Abstract
Background:
Structural racism is a powerful determinant of health that drives health disparities, morbidity, and mortality across racialized and minoritized groups.
Purpose:
This article discusses approaches for measuring structural racism and its resultant network of negative biopsychosocial consequences for health and well-being.
Methods:
We draw on prevailing theoretical models and approaches to characterize both the nature of structural racism and integrated methods for assessing its consequences across mental and physical health.
Discussion:
This article will serve to guide researchers in health-related disciplines to accurately assess the biopsychosocial consequences of structural racism in key populations.
Keywords: Structural racism, Multilevel, Multidimensional, Biopsychosocial model, Biomarkers
What is X? Structural Racism
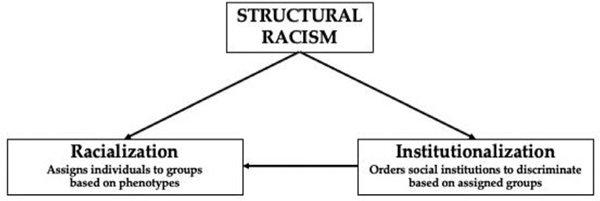
Racism is a powerful structural determinant of health and health care for all persons within the United States (US) (Bailey, Feldman, & Bassett, 2021). At birth, individuals endure a process of racialization where they are categorized based on their, or their parents’, phenotypic characteristics (i.e., skin color), and assigned a racialized group (i.e., Black, Indian, Asian etc.) (Racialization, 2022). From this moment forward, opportunities in the US are structured based on one’s racialized group (Hamilton et al., 2015). From the health care providers and facilities available for birthing, to the quality of the homes and schools within neighborhoods, to the nature of interactions with arbiters of society (e.g., police, courts)—the experiences of persons in the US are conditioned largely on the value assigned to one’s racialized group (Bailey et al., 2017). (see Figure 1)
Figure 1 –
Structural racism pathway.
The classification of humans has origins in evolutionary concepts of how Homo sapiens came to exist. In the 18th century, European scientists like Carl Linnaeus and Johann Blumenbach developed taxonomic systems to distinguish groups of people from each other by relying on differences in skin color (Smedley, 1999; Smedley & Smedley, 2005). Such differences between Europeans and the darker-skinned persons they encountered throughout the world served to justify a ranking system where European-like skin was assigned values of beauty, intelligence, and civility, and other groups were ranked below this self-described “white skin.” This ranked system of racialized groups is a part of the fabric of the founding of the US as its constitution legitimized the dislocation and genocide of Indigenous persons (i.e., Native Americans), the indentured servitude of Asian persons, and the enslavement of African persons and their descendants (Zinn, 1990). Later, that ranking system was used to justify the colonization of northern Mexico and the Pacific and Caribbean Islands and the imperialization of Middle Eastern nations.
When examining the role of structural racism on health and health care in the present, it is imperative that a discussion of the past is undertaken. The policies and procedures of the present are rooted in a past where the Indian Removal Act and Jim Crow segregation laws established segregated and impoverished Indigenous and Black neighborhoods that exist today. The Immigration Act of 1965 not only determined who could migrate to the US, but what jobs they could take when they arrived—an example of this was the recruitment of Filipino immigrants into the US field of nursing (Cachero, 2021). Many of these policies and procedures still actively influence the health of all US persons in multidimensional ways, although adversely for racialized and minoritized groups (Bailey et al., 2021).
Racism is Multilevel
Scholars have conceptualized racism as a multilevel system with the following tiers: internalized racism, interpersonal racism or personally-mediated racism, and institutional or institutionalized racism (Jones, 2000). Internalized racism refers to the ways individuals and communities adopt negative images, messages, and beliefs about their nature, ability, and worth as well as about those who look like them (David, et al., 2019). Internalized racism can take the form of imposing limitations on self-determination and self-expression, and placing whiteness on a ranking system by which certain attributes (e.g., light skin, straightened hair) are conflated with the most desirable aspects of society (e.g., success, beauty) (Jones, 2000). Well-examined literature on internalized racism can be found in the fields of psychology, sociology, anthropology, and media studies (Durkee & Gómez, 2021).
Interpersonal racism or personally-mediated racism occurs when prejudicial and ethnocentric beliefs are imposed upon individuals and communities in the form of discriminatory acts. This type of racism can be performed irrespective of intention or motive. Jones (2000) outlines a number of actions that comprise of interpersonal and/or personally-mediated racism including being suspicious of individuals (e.g., 17-year-old Trayvon Martin walking home from a convenience store), which can lead to over-vigilance of communities (e.g., FBI surveillance of Middle Eastern persons). Other actions entail avoidance (e.g., not hiring persons with Spanish last names assuming they need citizenship) that can occur with regularity (e.g., ignoring self-reported health of Asian seniors). These acts demonstrate a devaluing of individuals and/or communities from racialized and minoritized groups that can be expressed passively by not considering the needs or concerns of groups (e.g., white seniors taking vaccination slots in predominantly Black and Latinx/a/o neighborhoods); scapegoating individuals and/or communities for their marginalization (e.g., questioning why 13-year old Adam Toledo ran from the police); expressing fascination or wonderment with the success of individuals and/or communities; and generally lacking respect for diverse communities.
Institutional and institutionalized racism once referred to the ways a larger system of oppression is facilitated. This definition better represents structural racism (see below). Institutional racism now refers to an organization’s practice of racism via policies and procedures (Adkins-Jackson et al., 2021; Barbarin & Gilbert, 1981). Health care organizations like academic research institutions and academic health centers play significant roles in perpetuating institutional racism by enacting procedures that disproportionately screen for chronic conditions (Chan et al., 2021). Such organizations demonstrate a lack of respect of racialized and minoritized individuals and/or communities by refusing service or providing poor quality service, and furthermore by training the next generation of providers to do the same by teaching indifference to pain and using materials that perpetuate biological determinism (e.g., asthma, kidney, and breast screening devices) (Matthew, 2018). Paradoxically, patients have the right to refuse service, under the current health care doctrine; however, there are severe consequences in health care settings for racialized and minoritized individuals who exercise this right (e.g., multiple Black couples arrested, or babies being removed from the custody of the parents for opting out of select medical services; Savage, 2021).
Structural racism encompasses all three of the aforementioned levels. Subsequently, structural racism is the complex structure by which multiple systems operate (Bailey et al., 2017). Within structural racism, policies and procedures allow organizations to engage in discriminatory acts against individuals and communities (e.g., continued lack of inclusion of diverse groups in clinical trials) (Bailey et al., 2021). Organizational policies and procedures set the tone for how actors (i.e., employees of an organization) are to view individuals from racialized and minoritized communities (e.g., nurses and police officers alike “just doing their job”) and provide legal cover for interpersonal racism (e.g., no consequences to the US Public Health Service or its researchers for the abuses conducted during the Tuskegee Syphilis Study) (Adkins-Jackson, Sanchez, Ison, & Williams-Gray, 2021; Griffith et al., 2007; Hardeman et al., 2020). Consequently, it is important to explore multilevel structural racism as the exposure may occur on specific levels or across multiple.
Structural Racism is Multidimensional
Choosing an approach for measuring structural racism requires an understanding of its multidimensional nature. Structural racism mobilizes across organizations and institutions within the US context to engage in and enact multiple levels of racism and discrimination (Adkins-Jackson et al., 2021; Hardeman et al., 2022). The collaboration of these organizations and institutions produces domains of structural racism that can be studied. Bailey et al. (2017) identified seven domains of structural racism: (a) housing, (b) education, (c) employment, (d) earnings, benefits, and credit, (e) media, (f) health care, and (g) criminal justice. LaFave et al. (2022) included housing within neighborhood factors along with segregation and food access, and added the domains of marketing, civics, and the environment. Central to these models is the reality that the compounded effects of these domains influence a range of health and well-being markers. For instance, combinations of these domains predict COVID-19 vaccination rates, cognitive decline, infant mortality, gestational age at delivery, maternal mortality, Body Mass Index, and self-reported health (Bell & Owens-Young, 2020; Chantarat et al., 2021; Dougherty et al., 2020; Liu et al., 2019; Owens-Young & Bell, 2020; Pohl et al., 2021; Wallace et al., 2015).
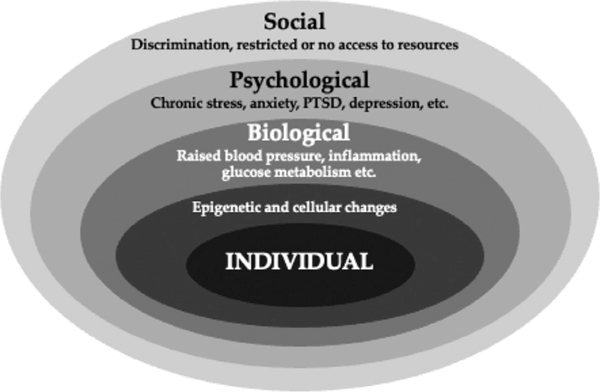
The pathway of this influence differs, which can determine how racialized and minoritized individuals and/or communities experience the exposure of structural racism. Socially through institutional racism, racialized and minoritized individuals and/or communities have restricted or no access to resources like education, wealth, nutrient-rich foods, and health insurance that influence health over the life course (Chisolm et al., 2021; Hudson et al., 2020). Psychologically, racialized and minoritized individuals and/or communities experience interpersonal racism leading to chronic stress and heightened anxiety and trauma (Adkins-Jackson et al., 2022; Robinson & Tobin, 2021). Over time, these experiences get under the skin to influence biological processes like increasedblood pressure and glucose, as well as heart palpitations (Geronimus et al., 2006; Goetsch et al., 1990; Harrell et al., 2003; Lavretsky & Newhouse, 2012). Such biopsychosocial responses can ultimately lead to cellular and epigenetic changes that are felt over the life course and across generations. Given that exposure to structural racism is multilevel and multidimensional, examining outcomes of exposure also requires a similar integrative framework (Harrell, 2000). (see Figure 2)
Figure 2 –
Levels of biopsychosocial impact and examples.
WHAT IS Y? Using a Biopsychosocial Framework to Measure Outcomes
The Biopsychosocial Model was proposed to address the fundamental challenges posed to biomedicine by the burden of chronic disease, including and of primary relevance here, measuring and assessing mechanisms and downstream health outcomes (Engel, 1977). Clark et al. (1999) expanded upon this model to include a framework for examining racism as a determinant of health outcomes and disparities. Both approaches contend that Eurocentric biomedical models of illness assume that a biochemical defect or diagnostic indicator of a disease should translate into actual disease existence. However, indicators of a disease actually imply only the potential for a disease, one that must be considered in light of the full biopsychosocial context of risk and resilience. Structural and social determinants like structural racism often play monumental roles in disease manifestation. However, Eurocentric biomedical models of health care rarely solicit and incorporate patient-reported symptomatology of social factors in diagnosis, resulting in too few practitioners poised to contend with structural determinants.
For example, a patient may not be aware of the ways in which complex social structures impact their health. However, the patient is aware that they have to take time off of work and access multiple forms of transportation to attend an appointment. In this scenario, the location of the health care facility, the costs of transportation, and the policies that dictate health care operating hours all disproportionately and adversely impact racialized and minoritized groups in the US. While some of these actions can be changed with intentional anti-racist decision-making (e.g., offering evening and weekend hours, including transportation costs in health care), other aspects of this scenario (i.e., location) are relics of historically racist policies like segregation and redlining that established modern-day academic health centers and research universities in white neighborhoods where Black residents were prohibited from homeownership (Rothstein, 2018). Thus, by relying on a Eurocentric biomedical model, one’s ability to understand the process by which structural racism influences health and health care is limited.
Additionally, biomedical models assume successfully treating or repairing a biochemical defect restores health. Yet, this is rarely the case. Even if an injury or illness can be identified, repairing it does not always translate into relief or better health when the precipitating structures are still at play. An example of this would be if a patient with persistent high blood glucose is chastised for not “eating less and moving more.” Such an approach negates the lived experience of many racialized and minoritized communities living in designated food deserts where the only accessible and affordable foods are saturated in salt and sugar (Berkowitz et al., 2018). Furthermore, such an approach ignores the body of literature on the role of epigenetics, trauma, and physiological stress (e.g., cortisol levels) on blood glucose and how individual behaviors are not the only drivers of poor health (Villeneuve et al., 2011). Thus, for many reasons in addition to these, a biopsychosocial lens is critical for understanding the boundaries between health and dis(ease) and the association of structural determinants as both the additive and interactive relationships among these factors are at play. The biopsychosocial model is able to provide an essential scaffolding for health research and health care management to improve patient outcomes (Wade & Halligan, 2017).
Potential Ys (Outcomes) Across Systems
Applying a biopsychosocial lens requires selecting both the appropriate structural and social constructs as well as targeting meaningful physiological indices that drive health and disease. A useful approach for selecting, assessing, and quantifying meaningful impact across physiological systems of interest comes from McEwen’s conceptualization of allostasis and allostatic load (McEwen, 1998). Here, the body’s physiological systems function to help with adapting to environmental demands (i.e., stressors) so as to maintain allostasis. When the body experiences stress, including social stressors such as structural racism, multiple systems are engaged to adapt to the stressor and restore the body to its baseline operating status. When allostatic challenges become recurrent, this can instantiate multi-system dysregulation, which over time increases and drives physical disease risk (Geronimus et al., 2006). These physiological systems—from the autonomic nervous system to the hypothalamicpituitary-adrenal (HPA) axis to the immune system— all work in tandem through intricate cascades of negative feedback loops and permissive versus suppressive functions (Selye, 1951). When dysregulation emerges across these systems, it creates allostatic load. Through this concept of allostatic load, it becomes clear how structural racism can impact individuals and/or communities under the skin in deleterious ways. This is why comprehensively addressing the impact of structural racism on health using the biopsychosocial model is necessary. Doing so may entail evaluating not any one biomarker or physiological measure, but optimally, a multi-system approach.
Gruenewald et al. (2012) quantified systemic allostatic load by identifying seven systems and 24 biomarkers measured from seven distinct allostatic systems. These systems include the sympathetic nervous system, parasympathetic nervous system (e.g., various indices of heart rate variability), HPA axis (e.g., cortisol), cardiovascular system (e.g., systolic and diastolic blood pressure), lipid metabolic system (e.g., adverse profiles for cholesterol), glucose metabolic system (e.g., fasting blood glucose and insulin), and immune system via inflammatory activity (e.g., C-reactive protein). This study characterized “high risk” for allostatic load as the proportion of biomarkers for each system that fell in the outermost quartile for conferring poor health risk (Gruenewald et al., 2012). This approach for quantifying allostatic load is useful for cumulatively measuring life course health risk due to structural determinants like lifetime adversity from socioeconomic conditions, which was associated with higher allostatic load scores in the aforementioned study. Though conducted with predominantly White participants, this study design yields promise for linking structural racism with biological responses in racialized and minoritized groups.
A wealth of research has investigated allostatic load in racialized and minoritized communities that are most at risk for health inequities—a seminal study includes Geronimus et al. (2006). Comparing over 4,000 Black and White persons across ten biomarkers, Duru et al. (2012) found that Black participants did indeed have higher allostatic load scores than White participants. Moreover, higher allostatic load partially accounted for the well-established heightened risk of mortality among Black participants, even when controlling for socioeconomic factors and health behaviors (Duru et al., 2012). Though this study did not formally include a measure of structural racism, with the Human Genome Project verifying that there are no meaningful genetic differences between socially constructed racialized groups, the Duru et al. study leaves one likely prime candidate for the disparity in allostatic load and mortality risk—structural racism (Collins & Mansoura, 2001). A recently published review of 11 studies examining discrimination and allostatic load found a consistent link with allostatic load across various measures of discrimination (e.g., lifetime exposure to discrimination, racial discrimination in childhood, and everyday perceived discrimination) (Miller et al., 2021).
While examining the full arc of allostatic systems may lay outside the realm of feasibility for many studies, there are nonetheless key biomarkers and health outcomes that can offer meaningful insight into the burden of structural racism for health over the life course. Such elucidation of the impact of structural racism on various biomarkers and health outcomes is not only clinically relevant, but epidemiologically salient to delineate disease incidence, morbidity, and mortality. Seminal research linking racism-related stress with health in racialized and minoritized communities has used hypertension and inflammation as indicators of biopsychosocial impact (Harrell et al.,2003). A growing body of literature has since demonstrated that racism over the life course promotes accelerated cellular aging via telomere degradation (Chae et al., 2020; Lu et al., 2019). Similarly, epigenetic clocks obtained through DNA methylation provide a biological age, often disparate from chronological age, that indicates age acceleration (Lu et al., 2019). In addition to biological aging, structural racism also drives social aging as time is a key social resource for health and well-being (e.g., time for engaging in activities that may improve mental and physical health) (Gee, Hing, Mohammed, Tabor, & Williams, 2019). Such experiences widen the range of outcomes from traditional health care outcomes like acute health hospitalizations (e.g., fractures) to long-term outcomes like morbidity (e.g., cognitive decline) (Barnes et al., 2012; Caunca et al., 2020;Paltaetal.,2015).
With this in mind, depending on the particular individuals/communities of interest, focusing on key biological systems may provide critical insight into trajectories of health. As an example of an integrated biopsychosocial approach, several recent papers draw from a study of 150 Latinx mothers residing in the US, the majority of whom were foreign-born, who were assessed while pregnant at 24–32 weeks gestation and again at 4–6 weeks postpartum (Incollingo Rodriguez et al., 2022a,b; Sluiter et al., 2020). Perceived discrimination assessed during pregnancy predicted postpartum mental health concerns. Furthermore, incorporating physiological measures assessed during pregnancy—DNA methylation at two key regions: (a) FOXP3 Treg–cell–specific demethylated region (TSDR), a marker of inflammation regulation; and (b) the promoter of tumor necrosis factor-alpha (TNF-α), a pro-inflammatory cytokine—revealed that prenatal discrimination predicted postnatal depression and anxiety specifically among those with high FOXP3 methylation (Sluiter et al., 2020). These relationships were mediated by TNFα in those with high FOXP3 methylation implying an interconnected network between discrimination, stress, and markers of epigenetic immunoregulation alternations.
Incollingo Rodriguez et al. (2022a,b) also revealed how other structural determinants like acculturation, which occurs as one assimilates (by choice or force) to another culture (Redfield, Linton, & Herskovits, 1936)—can have nuanced effects on downstream health. This includes through increasing acculturative stress, an established risk factor for postpartum depression in Latinx mothers (Alhasanat & Giurgescu, 2017; LaraCinisomo, Girdler, Grewen, & Meltzer-Brody, 2016). Here, among mothers with low oxytocin receptor levels, acculturation level was associated with postpartum depression and anxiety symptoms (Incollingo Rodriguez et al., 2022b). Moreover, acculturative stress predicted shorter prenatal telomere length, particularly among participants with high methylation of the FOXP3 TSDR. Shorter telomere length also predicted greater postpartum depression symptoms (Incollingo Rodriguez et al., 2022a). These findings reveal a role for epigenetic modifications in sensitivity to prenatal acculturation-related stress in a population already at risk for health disparities.
The aforementioned examples, and many others, highlight the utility of examining biomarker and health indicators as dependent variables influenced by structural racism. However, different racialized and minoritized groups experience varying combinations of the domains of structural racism (Adkins-Jackson et al., 2021; Liu et al., 2019). Thus, it is vital to engage in community-based partnerships and prioritize cultural competency in the design and implementation of research on the impact of structural racism. Such communities and partners will be able to guide the science undertaken. We conclude this article with recommendations for how to move forward in this research.
Conclusion
While conducting research examining the impact of structural racism can appear complex, it is feasible when engaging interdisciplinary research with colleagues from the humanities and social sciences (Adkins-Jackson et al., 2021). Often, these colleagues specialize in the historiographies and literature that describe over time how racialized and minoritized persons have weathered structural racism. However, the most informed source on the interaction between structural racism and health and health care will always be the communities impacted. Thus, to select factors that may be most appropriate to examine, researchers must partner with racialized and minoritized communities, instead of the typical convenience sample of persons privileged by structural racism.
Community participation goes beyond engagement of key informants to understand salient pathways. Community participation requires partnership with the community in all aspects of the study, from conception to publication (Adkins-Jackson et al.). True community partnership would create opportunities for the research to be conducted together to influence advocacy in ways that improve the lives of racialized and minoritized communities. Therefore, it is vital that the research conducted be modeled to reflect the lived experiences of communities, and not a reflection of how we have always done science.
New ways of doing the science will reposition structural racism from a moderator in the relationship between two factors, to the primary causal factor (i.e., X). This restructuring of the guiding analytical approach may mean that one health outcome (e.g., sleep disturbance) mediates or moderates the impact of structural racism on another (e.g., anxiety), which helps to magnify potential interventions (e.g., The Nap Ministry encourages rest as an intervention; Hersey, 2016). Identifying and utilizing culturally sensitive and relevant interventions will also necessitate repositioning our analyses so that the intervention serves as a mediator or moderator in the relationship between structural racism, the root cause, and the health change we seek (Adkins-Jackson et al., 2022). Thus, the pharmacological, behavioral, or otherwise intervention moderates the relationship between structural racism and the health outcome hopefully in ways that reduce its impact. Repositioning the model of structural racism and its resultant disparities also necessitates that sociodemographic individual-level variables (e.g., socioeconomic status, perceived discrimination and/or racism, accessibility, cultural identity and acculturative status) are re-described as direct outcomes of structural racism and mediators to structural racism’s influence on health. For recommendations on how to incorporate covariates in ways that reduce collinearity, please see Adkins-Jackson et al. (2021).
Learning vital structural determinants, salient individual-level variables, and meaningfully engaging community participation in culturally respectful ways is a crucial prerequisite to successfully incorporate a biopsychosocial framework. However, this approach is not additive or merely the piecing together of a biological, psychological, and social construct. Such a reductionist lens is rarely sufficient to assess the negative impact of structural racism on human health. Rather, effectively applying a biopsychosocial framework necessitates a deep knowledge of the lived experiences of racialized and minoritized communities of interest. This allows for the integration of biomarkers and health outcomes in the study of the impact of structural racism on health. This again highlights the need for deep cultural competency to develop interventions addressing inequities. By conducting research with informed and socially aware intentionality, health and health care researchers can make great strides in illuminating the impact of structural racism on health and health care for US individuals and communities in ways that reduce this determinant’s effect on quality and quantity of life.
Acknowledgments
“Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers DP1AG069874 and DP1AG069874–01S1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.”
REFERENCES
- Adkins-Jackson PB, Sanchez AV, Ison J, & Williams-Gray S. (2021). Clinical Trials and Trust: Understanding the role of social determinants on clinical trial participation and trust. Applied Clinical Trials, 30(3). [Google Scholar]
- Adkins-Jackson PB, Burke N, Espinoza GP, Rosas GL, Doubeni C, Goold S, & Brown AF (in press). The STOP COVID-19 CA trial participation & vaccine hesitancy workgroups. Inclusionary trials: Lessons not learned in vaccine and clinical trials. Epidemiologic Reviews. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adkins-Jackson PB, Chantarat T, Bailey ZD, & Ponce NA (2021). Measuring structural racism: A guide for epidemiologists and other health researchers. American Journal of Epidemiology, doi: 10.1093/AJE/KWAB239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adkins-Jackson PB, Jackson Preston PA, & Hairston T. (2022). The only way out’: How self-care is conceptualized by Black women. Ethnicity & health 1–17, doi: 10.1080/13557858.2022.2027878 Advance online publication. [DOI] [PubMed] [Google Scholar]
- Adkins-Jackson PB, Legha RK, & Jones KA (2021). How to measure racism in academic health centers. AMA Journal of Ethics, 23(2), E140–E145, doi: 10.1001/AMAJETHICS.2021.140. [DOI] [PubMed] [Google Scholar]
- Alhasanat D, & Giurgescu C. (2017). Acculturation and postpartum depressive symptoms among Hispanic women in the United States: Systematic review. The American Journal of Maternal/Child Nursing, 42(1), 21–28, doi: 10.1097/NMC.0000000000000298. [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Feldman JM, & Bassett MT (2021). How structural racism works - Racist policies as a root cause of U.S. racial health inequities. The New England Journal of Medicine, 384(8), 768–773, doi: 10.1056/NEJMMS2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequities in the USA: Evidence and interventions. Lancet, 389(10077), 1453–1463, doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Barbarin OA, & Gilbert R. (1981). Institutional Racism Scale: Assessing Self and Organizational Attributes. ERIC. [Google Scholar]
- Barnes LL, Wilson RS, Everson-Rose SA, Hayward MD, Evans DA, & De Leon CFM (2012). Effects of early-life adversity on cognitive decline in older African Americans and whites. Neurology, 79(24), 2321–2327, doi: 10.1212/WNL.0B013E318278B607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CN, & Owens-Young JL (2020). Self-rated health and structural racism indicated by county-level racial inequalities in socioeconomic status: The role of urban-rural classification. Journal of Urban Health : Bulletin of the New York Academy of Medicine, 97(1), 52–61, doi: 10.1007/S11524-019-00389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkowitz SA, Karter AJ, Corbie-Smith G, Seligman HK, Ackroyd SA, Barnard LS, & Wexler DJ (2018). Food insecurity, food “deserts,” and glycemic control in patients with diabetes: A longitudinal analysis. Diabetes Care, 41(6), 1188–1195, doi: 10.2337/DC17-1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cachero P. (2021). From AIDS to COVID-19, America’s medical system has a long history of relying on Filipino nurses to fight on the frontlines. May 30, 2021Time Magazine. Available at: https://time.com/6051754/history-filipinonurses-us/.
- Caunca MR, Odden MC, Glymour MM, Elfassy T, Kershaw KN, Sidney S, & Zeki Al Hazzouri A. (2020). Association of racial residential segregation throughout young adulthood and cognitive performance in middle-aged participants in the CARDIA Study. JAMA Neurology, 77(8), 1000–1007, doi: 10.1001/JAMANEUROL.2020.0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Wang Y, Martz CD, Slopen N, Yip T, Adler NE, & Epel ES (2020). Racial discrimination and telomere shortening among African Americans: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Health Psychology, (3), 39, doi: 10.1037/HEA0000832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan AL, Guo N, Popat R, Robakis T, Blumenfeld YY, Main E, & Butwick AJ (2021). Racial and ethnic disparities in hospital-based care associated with postpartum depression. Journal of Racial and Ethnic Health Disparities, 8(1), 220–229, doi: 10.1007/S40615-020-00774-Y. [DOI] [PubMed] [Google Scholar]
- Chantarat T, Van Riper DC, & Hardeman RR (2021). The intricacy of structural racism measurement: A pilot development of a latent-class multidimensional measure. EClinical Medicine, 40, doi: 10.1016/J.ECLINM.2021.101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisolm DJ, Bell BA, Yamoah O, & Freedman DA (2021). Racialized experiences differentiate food security among African American adults. Nursing research, 70(5S), S13–S20, doi: 10.1097/NNR.0000000000000533 Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, & Williams DR (1999). Racism as a stressor for African Americans. A biopsychosocial model. The American psychologist, 54 (10), 805–816, doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Collins FS, & Mansoura MK (2001). The human genome project. Revealing the shared inheritance of all humankind. Cancer, 91(1), 221–225, doi: Suppl. [DOI] [PubMed] [Google Scholar]
- David EJR, Schroeder TM, & Fernandez J. (2019). Internalized racism: A systematic review of the psychological literature on racism’s most insidious consequence. Journal of Social Issues, 75(4), 1057–1086, doi: 10.1111/JOSI.12350. [DOI] [Google Scholar]
- Dougherty GB, Golden SH, Gross AL, Colantuoni E, & Dean LT (2020). Measuring structural racism and its association with BMI. American Journal of Preventive Medicine, 59(4), 530–537, doi: 10.1016/J.AMEPRE.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkee MI, & Gomez JM (2021). Mental health impli- cations of the acting white accusation: The role of cultural betrayal and ethnic-racial identity among Black and Latina/o emerging adults. American Journal of Orthopsychiatry, doi: 10.1037/ORT0000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duru OK, Harawa NT, Kermah D, & Norris KC (2012). Allostatic load burden and racial disparities in mortality. Journal of the National Medical Association, 104 (12), 89–95, doi: 10.1016/S0027-9684(15)30120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel GL (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129–136. Available at: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=847460. [DOI] [PubMed] [Google Scholar]
- Gee GC, Hing A, Mohammed S, Tabor DC, & Williams DR (2019). Racism and the life course: Taking time seriously. American Journal of Public Health, 109 (S1), S43–S47, doi: 10.2105/AJPH.2018.304766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, & Bound J. (2006). “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health, 96(5), 826–833, doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetsch VL, Wiebe DJ, Veltum LG, & Van Dorsten B. (1990). Stress and blood glucose in type II diabetes mellitus. Behavior research and therapy, 28(6), 531–537, doi: 10.1016/0005-7967(90)90140-e. [DOI] [PubMed] [Google Scholar]
- Griffith DM, Childs EL, Eng E, & Jeffries V. (2007). Racism in organizations: The case of a county public health department. Journal of Community Psychology, 35 (3), 287–302, doi: 10.1002/jcop.20149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald TL, Karlamangla AS, Hu P, SteinMerkin S, Crandall C, Koretz B, & Seeman TE (2012). History of socioeconomic disadvantage and allostatic load in later life. Social Science & Medicine, 74 (1), 75–83, doi: 10.1016/J.SOCSCIMED.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton D, Darity W, Price AE, Sridharan V, & Tippett R. (2015). Umbrellas don’t make it rain: Why studying and working hard isn’t enough for Black Americans. Insight Center for Community Economic Development Report, 1–10. [Google Scholar]
- Hardeman R, Chantarat T, & Karbeah J. (2020). Police exposure as a determinant of structural racism: An exploration of the association between preterm birth in neighborhoods with high police exposure. Health Services Research, 55, doi: 10.1111/1475-6773.13396 50–50. [DOI] [Google Scholar]
- Hardeman RR, Homan PA, Chantarat T, Davis BA, & Brown TH (2022). Improving the measurement of structural racism to achieve antiracist health Policy. Health affairs (Project Hope), 41(2), 179–186, doi: 10.1377/hlthaff.2021.01489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell JP, Hall S, & Taliaferro J. (2003). Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health, 93(2), 243–248, doi: 10.2105/AJPH.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP (2000). A multidimensional conceptualization of racism-related stress: Implications for the wellbeing of people of color. The American journal of orthopsychiatry, 70(1), 42–57, doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Hersey T. (2016). The nap ministry. Accessed on July 4, 2022, Available at: https://thenapministry.com
- Hudson D, Sacks T, Irani K, & Asher A. (2020). The price of the ticket: Health costs of upward mobility among African Americans. International Journal of Environmental Research and Public Health, 17(4), 1179, doi: 10.3390/ijerph17041179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Incollingo Rodriguez AC, Polcari JJ, Nephew BC, Harris R, Zhang C, Murgatroyd C, & Santos HP Jr (2022a). Acculturative stress, telomere length, and postpartum depression in Latinx mothers. Journal of Psychiatric Research, 147, 301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Incollingo Rodriguez AC, Smith L, Harris R, Nephew BC, Santos HP Jr, & Murgatroyd C. (2022b). Oxytocin modulates sensitivity to acculturation and discrimination stress in pregnancy. Psychoneuroendocrinology, 141 105769. [DOI] [PubMed] [Google Scholar]
- Jones CP (2000). Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health, 90(8), 1212–1215, doi: 10.2105/AJPH.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaFave SE, Bandeen-Roche K, Gee G, Thorpe RJ, Li Q, Crews D, & Szanton SL (2022). Quantifying older Black Americans’ exposure to structural racial discrimination: How can we measure the water in which we swim? Journal of Urban Health: Bulletin of the New York Academy of Medicine, doi: 10.1007/s11524-02200626-6 doi:Advance online publication. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Cinisomo S, Girdler SS, Grewen K, & MeltzerBrody S. (2016). A biopsychosocial conceptual framework of postpartum depression risk in immigrant and U.S.-born latina mothers in the United States. Women’s Health Issues, 26(3), 336–343, doi: 10.1016/J.WHI.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavretsky H, & Newhouse PA (2012). Stress, inflammation, and aging. The American journal of geriatric psychiatry: Official journal of the American Association for Geriatric Psychiatry, 20(9), 729–733, doi: 10.1097/JGP.0b013e31826573cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu SY, Fiorentini C, Bailey Z, Huynh M, McVeigh K, & Kaplan D. (2019). Structural racism and severe maternal morbidity in New York State. Clinical Medicine Insights: Women’s Health, 12, 1–8, doi: 10.1177/1179562X19854778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu AT, Quach A, Wilson JG, Reiner AP, Aviv A, Raj K, & Horvath S. (2019). DNA methylation GrimAge strongly predicts lifespan and healthspan. Aging, 11(2), 303–327, doi: 10.18632/AGING.101684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu D, Palmer JR, Rosenberg L, Shields AE, Orr EH, DeVivo I, & Cozier YC (2019). Perceived racism in relation to telomere length among African American women in the Black Women’s Health Study. Annals of Epidemiology, 36, 33–39, doi: 10.1016/J.ANNEPI-DEM.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthew DB (2018). Just Medicine: A Cure for Racial Inequality in American Health Care. NYU Press. [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840(1), 33–44. Available at: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9629234. [DOI] [PubMed] [Google Scholar]
- Miller HN, LaFave S, Marineau L, Stephens J, & Thorpe RJ (2021). The impact of discrimination on allostatic load in adults: An integrative review of literature. Journal of Psychosomatic Research, 146(110434), 1–11, doi: 10.1016/J.JPSYCHORES.2021.110434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens-Young J, & Bell CN (2020). Structural racial inequities in socioeconomic status, urban-rural classification, and infant mortality in US counties. Ethnicity & Disease, 30(3), 389–398, doi: 10.18865/ED.30.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palta P, Szanton SL, Semba RD, Thorpe RJ, Varadhan R, & Fried LP (2015). Financial strain is associated with increased oxidative stress levels: The Women’s Health and Aging Studies. Geriatric Nursing, 36(2), S33–S37, doi: 10.1016/J.GERINURSE.2015.02.020 Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohl DJ, Seblova D, Avila JF, Dorsman KA, Kulick ER, Casey JA, & Manly J. (2021). Relationship between residential segregation, later-life cognition, and incident dementia across race/ethnicity. International Journal of Environmental Research and Public Health, 18(21), 11233, doi: 10.3390/IJERPH182111233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- racialization. (2022). Merriam-Webster.Com. Available at: https://www.merriam-webster.com/dictionary/racialization
- Redfield R, Linton R, & Herskovits MJ (1936). Memorandum for the study of acculturation. American Anthropologist, 38(1), 149–152, doi: 10.1525/AA.1936.38.1.02A00330. [DOI] [Google Scholar]
- Robinson MN, & Thomas Tobin CS (2021). Is John Henryism a health risk or resource?: Exploring the role of culturally relevant coping for physical and mental health among Black Americans. Journal of Health and Social Behavior, 62(2), 136–151, doi: 10.1177/00221465211009142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein Richard. (2018). The Color of Law. New York, NY: Liveright Publishing Corporation. [Google Scholar]
- Savage N. (2021). ‘We said no’: Los Angeles officers storm Black couple’s home hours after they refused a blood draw for their newborn daughter following a home birth. Atlanta Black Star. Available at: https://atlantablackstar.com/2021/07/17/we-said-no-los-angeles-officers-storm-black-couples-home-hours-after-they-refused-a-blood-draw-fortheir-newborn-daughter-following-a-home-birth [Google Scholar]
- Selye H. (1951). The General-Adaptation-Syndrome. Annual Review of Medicine, 2, 327–342, doi: 10.1146/ANNUREV.ME.02.020151.001551. [DOI] [PubMed] [Google Scholar]
- Sluiter F, Incollingo Rodriguez AC, Nephew BC, Cali R, Murgatroyd C, & Santos HP (2020). Pregnancy associated epigenetic markers of inflammation predict depression and anxiety symptoms in response to discrimination. Neurobiology of Stress, 13 100273, doi: 10.1016/J.YNSTR.2020.100273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley A. (1999). Race in North America: Origin and Evolution of a Worldview (2nd ed.). Westview Press. Available at: http://books.google.com/books?hl=en&lr=&id=GoCm-sJXclUC&pgis=1. [Google Scholar]
- Smedley A, & Smedley BD (2005). Race as biology is fiction, racism as a social problem is real: Anthropological and historical perspectives on the social construction of race. The American Psychologist, 60(1), 16–26, doi: 10.1037/0003-066X.60.1.16. [DOI] [PubMed] [Google Scholar]
- Villeneuve LM, Reddy MA, & Natarajan R. (2011). Epigenetics: Deciphering its role in diabetes and its chronic complications. Clinical and Experimental Pharmacology and Physiology, 38(7), 451–459, doi: 10.1111/J.1440-1681.2011.05497.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade DT, & Halligan PW (2017). The biopsychosocial model of illness: A model whose time has come. Clinical Rehabilitation, 31(8), 995–1004, doi: 10.1177/0269215517709890. [DOI] [PubMed] [Google Scholar]
- Wallace ME, Mendola P, Liu D, & Grantz KL (2015). Joint effects of structural racism and income inequality on small-for-gestational-age birth. American Journal of Public Health, 105(8), 1681–1688, doi: 10.2105/AJPH.2015.302613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinn H. (1990). A People’s History of the United States. Harper & Row. [Google Scholar]