Key message.
Muscular polyarteritis nodosa should be considered in patients with extremity pain without creatine kinase elevation.
Dear Editor, Polyarteritis nodosa (PAN) is a necrotizing arteritis of the medium to small arteries. The Chapel Hill consensus conference in 2012 defined PAN as necrotizing arteritis not involving glomerulonephritis or vasculitis in arterioles, capillaries or venules and not showing a relation with ANCA vasculitis [1]. PAN is more common in males, and the average age of onset is ∼50 years [2]. The skin, peripheral nerves, gastrointestinal tract, kidneys and testicles are mainly involved; however, any organ, except the lungs, could be affected [3]. Although PAN is a systemic disease, there are limited forms of PAN, such as cutaneous PAN [4]. PAN limited to the calf muscles is extremely rare, but several cases have been reported, and this form of PAN has been named ‘muscular PAN (m-PAN)’ [5]. Here, we report the first case of muscular PAN (m-PAN) affecting not only the lower limbs but also the forearms.
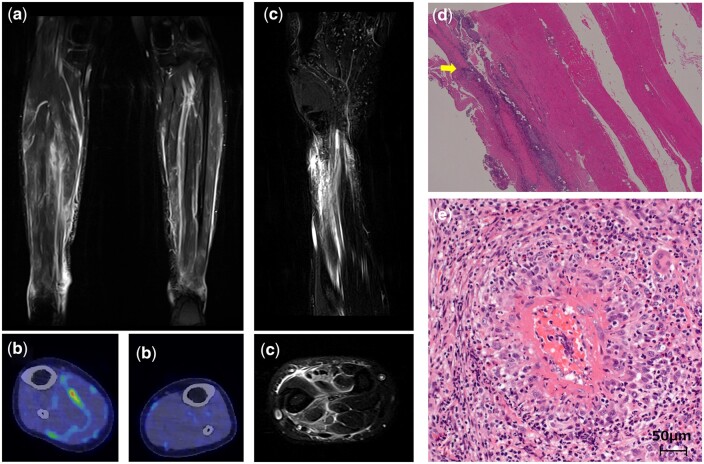
A 20-year-old female patient without any relevant medical history presented with bilateral lower limb pain that continued for the past 2 months. She had difficulty walking without a crutch owing to the pain. Her family and social histories were unremarkable. Physical examination revealed swelling, redness and tenderness of the bilateral lower limbs with right predominance. Laboratory findings showed leucocytosis (8960/μl) with normal eosinophil count (128/μl), normal creatine kinase (CK) level (74 U/l), elevated CRP level (3.8 mg/dl) and slightly elevated D-dimer level (1.6 μg/ml). All immunological tests, including MPO-ANCA and PR3-ANCA, were negative. Moreover, blood cultures and other workups for infectious diseases, including tuberculosis, hepatitis B and C, syphilis and human immunodeficiency virus, were negative. Electromyography of the left rectus femoris, tibialis anterior and medial head of the gastrocnemius revealed fibrillation potentials of spontaneous activity and a low amplitude and short duration of voluntary contraction, which are consistent with a myogenic pattern. Contrast-enhanced MRI of the lower extremities showed several high-density areas in the muscles and fascia of the lower extremities (tibialis anterior and gastrocnemius) (Fig. 1a). Fluorodeoxyglucose (FDG)-PET/CT showed increased FDG accumulation mainly in the fascia of the lower extremities (Fig. 1b). On day 8 of admission, the patient had newly developed bilateral forearm pain. Contrast-enhanced MRI of the right wrist joint revealed high-density areas in the muscles and fascia of the anterior and posterior forearm, which were similar to the findings in the lower extremities (Fig. 1c).
Figure 1.
Imaging and biopsy findings. (a) Contrast-enhanced magnetic resonance imaging (MRI) of the lower extremities shows several high-density areas in the muscles and fascia of the lower extremities (tibialis anterior and gastrocnemius). (b) Positron emission tomography scan shows increased fluorodeoxyglucose accumulation mainly in the fascia of the lower extremities. (c) Contrast-enhanced MRI of the right wrist joint reveals high-density areas in the muscles and fascia of the forearm (brachioradialis, muscle flexor pollicis longus, musculus extensor digitorum and musculus extensor pollicis longus). (d) Biopsy of the right gastrocnemius. Intense lesions are observed at the margins of the specimen (fascial side), while deeper vessels appear to be relatively preserved (haematoxylin–eosin staining; original magnification ×40). (e) Biopsy of the right gastrocnemius. Vasculitis is seen in all layers of the arteries within 200 µm in diameter. Fibrinoid deposition within the intima is observed. Infiltration of neutrophils, eosinophils and lymphocytes is detected (haematoxylin–eosin staining; original magnification ×400)
On day 10, muscle biopsy of the right gastrocnemius was performed. As the patient had difficulty walking and new symptoms in both upper arms, treatment was prioritized before making a definitive diagnosis. Prednisolone (40 mg) was initiated on day 11, and the CRP level and clinical symptoms, including pain in the extremities and difficulty walking, improved soon after the treatment started. On day 24, the prednisolone dose was tapered to 35 mg. The patient was discharged on day 25.
The muscle biopsy results were received after discharge. Small- and medium-sized arteritis were detected in several muscles and the fascia, and fascia-predominant lesions were observed (Fig. 1d). Fibrinoid deposition was observed within the intima in areas of intense lesions (Fig. 1e). Disappearance of the inner elastic lamina was not observed. Major histocompatibility complex class I and II immunostaining findings were normal. Thus, a diagnosis of m-PAN with fasciitis was made.
The prednisolone dose was reduced by 5 mg every 2 weeks in an outpatient clinic. Follow-up contrast-enhanced MRI of the lower extremities and right wrist joint at 3 months after discharge showed complete recovery of the abnormal high-density areas. The patient has remained in remission.
According to the Chapel Hill consensus conference in 2012, the differential diagnoses of small- and medium-sized arteritis other than PAN include Kawasaki disease, ANCA-associated vasculitis, immune complex vasculitis, Bechet’s disease, Cogan’s syndrome, rheumatoid vasculitis, lupus vasculitis and sarcoid vasculitis. However, none of these diseases matched our patient’s symptoms, immunological test results and FDG-PET/CT scan results, which did not indicate any large vessel vasculitis, sinusitis or heart involvement.
In terms of fasciitis, eosinophilic fasciitis is an important differential diagnosis. However, in this case, there was no eosinophilia, and the pathological findings of the muscle biopsy were mainly vasculitis. These findings were not consistent with eosinophilic fasciitis.
Previous reports have shown several cases of lower extremity pain without CK elevation and with small- or medium-sized arteritis on muscle biopsy. They suggested a new grouping of PAN called muscular PAN or m-PAN [5]. Patients with m-PAN are comparatively younger and have a good response to glucocorticoids [5]. The course of the disease tends to be benign without progression to the viscera [5]. Fasciitis is comparatively rare among m-PAN cases [5–7]. Our case was incredibly rare because of the presence of fasciitis and upper extremity involvement. To our knowledge, no case of m-PAN affecting the forearms has been reported.
In conclusion, we report the first case of m-PAN with fasciitis in the upper extremities. In patients with lower extremity pain without CK elevation, we should consider the possibility of PAN, including m-PAN, even at a young age.
Contributor Information
Setsuko Oyama, Division of Rheumatic Diseases, National Center for Global Health and Medicine, Tokyo, Japan.
Hiroyuki Yamashita, Division of Rheumatic Diseases, National Center for Global Health and Medicine, Tokyo, Japan.
Misa Yamaji, Division of Rheumatic Diseases, National Center for Global Health and Medicine, Tokyo, Japan.
Toshiaki Kobayashi, Division of Rheumatic Diseases, National Center for Global Health and Medicine, Tokyo, Japan.
Akatsuki Kubota, Department of Neurology, The University of Tokyo, Tokyo, Japan.
Jun Shimizu, Department of Neurology, The University of Tokyo, Tokyo, Japan; Department of Physical Therapy, Tokyo University of Technology, Tokyo, Japan.
Tamiko Takemura, Department of Pathology, Kanagawa Cardiovascular and Respiratory Center, Yokohama, Japan.
Hiroshi Kaneko, Division of Rheumatic Diseases, National Center for Global Health and Medicine, Tokyo, Japan.
Data availability
Data are available upon request.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Disclosure statement: The authors have declared no conflicts of interest.
Patient consent statement: The authors have written permission from the patient to report this case. All procedures complied with the ethical principles enshrined in the Declaration of Helsinki.
References
- 1. Jennette JC, Falk RJ, Bacon PA. et al. 2012 revised International Chapel Hill Consensus conference nomenclature of vasculitides. Arthritis Rheum 2013;65:1–11. [DOI] [PubMed] [Google Scholar]
- 2. Gonzalez-Gay MA, Garcia-Porrua C, Guerrero J, Rodriguez-Ledo P, Llorca J.. The epidemiology of the primary systemic vasculitides in northwest Spain: implications of the Chapel Hill Consensus Conference definitions. Arthritis Rheum 2003;49:388–93. [DOI] [PubMed] [Google Scholar]
- 3. De Virgilio A, Greco A, Magliulo G. et al. Polyarteritis nodosa: a contemporary overview. Autoimmun Rev. 2016;15:564–70. [DOI] [PubMed] [Google Scholar]
- 4. Karadag O, Jayne DJ.. Polyarteritis nodosa revisited: a review of historical approaches, subphenotypes and a research agenda. Clin Exp Rheumatol 2018;36(Suppl 111):135–42. [PubMed] [Google Scholar]
- 5. Ganeshanandan LR, Brusch AM, Dyke JM, McLean-Tooke APC.. Polyarteritis nodosa isolated to muscles-a case series with a review of the literature. Semin Arthritis Rheum 2020;50:503–8. [DOI] [PubMed] [Google Scholar]
- 6. Ahmed S, Kitchen J, Hamilton S, Brett F, Kane D.. A case of polyarteritis nodosa limited to the right calf muscles, fascia, and skin: a case report. J Med Case Rep 2011;5:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kang Y, Hong SH, Yoo HJ. et al. Muscle involvement in polyarteritis nodosa: report of eight cases with characteristic contrast enhancement pattern on MRI. AJR Am J Roentgenol 2016;206:378–84. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request.