To the editor:
Eating disorder (ED), as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), is a persistent disturbance of eating or eating-related behaviour that results in the altered consumption or absorption of food and that significantly impairs physical health or psychosocial functioning.1 The DSM-5 outlines criteria for EDs, including anorexia nervosa, bulimia nervosa, binge-eating disorder, pica, rumination disorder and avoidant/restrictive food intake disorder. EDs are relatively common in young people, affecting 5.5%–17.9% of young women and 0.6%–2.4% of young men by the time they reach early adulthood.2 EDs are more prevalent in females, with recent increases in prevalence reported primarily in females 15–19 years of age.2 People with EDs face a mortality risk twice that of the general population2 and, without treatment, have higher rates of medical and psychiatric comorbidity.3
Since the start of the coronavirus disease 2019 (COVID-19) pandemic, concerns have been raised about increasing rates of ED diagnoses, and ED-related hospitalisation, outpatient care-seeking, depression, anxiety and suicidal ideation.4 In February 2023, the American Psychiatric Association released updated guidelines for EDs with implementation tools that include screening questionnaires to assist in detection.5 The US Surgeon General also underscored the need for real-time data to address the evolving mental health needs in adolescents and young adults, particularly with regard to EDs. Against this backdrop, population-level administrative data on the prevalence of EDs are needed to inform a robust public health response. Our study aimed to evaluate the estimated prevalence of ED diagnoses from 2017 to 2022 and the demographic profile of people with EDs using a large multicountry collection of electronic medical records.
Data source and collection
We used the 2017–2022 TriNetX data, a federated multinational research network that captures de-identified, real-time electronic medical records. This dataset included diagnoses, procedures and treatments, medications and laboratory data, sourced from over 110 million patients across over 80 healthcare organisations in multiple nations (>80% US-based). The TriNetX databases adhere to the Health Insurance Portability and Accountability Act and are certified by the International Organization for Standardization and the International Electrotechnical Commission, maintaining an Information Security Management System to ensure the protection of healthcare data. Detailed methods on the TriNetX databases have been previously described.6
Our population of interest was children, adolescents and young adults with healthcare enrolment in the TriNetX databases. We defined the ED cohort as individuals between the ages of 5 and 26 years spanning from 1 January 2017 through 31 December 2022, which encompassed the pre-COVID-19 and post-COVID-19 time periods. The presented data were queried on 28 May 2023. As shown in online supplemental figure 1, we excluded people outside the 5–26 years age range.
Our primary outcome was the estimated prevalence of ED diagnoses, requiring people to have at least one ED diagnosis (International Statistical Classification of Diseases Clinical Modification, International Classification of Diseases, 10th Revision, Clinical Modification, F50; identified via inpatient or outpatient encounters, encapsulating any DSM-5 ED). Among people meeting the inclusion criteria, we extracted covariates such as age of diagnosis and sex (male vs female, as per TriNetX data availability).
We first conducted descriptive and univariate analyses using Health Insurance Portability and Accountability Act-compliant built-in analytical tools in the TriNetX data; Fisher’s exact tests or χ2 tests were applied for categorical variables, while analyses of variance were employed for continuous variables. We compared baseline characteristics including sex and age at the time of ED diagnosis between people with and without at least one ED diagnosis. We considered statistical significance to be indicated by a two-tailed p<0.05.
To investigate age trends in estimated ED prevalence by calendar year (2017–2022) and their association with sex, logistic regression models were estimated using STATA V.17 (College Station, Texas, USA) with secure, de-identified data retrieved from the TriNetX network. We explored potential differential time trends in ED diagnosis between sex and age at the ‘index’ event (first ED diagnosis within the time frame), through two-way interactions of the sex and age in binary logistic regression. We categorised age into three subgroups: pre-adolescent (5–12 years), adolescent (13–18 years) and transitional age (19–26 years). Age groups were stratified with respect to puberty because previous studies have established associations between pubertal development and ED in females7; age 12–13 years was used as the youngest cut-off for definitive entry into puberty due to expected physiological changes associated with puberty normally beginning by age 12 years in female individuals and by age 13 years in male individuals.7
A total of 46 388 498 patients between the ages of 5 and 26 years were included in this study (mean age=15.4 years; standard error (SE)=0.001), with 48.1% males and 51.9% females. We identified 117 213 individuals with EDs. The overall estimated prevalence of EDs was 250/100 000, with a higher estimated prevalence of EDs among females compared with males (370/100 000 and 130/100 000, respectively, p<0.001). The mean age at first diagnosis of an ED was 17.57 years (SE=0.02).
The mean age of diagnosis for EDs was 18.66 years (SE=0.05) in 2017, compared with 17.01 years (SE=0.03) in 2022 (p<0.001). The mean age of diagnosis was higher for females than for males (mean (age): 18.71 vs 14.08, p<0.001) (online supplemental table 1).
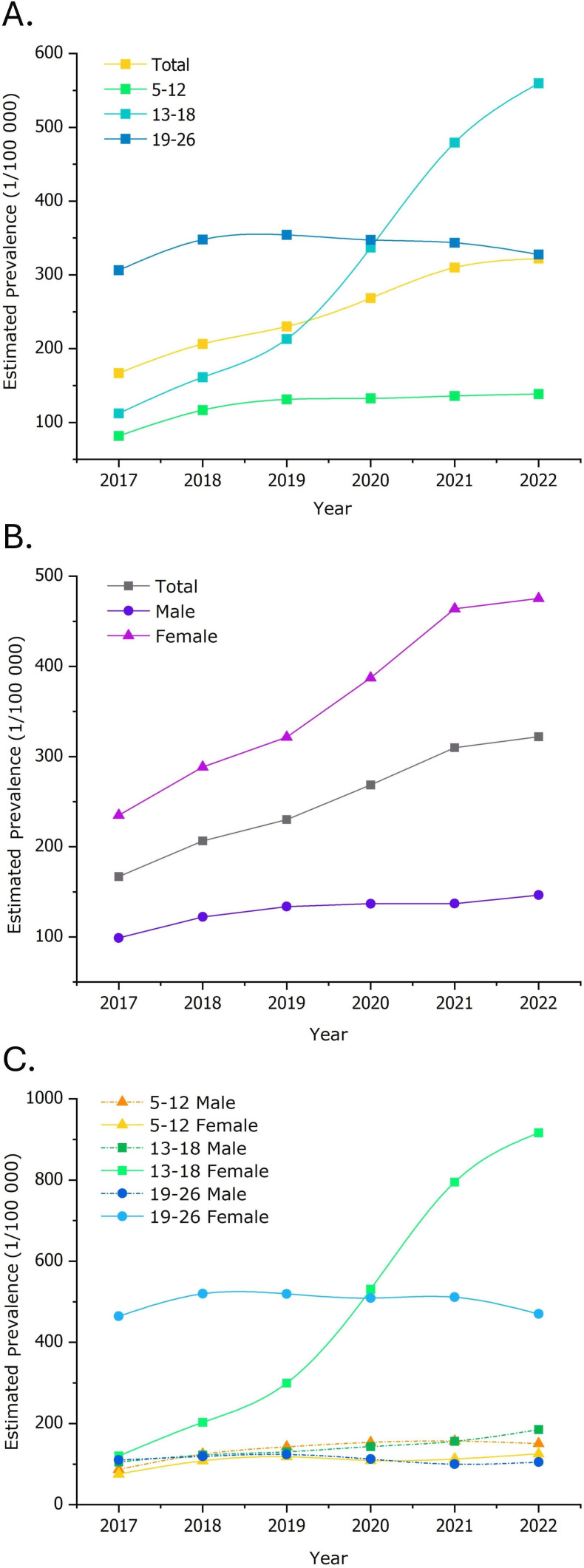
In univariate analyses, we compared the differences in prevalence of EDs between 2017 and 2022. The prevalence of EDs was 167/100 000 in 2017, compared with 322/100 000 in 2022 (p<0.001). In the female cohort, the prevalence of EDs was 235/100 000 in 2017, compared with 475/100 000 in 2022; in the male cohort, the prevalence of EDs was 99/100 000 in 2017, compared with 146/100 000 in 2022 (figure 1). For the 13–18 years age group, the ED prevalence was 112/100 000 in 2017, compared with 560/100 000 in 2022. In the 5–12 years age group, the ED prevalence was 81/100 000 in 2017, compared with 139/100 000 in 2022. In the transitional age group (19–26 years old), the ED prevalence remained relatively stable, at 306/100 000 in 2017 and 328/100 000 in 2022 (figure 1).
Figure 1. Prevalence of eating disorders (A) by age group, (B) by sex and (C) by age×sex.
Across all years, the overall prevalence of ED was 123/100 000, 321/100 000 and 338/100 000 among pre-adolescent, adolescent and transitional age groups, respectively. In the cohort 5–12 years old (pre-adolescent), we observed a slightly higher prevalence of EDs in males compared with females (135/100 000 vs 108/100 000, respectively). Binary logistic regression models showed that males in the age group of 5–12 years were more likely to be diagnosed with EDs compared with their female peers (OR=1.25; 95% CI 1.21 to 1.28, Z=16.03, p<0.001; F(6,17480374)=852.16; p<0.001). However, during puberty (13–18 years) and after puberty (age 19–26 years), the prevalence of diagnosed EDs was higher in females compared with their male counterparts (p<0.001; figure 1).
Among people aged 13–18 years, females were more likely to be diagnosed with EDs compared with their male peers (OR=3.58; 95%CI 3.49 to 3.67, Z=101.76, p<0.001; F(6,11949412)=23 214.23; p<0.001 for overall model). Similarly, females in the age group of 19–26 years were more likely to be diagnosed with EDs compared with their male peers (OR=1.25; 95% CI 4.40 to 4.61, Z=123.68, p<0.001; F(6,169586994)=21 342.70; p<0.001 for overall model).
Finally, we observed an increase in the prevalence of diagnosed EDs among females aged 13–18 years, raising from 120/100 000 in 2017 to 916/100 000 in 2022 (figure 1).
We found an increasing estimated prevalence of EDs in young people between 2017 and 2022, particularly among female adolescents, in a real-time population-level dataset. To our knowledge, this is among the first studies to describe the real-world estimated prevalence of EDs before and after the COVID-19 pandemic, a period during which ED diagnoses, symptoms, hospitalisation and related complications have increased.4 Our study also builds on existing knowledge that EDs are more prevalent in females.2 8
When further stratified by developmental stage, the prevalence of ED was higher among females in the pubertal (age 13–18 years) and post-pubertal (age 19–26 years) stages, whereas the prevalence of ED was higher among males in the pre-pubertal subgroup (age 5–12 years). Although the mechanism behind the sex and age differences was not fully understood, previous studies have suggested that sex differences in ED prevalence may not appear until puberty,9 and data from community settings have suggested that ED prevalence may be rising faster among males.10 Further, rates of ED diagnosis by subtype vary by age8; for example, patients with avoidant/restrictive food intake disorder tend to be younger10 and are more likely to be identified in males.11 Thus, the higher prevalence of ED in pre-pubertal males observed in our study may support this finding. Considering that our dataset includes the period of massive sociocultural changes during the COVID-19 pandemic, these data may represent the evolving estimated prevalence of EDs, informing calls for heightened clinician, educator and parent awareness of counterstereotypical presentations of EDs.10
We found a substantial increase in the estimated prevalence of EDs among females 13–18 years old from 2017 to 2022, along with younger average ages at diagnosis. Notably, the higher mean age of ED diagnoses among females, compared with their male peers, contradicts past studies suggesting that age of onset does not vary significantly by sex.12 This shift in ED demographics necessitates heightened vigilance from clinicians, educators and parents in detecting potential ED-related behaviours at younger ages. Early detection and intervention are crucial for successful ED prevention and treatment, as studies show that a shorter duration of illness predicts better outcomes.12 Preliminary screening tools for adolescent depression have been introduced starting at the age of 12 years, as per the Guidelines for Adolescent Depression in Primary Care by American Academy of Pediatrics.13 However, the risk factors for EDs are complex and multifactorial, including biological, psychosocial and environmental factors such as adverse childhood events, social pressures and personality traits related to rigidity and perfectionism, which complicate epidemiological and clinical studies.14 While EDs are more common among people with pre-existing mental health problems, they can also bidirectionally contribute to disturbances in cognitive and emotional functioning and psychiatric conditions, further complicating diagnosis and treatment. While recent US Preventive Services Task Force guidance illustrates an ongoing lack of consensus on ED screening guidelines,15 the real-time long-term epidemiological data in this study represent an important first step to improving our population-level surveillance of EDs.
Despite enhancing our understanding of ED diagnosis among young people, this study has several limitations. First, TriNetX data only include those people who seek medical care within certain healthcare organisations in the network. Therefore, the diagnostic data in TriNetX represent only a portion of the actual population prevalence of EDs, specifically those ill enough or who have sufficient access to healthcare to receive a diagnosis. Second, while the TriNetX data have a diverse representation of race, ethnicity, age, income and insurance types, due to strict patient privacy protections, we are not permitted to refine the cohort to specific healthcare organisations, regions or countries (recognising that >80% of the data stem from the USA). Third, TriNetX extracts data based on ‘sex’, which does not necessarily mean sex assigned at birth, nor does it necessarily capture gender identity, so we could not meaningfully reflect potential gender diversity. Finally, this observational analysis is intended to be descriptive rather than prescriptive; the reasons for the increasing estimated prevalence of any diagnosed ED within our study population between 2017 and 2022 are not well understood, and future qualitative and quantitative research is needed.
Our findings of the increasing estimated prevalence of EDs, notably the impact on pre-pubescent males and adolescent females, between 2017 and 2022, warrant the primary prevention and potential early intervention in children and adolescents. The findings also highlight the valuable role of quality real-time data for monitoring and informing the healthcare system effectively.
supplementary material
Acknowledgements
The authors thank Patricia Cavazos-Rehg and Laura Bierut of the NIDA K12 Program of Washington University for obtaining funding to support effort for personnel (KYX); Ginger Nicol from Washington University School of Medicine for providing professional viewpoints; and Mattie Tenzer from HART Carilion for technical support.
Biography
Binx Yezhe Lin graduated from Shanghai Jiao Tong University School of Medicine, Shanghai in 2017 with degrees of master’s in science and bachelor’s in clinical medicine (MD equivalent). She has worked as a psychiatry resident at Virginia Tech Carilion School of Medicine in the USA since 2021 and will join the University of California, San Francisco (UCSF) as a Child and Adolescent Psychiatry Fellow (public track) in 2024. She is working at the outpatient children, adult, and geriatric clinics providing mental health care. Her work also includes community free clinic and outreach for underserved populations, such as LGBTQ+, immigrants, and low socioeconomic status populations. She has been selected as a public psychiatry fellow by the APA/APA Foundation for 2023-2025. Her current research focuses on public mental health and intersectionality for LGBTQ+ and children, adolescents, and young adults, by utilizing big data and real-world data in multiple historically underserved populations and overlooked disorders (eg, eating disorders, conduct disorders, PNES, etc).

The contents of this publication are solely the responsibility of the author and do not necessarily represent the official views of the APA or APAF. Mention of trade names, commercial practices or organisations does not imply endorsement by the US Government.
Footnotes
Funding: Effort for some personnel was supported by grants K12 DA041449 (KYX, PI: Laura Bierut, Patricia Cavazos-Rehg), and the American Psychiatric Association Psychiatric Research Fellowship (KYX). Authors BYL and C-FS were American Psychiatric Association (APA)/APA Foundation (APAF) fellows at the time of publication. Research grant funding received from Gilead Pharmaceuticals, Liva Nova Therapeutics, Curemark and Alto Neuroscience (ASK).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: The study was determined by the Carilion Clinic Institutional Review Board as non-human subject research.
Contributor Information
Binx Yezhe Lin, Email: yezhe.lin@foxmail.com.
Dominic Moog, Email: d.moog@wustl.edu.
Hui Xie, Email: sphinx.hui@gmail.com.
Ching-Fang Sun, Email: chingfangsun@gmail.com.
Wisteria Yushan Deng, Email: wisteria.deng@yale.edu.
Erin McDaid, Email: erinmcdaid@vt.edu.
Katherine V Liebesny, Email: kvliebesny@carilionclinic.org.
Anita S Kablinger, Email: ASKablinger@carilionclinic.org.
Kevin Young Xu, Email: xukeviny@wustl.edu.
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders, 5th edition: DSM-5. BRAND NEW American Psychiatric Publishing; 2017. [Google Scholar]
- 2.Silén Y, Keski-Rahkonen A. Worldwide prevalence of DSM-5 eating disorders among young people. Curr Opin Psychiatry. 2022;35:362–71. doi: 10.1097/YCO.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 3.Swanson SA, Crow SJ, Le Grange D, et al. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–23. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.J Devoe D, Han A, Anderson A, et al. The impact of the COVID-19 pandemic on eating disorders: a systematic review. Int J Eat Disord. 2023;56:5–25. doi: 10.1002/eat.23704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crone C, Fochtmann LJ, Attia E, et al. The American psychiatric association practice guideline for the treatment of patients with eating disorders. Am J Psychiatry. 2023;180:167–71. doi: 10.1176/appi.ajp.23180001. [DOI] [PubMed] [Google Scholar]
- 6.Sun C-F, Xie H, Metsutnan V, et al. The mean age of gender dysphoria diagnosis is decreasing. Gen Psychiatr. 2023;36:e100972. doi: 10.1136/gpsych-2022-100972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jonsdottir-Lewis E, Feld A, Ciarlo R, et al. Timing of pubertal onset in girls and boys with constitutional delay. J Clin Endocrinol Metab. 2021;106:e3693–703. doi: 10.1210/clinem/dgab270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Culbert KM, Sisk CL, Klump KL. A narrative review of sex differences in eating disorders: is there a biological basis? Clin Ther. 2021;43:95–111. doi: 10.1016/j.clinthera.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanzari CM, Levin RY, Liu RT. Prevalence, predictors, and treatment of eating disorders in children: a national study. Psychol Med. 2023;53:2974–81. doi: 10.1017/S0033291721004992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchison D, Mond JM. Epidemiology of eating disorders, eating disordered behaviour, and body image disturbance in males: a narrative review. J Eat Disord. 2015;3:20. doi: 10.1186/s40337-015-0058-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorrell S, Murray SB. Eating disorders in males. Child Adolesc Psychiatr Clin N Am. 2019;28:641–51. doi: 10.1016/j.chc.2019.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vall E, Wade TD. Predictors of treatment outcome in individuals with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. 2016;49:432–3. doi: 10.1002/eat.22518. [DOI] [PubMed] [Google Scholar]
- 13.Zuckerbrot RA, Cheung A, Jensen PS, et al. Guidelines for adolescent depression in primary care (GLAD-PC): part I practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141:e20174081. doi: 10.1542/peds.2017-4081. [DOI] [PubMed] [Google Scholar]
- 14.Bould H, Newbegin C, Stewart A, et al. Eating disorders in children and young people. BMJ. 2017;359:j5245. doi: 10.1136/bmj.j5245. [DOI] [PubMed] [Google Scholar]
- 15.US Preventive Services Task Force Screening for eating disorders in adolescents and adults: US preventive services task force recommendation statement. JAMA. 2022;327:1061–7. doi: 10.1001/jama.2022.1806. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.