Abstract
Purpose:
To understand participant preferences for receiving specific types of research information, whether information preferences vary across sociodemographic groups, and the types of health providers participants could access to understand returned information.
Methods:
All of Us Research Program participants completed a value of returning research information survey. Stratified sampling was implemented to enhance participant diversity and avoid noncoverage. We used weighted multivariable logistic regression to evaluate associations between the most valuable information types, access to providers, and sociodemographic variables.
Results:
Participants (N = 20,405) were diverse in their race/ethnicity (eg, 52% were White, 18% were Hispanic/Latino or Spanish, 3% were Asian, and 20% were Black or African American). Most participants (78.6%) valued information about their risk of serious genetic diseases with available treatment. Primary care physicians, specialists, and genetic counselors were the top providers that participants could access for help understanding returned information. Information preferences and provider access varied across sociodemographic groups. For example, as income levels increased, the odds of placing value on genetic results indicating risk of serious disease with available treatment increased when compared with the lowest income levels (P value < .001).
Conclusion:
Although genetic information was most valuable to participants, preferences about specific information types varied across sociodemographic groups.
Keywords: Engagement, Health equity, Participant perspectives, Precision medicine, Return of value
Introduction
Precision medicine genomics research has sparked interest in the return of biomedical study findings to participants.1–4 Prior research in this field suggests that participants are highly interested in receiving research results because, for example, the information can inform future health care decisions.5 Accordingly, the National Academies of Sciences, Engineering, and Medicine developed recommendations on return of results and encouraged researchers to consider participant understanding of and value placed on the type of results once returned.6 Namely, reconceptualizing the return-of-results practice as return of value can help capture the ways participants may value different types of research information regardless of whether they are actionable.1 Accompanying this reconceptualization is the Return of Value Conceptual Framework, which posits relationships between contextual factors, influencers of participants’ values, returnable information types, and resources are needed to interpret returned information.1
Return of value is relevant for the National Institutes of Health’s All of Us Research Program, which aims to enroll one million or more diverse participants.7 All of Us aims to provide access to personalized information to support health and prioritizes including populations historically underrepresented in research. In 2021, All of Us developed its 5-year goals; and the fifth goal prioritizes return of value.
Although returning results is a core All of Us value and is of deep interest to researchers,1,2 little is known about the types of research information that participants value. Indeed, prior research has largely focused on whether research results should be returned but not which specific types of information should be returned.5 Even less is known about how these preferences for specific information types vary across sociodemographic groups. To address these knowledge gaps, All of Us data were analyzed to understand participant preferences for receiving research information and the types of health providers participants could access to help them understand this information once returned.
Materials and Methods
Study design
All of Us opened enrollment in 2018. Participants are eligible if they are 18 years old or older, live in the United States, and are able to provide informed consent.8,9 All of Us participants provide physical measurements, biospecimens, electronic health record data, digital health data, and responses to surveys about topics, such as their sociodemographic characteristics, experiences with COVID-19, and health care access/utilization. The All of Us Institutional Review Board approved this study.
A sampled subset of participants was invited to complete a survey after enrollment. A 15-item survey was developed to understand the value All of Us participants place on receiving research information. This survey was designed based on existing literature, the Return of Value Conceptual Framework,1 recommendations from the Precision Medicine Initiative’s Working Group, and experiences of the All of Us Engagement Core.10–15 Survey feedback was obtained from the All of Us Participant Evaluation and Assessment Board. Cognitive interviews were conducted with 11 individuals, including 4 All of Us Participant Ambassadors, to understand how respondents would interpret survey items.16 Supplemental Files 1, 2, and 3 present survey feedback from English/Spanish speakers and the final survey, respectively.
Participants and data collection
Survey data were collected from a subset of All of Us participants between November 2020 and March 2021 via Qualtrics software (Qualtrics). Out of 333,942 All of Us participants at the time of survey, invitations were sent to 179,378 participants with the goal of receiving approximately 20,000 complete surveys. Stratifying on intersections of age, race/ethnicity, gender, sexual orientation, insurance status, annual income, preferred language, and health literacy, the sampling strategy was developed to reflect participant diversity and avoid noncoverage. Invitations were sent in 2 waves—100,674 invitations in November 2020 and 78,704 new invitations in January 2021. A total of 20,405 surveys were completed, yielding a sampling rate of 11.4%. Surveys were sent to participants via email in the participant portal and short message service. Participants were able to complete the survey in English or Spanish.
Survey items
Most valuable research information
The survey displayed a list of 14 types of health information, and participants were asked to choose up to 5 types of information from the list that they viewed as most valuable. The list included genetic information (eg, their risk for a serious disease when treatment is available) and other general types of health information (eg, medical record information). The full list is shown in Supplemental File 3. Data for each information type were coded as 0 = not selected as most valuable and 1 = selected as most valuable.
Preferred health care provider to help understand genetic information
Participants were asked to identify the types of health care providers they could access to help them understand genetic information. Examples of providers listed include a primary care physician, specialist physician, and genetic counselor. Participants were asked to “select all that apply.” Each provider type was coded as 0 = not selected, 1 = selected. Participants could select that they were unsure or did not have a place to go.
Sociodemographic variables
At initial enrollment, All of Us asks participants to self-identify their sociodemographic information (age, race, ethnicity, gender, sexual orientation, education level, annual household income, and language preference, English or Spanish).17 Sociodemographic data from All of Us initial enrolment surveys were linked with responses to the return of value survey. Health literacy was assessed using the Brief Health Literacy Screening tool; scores range from 0 to 15.18,19 Health literacy scores of 0 to 5 were categorized as low, scores of 6 to 10 as medium, and scores of 11 to 15 as high.
Data analysis
A sampled subset of All of Us participants were invited to complete the survey. To allow generalization of the results to the total All of Us population, survey weights were calculated for each participant based on the number and demographics of respondents in the All of Us population. Weights were further adjusted to account for individual question completeness; 2 separate χ2 survey weightings were derived based on missingness for the 2 survey questions (ie, the most valuable information and provider access for help understanding genetic information) assuming that data were missing at random conditioning on the demographic information among respondents.20 All analyses were conducted using weighted survey results to represent the total All of Us population.
The sampled weighted cohort is described using means and standard deviations for continuous variables and count and percentages for categorical variables. To report descriptive statistics for the overall All of Us population, the probability-weighted method was used to estimate proportions regarding participant feedback about the most valuable information types and preferred providers for facilitating the understanding of genetic information. Marginal sociodemographic differences in perspectives were assessed separately regarding the most valuable types of health information and preferred providers using weighted χ2 tests for race/ethnicity, gender, education, income, sexual orientation, health literacy, and preferred language for completing the survey. We used weighted multivariable logistic regression models to evaluate the adjusted associations between demographic variables and responses to the survey questions. Because participants could provide multiple answers to both survey questions, we analyzed each answer and applied the Bonferroni correction to adjust for the multiple comparison conducted for the 22 binary outcomes. A 2-sided P value less than .002 was considered statistically significant. Analyses were conducted using the survey package in R 4.2.0 and Stata version 15.1.
Role of the funding sources
The funding sources had no role in the execution, analyses, data interpretation, or decision to submit results for this study.
Results
Weighted sociodemographic characteristics for sampled participants
A total of N = 20,405 individuals responded to the survey and were included in analyses. The weighted mean age of participants was 55.3 years. Adjusting for sampling weights, the survey represents a population in which 52% were White, 18% were Hispanic/Latino or Spanish, 20% were Black or African American, 3% were Asian, 3% identified as more than 1 race or ethnicity, and about 1% identified as American Indian or Alaska Native. Approximately 20% of participants had a high school or less education level. About 32% of participants had an annual household income of $24,999 or less (Table 1).
Table 1.
Weighted sociodemographic characteristics of sampled participants (N = 20,405)
| Characteristic | N or Mean | % or SD |
|---|---|---|
|
| ||
| Age (years) | ||
| Mean, SD (Range 18–97 years) | 55.3 | ±16.7 |
| Race and ethnicity | ||
| American Indian or Alaska Native | 231 | 1.1 |
| Another race or ethnicity | 204 | 1.0 |
| Asian | 631 | 3.1 |
| Black, African American, or African | 4036 | 19.8 |
| Hispanic, Latino, or Spanish | 3605 | 17.7 |
| Native Hawaiian or other Pacific Islander | 24 | 0.1 |
| Middle Eastern or North African | 115 | 0.6 |
| More than one race or ethnicity | 545 | 2.7 |
| White | 10,679 | 52.3 |
| Missing | 335 | 1.6 |
| Gender identity | ||
| Another gender | 33 | 0.2 |
| Man | 7757 | 38.0 |
| Multiple gender identities | 99 | 0.5 |
| Nonbinary | 44 | 0.2 |
| Transgender | 26 | 0.1 |
| Woman | 12,268 | 60.1 |
| Missing | 179 | 0.9 |
| Education | ||
| <High School | 1105 | 5.4 |
| High school/GED | 2893 | 14.2 |
| College 1–3 y | 5455 | 26.7 |
| College graduate | 5437 | 26.6 |
| Advanced degree | 5192 | 25.4 |
| Missing | 324 | 1.6 |
| Annual household income (US dollars) | ||
| ≤$24,999 | 5422 | 26.6 |
| $25,000-$49,999 | 3197 | 15.7 |
| $50,000-$99,999 | 3861 | 18.9 |
| ≥$100,000 | 4318 | 21.2 |
| Missing | 3607 | 17.7 |
| Sexual orientation | ||
| Another sexual orientation | 429 | 2.1 |
| Bisexual | 740 | 3.6 |
| Gay | 733 | 3.6 |
| Lesbian | 251 | 1.2 |
| Multiple sexual orientations | 31 | 0.2 |
| Heterosexual/straight | 17,744 | 87.0 |
| Missing | 476 | 2.3 |
| Health literacy | ||
| Low (score 0–5) | 297 | 1.5 |
| Medium (score 6–10) | 2782 | 13.6 |
| High (score 11–15) | 17,326 | 84.9 |
| Preferred language | ||
| English | 19,183 | 94.0 |
| Spanish | 1222 | 6.0 |
Most valuable types of health information
Tables 2 and 3 present weighted participant responses about the most valuable types of health information across sociodemographic groups for genetic information and other types of health information. Most participants (78.6%) indicated that it would be most valuable to receive genetic/DNA information about their risk for a serious disease when treatment is available. Over 50% of participants indicated that receiving DNA information about how they might respond to certain medications was most valuable. Out of the 14 information types listed in the survey, the top 5 most valued information types included genetic data (Table 2). The percentage of participants who selected “most valuable” for many types of genetic/DNA information increased with education level and annual household income. Nearly 80% of participants with high health literacy and who completed the survey in English thought that having information about their risk for a serious disease when treatment is available was most valuable. However, under 60% of participants with low/medium health literacy and who completed the survey in Spanish thought that this same information was most valuable. Less than 70% of participants who identified as American Indian/Alaska Native or Black thought that having information about their risk for a serious disease when treatment is available was most valuable (Table 2). About 40% of participants who identified as American Indian or Alaska Native, Black or African American, and Native Hawaiian or other Pacific Islander most valued receiving their medical record information. These results are numerically presented in Table 3 and visually presented in Supplemental Figures 1–7.
Table 2.
Weighted All of Us participant perspectives on the most valuable types of genetic information across sociodemographic groupsa,b
| Characteristic | Serious Dx, Tx Available | Pharmacogenetics | Serious Dx, No Tx Available | Genetic Ancestry | Genetic Carrier | Nonserious Dx, Tx Available | Raw Genetic Data | Nonserious Dx, No Tx Available |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Sample overall (weighted) | ||||||||
| Overall | 78.6 (13,276) | 53.2 (8985) | 49.9 (8428) | 49.7 (8394) | 48.4 (8175) | 39.9 (6739) | 18.4 (3108) | 16.1 (2719) |
| Race and ethnicityc | ||||||||
| American Indian/Alaskan Native | 65.4 (<20)d | 44.2 (<20) | 47.6 (<20) | 54.8 (<20) | 41.7 (<20) | 19.7 (<20) | 20.9 (<20) | 7.2 (<20) |
| Another Race or Ethnicity | 83.3 (<20) | 61.1 (<20) | 46.0 (<20) | 55.7 (<20) | 50.7 (<20) | 39.8 (<20) | 22.4 (<20) | 12.1 (<20) |
| Asian | 86.0 (<20) | 58.6 (<20) | 55.3 (<20) | 36.6 (<20) | 51.7 (<20) | 44.2 (<20) | 23.3 (<20) | 16.6 (<20) |
| Black | 60.3 (2013) | 40.5 (1352) | 42.1 (1405) | 59.8 (1996) | 40.7 (1359) | 20.0 (668) | 27.9 (931) | 11.7 (391) |
| Hispanic/Latino | 70.2 (2092) | 49.6 (1478) | 55.1 (1642) | 57.9 (1726) | 58.2 (1735) | 30.8 (918) | 20.2 (602) | 18.1 (540) |
| Middle Eastern/North African | 86.0 (<20) | 59.0 (<20) | 56.0 (<20) | 38.3 (<20) | 53.3 (<20) | 50.9 (<20) | 26.1 (<20) | 16.4 (<20) |
| More than One Race or Ethnicity | 79.0 (<20) | 51.7 (<20) | 49.2 (<20) | 56.2 (<20) | 49.6 (<20) | 39.1 (<20) | 22.9 (<20) | 15.0 (<20) |
| Pacific Islander | 100.0 (<20) | 53.5 (<20) | 33.8 (<20) | 52.1 (<20) | 29.6 (<20) | 29.6 (<20) | 18.3 (<20) | 11.2 (<20) |
| White | 87.8 (7768) | 58.7 (5193) | 50.9 (4503) | 43.5 (3848) | 47.7 (4220) | 50.5 (4468) | 13.6 (1203) | 17.4 (1539) |
| Gender identity | ||||||||
| Another gender | 87.5 (<20) | 70.2 (<20) | 67.4 (<20) | 37.6 (<20) | 29.8 (<20) | 49.8 (<20) | 15.0 (<20) | 29.8 (<20) |
| Man | 75.4 (4842) | 49.7 (3191) | 48.7 (3127) | 47.9 (3076) | 41.2 (2646) | 36.7 (2357) | 19.9 (1278) | 16.3 (1047) |
| Multiple gender identities | 84.1 (<20) | 68.9 (<20) | 55.4 (<20) | 37.0 (<20) | 31.1 (<20) | 48.1 (<20) | 16.3 (<20) | 13.1 (<20) |
| Nonbinary | 90.7 (<20) | 67.8 (<20) | 61.9 (<20) | 36.4 (<20) | 25.4 (<20) | 56.8 (<20) | 29.7 (<20) | 22.0 (<20) |
| Transgender | 70.7 (<20) | 54.6 (<20) | 49.9 (<20) | 55.1 (<20) | 19.5 (<20) | 42.1 (<20) | 35.0 (<20) | 28.4 (<20) |
| Woman | 80.5 (8174) | 55.2 (5605) | 50.5 (5128) | 51.0 (5178) | 53.2 (5402) | 41.8 (4244) | 17.5 (1777) | 15.9 (1614) |
| Education | ||||||||
| < High school | 51.9 (414) | 39.3 (313) | 47.9 (382) | 52.9 (422) | 50.0 (399) | 21.7 (173) | 27.3 (218) | 14.0 (112) |
| High school/GED | 61.1 (1313) | 44.6 (958) | 42.6 (915) | 55.6 (1195) | 47.9 (1029) | 24.8 (533) | 21.9 (471) | 12.7 (273) |
| College 1–3 yrs | 74.8 (3462) | 48.1 (2226) | 49.5 (2291) | 56.2 (2601) | 49.3 (2282) | 32.7 (1514) | 21.7 (1004) | 14.8 (685) |
| College Graduate | 85.8 (3969) | 55.9 (2586) | 52.5 (2429) | 47.9 (2216) | 48.1 (2225) | 45.4 (2100) | 16.6 (768) | 17.7 (819) |
| Advanced Degree | 88.8 (3966) | 62.4 (2787) | 51.8 (2314) | 41.2 (1840) | 47.5 (2122) | 52.7 (2354) | 13.6 (607) | 17.9 (800) |
| Annual household income | ||||||||
| ≤$24,999 | 65.0 (2898) | 45.6 (2033) | 46.7 (2082) | 58.6 (2613) | 43.1 (1922) | 27.3 (1217) | 24.8 (1106) | 13.4 (597) |
| $25,000-$49,999 | 82.3 (2175) | 54.1 (1430) | 50.1 (1324) | 52.5 (1387) | 49.5 (1308) | 39.5 (1044) | 20.1 (531) | 16.1 (425) |
| $50,000-$99,999 | 86.9 (2795) | 57.4 (1846) | 51.1 (1644) | 46.6 (1499) | 50.7 (1631) | 47.3 (1521) | 14.3 (460) | 18.2 (585) |
| ≥$100,000 | 91.6 (3313) | 60.6 (2192) | 53.7 (1942) | 37.1 (1342) | 51.8 (1873) | 56.7 (2050) | 11.9 (430) | 18.4 (665) |
| Sexual orientation | ||||||||
| Another sexual orientation | 72.1 (252) | 48.3 (169) | 48.0 (168) | 39.6 (138) | 32.1 (112) | 43.7 (153) | 15.2 (53) | 17.0 (59) |
| Bisexual | 77.1 (<20) | 54.3 (<20) | 51.6 (<20) | 50.4 (<20) | 42.7 (<20) | 39.5 (<20) | 29.9 (<20) | 17.4 (<20) |
| Gay | 73.9 (463) | 56.0 (351) | 53.9 (338) | 54.4 (341) | 12.7 (80) | 41.8 (262) | 21.6 (135) | 20.1 (126) |
| Lesbian | 82.0 (<20) | 57.8 (<20) | 51.6 (<20) | 51.4 (<20) | 27.1 (<20) | 43.1 (<20) | 19.9 (<20) | 13.5 (<20) |
| Multiple sexual orientations | 69.9 (<20) | 43.7 (<20) | 61.6 (<20) | 50.5 (<20) | 44.7 (<20) | 26.0 (<20) | 49.9 (<20) | 26.9 (<20) |
| Heterosexual/straight | 79.3 (11,646) | 53.0 (7784) | 49.7 (7299) | 49.7 (7299) | 51.0 (7490) | 40.0 (5874) | 17.7 (2599) | 15.9 (2335) |
| Health literacy | ||||||||
| Low | 56.9 (<20) | 37.2 (<20) | 46.3 (<20) | 47.7 (<20) | 35.3 (<20) | 30.6 (<20) | 26.1 (<20) | 12.4 (<20) |
| Medium | 59.4 (1305) | 44.1 (969) | 45.7 (1004) | 53.4 (1173) | 44.2 (971) | 23.7 (521) | 24.0 (527) | 13.3 (292) |
| High | 81.9 (11,826) | 54.9 (7927) | 50.6 (7306) | 49.2 (7104) | 49.2 (7104) | 42.5 (6137) | 17.4 (2512) | 16.6 (2397) |
| Preferred language | ||||||||
| English | 80.0 (12,702) | 53.3 (8463) | 49.3 (7828) | 49.3 (7828) | 47.3 (7510) | 40.8 (6478) | 19.0 (3017) | 15.8 (2509) |
| Spanish | 57.5 (582) | 50.9 (515) | 59.3 (600) | 56.2 (569) | 65.9 (667) | 26.4 (267) | 8.3 (84) | 21.1 (214) |
Dx, diagnosis, Tx, treatment.
Data presented in Tables 2 and 3 were collected as part of a single survey question but are shown in 2 separate tables for ease of interpretation.
Data shown are weighted results to allow for generalization to the entire All of Us population and are not raw statistics.
Results should not be interpreted to represent the views of everyone across diverse Tribal Nations or diverse racial/ethnic groups.
Because of All of Us privacy policies, any participant row containing a count of less than 20 must be hidden and marked as "<20."
Table 3.
Weighted All of Us participant perspectives on the most valuable types of general health information across sociodemographic groupsa,b
| Characteristic | Results of Environmental Marker Labs | Medical Records | Results of Routine Labs | Physical Measurements | All of Us Survey Responses | Fitness Tracker Data |
|---|---|---|---|---|---|---|
|
| ||||||
| Sample overall (weighted) | ||||||
| Overall | 35.1 (5928) | 24.6 (4155) | 22.8 (3851) | 6.7 (1132) | 4.8 (811) | 4.4 (743) |
| Race and ethnicityc | ||||||
| American Indian/Alaskan Native | 40.6 (<20)d | 38.1 (<20) | 38.1 (<20) | 11.7 (<20) | 10.8 (<20) | 7.3 (<20) |
| Another race | 38.5 (<20) | 22.5 (<20) | 15.3 (<20) | 3.3 (<20) | 4.4 (<20) | 3.7 (<20) |
| Asian | 37.6 (<20) | 21.3 (<20) | 21.4 (<20) | 8.4 (<20) | 3.4 (<20) | 3.9 (<20) |
| Black | 27.9 (931) | 39.5 (1319) | 35.9 (1198) | 14.2 (474) | 9.1 (304) | 7.6 (254) |
| Hispanic/Latino | 25.2 (751) | 24.1 (718) | 25.1 (748) | 8.8 (262) | 5.6 (167) | 3.9 (116) |
| Middle Eastern/North African | 28.9 (<20) | 13.1 (<20) | 17.7 (<20) | 7.0 (<20) | 3.3 (<20) | 3.6 (<20) |
| More than one race or ethnicity | 40.1 (<20) | 23.4 (<20) | 20.0 (<20) | 4.3 (<20) | 3.0 (<20) | 3.4 (<20) |
| Pacific Islander | 47.9 (<20) | 40.8 (<20) | 35.2 (<20) | 5.6 (<20) | 18.3 (<20) | 5.6 (<20) |
| White | 40.5 (3583) | 19.3 (1707) | 17.2 (1522) | 3.3 (292) | 3.0 (265) | 3.5 (310) |
| Gender identity | ||||||
| Another gender | 40.1 (<20) | 20.1 (<20) | 12.5 (<20) | 2.5 (<20) | 2.5 (<20) | 2.5 (<20) |
| Man | 34.1 (2190) | 29.8 (1914) | 25.9 (1663) | 8.3 (533) | 5.8 (372) | 6.3 (405) |
| Multiple gender identities | 48.8 (<20) | 16.8 (<20) | 19.7 (<20) | 5.6 (<20) | 4.8 (<20) | 3.3 (<20) |
| Nonbinary | 47.5 (<20) | 13.6 (<20) | 10.2 (<20) | 0.8 (<20) | 1.7 (<20) | 2.5 (<20) |
| Transgender | 30.7 (<20) | 20.7 (<20) | 20.6 (<20) | 8.1 (<20) | 11.1 (<20) | 1.8 (<20) |
| Woman | 35.5 (3604) | 21.4 (2173) | 20.9 (2122) | 5.8 (589) | 4.2 (426) | 3.3 (335) |
| Education | ||||||
| <High school | 18.9 (151) | 34.4 (274) | 36.7 (292) | 12.3 (98) | 14.4 (115) | 6.3 (50) |
| High school/GED | 27.6 (593) | 34.5 (741) | 33.2 (713) | 12.8 (275) | 8.9 (191) | 7.2 (155) |
| College 1–3 Years | 31.4 (1453) | 28.6 (1324) | 26.3 (1217) | 7.6 (352) | 4.2 (194) | 3.9 (181) |
| College Graduate | 39.1 (1809) | 21.4 (990) | 18.6 (860) | 4.7 (217) | 3.3 (153) | 4.4 (204) |
| Advanced Degree | 41.6 (1858) | 17.1 (764) | 15.8 (706) | 4.0 (179) | 3.3 (147) | 3.6 (161) |
| Annual household income | ||||||
| ≤ $24,999 | 28.5 (1271) | 33.4 (1489) | 30.1 (1342) | 10.4 (464) | 6.8 (303) | 6.3 (281) |
| $25,000-$49,999 | 35.7 (943) | 23.6 (624) | 21.9 (579) | 5.4 (143) | 3.6 (95) | 3.4 (90) |
| $50,000-$99,999 | 39.9 (1283) | 19.9 (640) | 18.9 (608) | 3.9 (125) | 3.1 (100) | 4.3 (138) |
| ≥$100,000 | 42.5 (1537) | 15.8 (571) | 13.7 (495) | 3.2 (116) | 2.9 (105) | 3.2 (116) |
| Sexual orientation | ||||||
| Another sexual orientation | 40.6 (142) | 29.5 (103) | 26.5 (93) | 10.2 (36) | 11.7 (41) | 5.7 (20) |
| Bisexual | 38.8 (<20) | 21.5 (<20) | 16.6 (<20) | 7.9 (<20) | 2.9 (<20) | 3.7 (<20) |
| Gay | 39.4 (247) | 30.8 (193) | 25.5 (160) | 9.2 (58) | 4.7 (29) | 5.8 (36) |
| Lesbian | 46.6 (<20) | 22.7 (<20) | 19.4 (<20) | 4.7 (<20) | 3.0 (<20) | 3.6 (<20) |
| Multiple sexual orientations | 48.6 (<20) | 17.7 (<20) | 42.9 (<20) | 0.0 (<20) | 0.0 (<20) | 3.7 (<20) |
| Heterosexual/straight | 34.5 (5067) | 24.3 (3569) | 22.7 (3334) | 6.4 (940) | 4.7 (690) | 4.4 (646) |
| Health literacy | ||||||
| Low | 27.7 (<20) | 33.8 (<20) | 41.7 (<20) | 12.4 (<20) | 7.8 (<20) | 6.6 (<20) |
| Medium | 28.5 (626) | 35.3 (776) | 33.2 (729) | 12.8 (281) | 9.8 (215) | 7.4 (163) |
| High | 36.2 (5227) | 22.8 (3292) | 20.9 (3018) | 5.7 (823) | 4.0 (578) | 3.9 (563) |
| Preferred language | ||||||
| English | 36.4 (5780) | 24.5 (3890) | 22.3 (3541) | 6.4 (1016) | 4.5 (715) | 4.5 (715) |
| Spanish | 13.6 (138) | 25.9 (262) | 31.5 (319) | 11.6 (117) | 9.9 (100) | 3.9 (39) |
Data presented in Tables 2 and 3 were collected as part of a single survey question but are shown in 2 separate tables for ease of interpretation.
Data shown are weighted results to allow for generalization to the entire All of Us population and are not raw statistics.
Results should not be interpreted to represent the views of everyone across diverse Tribal Nations or diverse racial/ethnic groups.
Because of All of Us privacy policies, any participant row containing a count of less than 20 must be hidden and marked as “<20.”
As income and education levels increased, the odds of placing value on genetic results indicating risk of serious or nonserious disease when treatment is available increased when compared with the lowest income and education levels (Figure 1). The odds of valuing information on serious disease with available treatment were 2.34 (P value < .001) times higher for the highest income group compared with the lowest, and 2.26 (P value < .001) times higher for the most educated group compared with the least. The odds of finding genetic heterozygote information valuable were much higher for participants who identified as heterosexual/straight compared with those who identified as gay (5.5), lesbian (2.9), or bisexual (1.4) (all P values < .001). The odds of placing the most value on All of Us survey responses were much higher for those with the lowest level of education compared with those with some college experience or greater. Those who completed the Spanish language version had higher odds of valuing genetic heterozygote information and the risk of a nonserious disease with no available treatment. Those who completed the survey in English had higher odds of valuing environmental marker lab tests, raw genetic data, and the risk of serious disease with treatment available.
Figure 1.
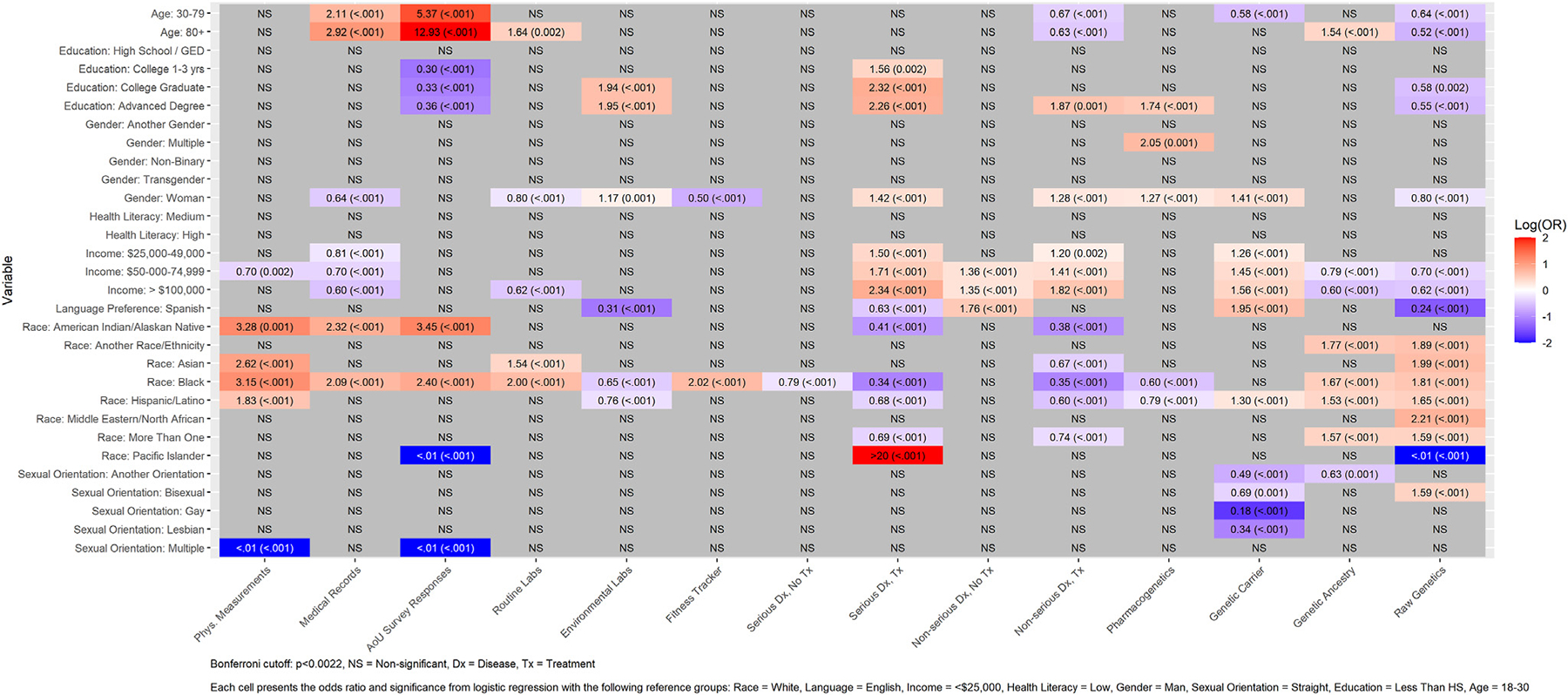
Weighted logistic regression results: Most valuable types of information to All of Us participants.
Access to providers to facilitate understanding of genetic information
The top 3 provider types that participants reported being able to access for help understanding genetic information were a primary care physician (74.6%), specialist physician (61.5%), and genetic counselor (45.4%). The percentage of participants who reported having access to these 3 provider types increased along with increasing education and income levels. The opposite pattern occurred for access to community health center providers; as education and income increased, smaller percentages of participants reported access to this provider type (Table 4). A greater percentage of participants with less than high school education reported not having a place to go for help when compared with those with an advanced degree (8.5% versus 2.0%). Only 26.8% of participants with low health literacy and 29.0% of participants who took the survey in Spanish could access a genetic counselor, but over 45% participants with high health literacy and who took the survey in English could access a genetic counselor. Also, a smaller percentage of those who completed the survey in Spanish could access a primary care or specialist provider compared with those who completed the survey in English (Table 4). Supplemental Figures 8 to 14 visually showcase participant access to provider types across sociodemographic groups.
Table 4.
Provider types All of Us participants can access for help understanding genetic information across sociodemographic groups, weighted resultsa
| Characteristic | Primary Care Physician | Specialist Physician | Genetic Counselor | Community Health Center | Emergency Department | Unsure | Urgent Care | Don’t Have a Place |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Sample overall (weighted) | ||||||||
| Overall | 74.6 (13564) | 61.5 (11182) | 45.4 (8255) | 12.8 (2327) | 10.8 (1964) | 10.5 (1909) | 10.4 (1891) | 3.8 (691) |
| Race and ethnicityb | ||||||||
| American Indian/ Alaskan Native | 78.3 (<20)c | 60.6 (<20) | 34.3 (<20) | 20.7 (<20) | 16.2 (<20) | 11.5 (<20) | 17.6 (<20) | 1.4 (<20) |
| Another race or ethnicity | 71.0 (<20) | 59.5 (<20) | 47.9 (<20) | 10.3 (<20) | 8.1 (<20) | 14.0 (<20) | 9.1 (<20) | 4.1 (<20) |
| Asian | 70.5 (397) | 60.3 (340) | 52.3 (295) | 11.2 (63) | 7.4 (42) | 10.7 (60) | 8.7 (49) | 3.6 (20) |
| Black | 76.3 (2742) | 55.3 (1987) | 38.5 (1384) | 20.3 (730) | 17.0 (611) | 12.2 (438) | 17.8 (640) | 4.9 (176) |
| Hispanic/Latino | 64.3 (2065) | 50.3 (1615) | 37.0 (1188) | 18.8 (604) | 10.3 (331) | 13.8 (443) | 10.2 (328) | 7.5 (241) |
| Middle Eastern/ North African | 59.1 (<20) | 57.9 (<20) | 46.4 (<20) | 10.3 (<20) | 8.6 (<20) | 12.7 (<20) | 9.8 (<20) | 4.8 (<20) |
| More than one race or ethnicity | 71.8 (347) | 61.6 (298) | 48.5 (234) | 11.9 (58) | 10.2 (49) | 12.9 (62) | 9.7 (47) | 5.1 (25) |
| Pacific Islander | 84.0 (<20) | 57.0 (<20) | 58.0 (<20) | 26.0 (<20) | 21.0 (<20) | 0.0 (<20) | 26 (<20) | 0.0 (<20) |
| White | 78.0 (7426) | 67.7 (6445) | 50.4 (4798) | 8.0 (762) | 8.8 (838) | 8.6 (819) | 7.8 (743) | 2.2 (209) |
| Gender identity | ||||||||
| Another gender | 66.2 (<20) | 66.2 (<20) | 56.4 (<20) | 12.3 (<20) | 4.9 (<20) | 17.2 (<20) | 7.4 (<20) | 6.9 (<20) |
| Man | 76.0 (5255) | 61.3 (4239) | 41.0 (2835) | 14.6 (1010) | 13.0 (899) | 10.3 (712) | 13.0 (899) | 3.9 (270) |
| Multiple gender identities | 75.2 (<20) | 60.0 (<20) | 53.9 (<20) | 19.5 (<20) | 7.0 (<20) | 14 (<20) | 7.0 (<20) | 7.1 (<20) |
| Nonbinary | 72.4 (<20) | 58.5 (<20) | 53.7 (<20) | 10.6 (<20) | 4.9 (<20) | 18.7 (<20) | 4.1 (<20) | 6.5 (<20) |
| Transgender | 76.0 (<20) | 60.5 (<20) | 63.2 (<20) | 12.8 (<20) | 16.5 (<20) | 8.2 (<20) | 14.5 (<20) | 2.6 (<20) |
| Woman | 73.8 (8065) | 61.6 (6731) | 48.1 (5256) | 11.7 (1279) | 9.4 (1027) | 10.6 (1158) | 8.8 (962) | 3.7 (404) |
| Education | ||||||||
| <High school | 60.5 (533) | 39.5 (348) | 23.6 (208) | 25.3 (223) | 13.8 (122) | 17.2 (152) | 14.0 (123) | 8.5 (75) |
| High school/GED | 72.6 (1761) | 48.6 (1179) | 30.9 (749) | 19.4 (470) | 15.1 (366) | 14.5 (352) | 15.4 (373) | 5.2 (126) |
| College 1–3 years | 75.5 (3746) | 60.1 (2982) | 41.7 (2069) | 14.3 (709) | 12.8 (635) | 11.2 (556) | 11.9 (590) | 4.9 (243) |
| College graduate | 77.0 (3799) | 66.0 (3257) | 50.0 (2467) | 11.0 (543) | 9.6 (474) | 9.1 (449) | 9.7 (479) | 2.7 (133) |
| Advanced degree | 75.2 (3555) | 69.5 (3286) | 56.5 (2671) | 7.3 (345) | 7.0 (331) | 7.5 (355) | 6.5 (307) | 2.0 (95) |
| Annual household income | ||||||||
| ≤ $24,999 | 72.9 (3501) | 53.5 (2570) | 38.5 (1849) | 20.0 (961) | 15.0 (720) | 12.6 (605) | 14.8 (711) | 5.6 (269) |
| $25,000-$49,999 | 76.1 (2167) | 60.2 (1714) | 43.2 (1230) | 12.3 (350) | 10.1 (288) | 11.3 (322) | 9.9 (282) | 3.3 (94) |
| $50,000-$99,999 | 75.9 (2633) | 66.4 (2304) | 50.2 (1742) | 8.0 (278) | 7.7 (267) | 8.2 (284) | 7.3 (253) | 2.8 (97) |
| ≥$100,000 | 78.0 (3019) | 72.4 (2802) | 57.6 (2230) | 5.7 (221) | 7.0 (271) | 6.4 (248) | 7.1 (275) | 1.5 (58) |
| Sexual orientation | ||||||||
| Another sexual orientation | 70.6 (270) | 61.6 (236) | 42.7 (164) | 20.7 (79) | 14.2 (54) | 14.0 (54) | 14.8 (57) | 5.9 (23) |
| Bisexual | 78.7 (<20) | 58.8 (<20) | 52.9 (<20) | 18.8 (<20) | 14.9 (<20) | 12.4 (<20) | 13.7 (<20) | 2.5 (<20) |
| Gay | 76.0 (<20) | 61.4 (<20) | 44.0 (<20) | 15.0 (<20) | 11.0 (<20) | 11.5 (<20) | 9.8 (<20) | 2.6 (<20) |
| Lesbian | 69.0 (<20) | 59.1 (<20) | 47.3 (<20) | 7.3 (<20) | 9.9 (<20) | 10.8 (<20) | 6.9 (<20) | 2.4 (<20) |
| Multiple sexual orientations | 83.7 (<20) | 79.1 (<20) | 66.5 (<20) | 35.2 (<20) | 25.2 (<20) | 11.9 (<20) | 29.9 (<20) | 1.4 (<20) |
| Heterosexual/straight | 74.6 (11,787) | 61.8 (9765) | 45.2 (7142) | 12.2 (1928) | 10.4 (1643) | 10.2 (1612) | 10.2 (1612) | 3.9 (616) |
| Health literacy | ||||||||
| Low | 67.3 (<20) | 39.6 (<20) | 26.8 (<20) | 17.2 (<20) | 8.3 (<20) | 19.6 (<20) | 7.3 (<20) | 4.1 (<20) |
| Medium | 72.1 (1738) | 51.0 (1230) | 31.7 (764) | 20.6 (497) | 16.9 (407) | 14.7 (354) | 15.4 (371) | 5.3 (128) |
| High | 75.2 (11,659) | 63.5 (9845) | 47.8 (7411) | 11.5 (1783) | 9.9 (1535) | 9.7 (1504) | 9.7 (1504) | 3.6 (558) |
| Preferred language | ||||||||
| English | 76.1 (13,008) | 62.5 (10,683) | 46.4 (7931) | 11.9 (2034) | 10.7 (1829) | 10.2 (1743) | 10.4 (1778) | 3.4 (581) |
| Spanish | 51.0 (556) | 46.2 (503) | 29.0 (316) | 26.4 (228) | 12.8 (139) | 15.0 (163) | 11.0 (120) | 10.1 (110) |
Data shown are weighted results to allow for generalization to the entire All of Us population and are not raw statistics.
Results should not be interpreted to represent the views of everyone across diverse Tribal Nations or diverse racial/ethnic groups.
Because of All of Us privacy policies, any participant row containing a count of less than 20 must be hidden and marked as “<20.”
The odds of specialist physician access were 1.98, 1.97, and 1.64 times higher for gay, lesbian, and bisexual participants (all P values < .001), respectively, compared with heterosexual/straight respondents, whereas the respective odds were 2.07, 2.60, and 1.59 times higher (all P values < .001) for genetic counselor access. Those in the highest 2 income levels reported higher odds of having access to a specialist physician compared with the lowest income level, and White respondents had higher odds compared with Hispanic and Asian respondents for access to this provider type (Supplemental Figure 15).
Discussion
We surveyed over 20,000 All of Us participants about the return of value in research. The top 5 most valued information types were information about genetic risk for serious disease when treatment is available, pharmacogenetics, genetic risk for serious disease when treatment is unavailable, genetic ancestry, and risk for being a genetic heterozygote. Our findings echo previous literature suggesting that receiving genetic information is highly valuable to research participants, providing them an avenue to assess personal utility of results for themselves and their families.21–23 Our study provides new insights about the specific types of genetic data participants find most valuable and how these preferences vary across diverse sociodemographic populations. Considerable variation appeared in perspectives about the most valuable information types within sociodemographic groups. Information about genetic risk for serious disease when treatment is available was selected as the most valuable by the greatest percentage of participants in the overall sample (78.6%); yet, there were notable differences in the value of this information within sociodemographic groups. Nearly 90% of participants with an advanced degree perceived this type of information was most valuable compared with 52% of participants with less than a high school education. Likewise, participants with high health literacy who preferred English had a 20% higher preference for this information compared with those with low health literacy preferring Spanish. It is possible that individuals with higher education or socioeconomic status place greater value on receiving information about genetic risk for serious disease when treatment is available because of increased access to resources needed to act on these results. Relatedly, prior research suggests populations with lower socioeconomic status may place higher value on health-related topics that have an immediate impact on their life compared with genetic information that may pose future risk.24 A similar relationship may exist with health literacy and preferred language because those with lower health literacy and who prefer Spanish may face additional barriers accessing resources needed to act on genetic results. Accordingly, initiatives are needed to ensure that individuals with fewer resources receive results that matter most to them and can access help to understand how these results may affect health outcomes.
There are also consistent differences in the proportion of participants who placed value on serious diseases with and without treatments. As a whole, the average proportion of respondents who valued information on serious diseases with a treatment was 30% higher than diseases with no treatment. Although information on diseases with no treatments was still increasingly valued as education and income levels increased, the association was much weaker. The difference between the lowest and highest income levels was just 7% for diseases without a treatment compared with a 35% difference if there was a treatment. Similarly, only a 4% difference existed between the highest and lowest education levels for diseases without a treatment compared with a 25% difference for treatable diseases. Differences also existed between racial groups. People identifying as Asian or Native Hawaiian or other Pacific Islanders saw declines over 30% for untreatable diseases compared with treatable ones, whereas Hispanic and Black or African American respondents had declines less than 18%. A reason may be that participants as a whole saw considerably less value in learning about conditions over which they had no control, which appears to have been more pronounced among certain racial and ethnic groups. Removing the treatment ability from the disease information also removed the association between income and education level, indicating that lack of resources may have played a lesser role for untreatable diseases.
Variation also appeared in preferences for receiving information types not considered highly valuable by the overall sample. Around 40% of participants who identified as American Indian or Alaska Native, Black or African American, or Native Hawaiian or other Pacific Islander thought receiving information about their medical records was most valuable compared with 25% in the overall sample. This result may reflect racial and ethnic inequities in use of and access to electronic patient portals, which is an increasingly common way for patients to access their clinical medical records.25,26 Accordingly, returning medical record information, especially to populations from minoritized racial and ethnic groups who express interest in receiving this information, may represent an important strategy for reducing inequities in access to personal health information. Pairing returned medical record information with support from primary care or other providers to help participants understand this information may have the most impact. Overall, our findings suggest researchers should not presume information types reported as low value among most study participants are also of low value to racially and ethnically diverse participants.
Primary care physicians, specialist physicians, and genetic counselors were the top 3 provider types that participants reported having access to for support to help them understand and use the information they receive.6 Access to these 3 provider types generally increased with increasing education and annual income levels. About three-quarters of participants overall reported having access to a primary care provider, but only 60% of participants with less than a high school education and half of participants who completed the survey in Spanish could access a primary care provider. These results correspond to prior research suggesting that individuals with lower education levels and limited English proficiency experience greater barriers to accessing health care in the US.27,28 Additionally, genetic counselors may be uniquely positioned to help participants gain value from returned genetic results.29 About 45% of participants overall could access a genetic counselor for help interpreting results, but fewer than 25% of participants with less than a high school education could access a genetic counselor. These results suggest that policies are needed to increase access to health providers who can help patients understand returned results, especially for patients with lower education levels and who speak Spanish as a preferred language. It may also be beneficial to support programs that increase access to providers with similar expertise at community health centers—a location that our results suggest may be more accessible among participants with lower income levels and who prefer Spanish. These providers should be prepared to present findings in a way that is comprehendible and demonstrate benefit, whether now or distally. Ideally, researchers will connect participants with providers who have the expertise necessary to explain returned information (eg, genetic counselors may be most appropriate for genetic information, whereas primary care or specialist providers may be most appropriate for medical record information).
Aligning with participant priorities to present findings in a comprehendible and useful way, All of Us is providing a genetic counseling resource to participants who have certain genetic findings. All of Us held listening sessions before enrolling its first participant, and community participants expressed the importance of ensuring that study participants who received genetic results were also provided with resources and tools to discuss the research results and understand any clinical implications of their results. Subsequently, All of Us partnered with Color (a genetic testing support service) and the All of Us Genetic Counseling Resource. Resources are also available to participants in the program through the regional medical centers, Federally Qualified Health Centers, Veteran’s Administration, and other places that can provide a medical home (eg, primary care providers). The All of Us program took additional steps to provide resources to Color to ensure that each participant who received an actionable finding had access to a genetic counselor. To address issues of inequity potentially arising from limited access to follow-up testing, the program also provides a free clinical confirmatory test through Color for all participants who request one. Additionally, Color provides tools that participants can use to discuss their findings with their medical team and family members. Future programs should consider identifying the needed resources to support the interpretation of research versus clinical findings and to address inequities in access to care by ensuring participants have awareness of and access to genetic counseling resources.
Important limitations should be noted. First, this was a cross-sectional survey. Results reflect perspectives at a single time point. Second, All of Us only recruits participants in the United States. Participants in other countries may have different perspectives regarding return of value.30 Third, because All of Us is not a representative sample of the US population, the analysis incorporated sampling weights to reflect the All of Us cohort from which participants were sampled and invited to complete the survey, rather than to represent the entire US population.
A key strength of this study is our sampling strategy, which focused on surveying participants from diverse sociodemographic groups. Of note, our sampling rate was 11.4%, which was not entirely unexpected as previous research has found significant differences in response rates across diverse sociodemographic groups.31 The diverse participant sample also facilitated a data analysis approach in which we did not combine participants from multiple historically minoritized identities into single categories. This approach allowed us to conduct a novel analysis of perspectives for receiving health-related information across a diverse sample of participants, traditionally underrepresented in research. Although respondents were diverse in their self-identified race/ethnicity, results should not be interpreted to represent the views of everyone across diverse racial/ethnic groups or diverse Tribal Nations. Also, our study focused on the return of value for individual study participants. Future research is needed to understand return of value to communities. Future research is also needed to apply intersectionality theory32 to examine how intersecting systems of oppression affect return of value perspectives for populations who have been historically marginalized at multiple intersections (eg, individuals who identify with a historically marginalized racial, ethnic, and/or sexual orientation group who also have low education, income, and/or health literacy). Examining intersecting barriers to care is an important call for future research that applies intersectionality theory to conduct such investigations.
Conclusion
Although genetic information was most valuable to participants, preferences about specific information types varied across sociodemographic groups. Researchers should not assume that participant preferences for receiving research results are uniform within diverse study populations. Future work is needed to ensure that all research participants receive results they find valuable and understandable, and to identify other information of value that research participants want to receive in addition to genetic health information.
Supplementary Material
Acknowledgments
The authors are grateful for Xiaoke Feng’s support on participant sampling. The authors gratefully acknowledge the All of Us participants for their contributions, without whom this research would not have been possible. The authors also thank the National Institutes of Health’s All of Us Research Program for making available the participant cohort data examined in this study. The authors appreciate the support of the Participant Evaluation and Assessment Board (PEAB), Spanish Translation Team, the All of Us Data and Research Center at Vanderbilt University Medical Center. The authors also appreciate the review by the Tribal Engagement Team Lead and the All of Us Division of Engagement and Outreach.
Funding
This work was supported by the National Institutes of Health (NIH) National Center for Advancing Translational Sciences grant UL1TR002243; All of Us Data and Research Center NIH grant 1 OT2 OD35404 and the All of Us Research Program Engagement Core NIH grant 1 OT2 OD035980; the National Cancer Institute (K99CA277366, R00CA277366, and L60CA264691); and the Agency for Healthcare Research and Quality (T32HS026122).
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
Ethics Declaration
The study protocol was approved by the All of Us Institutional Review Board. The All of Us Institutional Review Board deemed this study exempt. Informed consent was not required as this study received a non-human subject’s research determination exempt review.
Other Disclosures
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional Information
The online version of this article (https://doi.org/10.1016/j.gim.2024.101163) contains supplemental material, which is available to authorized users.
Data Availability
The authors will make relevant anonymized survey data available to collaborators external to their team on email request, assuming that they can make appropriate arrangements to safeguard any sensitive information participants might have revealed in the course of the survey and ensure that collaborators receiving data are able to adhere to the expressed preferences and concerns of the researchers and participant partners involved in governance of this project. In accordance with All of Us policies, row-level participant data for this study will not be made available to individuals who were not involved in the study.
References
- 1.Wilkins CH, Mapes BM, Jerome RN, Villalta-Gil V, Pulley JM, Harris PA. Understanding what information is valued by research participants, and why. Health Aff (Millwood). 2019;38(3):399–407. 10.1377/hlthaff.2018.05046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canedo JR, Villalta-Gil V, Grijalva CG, Schlundt D, Jerome RN, Wilkins CH. How do hispanics/latinos perceive and value the return of research results? Hisp Health Care Int. 2022;20(4):238–247. 10.1177/15404153211070821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong CA, Hernandez AF, Califf RM. Return of research results to study participants: uncharted and untested. JAMA. 2018;320(5):435–436. 10.1001/jama.2018.7898 [DOI] [PubMed] [Google Scholar]
- 4.Wolf SM, Green RC. Return of results in genomic research using largescale or whole genome sequencing: toward a new normal. Annu Rev Genomics Hum Genet. 2023;24:393–414. 10.1146/annurev-genom-101122-103209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vears DF, Minion JT, Roberts SJ, et al. Return of individual research results from genomic research: a systematic review of stakeholder perspectives. PLoS One. 2021;16(11):e0258646. 10.1371/journal.pone.0258646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Academies of Sciences, Engineering, and Medicine. Returning Individual Research Results to Participants: Guidance for a New Research Paradigm. The National Academies Press; 2018. [PubMed] [Google Scholar]
- 7.All of US research program overview. All of US Research Program. Accessed November 20, 2023. https://allofus.nih.gov/about/program-overview
- 8.Denny JC, Rutter JL, et al. , All of Us Research Program Investigators. The “All of Us” research program. N Engl J Med. 2019;381(7):668–676. 10.1056/NEJMsr1809937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.All of US Research Program protocol. All of US Research Program. Accessed November 20, 2023. https://allofus.nih.gov/about/all-us-research-program-protocol [Google Scholar]
- 10.Bennette CS, Trinidad SB, Fullerton SM, et al. Return of incidental findings in genomic medicine: measuring what patients value—development of an instrument to measure preferences for information from next-generation testing (IMPRINT). Genet Med. 2013;15(11):873–881. 10.1038/gim.2013.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bacon PL, Harris ED, Ziniel SI, et al. The development of a preference-setting model for the return of individual genomic research results. J Empir Res Hum Res Ethics. 2015;10(2):107–120. 10.1177/1556264615572092 [DOI] [PubMed] [Google Scholar]
- 12.Wynn J, Martinez J, Duong J, et al. Research participants’ preferences for hypothetical secondary results from genomic research. J Genet Couns. 2017;26(4):841–851. 10.1007/s10897-016-0059-2 [DOI] [PubMed] [Google Scholar]
- 13.Precision Medicine Initiative (PMI) Working Group. Precision Medicine Initiative Cohort Program; Waltham – Building a Research Foundation for 21st Century Medicine. 2015. Accessed May 28, 2024 https://acd.od.nih.gov/documents/reports/PMI_WG_report_2015-09-17-Final.pdf [Google Scholar]
- 14.Grande D, Mitra N, Shah A, Wan F, Asch DA. The importance of purpose: moving beyond consent in the societal use of personal health information. Ann Intern Med. 2014;161(12):855–862. 10.7326/M14-1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The GenIUSS Group. Best Practices for Asking Questions to Identify Transgender and Other Gender Minority Respondents on Population-Based Surveys. The Williams Institute. 2014. Accessed May 28, 2024 https://williamsinstitute.law.ucla.edu/wp-content/uploads/Survey-Measures-Trans-GenIUSS-Sep-2014.pdf [Google Scholar]
- 16.Fair A, Watson KS, Cohn EG, Carpenter SM, Richardson-Heron D, Wilkins CH. Innovation in large-scale research programs: elevating research participants to governance roles through the All of US research program engagement core. Acad Med. 2022;97(12):1794–1798. 10.1097/ACM.0000000000004950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Survey explorer. All of US Research Hub. Accessed November 21, 2023. https://www.researchallofus.org/data-tools/survey-explorer/
- 18.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 19.Three-item brief health literacy screen – BHLS. Health Literacy Tool Shed. Accessed November 21, 2023. https://healthliteracy.bu.edu/bhls [Google Scholar]
- 20.Little R, Rubin D. Statistical Analysis With Missing Data. 3rd ed. Wiley; 2019. [Google Scholar]
- 21.Sayeed S, Califf R, Green R, et al. Return of individual research results: what do participants prefer and expect? PLoS One. 2021;16(7):e0254153. 10.1371/journal.pone.0254153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bollinger JM, Scott J, Dvoskin R, Kaufman D. Public preferences regarding the return of individual genetic research results: findings from a qualitative focus group study. Genet Med. 2012;14(4):451–457. 10.1038/gim.2011.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turbitt E, Kohler JN, Angelo F, et al. The PrU: development and validation of a measure to assess personal utility of genomic results. Genet Med. 2023;25(3):100356. 10.1016/j.gim.2022.12.003 [DOI] [PubMed] [Google Scholar]
- 24.Butterfield RM, Evans JP, Rini C, et al. Returning negative results to individuals in a genomic screening program: lessons learned. Genet Med. 2019;21(2):409–416. 10.1038/s41436-018-0061-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26(10):1112–1116. 10.1007/s11606-011-1728-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gordon NP, Hornbrook MC. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan. J Med Internet Res. 2016;18(3):e50. 10.2196/jmir.5105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Himmelstein J, Himmelstein DU, Woolhandler S, et al. Health Care Spending and use among Hispanic adults with and without limited English proficiency, 1999–2018. Health Aff (Millwood). 2021;40(7):1126–1134. 10.1377/hlthaff.2020.02510 [DOI] [PubMed] [Google Scholar]
- 28.Zimmerman E, Woolf SH. Understanding the Relationship between Education and Health. National Academy of Medicine; 2014. [Google Scholar]
- 29.Biesecker BB. Genetic counselors as social and behavioral scientists in the era of precision medicine. Am J Med Genet C Semin Med Genet. 2018;178(1):10–14. 10.1002/ajmg.c.31609 [DOI] [PubMed] [Google Scholar]
- 30.Milne R, Morley KI, Almarri MA, et al. Return of genomic results does not motivate intent to participate in research for all: perspectives across 22 countries. Genet Med. 2022;24(5):1120–1129. 10.1016/j.gim.2022.01.002 [DOI] [PubMed] [Google Scholar]
- 31.Wu MJ, Zhao K, Fils-Aime F. Response rates of online surveys in published research: a meta-analysis. Comp Hum Behav Rep. 2022;7:100206. 10.1016/j.chbr.2022.100206 [DOI] [Google Scholar]
- 32.Crenshaw K Demarginalizing the intersection of race and sex: a Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989;1989:Article 8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors will make relevant anonymized survey data available to collaborators external to their team on email request, assuming that they can make appropriate arrangements to safeguard any sensitive information participants might have revealed in the course of the survey and ensure that collaborators receiving data are able to adhere to the expressed preferences and concerns of the researchers and participant partners involved in governance of this project. In accordance with All of Us policies, row-level participant data for this study will not be made available to individuals who were not involved in the study.


