Abstract
Background
Post-donation regret in family living liver donors can impact their mental well-being. This study examined whether the relationship between post-donation regret and anxiety is mediated by family relationships and a sense of mastery.
Material/Methods
We conducted a secondary analysis of de-identified cross-sectional data from a prior study that included 124 living liver donors. These donors underwent partial hepatectomy between January 2011 and March 2021 at a tertiary hospital in Seoul, South Korea. The data included demographic and clinical characteristics, along with the results from administering the following measures: the Post-Donation Regret Scale, Family Relationships Index, Pearlin Mastery Scale, and the Generalized Anxiety Disorder-2 scale.
Results
Among family living liver donors, 5.6% had anxiety after donation. The total effect of post-donation regret on anxiety was significant (B=0.41, p<0.05). However, the direct effect of regret on anxiety was not significant (B=−0.05, p=0.733). Post-donation regret had indirect effects on anxiety, solely through family relationships (B=0.329, 95% CI=0.130, 0.563) and sequentially through family relationships and mastery (B=0.088, 95% CI=0.008, 0.232), even after controlling for sex, age, postoperative complications, years since donation, and recipient’s death. In addition, postoperative complication was a predictor of anxiety (B=0.64, p<0.05).
Conclusions
Providing family-centered and mastery-enhancing interventions may help alleviate the anxiety of family living liver donors.
Keywords: Anxiety, Emotions, Family Relations, Liver Transplantation, Living Donors
Introduction
Liver transplants are the second most frequently performed solid organ transplantation [1]. Over the past decade, living donor liver transplants (LDLTs) have become increasingly popular, especially in Asia, with South Korea emerging as the leading country in terms of LDLT activity [2]. A total of 1158 LDLTs were performed in South Korea in 2021, representing 76% of all liver transplants [3]. Characteristically, more than 90% of donor–recipient relationships of LDLTs in Asia, including South Korea, were within a second degree of familial relation [3–5].
Liver living donors (LLDs) reported moderate anxiety during the postoperative phase, with no discernible decline in anxiety levels over time [6]. Prevailing research indicates a higher prevalence of postoperative anxiety compared to postoperative depression among organ donors [7,8]. Qualitative investigations have shed light on the LLDs’ postoperative psychosocial experiences, emphasizing the importance of valuing the donation decision as pivotal for effective adjustment after donation [9,10]. Additionally, quantitative studies have highlighted the impact of negative emotions such as regret on the mental quality of life of LLDs, with post-donation regret correlating with anxiety [11,12].
Family donors have acknowledged their vulnerability to ongoing uncertainties after donation, endeavoring to reaffirm the significance of their donation, restore normalcy to familial routines, and maintain control over their well-being [13]. The adjustment of the donor has been shown to exert a substantial influence on the overall familial well-being, with strained relationships with the recipient exacerbating anxiety among LLDs [13,14]. Nevertheless, despite familial relationships being central to the majority of donation cases, their assessment and impact within the transplant process have remained relatively underexplored [15]. Moreover, many family LLDs embark on the donation process willingly, perceiving it as a means to contribute to the recipient’s and their own family’s future well-being [16]. Such donors may approach the donation process with a sense of mastery, believing in their ability to shape the trajectory of their lives. Conversely, individuals who experience coercion or exhibit hesitation until the eve of surgery tend to manifest greater anxiety regarding their future after donation [13]. Therefore, there exists a need to explore the roles of family relationships and the sense of mastery in understanding the association between post-donation regret and anxiety.
The stress process model (SPM) posits that individuals’ resources serve as crucial mediators between stressors and mental health outcomes, delineating the process through which stressors manifest into psychological distress [17]. The SPM framework, previously applied to elucidate the psychological dynamics of caregivers and general adult populations [18,19], holds relevance for understanding the experiences of family organ donors. Given their comparable health status and the caregiving strain experienced by donors in supporting recipients [20,21], the SPM framework can be effectively utilized to identify stressors and resources influencing post-donation anxiety symptoms among family LLDs. According to this theory, primary stressors include subjective indicators (eg, negative reaction to an event), which predict mental health outcomes (eg, anxiety). In these relationships, role strains (eg, family conflicts) and personal resources (eg, mastery, self-esteem) can mediate stressors’ effects on mental health [22].
The literature shows that negative perceptions and reactions to caregiving predicted family caregivers’ distress, which was mediated by poor family relationships [23]; anxiety in caregivers was found to be inversely correlated with mastery [24]. In general adult populations, regret influences anxious arousal [25], people with problematic family relationships and family functioning were likely to have high anxiety [26,27], greater mastery can decrease levels of anxiety symptoms [28,29], and family functioning satisfaction and sense of mastery show a positive relationship [30]. Therefore, the relationships between these 4 variables can be extended to family organ donors. Identifying roles in post-donation regret, family relationships, and mastery could be helpful in designing effective management strategies for post-donation anxiety. Therefore, for family LLDs, it is worth exploring how the resources may buffer the effect of post-donation regret on anxiety. Consequently, we propose the following hypotheses:
H1: Post-donation regret is positively associated with anxiety.
H2: The association between post-donation regret and anxiety is mediated by family relationships.
H3: The association between post-donation regret and anxiety is mediated by mastery.
H4: Family relationships and mastery sequentially mediate the association between post-donation regret and anxiety.
Material and Methods
Study Design
This cross-sectional study utilized secondary data collected from a project aimed at identifying the well-being and health adaptation of LLDs after donation [11].
Data Source and Participants
The dataset utilized in this study comprised survey responses pertaining to post-donation regret, family relationships, mastery, and anxiety, along with a review of medical records. Medical records of the participants who responded to the survey were obtained, including length of hospital stay, postoperative complications, years since donation, and recipient death. Data collection of survey and medical record occurred between February and July 2021 at the transplant center of the Seoul National University Hospital (SNUH), in South Korea. The accessible population consisted of 535 LLDs who underwent partial hepatectomy at this transplant center within the preceding decade (from January 2011 to March 2021). Out of the 535 potential participants, 124 donors participated in the original study. The sample of the dataset comprised a total of 124 LLDs who were 19 years or older, within the second degree of familial relations with the recipients (donors were the recipients’ child, spouse, sibling, or parent), and were at least 1 month after donation [11]. For the analysis of the mediation effect, 120 LLDs were included in the mediation model after accounting for missing data.
A post hoc power analysis for linear multiple regression was performed utilizing the G*Power 3.1.9.4. With an alpha level of 0.05, a medium effect size of 0.15, 8 predictors (including post-donation regret, family relationships, mastery, and 5 covariates), and a total sample size of 120, the calculated post hoc power (1−β) was 85.1%. Moreover, considering the recommendation that the sample size for path analysis should be 15 times the number of variables [31], the sample size of this study was deemed acceptable.
Instruments
Post-Donation Regret
Post-donation regret was evaluated by a one-item questionnaire, “If you could go back to before your donation, would you still donate?” LLDs could answer based on their prevailing thoughts and sentiments from the immediate postoperative period to the time of the survey. The questionnaire employed a 4-point Likert scale, ranging from 1 (very likely), to 4 (definitely not). A higher score represents greater regret. The questionnaire was developed after a literature review [12,32], and its face validity was reviewed by 5 LLDs and 5 liver transplant professionals. They qualitatively assessed its readability, suitability, and clarity.
Family Relationships
The Family Relationships Index (FRI) [33] was utilized to evaluate the quality of familial relationships. Employing a Korean adaptation of the FRI [34], this instrument gauged LLDs’ usual perceptions of internal family dynamics, including those involving the recipient. Designed primarily for conjugal and nuclear family units, the FRI assesses familial adjustments to life transitions and crises [33]. The instrument comprises cohesion and expression-conflict subscales, consisting of a total of 20 items rated on a 5-point Likert scale (ranging from 1=“not at all true” to 5=“very true”). The cohesion subscale assesses levels of support, dedication, assistance, and open communication among family members while the expression-conflict subscale assesses the degree to which family members express anger and disagreement [34]. Total scores on the FRI range from 20 to 100. Higher scores indicate that a family has greater cohesion and expressiveness, as well as lower conflict, which reflects a supportive family environment [33]. The Korean adaptation of the FRI was validated and proved to be reliable, with Cronbach’s α values ranging between 0.74 and 0.77 [34]. In this study, the Korean version of the FRI showed an excellent Cronbach’s α coefficient of 0.93.
Mastery
The Pearlin Mastery Scale (PMS) [35,36] was used to assess LLDs’ sense of mastery, reflecting their usual belief in the degree of control they exert over their life circumstances, as opposed to viewing life events fatalistically. It comprised 7 items rated on a 4-point scale: 1 (strongly disagree) to 4 (strongly agree). The total score could vary from 7 to 28, with higher values suggesting stronger mastery. The Korean version of the PMS proved to be reliable, with a Cronbach’s α value of 0.75 [36]. A Cronbach’s α in this study was 0.83.
Anxiety
Anxiety symptoms were evaluated using the Generalized Anxiety Disorder-2 (GAD-2) [37], a brief two-item measure. This instrument assesses the presence of anxiety symptoms experienced over the preceding 2 weeks. Further details and access to the GAD-2 screener are available at https://www.phqscreeners.com/select-screener. Every response is rated on a 4-point Likert scale (0=“not at all” to 3=“nearly every day”), with total scores between 0 and 6. An increased level of anxiety symptoms is indicated by a higher overall score. A total score of 3 or greater was considered positive for anxiety screening. It has already been established that the GAD-2 has suitable validity and reliability in the Korean population [38]. The Cronbach’s α in this study was 0.84.
Demographic and Clinical Information
Demographic information about LLDs was obtained, including data on sex (1=female/0=male), age (continuous), relationship to the recipient (1=child/0=spouse, sibling, parent), and marital status (1=married/0=else). Clinical information was obtained, including length of hospital stay (continuous), postoperative complications (1=Grade II–III in Clavien-Dindo classification/0=no complication or Grade I in Clavien-Dindo classification), years since donation (continuous), and recipient death (1=death/0=alive). According to Clavien-Dindo classification, Grade I complications are considered natural sequelae after surgery not requiring any intervention; Grade II or III complications need medication or medical intervention [39].
Ethical Consideration
The current study was approved by the Institutional Review Board (IRB) of SNUH; since this study used secondary data, informed consent from the participants was waived by the IRB of SNUH (approval no.: 2210-085-1368). Data without identifiers were used for data analysis.
Data Analysis
Descriptive analyses were performed to determine sample characteristics. The normality of the study variables (post-donation regret, family relationships, mastery, and anxiety) was examined using the Shapiro-Wilk test, suggesting that these continuous variables were not normally distributed. Hence, Spearman’s rho correlation coefficient, a nonparametric statistical method for correlations, was used to detect the association between the 4 variables. SPSS version 25.0 was used to perform all the analyses.
To test the serial multiple mediation hypotheses illustrating psychological mechanism of LLDs after donation, Model 6 of SPSS PROCESS v.4.1 macro was utilized [40]. This approach, employing bootstrapping, does not require the assumption of normality [41]. Post-donation regret was entered as the independent variable, anxiety as the dependent variable, family relationships as the first mediator, and mastery as the second mediator. These 4 variables were treated as continuous variables. Notably, mediation analysis of the effect of post-donation regret on anxiety was conducted after controlling for sex, age, postoperative complications, time since donation, and the recipient’s death, which were identified as predictors of anxiety in previous research [14]. Using 10 000 bootstrap resamples and a 95% confidence interval (CI), the significance of the direct and indirect effects was evaluated.
Cases were excluded if the missing values constituted more than 50% of the items for each instrument, or if the information for control variables was missing (1 case for the FRI, 1 case for the GAD-2, and 2 cases for recipient death). If the missing values were less than 50% of items for each instrument, the expectation-maximization approach was used (3 cases for the FRI and 3 cases for the PMS). This imputation algorithm substitutes missing data with the best value using maximum likelihood estimation. Consequently, a total of 120 cases were analyzed in the mediation model.
Results
Sample Characteristics
Table 1 shows LLDs’ demographic and clinical characteristics. Seventy LLDs were male (56.5%). Their mean age was 37.9±11.4 years. Most of LLDs were children of the recipients (71.0%). Over half of the LLDs were single (55.6%). Among 124 LLDs, 7 (5.7%) experienced Grade II complications, and only 3 (2.4%) had Grade III complications. The average time since donation was 2.1±2.2 years. A small percentage of the recipients (8.9%) had died. The prevalence of regret and anxiety was 3.2% and 5.6%, respectively.
Table 1.
Sample demographic and clinical characteristics (N=124).
| n (%) | M±SD | |
|---|---|---|
| Sex | ||
| Male | 70 (56.5) | |
| Female | 54 (43.5) | |
| Age (years) | 37.9±11.4 | |
| Relationship to the recipient | ||
| Children | 88 (71.0) | |
| Spouses | 17 (13.7) | |
| Siblings | 11 (8.9) | |
| Parents | 8 (6.4) | |
| Marital status | ||
| Single (includes divorced) | 69 (55.6) | |
| Married | 55 (44.4) | |
| Length of hospital stay (days) | 9.5±3.2 | |
| Postoperative complications | ||
| None | 64 (51.6) | |
| Grade I | 50 (40.3) | |
| Grade II | 7 (5.7) | |
| Grade III | 3 (2.4) | |
| Time since donation (years) | 2.1±2.2 | |
| Recipient status | ||
| Survived | 111 (89.5) | |
| Died | 11 (8.9) | |
| Unknown | 2 (1.6) |
Correlations Between Study Variables
Table 2 outlines the ranges, mean scores, and bivariate correlations between the 4 main variables. Post-donation regret was negatively correlated with family relationships (p<0.001) and mastery (p=0.003); regret was positively correlated with anxiety (p<0.001). Worse family relationships were linked to lower levels of mastery (p<0.001) and higher degrees of anxiety (p<0.001). Furthermore, a negative association was discovered between mastery and anxiety (p<0.001).
Table 2.
Descriptive statistics and correlations among post-donation regret, family relationships, mastery, and anxiety (N=124).
| Variables | Range | M±SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| ρ | ρ | ρ | ρ | |||
| 1. Post-donation regret | 1–4 | 1.28±0.55 | 1 | |||
| 2. Family relationships | 34–96 | 77.02±12.42 | −0.405*** | 1 | ||
| 3. Mastery | 10–28 | 23.97±3.68 | −0.264** | 0.411*** | 1 | |
| 4. Anxiety | 0–6 | 0.46±0.99 | 0.311*** | −0.494*** | −0.343*** | 1 |
p<0.01,
p<0.001.
Serial Multiple Mediating Effects of Family Relationships and Mastery
Table 3 and Figure 1 show the serial multiple mediation effects of family relationships and mastery on the association between post-donation regret and anxiety after controlling all covariates. Post-donation regret had a statistically significant total effect on anxiety (B=0.41, p<0.05; R2=0.15, p<0.01). However, the direct effect of post-donation regret on anxiety was insignificant (B=−0.05, p=0.733), indicating a significant total indirect effect. In the multiple mediation model, an additional predictor of anxiety was postoperative complications of Grade II or III (B=0.64, p<0.05).
Table 3.
Results of the regression analyses testing the serial multiple mediation effect of family relationships and mastery on the relationship between post-donation regret and anxiety (N=120).
| Predictors | Direct effect (SE) | Total effect (SE) | ||
|---|---|---|---|---|
| Family relationships | Mastery | Anxiety | Anxiety | |
| Post-donation regret | −10.60 (1.91)*** | −0.49 (0.64) | −0.05 (0.15) | 0.41 (0.16)* |
| Family relationships | 0.10 (0.03)*** | −0.03 (0.01)*** | ||
| Mastery | −0.08 (0.02)** | |||
| Covariates | ||||
| Sex | 0.90 (2.12) | −0.73 (0.63) | −0.26 (0.15) | −0.24 (0.18) |
| Age | 0.19 (0.09)* | 0.05 (0.03) | 0.01 (0.01) | 0.00 (0.01) |
| Postoperative complications | −0.99 (3.78) | −2.82 (1.12)* | 0.64 (0.28)* | 0.91 (0.32)* |
| Years since donation | −0.35 (0.48) | −0.17 (0.14) | 0.02 (0.04) | 0.04 (0.04) |
| Recipient death | 1.18 (3.64) | 0.30 (1.08) | −0.17 (0.26) | −0.24 (0.31) |
| R 2 | 0.24*** | 0.24*** | 0.41*** | 0.15** |
p<0.05,
p<0.01,
p<0.001.
Figure 1.
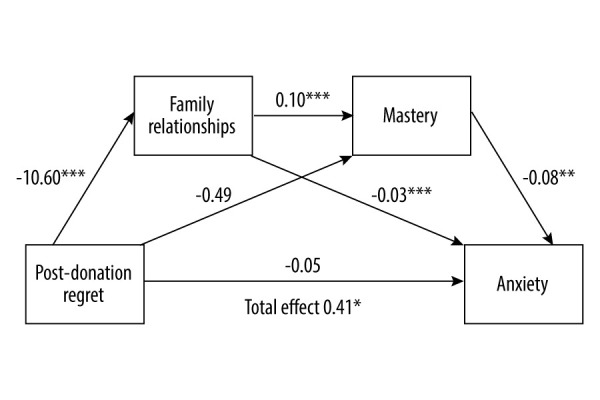
The relationship between post-donation regret and anxiety mediated by family relationships and mastery (N=120). All path coefficients are shown in unstandardized values. * p<0.05, ** p<0.01, *** p<0.001. The figure was created using PowerPoint (Version: 2403; Manufacturer: Microsoft).
Table 4 presents the indirect effects in the serial multiple mediation model. The total indirect effect of post-donation regret on anxiety was significant (B=0.457, 95% CI=0.194, 0.761). The indirect effect through family relationships was found to be significant (B=0.329, 95% CI=0.130, 0.563). Also, the indirect effect through family relationships and mastery in serial were significant (B=0.088, 95% CI=0.008, 0.232). However, the indirect effect through mastery was insignificant (B=0.040, 95% CI=−0.105, 0.180).
Table 4.
Indirect effects in the serial multiple mediation model (N=120).
| B | Boot SE | Boot LLCI | Boot ULCI | |
|---|---|---|---|---|
| Total indirect effect | 0.457 | 0.146 | 0.194 | 0.761 |
| Post-donation regret → family relationships → anxiety | 0.329 | 0.110 | 0.130 | 0.563 |
| Post-donation regret → mastery → anxiety | 0.040 | 0.069 | −0.105 | 0.180 |
| Post-donation regret → family relationships → mastery → anxiety | 0.088 | 0.058 | 0.008 | 0.232 |
LLCI – lower limit confidence interval; ULCI – upper limit confidence interval.
Discussion
This study found that post-donation regret had total effects on anxiety, solely mediated by family relationships, and sequentially mediated by family relationships and mastery. However, post-donation regret had no significant direct effect on anxiety, and the simple mediating effect of mastery was not significant. These results partially supported our hypotheses, underpinned by the SPM.
Among the study participants, a prevalence rate of anxiety was 5.6%. This rate appears marginally higher than the reported 12-month prevalence rate of anxiety disorder within the general Korean population in 2021 [42], the year during which our dataset was compiled. Notably, the variance between these rates may be attributed to demographic disparities, particularly in age composition, between the study sample and the general population. The study sample had an age range of 19–63 years, with most in the 20–30 age bracket. Conversely, the general population encompassed individuals aged 18–79 years, with a higher representation in the 50–60 age group. Such findings suggest that young adults, grappling with the uncertainties inherent in early adulthood and associated developmental milestones like employment and marriage, may be predisposed to heightened levels of anxiety, potentially exacerbated by the postponement or disruption of these life pursuits owing to organ donation [43]. Moreover, our study revealed that postoperative complications exerted a discernible impact on LLD’s anxiety levels. While a minority of LLDs reported complications exceeding their expectations [11], the resultant unmet expectations could plausibly contribute to heightened anxiety levels. Additionally, the anxiety experienced by donors may stem from the unfamiliarity of undergoing surgery when previously in good health, juxtaposed with the experience of acute pain and discomfort. A meta-analysis corroborates these findings, indicating a post-donation prevalence rate of anxiety among LLDs at 10.0%, with anxiety being most pronounced within the initial 3 months after donation [14]. Concerns over unforeseen medical expenses stemming from complications may further exacerbate anxiety levels [14]. Consequently, implementing policies that offer financial support for both donors and recipients may be a salient intervention strategy [43].
Our study underscores the notable influence of post-donation regret on anxiety symptomology. Hence, vigilantly monitoring and addressing feelings of regret among LLDs is important, given their susceptibility to heightened anxiety levels. Notably, only 3.2% of participants in this study reported experiencing feelings of regret regarding their donation decision. This finding aligns with the literature, as evidenced by a systematic review reporting a prevalence rate of post-donation regret among LLDs ranging from 0% to 11.4% [8]. However, more recent research conducted in Germany and Turkey, encompassing a follow-up period of up to 20 years after donation, revealed a regret prevalence rate of 27.5% [44]. Furthermore, a study in Egypt found that 67% of LLDs would not donate again [45]. Noteworthy distinctions between these studies and our own lie in the scope of donor–recipient relationships examined, with our study focusing on second-degree relatives, while the aforementioned studies encompassed relatives up to the fourth degree and non-relatives [44,45]. This may have contributed to the prevalence of regret. The cultural atmosphere may also have influenced the rate of regret across studies. Furthermore, short-term regret (a year after donation) has been reported to be associated with health perceptions and social functioning [46]. Donors had also expressed feeling abandoned owing to the sudden lack of tracking of their psychological issues in a clinical setting after donation [47], which might lead to long-term regret. Therefore, to prevent regret, healthcare providers should continue to care for and help donors to be aware of their health status and to reintegrate into society.
This study also demonstrated that family relationships mediate the associations between post-donation regret and anxiety. Family LLDs with greater regret had worse family relationships, ultimately leading to higher levels of anxiety, but good family relationships can buffer against anxiety. This aligns with findings from a qualitative study that showed the importance of adequate support from family members in facilitating donors’ recovery and adapting to their future lives [9]. Additionally, Noma et al discovered that the availability of family support prior to donation is crucial in determining donors’ psychosocial states after donation [48]. Our study is meaningful in that it quantitively explores the positive impact of supportive family relationships on family LLDs after donation. Especially in Asian societies, decision-making for an LDLT is family-centered [49]. In this context, the greater the donor’s regret about the decision to donate, the more likely it is for family conflict or discord to arise. Moreover, poorer family relationships might be correlated with higher levels of anxiety in family LLDs.
An interesting finding in our study is that family relationships and mastery sequentially mediated the association between post-donation regret and anxiety. Similarly, high levels of personal mastery alleviate anxiety symptoms among Asian family caregivers [24]. Our study adds to the evidence that personal mastery among LLDs is influenced by family relationships, which in turn affects anxiety levels. In Eastern cultures, such as South Korea, which value familial commitment, family donor candidates were reported to have more family-related motives for liver donation than self-related motives [50]. Our study suggests that this trend persists after surgery; lower levels of support, help, and encouragement, along with higher levels of conflict within a family, may undermine the sense of mastery among LLDs experiencing regret. However, family members’ expressions of gratitude for the bravery and commitment shown in donating a liver can bolster LLDs’ sense of personal mastery. Moreover, this enhanced sense of mastery might help to alleviate anxiety. Therefore, this study is meaningful as it empirically demonstrates the importance of a family-centered and mastery-based intervention in the care of family LLDs, even after donation.
To provide family-centered care, the first step is to strengthen the relationship between the donor and recipient. Although LLDs may experience both physical and psychological discomfort after donation, they often hesitate to express their struggles for fear of burdening or worrying the recipient, leading them to endure their feelings alone [43,51]. Recipients may feel infinite gratitude towards the donor but may also experience feelings of guilt and hesitation in expressing these openly [51,52]. In some cases, living donation can intensify unsolved tension, disappointments, and resentments between them [52]. Therefore, healthcare professionals should provide education and counseling to help them understand, appreciate, and navigate their shared journey together, facilitating better adaptation to changes in the dynamics of their relationships [20,52].
Additionally, in transplant families, family caregivers may feel overwhelmed with the responsibility of caring for both the recipient and the donor, potentially leading to feelings of inadequacy in attending to the donor’s needs [53]. Conversely, donors may perceive a lack of attention from the family owing to the focus on the recipient’s care [49]. To alleviate the care burden on family caregivers and ensure adequate support for donors, it is essential to implement support systems tailored to the needs of transplant families. These may include the use of care assistants for the recipient, home care services specifically designed for transplant families, and support plans for leisure activities to promote overall well-being within these families [53].
Although the effects of mastery on anxiety are more likely to be significant when preceded by positive family relationships, interventions such as cognitive behavioral therapy can be applied to promote mastery. Providing LLDs with psychoeducation regarding the mechanisms of change can help them recognize fatalistic and helpless attitudes and shift towards more flexible and constructive thoughts, thereby enhancing their sense of mastery [54]. For instance, Wirken et al [55] demonstrated improvements in postoperative psychosocial outcomes by providing cognitive behavioral therapy to living donors via a website. Incorporating the content of mastery into such interventions could further enhance their effectiveness.
This study has limitations. First, the cross-sectional design of the study may not be able to demonstrate causal relationships. However, given that the SPM was used to establish these relationships, they appear plausible. Second, the data collected from a single transplant center could hinder the generalization of our findings. Future prospective studies should include multiple transplant centers in different countries. Third, post-donation regret was measured using a single item with 4 scores, which could result in response bias. Future research should measure regret using questionnaires with more items or granular scoring. Lastly, it is pertinent to acknowledge the inherent limitations stemming from the secondary analysis used in this study. The dataset under scrutiny lacked inclusion of certain potential confounding factors, such as financial status, perceptions of overall health, and social activity, which consequently precluded their incorporation into the mediation model. This limitation necessitates a cautious interpretation of the research findings, mindful of the contextual constraints imposed by the available data.
Conclusions
Family LLDs with greater post-donation regret were more susceptible to anxiety symptoms. Furthermore, family relationships and mastery sequentially mediated the relationship between post-donation regret and anxiety, with family relationships being a key element in this mediation. Therefore, regular psychosocial counseling and education that includes family members are recommended. To ultimately reduce anxiety, healthcare professionals and clinical nurses should consistently monitor the psychological status of LLDs and develop intervention programs that foster a positive family environment and enhance mastery.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151–71. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 2.Hill AL, Khan M, Kiani AZ, et al. Global liver transplantation: Emerging trends and ethical challenges. Langenbecks Arch Surg. 2023;408:418. doi: 10.1007/s00423-023-03144-4. [DOI] [PubMed] [Google Scholar]
- 3.Korean Network for Organ Sharing (KONOS) Annual report of the transplant 2021. Seoul: Ministry of Health and Welfare KONOS; 2022. [Google Scholar]
- 4.Morooka Y, Umeshita K, Taketomi A, et al. Long-term donor quality of life after living donor liver transplantation in Japan. Clin Transplant. 2019;33:e13584. doi: 10.1111/ctr.13584. [DOI] [PubMed] [Google Scholar]
- 5.Shen CJ, Huang HL, Chen KH, et al. Comparison of liver function, emotional status, and quality of life of living liver donors in Taiwan. Transplant Proc. 2016;48:1007–11. doi: 10.1016/j.transproceed.2015.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Tseng SC, Lee WC, Chen KH, et al. Anxiety, pain intensity, and decision regret of living liver donors during postoperative period. Appl Nurs Res. 2023;69:151662. doi: 10.1016/j.apnr.2022.151662. [DOI] [PubMed] [Google Scholar]
- 7.Bhurtyal N, Paudel K, Shah S, et al. Anxiety and depression among living kidney donors in tertiary care hospital of low resource country setting Nepal. Ann Med Surg (Lond) 2022;80:104119. doi: 10.1016/j.amsu.2022.104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ong JQ, Lim LJ, Ho RC, Ho CS. Depression, anxiety, and associated psychological outcomes in living organ transplant donors: A systematic review. Gen Hosp Psychiatry. 2021;70:51–75. doi: 10.1016/j.genhosppsych.2021.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Papachristou C, Walter M, Frommer J, Klapp BF. A model of risk and protective factors influencing the postoperative course of living liver donors. Transplant Proc. 2009;41:1682–86. doi: 10.1016/j.transproceed.2009.02.096. [DOI] [PubMed] [Google Scholar]
- 10.Weng LC, Huang HL, Wang YW, et al. The coping experience of Taiwanese male donors in living donor liver transplantation. Nurs Res. 2012;61:133–39. doi: 10.1097/NNR.0b013e3182475688. [DOI] [PubMed] [Google Scholar]
- 11.Lee YS, Koh CK, Yi NJ, et al. Does living liver donors’ underestimation about surgical outcomes impact on their health-related quality of life after donation?: A descriptive cross-sectional study. Health Qual Life Outcomes. 2022;20:146. doi: 10.1186/s12955-022-02055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holscher CM, Leanza J, Thomas AG, et al. Anxiety, depression, and regret of donation in living kidney donors. BMC Nephrol. 2018;19:218. doi: 10.1186/s12882-018-1024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang DHS, Yang J. Adaptation experience of living kidney donors after donation. J Korean Acad Nurs. 2016;46:271–82. doi: 10.4040/jkan.2016.46.2.271. [DOI] [PubMed] [Google Scholar]
- 14.Fan Y, Nashan B, Wu X, Shi Y. Prevalence and factors associated with depression and anxiety in living liver donors: A systematic review and meta-analysis. J Psychosom Res. 2023;173:111443. doi: 10.1016/j.jpsychores.2023.111443. [DOI] [PubMed] [Google Scholar]
- 15.Crombie AK, Franklin PM. Family issues implicit in living donation. Mortality (Abingdon) 2006;11:196–210. [Google Scholar]
- 16.Lee SH, Lim KC, Jeon MK, et al. Postoperative pain and influencing factors among living liver donors. Transplant Proc. 2012;44:363–65. doi: 10.1016/j.transproceed.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: An overview of concepts and their measures. Gerontologist. 1990;30:583–94. doi: 10.1093/geront/30.5.583. [DOI] [PubMed] [Google Scholar]
- 18.Hish AJ, Nagy GA, Fang CM, et al. Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci Educ. 2019;18:ar51. doi: 10.1187/cbe.19-03-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirk DL, Kabdebo I, Whitehead L. Prevalence of distress and its associated factors among caregivers of people diagnosed with cancer: A cross-sectional study. J Clin Nurs. 2022;31:3402–13. doi: 10.1111/jocn.16167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ralph AF, Butow P, Craig JC, et al. Living kidney donor and recipient perspectives on their relationship: Longitudinal semi-structured interviews. BMJ Open. 2019;9:e026629. doi: 10.1136/bmjopen-2018-026629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halverson CM, Crowley-Matoka M, Ross LF. Unspoken ambivalence in kinship obligation in living donation. Prog Transplant. 2018;28:250–55. doi: 10.1177/1526924818781562. [DOI] [PubMed] [Google Scholar]
- 22.Pearlin LI, Bierman A. Current issues and future directions in research into the stress process. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the sociology of mental health. 2nd ed. Springer; 2013. pp. 325–40. [Google Scholar]
- 23.Knussen C, Tolson D, Swan IRC, et al. Stress proliferation in caregivers: The relationships between caregiving stressors and deterioration in family relationships. Psychol Health. 2005;20:207–21. [Google Scholar]
- 24.Chan EY, Glass G, Chua KC, et al. Relationship between mastery and caregiving competence in protecting against burden, anxiety and depression among caregivers of frail older adults. J Nutr Health Aging. 2018;22:1238–45. doi: 10.1007/s12603-018-1098-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roese NJ, Epstude KA, Fessel F, et al. Repetitive regret, depression, and anxiety: Findings from a nationally representative survey. J Soc Clin Psychol. 2009;28:671–88. [Google Scholar]
- 26.Hawi NS, Samaha M. Relationships among smartphone addiction, anxiety, and family relations. Behav Inf Technol. 2017;36:1046–52. [Google Scholar]
- 27.Ballash NG, Pemble MK, Usui WM, et al. Family functioning, perceived control, and anxiety: A mediational model. J Anxiety Disord. 2006;20:486–97. doi: 10.1016/j.janxdis.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Burns RA, Anstey KJ, Windsor TD. Subjective well-being mediates the effects of resilience and mastery on depression and anxiety in a large community sample of young and middle-aged adults. Aust N Z J Psychiatry. 2011;45:240–48. doi: 10.3109/00048674.2010.529604. [DOI] [PubMed] [Google Scholar]
- 29.Zalta AK, Chambless DL. Understanding gender differences in anxiety: The mediating effects of instrumentality and mastery. Psychol Women Q. 2012;36:488–99. [Google Scholar]
- 30.Desrochers S, Sargent LD, Hostetler AJ. Boundary-spanning demands, personal mastery, and family satisfaction: Individual and crossover effects among dual-earner parents. Marriage Fam Rev. 2012;48:443–64. [Google Scholar]
- 31.Lee HY. Research methodology. 2nd ed. Seoul: Cheongram; 2012. [Google Scholar]
- 32.Rodrigue JR, Schold JD, Morrissey P, et al. Mood, body image, fear of kidney failure, life satisfaction, and decisional stability following living kidney donation: Findings from the KDOC study. Am J Transplant. 2018;18:1397–407. doi: 10.1111/ajt.14618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moos R, Moos B. Family environment scale manual: Development, applications and research. 4th ed. Palo Alto (CA): Mind Garden Inc; 2009. [Google Scholar]
- 34.Park JH. Validity of the family environment scale-Korean version (FES-K) J Korean Fam Ther. 2004;12:1–26. [Google Scholar]
- 35.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- 36.Kim MH, Chung SD, Lee GY. Development and evaluation of preventive mental health program for depression among the elderly in community. Korean J Soc Welf. 2001;44:318–46. [Google Scholar]
- 37.Kroenke K, Spitzer RL, Williams JB, et al. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 38.Ahn JK, Kim Y, Choi KH. The psychometric properties and clinical utility of the Korean version of GAD-7 and GAD-2. Front Psychiatry. 2019;10:127. doi: 10.3389/fpsyt.2019.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: The Guilford Press; 2013. [Google Scholar]
- 41.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 42.Rim SJ, Hahm BJ, Seong SJ, et al. Prevalence of mental disorders and associated factors in Korean adults: National Mental Health Survey of Korea 2021. Psychiatry Investig. 2023;20:262. doi: 10.30773/pi.2022.0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bang M, Shin H, Ryu M, Kwon S. Young adult donor’s experiences of living donor liver transplantation. J Korean Acad Nurs. 2021;51:105–18. doi: 10.4040/jkan.20235. [DOI] [PubMed] [Google Scholar]
- 44.Andacoglu O, Sabisch E, Malamutmann E, et al. Multi-center living liver donor quality of life survey up to 20 years after donor hepatectomy and association with surgical outcomes. HPB (Oxford) 2022;24:1975–79. doi: 10.1016/j.hpb.2022.06.007. [DOI] [PubMed] [Google Scholar]
- 45.El-Meteini M, Shorub E, Mahmoud DA, et al. Psychosocial profile and psychiatric morbidity among Egyptian patients after living donor liver transplantation. Middle East Current Psychiatry. 2019;26:1–8. [Google Scholar]
- 46.Wirken L, van Middendorp H, Hooghof CW, et al. Psychosocial consequences of living kidney donation: A prospective multicentre study on health-related quality of life, donor–recipient relationships and regret. Nephrol Dial Transplant. 2019;34:1045–55. doi: 10.1093/ndt/gfy307. [DOI] [PubMed] [Google Scholar]
- 47.Bahador RS, Mangolian P, Farokhzadian J, et al. Analysis of implications of organ donation on living donors in southeastern Iran: A qualitative study. Russ J Transplantol Artif Organs. 2022;24:126–36. [Google Scholar]
- 48.Noma SI, Hayashi A, Uehara M, et al. Comparison between psychosocial long-term outcomes of recipients and donors after adult-to-adult living donor liver transplantation. Clin Transplant. 2011;25:714–20. doi: 10.1111/j.1399-0012.2010.01337.x. [DOI] [PubMed] [Google Scholar]
- 49.Lin YP, Chen J, Lee WC, Chiang YJ, Huang CW. Understanding family dynamics in adult-to-adult living donor liver transplantation decision-making in Taiwan: Motivation, communication, and ambivalence. Am J Transplant. 2021;21:1068–79. doi: 10.1111/ajt.16281. [DOI] [PubMed] [Google Scholar]
- 50.Ryu S, Yoon SC, Hong KE, Kim JM. Psychosocial issues related to donor’s decision-making in living donor liver transplantation. Ann Transplant. 2019;24:576–83. doi: 10.12659/AOT.916340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jang HY, Im HY, Nam HJ. The life experiences of living liver donors: A qualitative meta-synthesis. Res Nurs Health. 2022;45:693–706. doi: 10.1002/nur.22273. [DOI] [PubMed] [Google Scholar]
- 52.Ralph AF, Butow P, Hanson CS, et al. Donor and recipient views on their relationship in living kidney donation: Thematic synthesis of qualitative studies. Am J Kidney Dis. 2017;69:602–16. doi: 10.1053/j.ajkd.2016.09.017. [DOI] [PubMed] [Google Scholar]
- 53.Bang M, Kwon S. The caring experience of family caregivers for patients of living donor liver transplantation from the family members. J Korean Acad Nurs. 2022;52:435–50. doi: 10.4040/jkan.22043. [DOI] [PubMed] [Google Scholar]
- 54.Jackson C, Nissenson K, Cloitre M. Cognitive-behavioral therapy. In: Courtois CA, Ford JD, editors. Treating complex traumatic stress disorders: An evidence-based guide. New York: The Guilford Press; 2009. pp. 243–63. [Google Scholar]
- 55.Wirken L, van Middendorp H, Hooghof CW, et al. Development and feasibility of a guided and tailored internet-based cognitive-behavioural intervention for kidney donors and kidney donor candidates. BMJ open. 2018;8:e020906. doi: 10.1136/bmjopen-2017-020906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


