.76369.13) [DOI] [PubMed] [Google Scholar]
- 80.Burton DC, Carlson BB, Place HM, Fuller JE, Blanke K, Cho R, Fu KM, Ganju A, Heary R, Herrera-Soto JA, et al.Results of the Scoliosis Research Society morbidity and mortality database 2009–2012: a report from the Morbidity and Mortality Committee. Spine Deformity 20164338–343. ( 10.1016/j.jspd.2016.05.003) [DOI] [PubMed] [Google Scholar]
- 81.Kim YJ Lenke LG Bridwell KH Kim J Cho SK Cheh G & Yoon J. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine 2007322731–2738. ( 10.1097/BRS.0b013e31815a7ead) [DOI] [PubMed] [Google Scholar]
- 82.Lee GA Betz RR Clements DH & Huss GK. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine 199924795–799. ( 10.1097/00007632-199904150-00011) [DOI] [PubMed] [Google Scholar]
- 83.Lonner BS Ren Y Newton PO Shah SA Samdani AF Shufflebarger HL Asghar J Sponseller P Betz RR & Yaszay B. Risk factors of proximal junctional kyphosis in adolescent idiopathic scoliosis—the pelvis and other considerations. Spine Deformity 20175181–188. ( 10.1016/j.jspd.2016.10.003) [DOI] [PubMed] [Google Scholar]
- 84.Yagi M Akilah KB & Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine 201136E60–E68. ( 10.1097/BRS.0b013e3181eeaee2) [DOI] [PubMed] [Google Scholar]
- 85.Weiss HR & Goodall D. Rate of complications in scoliosis surgery: a systematic review of the Pub Med literature. Scoliosis 200839. ( 10.1186/1748-7161-3-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Matsumoto H Colacchio ND Schwab FJ Lafage V Roye DP & Vitale MG. Flatback revisited: reciprocal loss of lumbar lordosis following selective thoracic fusion in the setting of adolescent idiopathic scoliosis. Spine Deformity 20153345–351. ( 10.1016/j.jspd.2015.01.004) [DOI] [PubMed] [Google Scholar]
- 87.Kim HJ Bridwell KH Lenke LG Park MS Ahmad A Song KS Piyaskulkaew C Hershman S Fogelson J & Mesfin A. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine 201338896–901. ( 10.1097/BRS.0b013e3182815b42) [DOI] [PubMed] [Google Scholar]
- 88.Kim YJ Bridwell KH Lenke LG Kim J & Cho SK. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine 2005302045–2050. ( 10.1097/01.brs.0000179084.45839.ad) [DOI] [PubMed] [Google Scholar]
- 89.Wiggins GC Ondra SL & Shaffrey CI. Management of iatrogenic flat-back syndrome. Neurosurgical Focus 200315E8. ( 10.3171/foc.2003.15.3.8) [DOI] [PubMed] [Google Scholar]
- 90.Lu DC & Chou D. Flatback syndrome. Neurosurgery Clinics of North America 200718289–294. ( 10.1016/j.nec.2007.01.007) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a