Abstract
Background
There are many factors that affect human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS)-related deaths, and different antiretroviral therapy (ART) strategies may affect HIV/AIDS-related fatality rates. However, studies on this area are very limited. This study aimed to evaluate the factors associated with HIV/AIDS-related mortality and the impact of different ART strategies in Lu’an City, Anhui Province, China, 1999–2023.
Material/Methods
Data of HIV/AIDS cases were downloaded from the China HIV/AIDS Comprehensive Response Information Management System, and were assessed to evaluate the impact of different ART strategies on the related fatality rate using interrupted time series (ITS).
Results
We found that age at diagnosis of 15 years, 25 years, 40 years, and 60 years, as well as receiving ART, were protective factors against death (with P below 0.05), while lower CD4 count at the last CD4 count and the year of diagnosis before 2007 and between 2007 and 2016 were risk factors (with P below 0.05). ITS analysis revealed that in the year of the introduction of free ART in 2006, the fatality rate decreased by 38.60% (P=0.015). The fatality rate trend from 2006 to 2015 was −1.1%, which was not statistically significant (P=0.434). The fatality rate trend from 2016 to 2023 was −0.33%, indicating a decreasing trend (P=0.000).
Conclusions
Children under 15 years old and elderly patients had a higher risk of death. The main reasons for the decrease in HIV/AIDS-related fatality rate were ART, especially the “early treatment” strategy.
Keywords: Antiretroviral Therapy, Highly Active; HIV; Interrupted Time Series Analysis; Mortality
Introduction
Acquired immunodeficiency syndrome (AIDS) is a severe infectious disease caused by the human immunodeficiency virus (HIV), resulting in a high fatality rate [1]. According to the 2023 Global AIDS Progress Report by The Joint United Nations Programme on HIV/AIDS (UNAIDS), in 2022 alone, 1.3 million people worldwide were infected with HIV, and 630 000 people died from AIDS-related illnesses [2]. Antiretroviral therapy (ART) is usually a combination of 3 or more antiretroviral drugs for the control and treatment of human immunodeficiency virus type 1 (HIV-1), which inhibits HIV replication through a variety of mechanisms. Most of the newly diagnosed patients were treated with 2 nucleoside reverse transcriptase inhibitors (NRTIs) and 1 non-nucleoside reverse transcriptase inhibitor (NNRTIs) or integrase strand transfer inhibitor (INSTIs) [3,4]. It has been confirmed that ART is the most effective measure to suppress HIV replication. It not only effectively improves the health status of HIV/AIDS patients and prolongs their lives [5–8], but also prevents the further spread of HIV, protecting the general population [9]. Data released by UNAIDS show that with the promotion of ART, the number of global deaths from AIDS-related diseases has decreased from 1.1 million in 2010 to 630 000 in 2022 [2]. In 2003, the Chinese government began providing free ART services to AIDS patients, with the eligibility criteria for inclusion changing from a CD4 count <200 cells/μL to <350 cells/μL, and then to <500 cells/μL. In 2016, the “early treatment” strategy was implemented, providing universal testing for high-risk populations and offering rapid treatment to all diagnosed HIV/AIDS patients regardless of their CD4 count or clinical stage. As of the end of December 2022, there were 1.135 million HIV-infected individuals under treatment in China, with the treatment rate for surviving patients increasing from 15.9% initially to 92.8% [10,11]. However, the case fatality rate of HIV/AIDS patients decreased from 5.4% in 2013 to 2.7% in 2022, showing a significant negative correlation [12]. Universal testing and treatment were widely implemented in some high-burden HIV countries before 2016 [13–15]. Results from a randomized population trial in Botswana showed that universal testing and treatment could improve viral suppression rates [16] and reduce the incidence and mortality of HIV/AIDS [16]. Studies in China have also confirmed that with the lowering of treatment entry thresholds and the increase in treatment coverage, the fatality rate of HIV/AIDS decreased from 39/100 person-years in 2002 to 3.7/100 person-years in 2019 [17]. A literature review by China Medical University showed that after more than 3 decades of AIDS prevention and control in China, by 2017, the viral suppression rate of HIV/AIDS patients had reached 91%, and the fatality rate had dropped to 3.6% [18]. Although many countries have adjusted and changed their HIV/AIDS treatment strategies at different times, there is limited research on the impact of different ART strategies on related fatality rates outside of Africa.
Lu’an City recorded its first case of HIV/AIDS in 1999 and launched free HIV voluntary counseling and testing (VCT) services citywide in 2004. Free ART became available in 2006, with cases selected based on national treatment standards. Patients were initially treated with a combination of 2 NRTIs and 1 NNRTIs. Patients who failed the first treatment regimen were treated with 2 NRTIs and 1 protease inhibitor (PIs) according to the results of drug resistance testing. Before 2014, we conducted a retrospective cohort study to investigate the survival time and influencing factors of HIV/AIDS patients. We found that the median survival time of HIV/AIDS patients was 12 years, and a low CD4 count at diagnosis was identified as a risk factor for death among patients receiving ART [19]. However, given the adjustments and changes in ART strategies, the fatality rate and influencing factors of HIV/AIDS patients might have changed. It is therefore crucial to promptly assess the impact of adjusted ART strategies on related fatality rates. Based on the data of reported HIV/AIDS cases in Lu’an City from 1999 to 2023, this study aimed to evaluate the influencing factors of HIV/AIDS-related deaths and the impact of different ART strategies on the HIV/AIDS-related fatality rate in Lu’an City, Anhui Province, China, 1999–2023.
Material and Methods
Ethics Statement
Since patients had already signed informed consent forms upon enrollment in the AIDS comprehensive prevention and control information system, the data used in this study were from existing anonymous patient records in the information system and did not require additional informed consent from the patients. Approval was obtained from the Ethics Committee of the Lu’an Center for Disease Control and Prevention (NO. 2024003).
Data Source
HIV/AIDS case data reported and managed in Lu’an City from 1999 to 2023 were obtained from the China HIV/AIDS Comprehensive Response Information Management System. The system contained very comprehensive information on the cases, including basic demographic information, the time of diagnosis of HIV infection, epidemiological investigation data, clinical examination and treatment records, observation and follow-up records at different periods, patient outcome, and cause of death. Inclusion criteria for cases were as follows: (1) current residence in Lu’an City; (2) audit status marked as final review; (3) HIV antibody confirmed positive with a diagnosis date between January 1, 1999, and December 31, 2023. We excluded duplicate case reports.
HIV screening has been carried out in medical institutions since 1997 in Lu’an City, and the first case of HIV/AIDS was found in 1999. We carried out epidemiological investigation and CD4 testing for confirmed HIV/AIDS patients, and those who met the treatment conditions were referred to designated medical institutions for treatment, and the treatment effect was continuously monitored. All the investigation information and clinical data of the patients were uploaded to the China Center for Disease Control and Prevention’s Comprehensive Information System for AIDS Prevention and Control. Details of the survey and information acquisition were previously published in the literature [9,19].
Calculation of HIV/AIDS-Related Fatality Rate
HIV/AIDS patients with HIV/AIDS-related diseases as the main cause of death were identified from the database. The crude fatality rate and annual fatality rate were computed. The crude fatality rate was used to analyze the influencing factors of death, while the annual fatality rate was utilized to assess the changing trend and evaluate the impact and effectiveness of different ART strategies on related fatality rates. The formula for calculating these rates was: Crude fatality rate=(number of deaths from HIV/AIDS-related diseases/number of HIV/AIDS patients)×100%. The annual fatality rate was calculated as the number of HIV/AIDS patients who died from HIV/AIDS-related diseases in a given year divided by the sum of the number of HIV/AIDS patients alive at the beginning of the year and half the difference between the number of new HIV/AIDS patients reported in that year and the number of HIV/AIDS patients who died in that year, multiplied by 100% [20]. The overall fatality rate was calculated as the number of deaths from HIV/AIDS-related diseases divided by the total person-years of observation. A retrospective cohort study design was employed, with the start point being the date of diagnosis and the endpoint being December 31, 2023. The outcome variable was death due to HIV/AIDS-related diseases, with censoring for death due to non-HIV/AIDS-related diseases or loss to follow-up. After diagnosis, HIV/AIDS patients underwent epidemiological investigations and CD4 testing by various levels of disease control and prevention institutions. Patients meeting the treatment criteria received medication at designated medical institutions, and all patient survey information and clinical data were uploaded to the National Comprehensive AIDS Prevention and Control Information System.
Construction of the ITS Model
Lu’an City initiated free ART services for HIV/AIDS patients in 2006 and introduced the “early treatment” strategy in June 2016. The interrupted time series (ITS) method was employed to assess the impact of these different treatment strategies on HIV/AIDS-related fatality rates. Accordingly, intervention time points were designated as 2006 and 2016, and the effects of various treatment strategies were evaluated across 3 phases: 1999–2005, 2007–2015, and 2017–2023. ITS analysis is a quasi-experimental design utilizing interrupted time series regression models to examine changes in outcome variables and slope changes resulting from different interventions, thereby assessing the effectiveness of these measures [21]. The model was formulated as follows:
In the ITS analysis, Yt represents the HIV/AIDS-related fatality rate in year t; time is a continuous variable taking values of 1, 2, 3, etc.; intervention1 and intervention2 are binary variables, with a value of 0 before the intervention and 1 after the intervention; and postslope1 and postslope2 are continuous variables after the intervention, with a value of 0 before the intervention and the same value as time after the intervention. β0 represents the fatality rate at the start of the study in 1999, β1 represents the slope before treatment, β2 represents the immediate change in fatality rate at the time of intervention1, reflecting the short-term effect of the treatment; β3 represents the long-term trend in fatality rate after intervention1; v4 represents the immediate change in fatality rate at the time of intervention2, β5 represents the long-term trend in fatality rate after intervention2; and ɛ is the error term, representing the part of the variation in the dependent variable that cannot be explained by the independent variables. ITS also requires that the outcome variables exhibit a linear trend before and after the intervention, and that there is no autocorrelation in the time series. For autocorrelated series, the Newey-West method was used to adjust the parameter standard errors. If there is no autocorrelation, ordinary least squares were used to construct the model.
Statistical Analysis
Data were organized and statistically analyzed using Excel 2013 and SPSS 20.0 software. Crude fatality rate, annual fatality rate, and overall fatality rate were calculated. Joinpoint regression program 4.9.0.1 software was utilized for Joinpoint regression analysis and drawing to calculate the average annual percent change (AAPC) and annual percentage change (APC) in different segments to assess the time trends in HIV/AIDS-related fatality rates. The chi-square test was used to compare the differences in HIV/AIDS-related fatality rate among different variables and univariate analysis, including gender, age, education level, marital status, route of infection, CD4 count at diagnosis, last CD4 count, whether to receive antiretroviral therapy, and the year of diagnosis. Non-conditional logistic regression modeling was used to conduct multivariate analysis on statistically significant variables in the chi-square test analysis to screen independent risk factors. ITS analysis was conducted to calculate the slope index, and evaluate the effect of different treatment strategies using Stata 17.0 software. All statistical tests used a significance level of α=0.05.
Results
Overview of Related Fatality Rate
From 1999 to 2023, there were a total of 2472 reported cases of HIV/AIDS in Lu’an City, with 416 HIV/AIDS-related deaths by the end of 2023, resulting in a cumulative fatality rate of 16.83%. The overall fatality rate was 3.80 per 100 person-years (416/10945), with the annual fatality rate decreasing from an initial 75.00 per 100 person-years to 2.54 per 100 person-years in 2023. Joinpoint regression analysis showed that the HIV/AIDS-related fatality rate declined generally, with an AAPC of −14.20% (Z=−8.20, P<0.001) from 1999 to 2023. The rate of decline was segmented into 2 phases, with a turning point in 2009. In the first phase (1999–2009), the fatality rate decreased rapidly (APC=−20.10%, Z=−6.60, P<0.001), while in the second phase (2009–2023), the rate of decline slowed down (APC=−9.70%, Z=−5.000, P<0.001). Refer to Figure 1.
Figure 1.
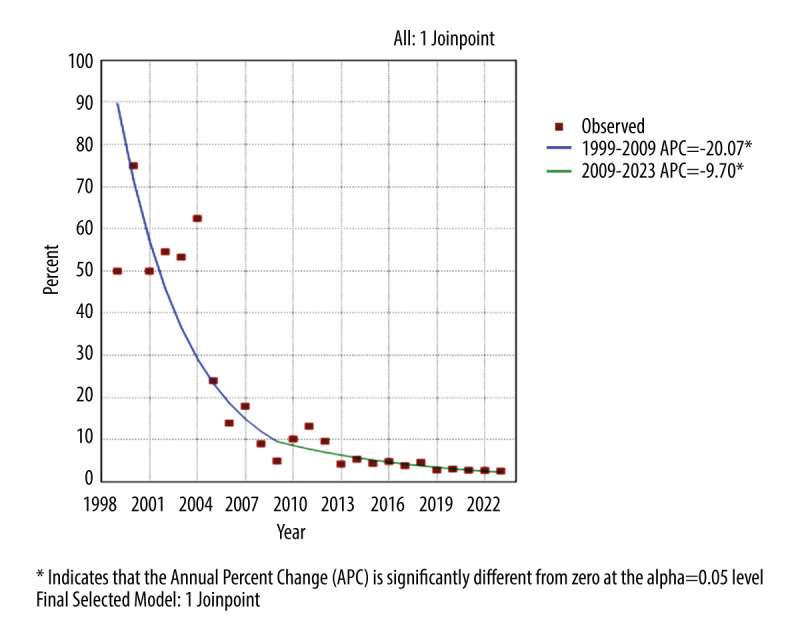
Trends in HIV/AIDS-related fatality rates in Lu’an City, 1999–2023. Models were based on Joinpoint regression analysis. Annual percentage change (APC) >0 indicated that the related mortality increased year by year, and APC <0 indicated that the related mortality decreased year by year. The authors utilized Joinpoint regression program 4.9.0.1 software (National Cancer Institute, NCI) to generate all figures.
Related Fatality Rate of HIV/AIDS Patients With Different Characteristics
Univariate analysis showed that there were no statistically significant differences in fatality rates between genders (χ2=0.219, P=0.640). However, fatality rates varied significantly based on age at diagnosis, education level, marital status, route of infection, CD4 count at diagnosis, last CD4 count, ART status, and year of diagnosis (all P<0.05). Fatality rates tended to increase with age, except for the group under 15 years old. Higher education levels were associated with lower fatality rates. Fatality rates were highest when the CD4 count was not detected, while they were lowest when the CD4 count was ≥350 cells/μL at both the first visit and endpoint (χ2=635.979 and 1101.784, respectively, all P<0.001). Cases diagnosed before 2007 had the highest fatality rates, which decreased over time (see Table 1).
Table 1.
HIV/AIDS-related fatality rates: Univariate analysis.
| Variables | Number of cases | Number of deaths | Fatality rate (%) | χ2 | P value |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 1994 | 339 | 17.00 | 0.219 | 0.640 |
| Female | 487 | 77 | 15.81 | ||
| Age at diagnosis (years) | |||||
| <15 | 26 | 8 | 30.77 | 89.207 | <0.001 |
| 15~ | 296 | 17 | 5.74 | ||
| 25~ | 786 | 95 | 12.09 | ||
| 40~ | 875 | 147 | 16.80 | ||
| 60~ | 304 | 83 | 27.30 | ||
| 70~ | 185 | 66 | 35.68 | ||
| Education Level | |||||
| Primary school and below | 881 | 210 | 23.84 | 51.063 | <0.001 |
| Junior high school | 884 | 131 | 14.82 | ||
| High school | 396 | 51 | 12.88 | ||
| College or above | 311 | 24 | 7.72 | ||
| Marital status | |||||
| Married with spouse | 1085 | 182 | 16.77 | 25.120 | <0.001 |
| Unmarried | 769 | 95 | 12.35 | ||
| Divorced or widowed | 612 | 138 | 22.55 | ||
| Unknown | 6 | 1 | 16.67 | ||
| Route of infection | |||||
| Blood donation/plasma | 8 | 3 | 37.50 | 131.258 | <0.001 |
| Blood transfusion/blood products | 48 | 30 | 62.50 | ||
| Mother-to-child transmission | 23 | 6 | 26.09 | ||
| Heterosexual transmission | 1557 | 298 | 19.14 | ||
| Homosexual transmission | 807 | 68 | 8.43 | ||
| Drug use | 8 | 3 | 37.50 | ||
| Unknown/other | 21 | 8 | 38.10 | ||
| CD4 count at diagnosis (cells/ul) | |||||
| Not tested* | 206 | 189 | 91.75 | 635.979 | <0.001 |
| <50 | 323 | 84 | 26.01 | ||
| 50~ | 514 | 69 | 13.42 | ||
| 200~ | 636 | 37 | 5.82 | ||
| 350~ | 793 | 37 | 4.67 | ||
| Last CD4 count (cells/ul) | |||||
| Not tested* | 206 | 189 | 91.75 | 1101.784 | <0.001 |
| <50 | 128 | 74 | 57.81 | ||
| 50~ | 286 | 71 | 24.83 | ||
| 200~ | 498 | 48 | 9.64 | ||
| 350~ | 1354 | 34 | 2.51 | ||
| ART | |||||
| Yes | 2197 | 222 | 10.10 | 637.903 | <0.001 |
| No | 275 | 194 | 70.55 | ||
| Year of diagnosis | |||||
| Before 2007 | 55 | 32 | 58.18 | 99.969 | <0.001 |
| 2007–2016 | 731 | 174 | 23.80 | ||
| After 2017 | 1686 | 210 | 12.46 |
These patients died before CD4 count testing due to severe illness or non-compliance.
Multivariate Analysis of Related Fatality Rate
In the multivariate analysis using logistic regression, the results showed that age at diagnosis of 15 years, 25 years, and 40 years, as well as receiving antiviral treatment, were protective factors against HIV/AIDS-related fatality, while lower CD4 count at the last CD4 count and the year of diagnosis before 2007 and 2007–2016 were risk factors. Refer to Table 2.
Table 2.
Factors influencing HIV related fatality: multivariable analysis.
| Variable | OR | 95.0% CI | P value |
|---|---|---|---|
| Age at diagnosis (70~yr as control) | |||
| 15 yr~ | 0.105 | 0.045~0.249 | <0.001 |
| 25 yr~ | 0.153 | 0.087~0.270 | <0.001 |
| 40 yr~ | 0.263 | 0.158~0.439 | <0.001 |
| 60 yr~ | 0.523 | 0.298~0.917 | 0.024 |
| CD4 counts at the end (350~cells/ul as control) | |||
| 6Not detected* | 234.469 | 110.029~499.646 | <0.001 |
| <50 | 83.915 | 47.464~148.358 | <0.001 |
| 50~ | 18.081 | 11.039~29.615 | <0.001 |
| 200~ | 4.557 | 2.793~7.436 | <0.001 |
| ART (No as control) | |||
| Yes | 0.269 | 0.153~0.473 | <0.001 |
| Year of diagnosis (After 2017 as control) | |||
| Before 2007 | 3.285 | 1.081~9.988 | 0.036 |
| 2007–2016 | 6.971 | 4.793~10.139 | <0.001 |
These patients died before CD4 count testing due to severe illness or non-compliance.
OD – odds ratio; CI – confidence interval.
ITS Analysis of HIV/AIDS-Related Related Rate from 1999 to 2023
Linear assessment and autocorrelation analysis were conducted on the data. In the regression analysis of HIV/AIDS-related fatality rate from 1999 to 2023, the BG statistic was 10.272, indicating the presence of autocorrelation. Therefore, the Prais-Winsten estimation method in generalized least squares was used for correction, leading to the construction of the interrupted linear regression equation:
The initial HIV/AIDS-related fatality rate at the beginning of the observation period was 40.23%. Before the implementation of free ART, the slope (β1) of the HIV/AIDS-related fatality rate was 1.79, indicating an upward trend, but the difference was not statistically significant (t=0.49, P=0.628). In the year when free ART was implemented (2006), the fatality rate decreased by 38.60% (β2), and the difference was statistically significant (t=−2.67, P=0.015). During the period of free ART implementation from 2006 to 2015, the slope of the fatality rate was β1+β3=−1.1%, showing a decreasing trend, but the difference was not statistically significant (t=−0.80, P=0.434). In the year when the “early treatment” strategy was implemented in 2016, the fatality rate increased by 1.29% (β4), but the difference was not statistically significant (t=2.03, P=0.056). During the period of “early treatment” strategy implementation from 2016 to 2023, the slope of the fatality rate was β1+β3+β5=−0.33%, indicating a decreasing trend, and the difference was statistically significant (t=5.72, P<0.001). See Table 3 and Figure 2.
Table 3.
ITS regression model parameter values for HIV/AIDS-related fatality rate in Lu’an City, 1999–2023.
| Parameters | Estimates | t value | P value |
|---|---|---|---|
| β0 | 40.23 | 3.20 | 0.005 |
| β1 | 1.79 | 0.49 | 0.628 |
| β2 | −38.60 | −2.67 | 0.015 |
| β3 | −2.89 | −0.80 | 0.434 |
| β4 | 1.29 | 2.03 | 0.056 |
| β5 | 0.77 | 5.72 | 0.000 |
Figure 2.
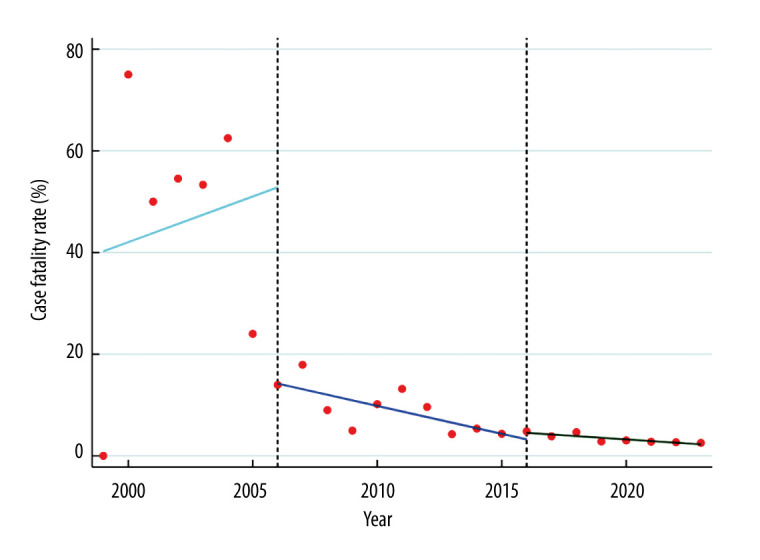
HIV/AIDS-related fatality rate in Lu’an City, 1999–2023. Models were based on interrupted time series (ITS) analysis. The period of no antiretroviral therapy (ART) was 1999–2005, the period of threshold-entry ART was 2007–2015, and the period of “early ART” was 2017–2023. The authors utilized Stata 17.0 software (StataCorp Inc., Texas, USA) to generate all figures.
Discussion
The survey revealed that the cumulative fatality rate of HIV/AIDS-related diseases in Lu’an City was 16.83%. However, among patients receiving antiretroviral therapy (ART), the cumulative fatality rate was notably lower, at 10.10%, resembling the findings of a study conducted in Liangshan Prefecture, Sichuan Province [22]. Notably, the total fatality rate was 3.80 per 100 person-years, significantly lower than our previous survey result of 8.06 per 100 person-years in 2014 [19]. The annual fatality rate declined from 75.00% in the initial period to 2.54 per 100 person-years in 2023,which was lower than the results of previous studies in China [12,18]. This decline underscores the advancement in HIV/AIDS prevention and control efforts, particularly with the implementation of the “early treatment” strategy, enabling most patients to receive timely treatment, thereby reducing the likelihood of HIV/AIDS-related diseases and subsequent fatality rates. Joinpoint regression analysis unveiled a general decline in the HIV/AIDS-related fatality rate from 1999 to 2023, characterized by a faster decline before 2009 and a slower decline thereafter. This progress is attributed to the gradual expansion of testing and treatment measures in China.
This study revealed that, except for the age group under 15 years, the older the age at diagnosis, the higher the fatality rate, consistent with findings from numerous reports [19,23–26]. A study from Qingdao University indicated that the risk of HIV/AIDS-related death in patients over 50 years old is more than twice that of the 15–50 age group [27]. It is believed that as age increases, the body’s immune capacity gradually decreases, further compounded by HIV’s primary attack on the body’s immune system, thereby escalating the susceptibility of elderly patients to HIV/AIDS-related diseases and subsequent mortality. Our prior research suggested that compared to the elderly, young individuals exhibit a stronger awareness of HIV testing, coupled with more opportunities for early diagnosis through premarital, prenatal, and antenatal check-ups, facilitating prompt treatment initiation [9]. Studies have underscored that elderly individuals exhibit poorer medication adherence compared to their younger counterparts [28], highlighting the crucial role of treatment adherence in influencing treatment outcomes [29]. Some studies have found that younger children at the time of diagnosis have a higher risk of death than older children. It is believed that the immunity level of younger children is lower, and the disease progresses faster after HIV infection, thus increasing the risk of death [30,31]. This survey also found that the high HIV/AIDS-related fatality rate in children under 15 years old may be related to the low immune level of children in this age group.
Since HIV primarily targets CD4+ T lymphocytes in the body, the count of these cells reflects the patient’s immune status and disease progression. A lower count indicates weaker immunity and a longer disease course. Most scholars believe that the baseline CD4+ T lymphocyte count of patients influences death risk, with a lower count indicating a higher risk of death [22,32–34], consistent with our earlier findings [19]. However, our study results indicate that although the univariate analysis found higher fatality rates in patients with lower CD4+ T lymphocyte counts at diagnosis, the multivariate analysis showed that the CD4+ T lymphocyte count at diagnosis did not influence HIV/AIDS-related disease death, but the last CD4+ T lymphocyte count did. Our analysis suggests that patients with lower CD4+ T lymphocyte counts at diagnosis pay great attention to their condition and adhere better to treatment. Some patients with higher CD4+ T lymphocyte count at diagnosis, due to milder symptoms, may gradually decrease their awareness of medication’s importance, reducing treatment adherence and leading to drug resistance development, and drug-resistant cases showed a 4.25 times higher death risk [35]. The above situation may reduce the impact of CD4+T lymphocyte count level at diagnosis on patient death. Additionally, due to changing criteria for CD4+ T lymphocyte counts for ART selection, some patients diagnosed before 2016, despite higher CD4+ T lymphocyte counts at diagnosis, did not receive timely treatment because they did not meet the treatment standards at that time, affecting treatment outcome. Another study found that HIV/AIDS patients with CD4+ T lymphocyte counts above 500 cells/μL at diagnosis who immediately received ART had a significantly lower fatality rate of 1.04/100 person-years compared to those who delayed treatment [36]. These findings emphasize the importance of “early treatment” strategies in reducing death risk and HIV/AIDS-related diseases, improving prognosis, and highlighting the need for healthcare providers to stress medication adherence to patients, ultimately improving treatment adherence and reducing fatality rates.
The ITS analysis revealed no significant change in HIV/AIDS-related fatality rates before 2006. However, after the introduction of free ART in 2006, although there was no significant long-term change in fatality rate trends, the short-term effect was notable, indicating the effectiveness of the free ART strategy in AIDS prevention and control. A study by the Chinese Center for Disease Control and Prevention showed that after the implementation of the free “one care” policy measures, including free HIV testing and treatment, by the Chinese government in 2004, the overall HIV/AIDS-related fatality rate declined. Free ART was believed to have improved patient health status and prognosis, while free HIV testing and screening enabled early detection and treatment of many HIV/AIDS patients, reducing death risk [20]. A cohort study from the Netherlands found a significantly lower fatality rate in patients who underwent multiple tests before their first positive result compared to those whose first test was positive [37]. The ITS analysis also indicated a significant long-term downward trend in HIV/AIDS-related fatality rates after the implementation of the “early treatment” strategy in 2016.
The results of both univariate and multivariate analyses in this study revealed a gradual decrease in fatality rates over time since diagnosis, with the years before 2007 and during 2007–2016 identified as risk factors for fatality. These findings, corroborated by 2 different analytical methods, confirm the effectiveness of the “early treatment” strategy in reducing HIV/AIDS-related fatality rates. Studies in China have shown that after the implementation of this strategy, the rate of initiating ART within 30 days of diagnosis of new cases increased by 12.6% [38], highlighting the importance of rapid ART initiation in preventing HIV/AIDS deaths [36,39]. Similarly, a study in Uganda found that after the implementation of universal treatment for HIV-infected individuals, the 6-month fatality rate decreased by 1.6%, continuing to decrease by 0.1% thereafter [40]. These findings collectively demonstrate the efficacy of the “early treatment” strategy in reducing HIV/AIDS-related fatality rates.
This study spans an important time period from 1999 to 2023, providing insights into the changing trend and influencing factors of HIV/AIDS-related fatality rates in Lu’an City. It also evaluates the impact of various ART strategies on fatality rates, a topic that is not widely reported in the literature in China. The rapid decline observed in HIV/AIDS-related fatality rates following expanded testing and the provision of free ART, as well as the sustained downward trend after the implementation of the “early treatment” strategy, underscores the effectiveness of these prevention and control strategies, which should be continued. However, the study has limitations. First, due to evolving criteria for selecting ART based on CD4+ T lymphocyte counts, the levels of CD4+ T lymphocytes at diagnosis may not fully reflect baseline levels before treatment. Second, utilizing ITS analysis to assess the impact of ART strategies on fatality rates without a control group may yield stable results, but other confounding variables could indirectly affect the outcome variable, making it challenging to establish causal relationships between changes in fatality rates and ART strategies. Third, information on medication adherence was not collected for patients receiving ART, and these factors could also have influenced the findings.
Conclusions
The overall HIV/AIDS-related fatality rate in Lu’an City is decreasing, with children under 15 years old and older patients facing a higher risk of death. Free ART, and particularly the implementation of the “early treatment” strategy, were the primary drivers behind this decline in HIV/AIDS-related fatality rates.
Acknowledgements
The authors acknowledge the cooperation of HIV/AIDS prevention and control staff from Lu’an Institutions for Disease Control and Prevention and all the medical staff from the department of infectious diseases of Lu’an People’s Hospital during data collection.
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity: All figures submitted have been created by authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: None declared
References
- 1.Pu XY, Zhong ZG, Zhu LY, et al. Age-period-cohort model analysis of AIDS mortality trend in China from 2006 to 2020. Modern Prevent Medicine, 2023;50(2):222–26. [Google Scholar]
- 2.The path that ends AIDS: UNAIDS Global AIDS Update 2023. Geneva: Joint United Nations Programme on HIV/AIDS; 2023. License: CC BY-NC-SA 3.0 IGO. Available from: https://thepath.unaids.org/wp-content/themes/unaids2023/assets/files/2023_report.pdf. [Google Scholar]
- 3.Eggleton JS, Nagalli S. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2024. Highly active antiretroviral therapy (HAART) [Updated 2023 Jul 3] Available from: https://www.ncbi.nlm.nih.gov/books/NBK554533/ [PubMed] [Google Scholar]
- 4.Kemnic TR, Gulick PG. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2024. HIV antiretroviral therapy. [Updated 2022 Sep 20] Available from: https://www.ncbi.nlm.nih.gov/books/NBK513308/ [PubMed] [Google Scholar]
- 5.Song MM, Zhang NN, Liu XQ, et al. Research progress of AIDS epidemic and antiretroviral treatment in China. Preventive Medicine Tribune. 2023;29(8):637–40. [Google Scholar]
- 6.Liang YM, Chen SJ, Wang FR, et al. Analysis on the efficacy of continuous antiviral treatment for AIDS. Journal of Guangdong Medical University. 2023;41(6):656–59. [Google Scholar]
- 7.Ma L, Zhang YL, Wang W, et al. Comparison of epidemic characteristics and analysis of survival time between patients who have not received antiviral treatment and those who have received antiviral treatment in Hebei Province. Journal of Medical Pest Control. 2022;38(1):9–13. [Google Scholar]
- 8.Li CF, Yang X, Yang XX, et al. Effects and influencing factors of antiretroviral therapy among HIV/AIDS patients of different ages in Zhengzhou. Chinese Journal of AIDS STD. 2023;29(12):1285–89. [Google Scholar]
- 9.Ma G, Chen H, Chen J, et al. HIV transmission between spouses living in Lu’an city, Anhui province, China: A longitudinal study. Epidemiol Infect. 2019;147:e205. doi: 10.1017/S095026881900089X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gan XM, Zhao DC, Zhao Y, et al. Progress on national antiretroviral therapy treatment program during 2003–2021 in China. Chinese Journal of AIDS STD. 2022;28(06):642–46. [Google Scholar]
- 11.Zhao Y, Gan XM, Zhao DC, et al. Thoughts on progress of HIV/AIDS antiretroviral treatment in China and promoting high-quality development. Chinese Journal of AIDS STD. 2023;29:619–22. [Google Scholar]
- 12.Zhao Y, Wei L, Dou Z, et al. Changing mortality and patterns of death causes in HIV infected patients – China, 2013–2022. China CDC Wkly. 2023;5(48):1073–78. doi: 10.46234/ccdcw2023.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV. Geneva: World Health Organization; Sep, 2015. [PubMed] [Google Scholar]
- 14.Chamie G, Clark TD, Kabami J, et al. A hybrid mobile approach for population-wide HIV testing in rural east Africa: An observational study. Lancet HIV. 2016;3(3):e111–e19. doi: 10.1016/S2352-3018(15)00251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iwuji CC, Orne-Gliemann J, Larmarange J, et al. Universal test and treat and the HIV epidemic in rural South Africa: A phase 4, open-label, community cluster randomised trial. Lancet HIV. 2018;5(3):e116–e25. doi: 10.1016/S2352-3018(17)30205-9. [DOI] [PubMed] [Google Scholar]
- 16.Makhema J, Wirth KE, Pretorius Holme M, et al. Universal testing, expanded treatment, and incidence of HIV infection in Botswana. N Engl J Med. 2019;381(3):230–42. doi: 10.1056/NEJMoa1812281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hao Y, Chen QF, Han MJ, et al. Initiation and development of free HIV/AIDS antiretroviral treatment in China – exploring a path of antiviral treatment with Chinese characteristics. Chinese Journal of AIDS STD. 2022;28(01):1–5. [Google Scholar]
- 18.Xu JJ, Han MJ, Jiang YJ, et al. Prevention and control of HIV/AIDS in China: Lessons from the past three decades. Chin Med J (Engl) 2021;134(23):2799–809. doi: 10.1097/CM9.0000000000001842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma GY, Ma T, Huang J, et al. Survival of people living with HIV/AIDS and related factors Lu’an, Anhui. Disease Surveillance. 2014;29(09):716–20. [Google Scholar]
- 20.Zhang HX, Han MJ, Zhou Y, et al. Interrupted time series analysis for influence on HIV related fatality of implementation of ‘Four Free Services One Care’ policy in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(03):406–11. doi: 10.3760/cma.j.issn.0254-6450.2020.03.024. [DOI] [PubMed] [Google Scholar]
- 21.Zhang F, Wagner AK, Soumerai SB, et al. Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J Clin Epidemiol. 2009;62(2):143–48. doi: 10.1016/j.jclinepi.2008.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang X, Xu JL, Jike KCN, et al. Epidemiological analysis of the deaths with antiretroviral treatment among adult HIV/AIDS patients in Liangshan Yi Autonomous Prefecture from 2005 to 2015. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40(9):1116–19. doi: 10.3760/cma.j.issn.0254-6450.2019.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Dai SY, Liu AW, Shen YL, et al. Influencing factors on the death of HIV/AIDS patients receiving antiretroviral therapy in Anhui Province. Chinese Journal of Disease Control & Prevention. 2022;26(12):1379–83. [Google Scholar]
- 24.Zhou Y, Yang Z, Liu M, et al. Independent risk factors for deaths due to AIDS in Chongqing, China: Does age matter? Front Med (Lausanne) 2021;7:586390. doi: 10.3389/fmed.2020.586390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carriquiry G, Giganti MJ, Castilho JL, et al. Virologic failure and mortality in older ART initiators in a multisite Latin American and Caribbean cohort. J Int AIDS Soc. 2018;21(3):e25088. doi: 10.1002/jia2.25088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bijker R, Kiertiburanakul S, Kumarasamy N, et al. Survival after long-term ART exposure: Findings from an Asian patient population retained in care beyond 5 years on ART. Antivir Ther. 2020;25(3):131–42. doi: 10.3851/IMP3358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li YH. Master’s thesis. Qinghai University; 2022. Research of the effects of HIV/AIDS antiretroviral treatment and related influencing factors in Qinghai province. [Google Scholar]
- 28.Zhen GZ, Yang X, Liu XJ, et al. Investigation and analysis on the medication compliance of HIV/AIDS patients receiving antiretroviral therapy in Xi’an. South China Journal of Preventive Medicine. 2023;49(4):514–17. [Google Scholar]
- 29.Biney IJK, Kyei KA, Ganu VJ, et al. Antiretroviral therapy adherence and viral suppression among HIV-infected adolescents and young adults at a tertiary hospital in Ghana. Afr J AIDS Res. 2021;20(4):270–76. doi: 10.2989/16085906.2021.1998783. [DOI] [PubMed] [Google Scholar]
- 30.Yin H, Ma Y, Yang X, et al. Survival analysis on HIV-infected children aged 14 years old and younger in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(6):850–55. doi: 10.3760/cma.j.cn112338-20191129-00844. [DOI] [PubMed] [Google Scholar]
- 31.Dai SY, Liu AW, Jin L, et al. Survival time and related factors among child HIV/AIDS patients in Anhui province. Chinese Journal of Public Health. 2022;38(12):1588–92. [Google Scholar]
- 32.Xie RQ, Li X, Zhao CQ, et al. Mortality analysis among HIV/AIDS cases in Huangshi, Hubei, 2000–2019. China Tropical Medicine. 2021;21(06):588–93. [Google Scholar]
- 33.Zhang N, Zhu XY, Wang GY, et al. Survival status and influencing factors of HIV/AIDS on highly active anti-retroviral therapy in Shandong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40(1):74–78. doi: 10.3760/cma.j.issn.0254-6450.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 34.Chen Y, Song XT, Yao YM, et al. Mortality and influencing factors on injecting drug users with HIV/AIDS in Guizhou province, 1996–2015. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40(7):765–69. doi: 10.3760/cma.j.issn.0254-6450.2019.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Zhang T, Liao L, Shao Y, et al. Relationship between drug resistance and death in HIV-infected patients receiving antiretroviral therapy – 7 PLADs, China, 2010–2019. China CDC Wkly. 2021;3(14):291–97. doi: 10.46234/ccdcw2021.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao Y, Wu Z, McGoogan JM, et al. Immediate antiretroviral therapy decreases mortality among patients with high CD4 counts in China: A nationwide, retrospective cohort study. Clin Infect Dis. 2018;66(5):727–34. doi: 10.1093/cid/cix878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gras L, van Sighem A, Bezemer D, et al. Lower mortality and earlier start of combination antiretroviral therapy in patients tested repeatedly for HIV than in those with a positive first test. AIDS. 2011;25(6):813–18. doi: 10.1097/QAD.0b013e3283454cd7. [DOI] [PubMed] [Google Scholar]
- 38.Wu X, Wu G, Ma P, et al. Immediate and long-term outcomes after treat-all among people living with HIV in China: An interrupted time series analysis. Infect Dis Poverty. 2023;12(1):73. doi: 10.1186/s40249-023-01119-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jin YC, Qin QQ, Cai C, et al. Characteristics and risk factors of early death among newly diagnosed HIV/AIDS in China, 2011–2020. Chinese Journal of Disease Control & Prevention. 2023;27(6):673–77. [Google Scholar]
- 40.Mugenyi L, Nanfuka M, Byawaka J, et al. Effect of universal test and treat on retention and mortality among people living with HIV-infection in Uganda: An interrupted time series analysis. PLoS One. 2022;17(5):e0268226. doi: 10.1371/journal.pone.0268226. [DOI] [PMC free article] [PubMed] [Google Scholar]


