Abstract
Purpose
To investigate the association between the oxidative balance score (OBS) and endometriosis.
Methods
This cross-sectional study used four cycles of the National Health and Nutrition Examination Survey (NHANES) (1999–2000, 2001–2002, 2003–2004, and 2005–2006). OBS involved 16 dietary nutrients and 4 lifestyle factors, including 5 pro-oxidants and 15 anti-oxidants. According to weighted quartiles, the OBS was divided into four categories: < 12.54, 12.54–18.70, 18.71–24.68, and > 24.68. Endometriosis was diagnosed based on a question from the reproductive health questionnaire. Weighted multivariate logistic analysis was used to investigate the association between OBS and endometriosis. Subgroup analysis was performed based on menstrual regularity and female hormone use.
Results
A total of 5095 women were included, with 1140 (22.37%), 1232 (24.18%), 1224 (24.02%), and 1499 (29.42%) women in the OBS < 12.54, of 12.54–18.70, of 18.71–24.68, and > 24.68 categories, respectively. After adjusting age, race, family poverty-to-income ratio (PIR), education level, uterine fibroids, menstrual regularity, oophorectomy, female hormone use, hypertension, dyslipidemia, and steroid drug, a high OBS (> 24.68) was found to be associated with lower odds of endometriosis [odds ratio (OR) = 0.70, 95% confidence interval (CI): 0.50–0.97, P = 0.033] compared to a low OBS (< 12.54). The similar result was also found in women with irregular menstruation (OR = 0.58, 95% CI: 0.37–0.91, P = 0.020) and with female hormone use (OR = 0.71, 95% CI: 0.52–0.98, P = 0.037).
Conclusion
A high OBS was associated with lower odds of endometriosis, especially in women with irregular menstruation and female hormone use.
Keywords: Oxidative balance score, endometriosis, menstruation, female hormones, NHANES
Introduction
Endometriosis is a chronic gynecological disease and defined as the presence of endometrial tissue outside the uterus, which affects 5–10% of women of childbearing age.1,2 It can cause infertility, pelvic pain, deep dyspareunia, dyschezia, dysuria, and dysmenorrhea.3,4 Endometrial cell apoptosis and proliferation may be associated with the pathogenesis of endometriosis.4,5 In addition, oxidative stress and inflammation play an important role in the pathogenesis of endometriosis.6,7
Intake of dietary nutrients is closely related to the body’s oxidative balance and inflammatory status.8 Researches have found that nutrients relevant to anti-oxidant and anti-inflammatory effects, such as vitamins and minerals, may be protective factors for endometriosis, while pro-oxidant and pro-inflammatory factors such as total fat pose a risk to endometriosis.9–11 In addition, limited cross-sectional studies have shown that physical activity12 and tobacco exposure13 may be associated with the odds of endometriosis. Evidence suggests that multiple pro-oxidant and anti-oxidant factors may have a comprehensive impact on endometriosis.14 Recently, oxidative balance score (OBS), which includes multiple pro-oxidant and anti-oxidant factors [nutrients, physical activity, body mass index (BMI), tobacco, and alcohol] and comprehensively reflects the oxidative status related to lifestyle, has been reported in studies on inflammation-related chronic diseases.15,16 Higher OBS indicates a better oxidative balance.15,16 Nevertheless, the relationship between the OBS and endometriosis remains unknown yet.
To bridge the above research gap, this study aimed to explore the association between the OBS and endometriosis, using the data from the National Health and Nutrition Examination Survey (NHANES). Subgroup analysis was further conducted based on menstrual regularity and female hormone use to show if or how the association differed among different subpopulations.
Methods
Study Population
In this cross-sectional study, data for analysis were extracted from the four cycles of NHANES (1999–2000, 2001–2002, 2003–2004, and 2005–2006). The NHANES is a cross-sectional survey, which uses a multilayered probability sampling design and collects demographic, clinical, behavioral, dietary, social, and laboratory data on the health and nutritional status of the non-institutionalized population in the United States.17 Women aged 20–54 years were investigated for endometriosis in the NHANES. Inclusion criteria: (1) women with assessment of endometriosis; (2) women with information for OBS calculation. Exclusion criteria: women without data on education level, menstrual regularity and C-reactive protein (CRP). Ethical approval was waived by the Institutional Review Board of the First Affiliated Hospital of Ningbo University because NHANES was a publicly available database. Written informed consent was not required for this study given that data in the NHANES database have been de-identified.
OBS Calculation
Calculation of OBS involved 16 dietary nutrients and 4 lifestyle factors, including 5 pro-oxidants and 15 anti-oxidants. For alcohol consumption, non-drinkers, non-heavy drinkers (0–15 g/d for female and 0–30 g/d for male), and heavy drinkers (≥ 15 g/d for female and ≥ 30 g/d for male) received 2, 1, and 0 points, respectively. Then, other components were divided into three groups by the sex-specific tertiles. Anti-oxidants were assigned points from 0 to 2 for groups from tertile 1 to tertile 3, respectively. The point assignment for pro-oxidants was inverse, with 0 points for the highest tertile and 2 points for the lowest tertile.18,19 The sum of all points was OBS, ranging from 0 to 40 points. According to weighted quartiles, the OBS was divided into four categories: < 12.54, 12.54–18.70, 18.71–24.68, and > 24.68.
Endometriosis Assessment
Endometriosis was diagnosed based on a question from the reproductive health questionnaire “Has a doctor or other health professional ever told you that you had endometriosis?” Participants who answered “yes” were regarded to have endometriosis. Those who answered “no” were considered as controls without endometriosis.
Study Covariates
The following covariates were extracted: age (years), race (Mexican American, non-Hispanic Black, non-Hispanic White, other Hispanic, other race), family poverty-to-income ratio (PIR) (< 1.3, 1.3–3.5, > 3.5, unknown), education level [less than 12th grade, high school graduate/general education development (GED) or equivalent, some college or associate (AA) degree or above], marital status (married, unmarried, unknown), age at menarche (≤ 11, 12–13, ≥ 14, unknown), ever pregnant (no, yes), uterine fibroids (no, yes, unknown), menstrual regularity (no, yes), oophorectomy (no, yes), female hormone use (no, yes), hypertension (no, yes), diabetes (no, yes), dyslipidemia (no, yes), hyperuricemia (no, yes), cardiovascular disease (CVD) (no, yes), CRP (mg/dL), steroid drug (no, yes), and energy (kcal). Uterine fibroids were determined if participants gave a positive answer to the question “Has a doctor or other health professional ever told you that you had uterine fibroids?” Oophorectomy was determined if participants answered “Yes” to the question “Had at least one ovary removed?” Diabetes was defined as any of the following: HbA1c ≥ 6.5%, fasting glucose ≥ 126mg/dL, any self-reported diagnosis of diabetes, or any self-reported use of insulin or other diabetes medication. CVD was defined as self-reported coronary heart disease, angina, heart failure, heart attack, stroke, or determined according to cardiovascular drug codes.
Statistical Analysis
Numerical data were described as mean ± standard error (Mean ± SE), and differences among groups were compared using analysis of variance. Categorical data were described as frequency and percentage [n (%)], and differences among groups were compared using the chi-square test. Weighted univariate logistic analysis was performed to identify covariates affecting endometriosis and to explore the association between OBS and endometriosis. Weighted multivariate logistic analysis was then used to investigate the association between OBS and endometriosis by adjusting age, race, family PIR, education level, uterine fibroids, menstrual regularity, oophorectomy, female hormone use, hypertension, dyslipidemia, and steroid drug. The results of weighted univariate and multivariate logistic analysis were shown as odds ratios (ORs) and 95% confidence intervals (CIs). Subgroup analysis was performed based on menstrual regularity and female hormone use. SAS 9.4 (SAS Institute Inc., Cary, NC, USA) was applied for data extraction, data cleaning, statistical analysis, and table output. R 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria) was used to generate forest plots for subgroup analysis. P value less than 0.05 was considered as statistical significance.
Results
Participant Characteristics
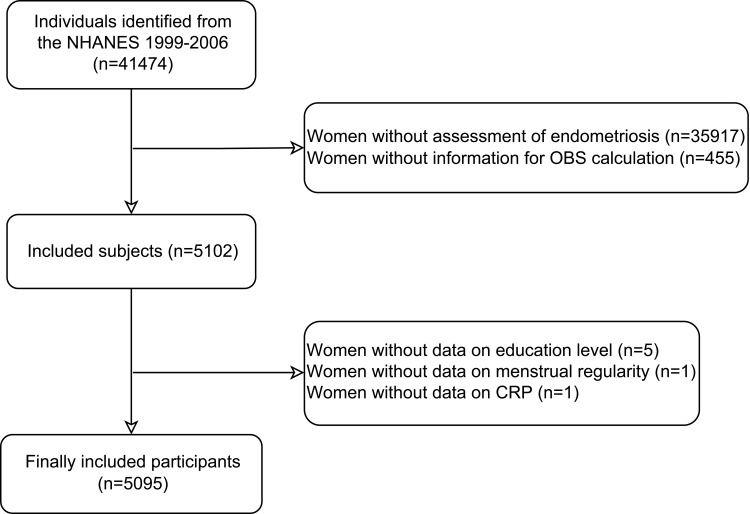
A total of 41,474 individuals were identified. After excluding women without assessment of endometriosis (n=35917), without information for OBS calculation (n=455), and without data on education level (n=5), menstrual regularity (n=1) and CRP (n=1), 5,095 women were finally included in this study (Figure 1). Table 1 exhibits the characteristics of these participants. There were 1,140 (22.37%), 1,232 (24.18%), 1,224 (24.02%), and 1,499 (29.42%) women in the OBS < 12.54, of 12.54–18.70, of 18.71–24.68, and > 24.68 categories, respectively. The included women had a mean age of 37.68 (0.19) years, and 9.24% of them (n = 355) had endometriosis. Most women were non-Hispanic White people (68.84%), had a family PIR of over 3.5 (41.51%), had an education level of some college or AA degree or above (61.34%), and were married (55.90%). Significant differences were observed in race, family PIR, education level, marital status, ever pregnant status, uterine fibroids, menstrual regularity, oophorectomy, hypertension, hyperuricemia, CRP, and energy among the four OBS categories (all P < 0.05).
Figure 1.
Flow chart of participant selection.
NHANES, the National Health and Nutrition Examination Survey; OBS, oxidative balance score; CRP, C-reactive protein.
Table 1.
Characteristics of Participants in Four OBS Categories
| Variables | Total (n=5095) |
OBS | Statistics | P | |||
|---|---|---|---|---|---|---|---|
| < 12.54 (n=1140) |
12.54–18.70 (n=1232) |
18.71–24.68 (n=1224) |
> 24.68 (n=1499) |
||||
| Age, years, Mean (SE) | 37.68 (0.19) | 37.71 (0.39) | 37.85 (0.39) | 37.76 (0.33) | 37.42 (0.31) | F=0.30 | 0.827 |
| Race, n (%) | χ2=70.378 | <0.001 | |||||
| Mexican American | 1231 (8.34) | 239 (7.31) | 314 (9.09) | 304 (8.25) | 374 (8.59) | ||
| Non-Hispanic Black | 1022 (11.87) | 331 (17.24) | 287 (14.22) | 207 (9.26) | 197 (7.72) | ||
| Non-Hispanic White | 2374 (68.84) | 467 (64.71) | 520 (64.82) | 587 (69.99) | 800 (74.74) | ||
| Other Hispanic | 246 (5.71) | 55 (5.28) | 69 (7.14) | 68 (6.58) | 54 (4.05) | ||
| Other race - including multi-racial | 222 (5.24) | 48 (5.46) | 42 (4.72) | 58 (5.92) | 74 (4.91) | ||
| Family PIR, n (%) | χ2=102.449 | <0.001 | |||||
| < 1.3 | 1377 (20.48) | 397 (29.23) | 342 (22.26) | 318 (18.41) | 320 (13.57) | ||
| 1.3–3.5 | 1737 (32.90) | 404 (34.29) | 412 (31.43) | 421 (34.77) | 500 (31.36) | ||
| > 3.5 | 1667 (41.51) | 262 (31.00) | 393 (41.23) | 409 (41.42) | 603 (50.48) | ||
| Unknown | 314 (5.11) | 77 (5.48) | 85 (5.09) | 76 (5.40) | 76 (4.59) | ||
| Education level, n (%) | χ2=116.848 | <0.001 | |||||
| Less than 12th grade | 1225 (15.42) | 345 (22.16) | 316 (17.15) | 266 (13.00) | 298 (10.52) | ||
| High school graduate/GED or equivalent | 1129 (23.24) | 310 (28.83) | 295 (24.96) | 278 (23.10) | 246 (17.27) | ||
| Some college or AA degree or above | 2741 (61.34) | 485 (49.02) | 621 (57.89) | 680 (63.90) | 955 (72.21) | ||
| Marital status, n (%) | χ2=21.432 | 0.002 | |||||
| Married | 2756 (55.90) | 506 (49.45) | 660 (56.85) | 648 (53.73) | 942 (62.30) | ||
| Unmarried | 2195 (41.42) | 594 (47.68) | 533 (40.57) | 548 (43.89) | 520 (34.81) | ||
| Unknown | 144 (2.68) | 40 (2.87) | 39 (2.59) | 28 (2.38) | 37 (2.88) | ||
| Age at menarche, n (%) | χ2=9.888 | 0.360 | |||||
| ≤ 11 | 1158 (21.79) | 279 (23.08) | 269 (21.26) | 272 (21.64) | 338 (21.32) | ||
| 12–13 | 2600 (52.73) | 563 (52.63) | 643 (52.35) | 631 (54.07) | 763 (51.96) | ||
| ≥ 14 | 1252 (23.64) | 273 (21.82) | 297 (24.59) | 310 (23.54) | 372 (24.40) | ||
| Unknown | 85 (1.84) | 25 (2.46) | 23 (1.80) | 11 (0.75) | 26 (2.32) | ||
| Ever pregnant, n (%) | χ2=30.274 | <0.001 | |||||
| No | 780 (19.57) | 151 (14.64) | 175 (16.73) | 205 (22.09) | 249 (23.87) | ||
| Yes | 4315 (80.43) | 989 (85.36) | 1057 (83.27) | 1019 (77.91) | 1250 (76.13) | ||
| Uterine fibroids, n (%) | χ2=14.042 | 0.029 | |||||
| No | 4446 (85.77) | 1001 (87.32) | 1041 (83.15) | 1061 (84.60) | 1343 (87.83) | ||
| Yes | 633 (13.98) | 137 (12.42) | 188 (16.74) | 158 (15.00) | 150 (11.92) | ||
| Unknown | 16 (0.25) | 2 (0.26) | 3 (0.11) | 5 (0.40) | 6 (0.25) | ||
| Menstrual regularity, n (%) | χ2=16.095 | 0.001 | |||||
| No | 1888 (35.14) | 458 (40.59) | 469 (36.97) | 427 (31.93) | 534 (31.91) | ||
| Yes | 3207 (64.86) | 682 (59.41) | 763 (63.03) | 797 (68.07) | 965 (68.09) | ||
| Oophorectomy, n (%) | χ2=20.727 | <0.001 | |||||
| No | 4691 (89.93) | 1018 (87.50) | 1111 (87.36) | 1135 (91.13) | 1427 (93.10) | ||
| Yes | 404 (10.07) | 122 (12.50) | 121 (12.64) | 89 (8.87) | 72 (6.90) | ||
| Female hormone use, n (%) | χ2=3.449 | 0.327 | |||||
| No | 1117 (17.26) | 246 (15.25) | 282 (18.42) | 269 (17.83) | 320 (17.38) | ||
| Yes | 3978 (82.74) | 894 (84.75) | 950 (81.58) | 955 (82.17) | 1179 (82.62) | ||
| Hypertension, n (%) | χ2=9.786 | 0.020 | |||||
| No | 3989 (76.98) | 843 (72.89) | 943 (77.23) | 964 (77.60) | 1239 (79.56) | ||
| Yes | 1106 (23.02) | 297 (27.11) | 289 (22.77) | 260 (22.40) | 260 (20.44) | ||
| Diabetes, n (%) | χ2=1.455 | 0.693 | |||||
| No | 4795 (94.97) | 1067 (94.36) | 1153 (95.06) | 1154 (95.53) | 1421 (94.87) | ||
| Yes | 300 (5.03) | 73 (5.64) | 79 (4.94) | 70 (4.47) | 78 (5.13) | ||
| Dyslipidemia, n (%) | χ2=4.485 | 0.214 | |||||
| No | 2173 (45.58) | 493 (41.88) | 538 (45.92) | 549 (47.29) | 593 (46.79) | ||
| Yes | 2922 (54.42) | 647 (58.12) | 694 (54.08) | 675 (52.71) | 906 (53.21) | ||
| Hyperuricemia, n (%) | χ2=12.705 | 0.005 | |||||
| No | 4641 (90.21) | 997 (87.60) | 1115 (90.03) | 1127 (91.30) | 1402 (91.53) | ||
| Yes | 454 (9.79) | 143 (12.40) | 117 (9.97) | 97 (8.70) | 97 (8.47) | ||
| CVD, n (%) | χ2=4.944 | 0.176 | |||||
| No | 4468 (86.30) | 971 (84.21) | 1062 (86.09) | 1076 (86.55) | 1359 (87.98) | ||
| Yes | 627 (13.70) | 169 (15.79) | 170 (13.91) | 148 (13.45) | 140 (12.02) | ||
| CRP, mg/dL, Mean (SE) | 0.49 (0.02) | 0.55 (0.03) | 0.45 (0.02) | 0.47 (0.03) | 0.48 (0.03) | F=3.36 | 0.025 |
| Steroid drug, n (%) | χ2=0.415 | 0.937 | |||||
| No | 5038 (98.74) | 1125 (98.50) | 1219 (98.80) | 1210 (98.80) | 1484 (98.84) | ||
| Yes | 57 (1.26) | 15 (1.50) | 13 (1.20) | 14 (1.20) | 15 (1.16) | ||
| Energy, kcal, Mean (SE) | 1944.23 (12.77) | 1329.75 (17.41) | 1678.88 (18.11) | 2094.10 (21.98) | 2548.23 (26.74) | F=490.24 | <0.001 |
| Endometriosis, n (%) | χ2=5.758 | 0.124 | |||||
| No | 4740 (90.76) | 1051 (88.99) | 1138 (89.87) | 1145 (91.28) | 1406 (92.54) | ||
| Yes | 355 (9.24) | 89 (11.01) | 94 (10.13) | 79 (8.72) | 93 (7.46) | ||
Notes: According to weighted quartiles, the OBS was divided into four categories: < 12.54, 12.54–18.70, 18.71–24.68, and > 24.68.
Abbreviations: OBS, oxidative balance score; PIR, poverty-to-income ratio; GED, general education development; AA, associate; CVD, cardiovascular disease; CRP, C-reactive protein; SE, standard error.
Association Between the OBS and Endometriosis
As illustrated in Table 2, compared to a low OBS (< 12.54), a high OBS (> 24.68) was associated with the lower odds of endometriosis (OR = 0.70, 95% CI: 0.50–0.97, P = 0.033) after adjusting age, race, family PIR, education level, uterine fibroids, menstrual regularity, oophorectomy, female hormone use, hypertension, dyslipidemia, and steroid drug (Supplementary Table S1).
Table 2.
Association Between the OBS and Endometriosis
| OBS | Model 1 | Model 2 | ||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| < 12.54 | Ref | Ref | ||
| 12.54–18.70 | 0.91 (0.61–1.36) | 0.644 | 0.84 (0.55–1.27) | 0.391 |
| 18.71–24.68 | 0.77 (0.51–1.17) | 0.217 | 0.79 (0.52–1.20) | 0.267 |
| > 24.68 | 0.65 (0.46–0.93) | 0.018 | 0.70 (0.50–0.97) | 0.033 |
Notes: Model 1, a univariate model; Model 2, a multivariate model, adjusting age, race, family PIR, education level, uterine fibroids, menstrual regularity, oophorectomy, female hormone use, hypertension, dyslipidemia, and steroid drug.
Abbreviations: OBS, oxidative balance score; PIR, poverty-to-income ratio; OR, odds ratio; CI, confidence interval; Ref, reference.
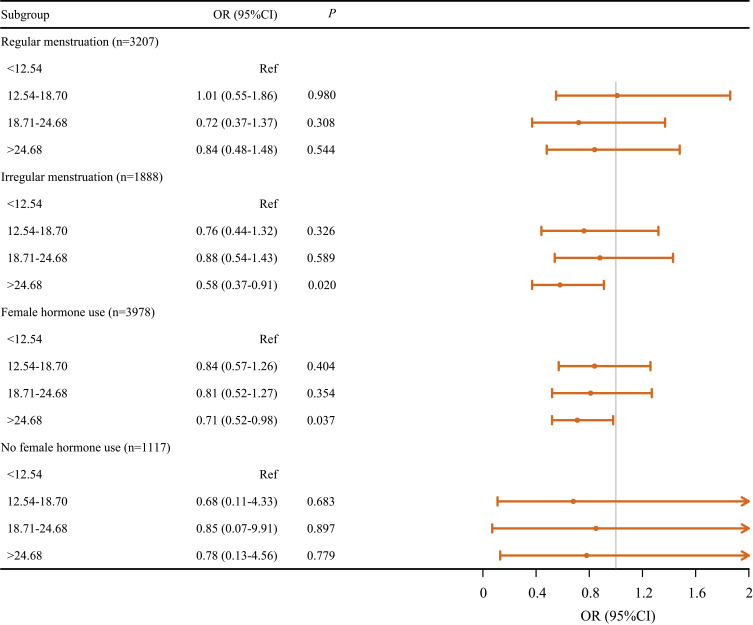
Association Between the OBS and Endometriosis by Menstrual Regularity and Female Hormone Use
In women with irregular menstruation (OR = 0.58, 95% CI: 0.37–0.91, P = 0.020) or with female hormone use (OR = 0.71, 95% CI: 0.52–0.98, P = 0.037), a high OBS (> 24.68) was associated with lower odds of endometriosis in contrast to a low OBS (< 12.54) (Figure 2).
Figure 2.
Association between the OBS and endometriosis by menstrual regularity and female hormone use.
Abbreviations: OR, odds ratio; CI, confidence interval; Ref, reference.
Discussion
The occurrence of endometriosis can be affected by oxidative stress and inflammation.6,7 The current study first explored the association between the OBS (a score combining pro-oxidants and anti-oxidants) and endometriosis. Results demonstrated that compared to a low OBS, a high OBS was associated with the lower odds of endometriosis, especially in women with irregular menstruation and female hormone use. These findings indicated that managing oxidative status in dietary intake and lifestyle may reduce the odds of endometriosis.
The OBS is calculated by incorporating 16 dietary nutrients and 4 lifestyle factors, including 5 pro-oxidants and 15 anti-oxidants.20 According to a previous review, excessive oxidative stress reflected by a lower OBS had deleterious effects on health, and the OBS was related to a decreased risk of CVD, chronic kidney disease, colorectal adenomas, and different cancer types (colorectal and breast cancer).21 Liu et al22 reported the association between the OBS and the risk of nonalcoholic fatty liver disease, and OBS may exert a protective effect indirectly through inflammation, oxidative stress, and glycolipid metabolism markers. Several studies have explored the association between the OBS and inflammation-related chronic diseases, such as hypertension, periodontitis and diabetes.15,16,18,23 Endometriosis is a disease characterized by chronic inflammation and can be affected by oxidative stress.24,25 This study investigated the relationship between the OBS and the odds of endometriosis, and found that high OBS was associated with a decreased odds of endometriosis, suggesting that a preference for antioxidant choices in diet nutrition and lifestyle may be beneficial.
Regarding dietary nutrients in the OBS, reducing dietary fat and increasing dietary fiber have been shown to reduce the concentration of estrogen, suggesting a potential benefit for individuals with endometriosis, as it is an estrogen-dependent disease.26 Chadchan et al27 reported that some gut bacteria protected against endometriosis by fermenting fiber to produce short-chain fatty acids. Besides, a diet rich in fruits and vegetables include higher levels of pro-vitamin A nutrients (alpha-carotene, beta-carotene, beta-cryptoxanthin), and women with endometriosis have been reported to have lower intake of vitamin A than women without endometriosis.28 The dietary intakes of calcium, potassium, vitamins B12, B2, B6, and C are inversely related to the risk of endometriosis.29 As for lifestyle factors, physical activity plays an important role in the development of endometriosis. A previous study has shown that women with endometriosis had a significantly lower level of physical activity than those without endometriosis.30 Further, the size of endometriotic lesions was reported to be decreased after physical exercise regardless of the frequency, indicating that physical exercise could be beneficial for the treatment of endometriosis.31 Various pro-oxidant and anti-oxidant factors are comprehensively taken into consideration in the OBS, and the negative association between the OBS and endometriosis in this study reflected the relationship between oxidative status and endometriosis. Based on the value of the OBS, the odds of endometriosis could be assessed. With respect to women with irregular menstruation and who used female hormones, an increased OBS was associated with reduced odds of endometriosis. Irregular menstruation belongs to an inflammatory event,32 and use of female hormones may also facilitate the occurrence of endometriosis, which is a hormone-dependent disease.33 These populations should pay attention to menstruation management and female hormone use. Keeping balanced oxidative status in dietary intake and lifestyle might reduce the odds of endometriosis through monitoring the OBS.
A nationally representative sample was used in the present study to investigate the association between the OBS and endometriosis for the first time. It was suggested that intake of diet rich in antioxidants such as fiber, vitamin C and calcium and doing exercise may help manage the initiation of endometriosis. In addition, counseling dieticians about improving beneficial dietary structures may contribute to the prevention and control of endometriosis. Prospective studies are warranted for verification. There are some limitations that should be acknowledged. Firstly, this study adopts a cross-sectional design, so the causal relationship between the OBS and endometriosis could not be determined. Secondly, most of the data used are collected through questionnaire surveys, and there may be recall bias. Thirdly, due to limited information in the NHANES database, some potential confounding factors, such as family history of endometriosis, pelvic medication and surgical history, cannot be taken into consideration, which may affect the reliability of the results.
Conclusion
A high OBS was associated with the low odds of endometriosis, especially in women with irregular menstruation and female hormone use, indicating that managing oxidative status in dietary intake and lifestyle might lower the odds of endometriosis. Further research is needed to confirm these findings.
Funding Statement
This work was supported by the Ningbo Natural Science Foundation (Grant numbers: 2023J201); Medical and Health Project of Zhejiang Province (Grant numbers: 2023KY291); Ningbo Clinical Medical Research Center for Gynecological Diseases (Grant numbers: 2024L002).
Ethics Approval and Informed Consent
Ethical approval was waived by the Institutional Review Board of the First Affiliated Hospital of Ningbo University because NHANES was a publicly available database. Written informed consent was not required for this study given that data in the NHANES database have been de-identified.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Singh SS, Missmer SA, Tu FF. Endometriosis and Pelvic Pain for the Gastroenterologist. Gastroenterol Clin North Am. 2022;51(1):195–211. doi: 10.1016/j.gtc.2021.10.012 [DOI] [PubMed] [Google Scholar]
- 2.Horne AW, Missmer SA. Pathophysiology, diagnosis, and management of endometriosis. BMJ. 2022;379:e070750. [DOI] [PubMed] [Google Scholar]
- 3.Lukac S, Schmid M, Pfister K, Janni W, Schäffler H, Dayan D. Extragenital endometriosis in the differential diagnosis of non-gynecological diseases. Dtsch Arztebl Int. 2022;119(20):361–367. doi: 10.3238/arztebl.m2022.0176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaya C, Alay I, Guraslan H, et al. The role of serum caspase 3 levels in prediction of endometriosis severity. Gynecol Obstet Invest. 2018;83(6):576–585. doi: 10.1159/000489494 [DOI] [PubMed] [Google Scholar]
- 5.Guney G, Taskin MI, Laganà AS, et al. Neutrophil gelatinase-associated lipocalin serum level: a potential noninvasive biomarker of endometriosis? Medicine. 2023;102(41):e35539. doi: 10.1097/MD.0000000000035539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jiang L, Yan Y, Liu Z, Wang Y. Inflammation and endometriosis. Front Biosci. 2016;21(5):941–948. doi: 10.2741/4431 [DOI] [PubMed] [Google Scholar]
- 7.Clower L, Fleshman T, Geldenhuys WJ, Santanam N. Targeting oxidative stress involved in endometriosis and its pain. Biomolecules. 2022;12(8):1055. doi: 10.3390/biom12081055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galland L. Diet and inflammation. Nutr Clin Pract. 2010;25(6):634–640. doi: 10.1177/0884533610385703 [DOI] [PubMed] [Google Scholar]
- 9.Parazzini F, Viganò P, Candiani M, Fedele L. Diet and endometriosis risk: a literature review. Reprod Biomed Online. 2013;26(4):323–336. doi: 10.1016/j.rbmo.2012.12.011 [DOI] [PubMed] [Google Scholar]
- 10.Arab A, Karimi E, Vingrys K, Kelishadi MR, Mehrabani S, Askari G. Food groups and nutrients consumption and risk of endometriosis: a systematic review and meta-analysis of observational studies. Nutr J. 2022;21(1):58. doi: 10.1186/s12937-022-00812-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huijs E, Nap A. The effects of nutrients on symptoms in women with endometriosis: a systematic review. Reprod Biomed Online. 2020;41(2):317–328. doi: 10.1016/j.rbmo.2020.04.014 [DOI] [PubMed] [Google Scholar]
- 12.Bonocher CM, Montenegro ML, Rosa ESJC, Ferriani RA, Meola J. Endometriosis and physical exercises: a systematic review. Reprod Biol Endocrinol. 2014;12:4. doi: 10.1186/1477-7827-12-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bravi F, Parazzini F, Cipriani S, et al. Tobacco smoking and risk of endometriosis: a systematic review and meta-analysis. BMJ Open. 2014;4(12):e006325. doi: 10.1136/bmjopen-2014-006325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HJ, Lee HS, Kazmi SZ, et al. Familial risk for endometriosis and its interaction with smoking, age at menarche and body mass index: a population-based cohort study among siblings. Bjog. 2021;128(12):1938–1948. doi: 10.1111/1471-0528.16769 [DOI] [PubMed] [Google Scholar]
- 15.Lee JH, Son DH, Kwon YJ. Association between oxidative balance score and new-onset hypertension in adults: a community-based prospective cohort study. Front Nutr. 2022;9:1066159. doi: 10.3389/fnut.2022.1066159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Yuan H, Li Q, et al. Lifestyle-based oxidative balance score and its association with cardiometabolic health of the community-dwelling elderly: a cross-sectional secondary analysis. Front Cardiovasc Med. 2022;9:1000546. doi: 10.3389/fcvm.2022.1000546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prevention CfDCa. About the national health and nutrition examination survey;2022. Available from: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed July 22, 2024.
- 18.Qu H. The association between oxidative balance score and periodontitis in adults: a population-based study. Front Nutr. 2023;10:1138488. doi: 10.3389/fnut.2023.1138488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang W, Peng SF, Chen L, Chen HM, Cheng XE, Tang YH. Association between the oxidative balance score and telomere length from the national health and nutrition examination survey 1999-2002. Oxid Med Cell Longev. 2022;2022:1345071. doi: 10.1155/2022/1345071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hasani M, Alinia SP, Khazdouz M, et al. Oxidative balance score and risk of cancer: a systematic review and meta-analysis of observational studies. BMC Cancer. 2023;23(1):1143. doi: 10.1186/s12885-023-11657-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hernández-Ruiz Á, García-Villanova B, Guerra-Hernández E, Amiano P, Ruiz-Canela M, Molina-Montes E. A review of a priori defined oxidative balance scores relative to their components and impact on health outcomes. Nutrients. 2019;11(4):774. doi: 10.3390/nu11040774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu Y, Chen M. Dietary and lifestyle oxidative balance scores are independently and jointly associated with nonalcoholic fatty liver disease: a 20 years nationally representative cross-sectional study. Front Nutr. 2023;10:1276940. doi: 10.3389/fnut.2023.1276940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwon YJ, Park HM, Lee JH. Inverse association between oxidative balance score and incident type 2 diabetes mellitus. Nutrients. 2023;15(11):2497. doi: 10.3390/nu15112497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehedintu C, Plotogea MN, Ionescu S, Antonovici M. Endometriosis still a challenge. J Med Life. 2014;7(3):349–357. [PMC free article] [PubMed] [Google Scholar]
- 25.Amini L, Chekini R, Nateghi MR, et al. The effect of combined vitamin c and vitamin e supplementation on oxidative stress markers in women with endometriosis: A randomized, triple-blind placebo-controlled clinical trial. Pain Res Manag. 2021;2021:5529741. doi: 10.1155/2021/5529741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barnard ND, Holtz DN, Schmidt N, et al. Nutrition in the prevention and treatment of endometriosis: a review. Front Nutr. 2023;10:1089891. doi: 10.3389/fnut.2023.1089891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chadchan SB, Popli P, Ambati CR, et al. Gut microbiota-derived short-chain fatty acids protect against the progression of endometriosis. Life Sci Alliance. 2021;4(12):e202101224. doi: 10.26508/lsa.202101224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris HR, Eke AC, Chavarro JE, Missmer SA. Fruit and vegetable consumption and risk of endometriosis. Hum Reprod. 2018;33(4):715–727. doi: 10.1093/humrep/dey014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roshanzadeh G, Jahanian Sadatmahalleh S, Moini A, Mottaghi A, Rostami F. The relationship between dietary micronutrients and endometriosis: a case-control study. Int J Reprod Biomed. 2023;21(4):333–342. doi: 10.18502/ijrm.v21i4.13272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vahiddastjerdi M, Vaghar ME, Manesh AH. An evaluation of the effect of lifestyle on the incidence of endometriosis. Maedica. 2023;18(3):432–436. doi: 10.26574/maedica.2023.18.3.432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Montenegro ML, Bonocher CM, Meola J, et al. Effect of physical exercise on endometriosis experimentally induced in rats. Reprod Sci. 2019;26(6):785–793. doi: 10.1177/1933719118799205 [DOI] [PubMed] [Google Scholar]
- 32.Vercellini P, Bandini V, Viganò P, Ambruoso D, Cetera GE, Somigliana E. Proposal for targeted, neo-evolutionary-oriented secondary prevention of early-onset endometriosis and adenomyosis. Part II: medical interventions. Hum Reprod. 2024;39(1):18–34. doi: 10.1093/humrep/dead206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abramiuk M, Mertowska P, Frankowska K, et al. How can selected dietary ingredients influence the development and progression of endometriosis? Nutrients. 2024;16(1):154. doi: 10.3390/nu16010154 [DOI] [PMC free article] [PubMed] [Google Scholar]