Abstract
Background
Twin pregnancies are associated with higher risks of adverse neonatal outcomes compared to singleton pregnancies. The choice of delivery mode, when twin A presents cephalic, remains a subject of debate. In low- and middle-income countries, where healthcare resources are limited, the decision on the mode of delivery is even more critical.
Objective
To evaluate the neonatal outcomes and the hospital costs of planned vaginal delivery compared to cesarean section (CS) in twin pregnancies with twin A presenting cephalic at Tenwek Hospital, Kenya.
Study Design
This retrospective cohort study analyzed data from all twin deliveries at Tenwek Hospital, Kenya from, April 1, 2017, to March 30, 2023. Maternal data, mode of delivery, and neonatal data were collected from delivery logs, electronic health records, and neonatal records. Neonatal outcomes were a composite of either Appearance, Pulse, Grimace, Activity, and Respiration score less than seven at 5 minutes, neonatal intensive care unit admission, resuscitation, birth trauma, or neonatal complications, including death before discharge from the hospital. A logistic regression model was created to assess the impact of the planned mode of delivery on neonatal outcomes, controlling for antenatal care clinic visits, noncephalic presentation of twin B, and birth weight category.
Results
The study included 177 twin deliveries: 129 (72.9%) were planned as vaginal deliveries and 48 (27.1%) were planned for CS. Among the planned vaginal deliveries, 66 (51.2%) experienced adverse outcomes, compared to 14 (29.2%) in the CS group (P=.009). Logistic regression showed that the odds of adverse outcomes were 0.35 times lower in the CS group compared to the planned vaginal delivery group (95% CI: 0.15–0.83; P=.017). The average total hospital costs for planned vaginal delivery were 104,608 Kenya Shillings (standard deviation 111,761) compared to 100,708 Kenya Shillings (standard deviation 75,468) for CS (P=.82).
Conclusion
Planned cesarean deliveries in twin pregnancies with twin A presenting cephalic at Tenwek Hospital were associated with fewer adverse neonatal outcomes compared to planned vaginal deliveries. There was no significant difference in hospital costs. These findings raise the question of the safest mode of delivery for patients in a resource-constrained setting.
Key words: Africa, cephalic twin A, cesarean section, delivery plan, hospital costs, low- and middle-income countries, noncephalic twin B, vaginal delivery, vertex-nonvertex
AJOG Global Reports at a Glance.
Why was this study conducted?
This study was conducted to compare neonatal outcomes and hospital costs between planned cesarean sections and planned vaginal deliveries in twin pregnancies with cephalic twin A at Tenwek Hospital, Kenya.
Key findings
Key findings indicate that planned cesarean sections for twin pregnancies with a leading cephalic twin are associated with fewer adverse neonatal outcomes compared to vaginal deliveries, without significant differences in hospital costs.
What does this add to what is known?
This study adds to the existing literature by providing evidence from a resource-constrained setting that planned cesarean sections may offer better neonatal outcomes for twin pregnancies without increasing hospital costs, challenging the perception of cesarean deliveries being invariably more expensive
Introduction
Twin gestations have a higher risk of adverse neonatal outcomes compared to singleton pregnancies.1, 2, 3, 4, 5, 6 A significant proportion of the risks to the neonate occur at delivery. The choice of delivery mode in twin pregnancies, when the leading twin presents cephalic, remains a subject of ongoing debate. Some studies have demonstrated that a planned vaginal and a planned cesarean section (CS) have equivalent neonatal outcomes7, 8, 9, 10, 11, 12; others have demonstrated an increase in adverse neonatal outcomes with vaginal delivery in this same group of twins.13, 14, 15 Interestingly, a group of studies have demonstrated an increased neonatal risk with a planned CS in this same population of twins.16, 17, 18 Thus, the best decision about the planned mode of delivery remains unclear when twin A presents cephalic.
The safest mode of delivery for a cephalic-presenting twin A has limited study in resource-constrained settings. Existing literature provides varying recommendations regarding the optimal delivery mode. There is a notable gap in research from resource-constrained settings, where different healthcare system limitations and demographic factors may influence outcomes. Healthcare costs influence decisions in such settings, and these have not been explored in the decision-making process with limited guidance to provide direction for shared decision-making to clinicians and patients.
Given the lack of clear recommendations, this study aims to investigate the impact of the planned mode of delivery on neonatal outcomes and associated healthcare costs in twin pregnancies delivered at Tenwek Hospital in Kenya. By comparing planned CS with planned vaginal deliveries, this study seeks to provide evidence-based insights to guide clinical practice in similar settings, contributing to the broader discourse on the management of twin pregnancies in resource-constrained settings.
Materials and methods
Study design and setting
This retrospective cohort study was conducted at Tenwek Hospital, Kenya, from April 1, 2017 to March 30, 2023. Ethics approval was obtained from the Tenwek Institutional Scientific and Ethical Review Committee with a research permit from the Kenya National Commission for Science, Technology, and Innovation. Tenwek Hospital is a teaching and referral hospital located in Bomet County in western Kenya, serving as a catchment center for over 800,000 people. The maternity unit, capable of managing twin deliveries, delivers approximately 3400 babies annually. Patients deliver in one of four delivery beds equipped with an electronic fetal monitor capable of monitoring twins simultaneously. The delivery area has two neonatal warmers, including oxygen and suction for initial evaluation and resuscitation.
The decision-making process for the mode of delivery in twins involves a hierarchical medical team model, formally standardized in 2019. Initially, patients are evaluated by midwives who are trained on general nursing, including obstetrics and midwifery. Their training encompasses normal and abnormal labor, and vaginal delivery of both cephalic and breech (frank and complete) presentation. Midwives manage all inductions of labor and normal labor, with varied experience levels with twin delivery. Almost all uncomplicated vaginal deliveries are performed by the midwives. When concerns arise, specialist OB/GYNs (also known as consultant OB/GYNs in Kenya or attending OB/GYNs in the United States) are called to assist. Cesarean deliveries are performed by medical officer interns, medical officers (licensed doctors without residency training), and residents under the supervision of OB/GYNs. If the patient has a twin gestation, the medical officer intern is informed and the OB/GYN then recommends the delivery plan, unless the patient presents in the second stage of labor. When both twins present cephalic, the OB/GYN typically recommends vaginal delivery. Ultimately, the mode of delivery is decided by the patient. On the rare occasions where the patient's choice differs from the recommendation, the delivery mode is chosen by the patient with ongoing communication and shared decision-making. Upon admission, twins are assessed with a period of fetal monitoring. If the fetal heart rates are satisfactory, with normal baseline rate, good variability, and no significant decelerations, the monitoring is performed intermittently depending on the progression of labor, and at minimum every 4 hours. If the FHR of either twin is not reassuring then continuous monitoring is implemented with left lateral positioning of the mother, intravenous fluids, and oxygen administration by nasal prongs until improvement of the fetal heart rates is noted or a CS is performed. Due to resource constraints and limited monitors, continuous monitoring is not always performed or documented in the medical chart. Decisions about the delivery method for twin B are based on fetal heart rate patterns and uterine contractions. The interval from cesarean decision to incision is approximately 10 to 40 minutes in emergencies.
The pediatric team, supervised by a pediatric or family medicine specialist, is present at all twin deliveries to perform immediate evaluations and necessary resuscitations, determining whether neonates require neonatal intensive care unit (NICU) admission. The hospital's infrastructure supports CS with a dedicated obstetric operating room for day procedures and additional general operating rooms for emergencies. The NICU, equipped with necessary neonatal care equipment and staffed by a specialized team, is situated near the delivery room, ensuring prompt care for newborns.
Participants
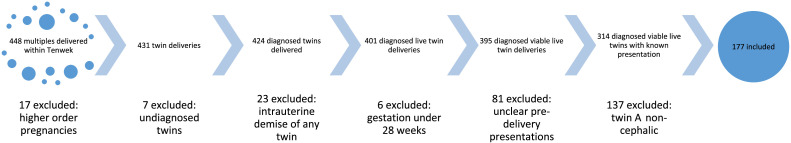
The study included both monochorionic and dichorionic twins. We reviewed records of all viable twin pregnancies delivered at Tenwek Hospital at or above 28 weeks gestation, where twin A presented cephalic. Figure illustrates the exclusions to determine the cohort.
Figure.
Flow chart describing inclusion and exclusion criteria for the cohort
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
Data collection
One hundred seventy-seven patient records meeting the inclusion criteria were retrieved from the Electronic Medical Records (EMR). Collected data included maternal age, weight, height, comorbidities, antenatal care (ANC) attendance, gestational age, presentation of twin B, gravidity, past obstetric history, labor status, planned and eventual delivery modes and their indications, birth weight, hospital bills, and neonatal outcomes.
Neonatal outcomes were a composite of either Appearance, Pulse, Grimace, Activity, and Respiration score (APGAR) score less than seven at 5 minutes, NICU admission, cardiopulmonary resuscitation, birth trauma, or neonatal complications, including death before hospital discharge. Neonatal resuscitation was defined as chest compressions or bag-valve-mask ventilation at the time of birth. Birth trauma was defined as a fracture or injury to the neonate sustained in the delivery process. A neonatal complication was defined as the presence of neonatal seizures, birth asphyxia, respiratory distress syndrome, sepsis, seizures, necrotizing enterocolitis, or severe hypoxic-ischemic encephalopathy (leading to death, or APGAR <4 at 5 minutes). Early neonatal death was defined as death after birth in the hospital, before discharge home.
The fetal presentation was documented by ultrasound at the time of admission for delivery. Gestational age was determined using the last normal menstrual dates. Very few patients in our population have first-trimester ultrasounds to date the pregnancy. When the menstrual date was uncertain or did not correlate with ultrasound, ultrasound dating was used. Because of the challenges with gestational age and missing records of estimated fetal weights, we used actual birth weight as a confounding factor. However, documentation did not clearly demarcate which birth weight corresponded to twin A or twin B. Thus, we created categories of any neonate less than 2.5 kg with low birth weight (LBW) or both twins greater than 2.5 kg.
The cost analysis was conducted by summing the charges incurred for the mother's care during admission for delivery and for the twins’ care until discharge. As a nonprofit mission hospital, patient charges are designed to closely reflect the actual costs of care. We analyzed costs from the provider's perspective, focusing on expenses related to delivering care. Patient fees include both fixed costs (eg, staff salaries, infrastructure) and variable costs (eg, consumables, medications). To accurately assess these costs, our hospital uses a bottom-up micro-costing method at the individual patient level, as previously described.19 This method involves a detailed accounting of every resource used in a patient's treatment. Indirect costs, such as administrative expenses, are allocated based on the number of inpatient days.
Data management and analysis
Data was entered and stored in a password-protected database. After duplicated data was removed, data was de-identified. Missing data was assumed to be missing completely at random. Data was analyzed using Stata version 16. Descriptive analysis was performed, and comparisons between the planned delivery modes for neonatal outcomes were made using two-sample t tests for continuous data and Pearson's chi-squared tests for nominal and categorical data. A logistic regression model was created for complete case analysis to analyze the outcome of any adverse neonatal event and the planned delivery modes, controlling for confounding factors of birth weight category, ANC visit, and noncephalic twin B presentation. These factors were carefully chosen as they impact both the exposure and outcome. Sensitivity analyses were performed to exclude all planned vaginal deliveries which were eventually delivered through CS, and also to exclude very LBW neonates (<1500 grams). Statistical significance was defined as P value ≤.05.
Results
The study analyzed 177 twin pregnancies at Tenwek Hospital. Among these, 129 (72.8%) were planned for vaginal delivery, while 48 (27.1%) were planned for CS. Demographics and characteristics are listed in Table 1. The indications for the planned mode of delivery are detailed in Table 2. The noncephalic presentation of twin B was the most common factor that determined the plan for CS. All patients with twin B presenting cephalic and the majority of those presenting twin A cephalic-twin B noncephalic had vaginal delivery planned. Two patients presented in the second stage of labor, where both twins were quickly assessed and found to be in cephalic presentation. The decision of a planned vaginal delivery was made without detailed discussion because delivery was imminent. The twins were admitted to NICU for prematurity in one set and for hypoglycemia and seizures in the other set, but without meeting any of the other components of the composite neonatal outcomes.
Table 1.
Maternal and neonatal characteristics according to the planned mode of delivery
| Factor | All | Vaginal | CS | P value |
|---|---|---|---|---|
| N | 177 | 129 | 48 | |
| Maternal age (y) | .9a | |||
| <20 | 9 (5.1%) | 7 (5.4%) | 2 (4.2%) | |
| 20–24 | 41 (23.2%) | 31 (24.0%) | 10 (20.8%) | |
| 25–29 | 60 (33.9%) | 42 (32.6%) | 18 (37.5%) | |
| 30–34 | 36 (20.3%) | 25 (19.4%) | 11 (22.9%) | |
| >35 | 31 (17.5%) | 24 (18.6%) | 7 (14.6%) | |
| BMI, mean (SD) | 28 (4) | 28 (4) | 30 (5) | .02b |
| Received antenatal care at Tenwek | 123 (69.5%) | 83 (64.3%) | 40 (83.3%) | .015a |
| Obstetric history | .067a | |||
| Primigravid | 42 (23.7%) | 26 (20.2%) | 16 (33.3%) | |
| Multiparous | 135 (76.3%) | 103 (79.8%) | 32 (66.7%) | |
| Maternal comorbidities | ||||
| Anemia | 56 (31.8%) | 44 (34.1%) | 12 (25.5%) | .38a |
| Chronic diabetes | 1 (0.6%) | 1 (0.8%) | 0 (0.0%) | .54a |
| Hypertensive disorders | 23 (13.0%) | 15 (11.6%) | 8 (16.7%) | .38a |
| Presence of any comorbidities | 92 (52.0%) | 72 (55.8%) | 20 (41.7%) | .094a |
| Estimated gestational age | .22a | |||
| >28–<34 wk | 17 (9.9%) | 15 (12.1%) | 2 (4.3%) | |
| >34–<35 wk | 10 (5.8%) | 9 (7.3%) | 1 (2.1%) | |
| >35–<37 wk | 42 (24.6%) | 30 (24.2%) | 12 (25.5%) | |
| >37 wk | 102 (59.6%) | 70 (56.5%) | 32 (68.1%) | |
| Noncephalic presentation of twin B | 101 (57.1%) | 59 (45.7%) | 42 (87.5%) | <.001a |
| Birth weight category | .124a | |||
| Either twin less than 2.5 kg | 119 (67.2%) | 91 (70.5%) | 28 (58.3%) | |
| Both twins greater than or equal to 2.5 kg | 58 (32.8%) | 38 (29.5%) | 20 (41.7%) | |
| Weight discordance >20% | 27 (15.3%) | 20 (15.6%) | 7 (14.6%) | .86a |
Pearson's chi-squared
Two-sample t test.
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
Table 2.
Indications for the planned mode of delivery
| Indication | All | Vaginal | CS |
|---|---|---|---|
| Twin A cephalic-twin B noncephalic | 96 (54.2%) | 69 (53.5%) | 27 (56.3%) |
| Both cephalic | 57 (32.2%) | 57 (44.2%) | 0 (0.0%) |
| Uterine scar | 8 (4.5%) | 0 (0.0%) | 8 (16.7%) |
| Uterine scar+noncephalic twin B | 5 (2.8%) | 0 (0.0%) | 5 (10.4%) |
| Maternal preference | 3 (1.7%) | 1 (0.8%) | 2 (4.2%) |
| Preeclampsia with severe features | 3 (1.7%) | 0 (0.0%) | 3 (6.2%) |
| Second stage labor | 2 (1.1%) | 2 (1.6%) | 0 (0.0%) |
| Preeclampsia+noncephalic twin B | 1 (0.6%) | 0 (0.0%) | 1 (2.1%) |
| Unknown HIV load | 1 (0.6%) | 0 (0.0%) | 1 (2.1%) |
| Hydrocephalus | 1 (0.6%) | 0 (0.0%) | 1 (2.1%) |
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
All 48 patients with a plan to deliver by CS were delivered as planned. Of the 129 patients who had a vaginal delivery planned, 26 patients had CS delivery of both twins or twin B.
The most common indication for change in plan prior to delivery of twin A was nonreassuring fetal heart tracing,8 and one instance each of cord prolapse, failed induction of labor, cord presentation, arrest of active labor, second stage arrest, failed trial of labor after uterine scar, prolonged rupture of membranes, and maternal request for change in plan.
Ten had combined delivery (vaginal delivery of twin A followed by CS for twin B). Three out of the ten, with combined delivery, had nonreassuring fetal heart tracing of twin B. In one set, neither twin experienced any component of the composite neonatal outcomes. One set had one neonate who weighed more than 20% less than the other twin and was admitted to the NICU for management of LBW and transient tachypnoea. The other set had both twins admitted to NICU for management of prematurity and LBW. Four of the ten had combined delivery because of the retained twin B. In one set, both twins were resuscitated, admitted to NICU, developed septic shock and DIC, and died. One set had one neonate being resuscitated, getting an APGAR score less than 7 in the 5th minute, getting admitted to NICU, and eventually dying. One set had both twins admitted to NICU for management of prematurity and LBW. The other set had no twin experiencing any component of the composite outcome. Two out of the ten had combined delivery cord prolapse of twin B. One set had one neonate resuscitated and admitted to NICU for seizure management. The other set had the twins admitted to NICU for prematurity and LBW and had birth weight discrepancy of more than 20%. One neonate experienced all of the individual components of composite neonatal outcomes except for birth trauma. One of the ten had combined delivery due to poor maternal effort without adverse outcomes.
The planned mode of delivery significantly impacted neonatal outcomes. Specifically, 51.2% (66/129) of the planned vaginal deliveries resulted in an adverse neonatal outcome, compared to only 29.2% (14/48) in the planned CS group (P=.009).
Table 3 details the individual components of the composite neonatal outcome. There were 19 total neonatal deaths (5.4%), 17 (6.6%) in the planned vaginal group, and 2 (2.1%) in the planned CS group (P=.08). Table 4 details the neonatal morbidities and deaths.
Table 3.
Neonatal outcomes according to planned mode of delivery
| Factor | Level | Value | Vaginal | CS | P valuea |
|---|---|---|---|---|---|
| 177 | 129 | 48 | |||
| APGAR score less than seven at 5 min | Not experienced | 170 (96.0%) | 123 (95.3%) | 47 (97.9%) | .084 |
| Experienced by one twin | 6 (3.4%) | 6 (4.7%) | 0 (0.0%) | ||
| Experienced by both twins | 1 (0.6%) | 0 (0.0%) | 1 (2.1%) | ||
| NICU admission | Not experienced | 102 (57.6%) | 67 (51.9%) | 35 (72.9%) | .041 |
| Experienced by one twin | 15 (8.5%) | 12 (9.3%) | 3 (6.2%) | ||
| Experienced by both twins | 60 (33.9%) | 50 (38.8%) | 10 (20.8%) | ||
| Resuscitation | Not experienced | 160 (90.4%) | 114 (88.4%) | 46 (95.8%) | .26 |
| Experienced by one twin | 13 (7.3%) | 12 (9.3%) | 1 (2.1%) | ||
| Experienced by both twins | 4 (2.3%) | 3 (2.3%) | 1 (2.1%) | ||
| Birth trauma | Not experienced | 177 (100.0%) | 129 (100.0%) | 48 (100.0%) | |
| Neonatal complications | Not experienced | 106 (59.9%) | 72 (55.8%) | 34 (70.8%) | .15 |
| Experienced by one twin | 19 (10.7%) | 14 (10.9%) | 5 (10.4%) | ||
| Experienced by both twins | 52 (29.4%) | 43 (33.3%) | 9 (18.8%) | ||
| Neonatal death before discharge | Not experienced | 163 (92.1%) | 116 (89.9%) | 47 (97.9%) | .17 |
| Experienced by one twin | 9 (5.1%) | 9 (7.0%) | 0 (0.0%) | ||
| Experienced by both twins | 5 (2.8%) | 4 (3.1%) | 1 (2.1%) | ||
| Composite outcome | Not experienced | 97 (54.8%) | 63 (48.8%) | 34 (70.8%) | .033 |
| Experienced by one twin | 17 (9.6%) | 14 (10.9%) | 3 (6.2%) | ||
| Experienced by both twins | 63 (35.6%) | 52 (40.3%) | 11 (22.9%) |
Pearsons’ chi-squared.
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
Table 4.
Morbidities and causes of death of twins that died
| Neonate | Planned mode of delivery | Gestational age | Birth weight (grams)a | Morbiditiesb | Causes of death |
|---|---|---|---|---|---|
| 1 | Vaginal | 29 wk 2 d | 1060, 1020 | PPROM, RDS | RDS |
| 2 | PPROM | … | |||
| 3 | Vaginal | 28 wk 2 d | 1190, 1125 | NNJ, RDS, HIE | RDS, HIE |
| 4 | HIE, RDS | RDS, HIE | |||
| 5 | Vaginal c | 30 wk 2 d | 1205, 1310 | NEC, PPROM, septic shock, DIC | Septic shock, DIC |
| 6 | PPROM, septic shock, DIC, | Septic shock, DIC | |||
| 7 | Cesarean section | 29 wk 5 d | 1005, 1200 | APH, PPROM | … |
| 8 | APH, PPROM | … | |||
| 9 | Vaginal | … | 805, 685 | … | … |
| 10 | … | … | |||
| 11 | Vaginald | 33 wk 5 d | 2120/2035 | … | … |
| 12 | Vaginal | 38 wk 4 d | 2675/2700 | HIE | HIE |
| 13 | Vaginald | 34 wk 3 d | 2000/1500 | Thrombocytopenia, birth asphyxia, PPROM, RDS | RDS |
| 14 | Vaginal | 31 wk 2 d | 1530/1425 | Gut perforation, neonatal infection | Neonatal infection |
| 15 | Vaginal | 30 wk 0 d | 1240/1295 | PPROM, shock, RDS | Shock, RDS |
| 16 | Vaginale | 39 wk 2 d | 1685/1860 | Fetal distress, fetal anomalyf, Aspiration pneumonitis | Aspiration pneumonitis |
| 17 | Vaginal | 35 wk 2 d | 2030/1770 | … | … |
| 18 | Vaginal | 29 wk 3 d | 920/830 | … | … |
| 19 | Vaginalc | 38 wk 5 d | 2440/2500 | HIE | HIE |
APH, antepartum hemorrhage; DIC, disseminated intravascular coagulation; HIE, hypoxic-ischemic encephalopathy; NEC, necrotizing enterocolitis; NNJ, neonatal jaundice; PPROM, preterm prolabor rupture of membranes; RDS, respiratory distress syndrome.
The birth weight is separated by comma (,) and cells merged where both twins died, and separated by slash (/) where only one twin died in a pair but could not confidently assign the respective birth weights
Diagnoses before and after delivery, excluding prematurity and low birth weight
Eventually had combined delivery because of retained second twin
Eventually had combined delivery because of cord prolapse
Eventually delivered both twins by cesarean section because of nonreassuring fetal heart rate tracing
The twin with fetal anomalies had umbilical and inguinal hernias and undescended testes.
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
Using logistic regression, controlling for ANC visits, the noncephalic presentation of twin B, and the birth weight category, revealed that the odds of experiencing any adverse outcome were lower in the planned CS group compared to the planned vaginal delivery group. The odds ratio was 0.35 (95% CI: 0.15–0.83; P=.017) for planned CS when compared to planned vaginal delivery, demonstrating a significant protective effect of planned CS against adverse neonatal outcomes (Table 5).
Table 5.
Logistic regression for neonatal outcomes to determine the impact of the planned mode of delivery
| Factor | Univariate odds ratio | 95% confidence interval | P value | Multivariable odds ratio | 95% confidence interval | P value |
|---|---|---|---|---|---|---|
| Planned mode of delivery | ||||||
| Vaginal | Reference | Reference | ||||
| CS | 0.39 | 0.19–0.80 | .01 | 0.35 | 0.15–0.83 | .017 |
| Antenatal care clinic visit | ||||||
| No | Reference | Reference | ||||
| Yes | 0.44 | 0.23–0.85 | .014 | 0.53 | 0.25–1.09 | .083 |
| Noncephalic presentation of twin B | ||||||
| No | Reference | Reference | ||||
| Yes | 1.25 | 0.68–2.27 | .474 | 1.92 | 0.93–3.98 | .08 |
| Birth weight category | ||||||
| Any twin<2500 grams | Reference | Reference | ||||
| Both twins≥2500 grams | 0.15 | 0.07–0.32 | <.001 | 0.15 | 0.07–0.33 | <.001 |
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
We found no significant difference in overall hospital costs between the two delivery modes (Table 6). The average total hospital costs for planned vaginal delivery were 104,608 KSh (SD 111,761) compared to 100,708 KSh (SD 75,468) for CS (P=.82).
Table 6.
Average costs of planned vaginal delivery compared to planned CS
| Planned delivery | Total costs average (SD) | Costs of delivery average (SD) | Neonatal costs average (SD) |
|---|---|---|---|
| Vaginal | 104,608 (111,761) | 45,304 (31,012) | 59,303 (98,233) |
| CS | 100,708 (75,468) | 76,229 (36,131) | 24,480 (51,208) |
| All | 103,551 (102,995) | 53,691 (35,187) | 49,860 (89,214) |
Omondi. Impact of planned delivery mode on neonatal outcomes and costs in twin pregnancies in Kenya. Am J Obstet Gynecol Glob Rep 2024.
On sensitivity analysis, when excluding patients who were planned for a vaginal delivery but eventually had a CS (N=26), CS was still associated with fewer adverse outcomes than vaginal delivery (29.2% compared to 47.6%; P=.033) and similar costs, respectively (100,708 vs 98,270; P=.90). Additionally, when excluding neonates below 1500 grams (N=11), planned CS remained associated with fewer adverse outcomes than planned vaginal delivery when controlling for noncephalic presentation, ANC visit, and birth weight category with an odds ratio of 0.40 (95% CI: 0.16–0.95; P=.037).
Comment
Principal findings
Our study of twins delivered at Tenwek Hospital revealed significantly better neonatal outcomes with a planned CS than with a planned vaginal delivery without substantial differences in hospital costs.
Results in the context of what is known
Similar to previous studies in other contexts,14,20 we observed a higher incidence of adverse neonatal outcomes associated with planned vaginal delivery. This finding aligns with research from resource-constrained settings,1,13,15 albeit differing from large multicenter trials like the twin birth study, which had more controlled environments and extensive resources. The twin birth study, however, had a small proportion of participants from sites with high neonatal mortality rates, which are primarily resource-constrained settings.
Regarding the neonatal outcomes, our findings correlate with the reported neonatal mortality rates for twins in resource-constrained settings. The observed 5.4% neonatal mortality rate in our study falls within the rates of 2.1% to 29% as found by other studies in similar settings.1,3,13,15,21,22 This correlation underscores the unique challenges and outcomes faced in resource-constrained environments. Similar to the study by Aisien et al.,13 the attendance of ANC clinics significantly impacted neonatal outcomes within our cohort, and should be highlighted as an area of quality improvement to increase ANC attendance.
Clinical implications
Our study suggests that in settings like Tenwek Hospital, where resources are limited, and the risk profile is unique with patients presenting without attending ANC clinics, a lack of continuous fetal monitoring throughout labor due to equipment shortage, and a higher perinatal mortality rate, CS might be a more favorable option for twin pregnancies with a leading cephalic twin. Hospitals in similar contexts could consider counseling patients to have a planned CS based on our findings.
Interestingly, our study did not identify a significant difference in the average total delivery and newborn care costs. The delivery costs were higher for CS; however, the costs of neonatal care were lower, due to the reduced complications, resulting in similar average total costs. This finding is particularly relevant as it contradicts the common perception that CSs are invariably more expensive than vaginal births. However, it is crucial to consider that the increased neonatal morbidity associated with vaginal deliveries raises postnatal care costs. Even if CS is recommended for twins based on evidence in resource-constrained settings, practitioners and patients may avoid this option due to the perception of it being more expensive than vaginal delivery. Our findings suggest that costs are similar. Thus, cost should not influence the decision.
Even though CS appears associated with improved neonatal outcomes, there is a maternal risk in future pregnancies of uterine rupture and Placenta Accreta Spectrum disorder, which should be factored into any discussion of the delivery plan.
Strengths and limitations
The strength of this study lies in its pragmatic focus on planned delivery mode and the novel inclusion of a cost analysis. However, the study's limitations, including its retrospective nature, single-center focus, and limited follow-up period, restrict the generalizability of our findings. Additionally, the plan of delivery based on admission decisions rather than ANC discussions may have impacted our results. The retrospective approach allowed for an investigation of our real-world experience; however, with limitations of record completeness and accuracy defining twin A and twin B, data collection should be performed prospectively. Even when excluding the unplanned CS from those planned to have a vaginal delivery, planned CS still had improved outcomes when compared to the group of planned and eventual vaginal delivery.
Research implications
These data would benefit from further study to determine causality, such as a large randomized prospective trial in similar settings. Future investigation into the experience level and training of the care providers involved could help provide clarity on potential contributors to the outcomes observed. Finally, with most patients lacking a first-trimester ultrasound scan, the limitations of estimated gestational age require further investigation to improve decision-making.
Conclusions
Our study suggests that planned CS for twin pregnancies with a leading cephalic twin is associated with fewer adverse neonatal outcomes compared to planned vaginal deliveries, without significant differences in hospital costs. This finding challenges the common perception that CS is invariably more expensive and suggests that cost should not be a deterrent in choosing the delivery mode in twin pregnancies in resource-constrained settings. While CS may offer better neonatal outcomes, it is crucial to consider the maternal risks in future pregnancies. The study's limitations highlight the need for further research, including prospective trials, to validate these findings and explore the impact of healthcare provider experience and training on outcomes. Our findings contribute to the ongoing debate about the optimal mode of delivery in twin pregnancies, particularly in resource-constrained environments, and suggest that CS may be a favorable option in such settings.
CRediT authorship contribution statement
Fred O. Omondi: Writing – review & editing, Writing – original draft, Visualization, Validation, Project administration, Methodology, Investigation, Data curation, Conceptualization. Meghan K. Murphy: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Conceptualization. Moselle M. Stark: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Conceptualization. Cheryl B. Cowles: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Conceptualization. Phillip C. Greig: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Conceptualization. Benoît J. Ndikumana: Writing – review & editing, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Conceptualization. Robert K. Parker: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Acknowledgments
Acknowledgments
We want to acknowledge the Medical Records and Finance Departments at Tenwek Hospital and, specifically, Fiona Chelangat for their help with data collection. Fiona Chelangat is a billing clerk employed by Tenwek Hospital.
Footnotes
Conflicts of interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this article.
Patient Consent Statement: Not required because no personal information or details are included.
Funding: None.
Tweetable Statement: At Tenwek Hospital, Kenya, planned cesarean sections for twin pregnancies with a leading cephalic twin have fewer adverse neonatal outcomes than planned vaginal deliveries, without significant cost differences.
References
- 1.Bellizzi S, Sobel H, Betran A, Temmerman M. Early neonatal mortality in twin pregnancy: findings from 60 low- and middle-income countries. J Glob Health. 2018;8 doi: 10.7189/jogh.08.010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarthy BJ, Sachs BP, Layde PM, et al. The epidemiology of neonatal death in twins. Am J Obstet Gynecol. 1981;141(3):252–256. doi: 10.1016/s0002-9378(16)32628-x. [DOI] [PubMed] [Google Scholar]
- 3.Miyahara R, Jasseh M, Mackenzie GA, et al. The large contribution of twins to neonatal and post-neonatal mortality in The Gambia, a 5-year prospective study. BMC Pediatr. 2016;16(1):39. doi: 10.1186/s12887-016-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Multifetal gestations: twin, triplet, and higher-order multifetal pregnancies: ACOG practice bulletin, number 231. Obstet Gynecol. 2021;137(6):e145. doi: 10.1097/AOG.0000000000004397. [DOI] [PubMed] [Google Scholar]
- 5.Santana DS, Silveira C, Costa ML, et al. Perinatal outcomes in twin pregnancies complicated by maternal morbidity: evidence from the WHO Multicountry Survey on Maternal and Newborn Health. BMC Pregnancy Childbirth. 2018;18(1):449. doi: 10.1186/s12884-018-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vogel JP, Torloni MR, Seuc A, et al. Maternal and perinatal outcomes of twin pregnancy in 23 low- and middle-income countries. PLoS One. 2013;8(8):e70549. doi: 10.1371/journal.pone.0070549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barrett JFR, Hannah ME, Hutton EK, et al. A randomized trial of planned cesarean or vaginal delivery for twin pregnancy. N Engl J Med. 2013;369(14):1295–1305. doi: 10.1056/NEJMoa1214939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen J, Shen H, Chen YT, Chen CH, Lee KH, Torng PL. Experience in different modes of delivery in twin pregnancy. PLoS One. 2022;17(3) doi: 10.1371/journal.pone.0265180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hofmeyr GJ, Barrett JF, Crowther CA. Planned caesarean section for women with a twin pregnancy. Cochrane Database Syst Rev. 2015;2015(12) doi: 10.1002/14651858.CD006553.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee HC, Blumenfeld YJ. Caesarean delivery for twin gestation at 32–38 weeks does not lead to improved clinical outcomes for neonates or mothers. BMJ Evid-Based Med. 2014;19(3):119. doi: 10.1136/eb-2013-101655. [DOI] [PubMed] [Google Scholar]
- 11.Mei-Dan E, Dougan C, Melamed N, et al. Planned cesarean or vaginal delivery for women in spontaneous labor with a twin pregnancy: a secondary analysis of the Twin Birth Study. Birth Berkeley Calif. 2019;46(1):193–200. doi: 10.1111/birt.12387. [DOI] [PubMed] [Google Scholar]
- 12.Schmitz T, Carnavalet C de C, Azria E, Lopez E, Cabrol D, Goffinet F. Neonatal outcomes of twin pregnancy according to the planned mode of delivery. Obstet Gynecol. 2008;111(3):695. doi: 10.1097/AOG.0b013e318163c435. [DOI] [PubMed] [Google Scholar]
- 13.Aisien AO, Olarewaju RS, Imade GE. Twins in Jos Nigeria: a seven-year retrospective study. Med Sci Monit. 2000;6:945–950. [PubMed] [Google Scholar]
- 14.Hartley RS, Hitti J. Please exit safely: maternal and twin pair neonatal outcomes according to delivery mode when twin A is vertex*. J Matern Fetal Neonatal Med. 2017;30(1):54–59. doi: 10.3109/14767058.2016.1161748. [DOI] [PubMed] [Google Scholar]
- 15.Nwankwo TO, Aniebue UU, Ezenkwele E, Nwafor MI. Pregnancy outcome and factors affecting vaginal delivery of twins at University of Nigeria Teaching Hospital, Enugu. Niger J Clin Pract. 2013;16:490–495. doi: 10.4103/1119-3077.116895. https://www.ajol.info/index.php/njcp/article/view/94242 [DOI] [PubMed] [Google Scholar]
- 16.Chimenea A, García-Díaz L, Antiñolo G. Mode of delivery, perinatal outcome and neurodevelopment in uncomplicated monochorionic diamniotic twins: a single-center retrospective cohort study. BMC Pregnancy Childbirth. 2022;22(1):89. doi: 10.1186/s12884-022-04425-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmitz T, Prunet C, Azria E, et al. Association between planned cesarean delivery and neonatal mortality and morbidity in twin pregnancies. Obstet Gynecol. 2017;129(6):986–995. doi: 10.1097/AOG.0000000000002048. [DOI] [PubMed] [Google Scholar]
- 18.Schmitz T, Goffinet F. [Delivery of twins: lessons learnt from the national observational prospective comparative study JUMODA] Gynecol Obstet Fertil Senol. 2024;52:410–417. doi: 10.1016/j.gofs.2023.11.005. S2468-7189(23)00230-1. [DOI] [PubMed] [Google Scholar]
- 19.Parker RK, Otoki K, Many HR, Parker AS, Shrime MG. The costs of complications after emergency gastrointestinal surgery in Kenya. Surgery. 2022;172(5):1401–1406. doi: 10.1016/j.surg.2022.08.006. [DOI] [PubMed] [Google Scholar]
- 20.Dong Y, Luo ZC, Yang ZJ, et al. Is cesarean delivery preferable in twin pregnancies at >=36 weeks gestation? PLoS One. 2016;11(5) doi: 10.1371/journal.pone.0155692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abasiattai AM, Umoiyoho AJ, Utuk NM, Shittu DG. Incidence and mode of delivery of twin pregnancies in Uyo, Nigeria. Niger Med J. 2010;51(4):170–172. [Google Scholar]
- 22.KNBS and ICF. 2023. Kenya Demographic and Health Survey 2022. Nairobi, Kenya, and Rockville, Maryland, USA: KNBS and ICF.