Abstract
Background
Atrial fibrillation (AF) is associated with an increased risk of hospital admission, but few data on reasons for hospitalization and on the role of anti-arrhythmic drugs are available.
Objectives
The purpose of this study was to investigate the incidence rate and factors associated with all-cause, cardiovascular, and AF-related hospitalizations.
Methods
Prospective ongoing ATHERO-AF (Atherosclerosis in Atrial Fibrillation) cohort study enrolling AF patients on oral anticoagulants. Primary end points were all-cause, cardiovascular, and AF-related hospitalization, the latter defined as AF recurrences for paroxysmal AF and high-rate symptomatic AF episodes for persistent/permanent AF patients.
Results
2,782 patients were included (43.5% female; mean age was 74.6 ± 9.1 years). During a mean follow-up of 31 ± 26.8 months, 1,205 (12.1%/year) all-cause, 533 cardiac (5.7%/year), and 180 (2.0%/year) AF-related hospitalizations occurred. Predictors of AF-related hospitalizations were the use of flecainide/propafenone in both paroxysmal and persistent/permanent AF patients (HR: 1.861; 95% CI: 1.116 to 3.101 and 1.947; 95% CI: 1.069 to 3.548, respectively). Amiodarone (HR: 3.012; 95% CI: 1.835-4.943), verapamil/diltiazem (HR: 2.067; 95% CI: 1.117-3.825), and cancer (HR: 1.802; 95% CI: 1.057-3.070) but not beta-blockers and digoxin were associated with an increased risk of AF-related hospitalizations in persistent/permanent AF patients.
Conclusions
Elderly AF patients frequently undergo hospitalizations for both cardiovascular and noncardiovascular causes. The use of anti-arrhythmic drugs was associated with an increased risk of AF-related hospitalization suggesting a scarce effect of these drugs in preventing AF episodes. Therefore, their use should be carefully considered and reserved for symptomatic patients with frequent AF recurrences.
Key words: amiodarone, antiarrhythmic, atrial fibrillation, digoxin, flecainide, hospitalization
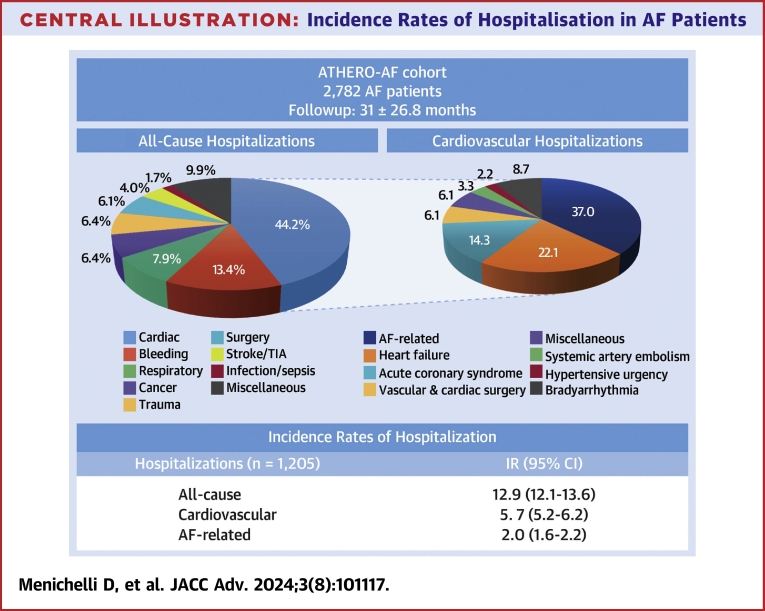
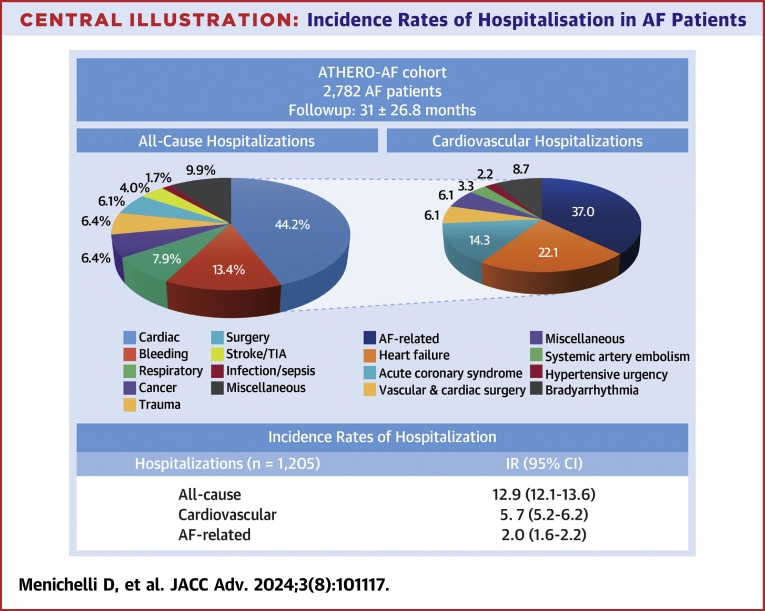
Central Illustration
Atrial fibrillation (AF) is a common arrhythmic disease with an increased risk of mortality, disability, and hospitalizations.1,2 Hospitalizations occur more frequently in patients with AF compared to patients not affected by this arrhythmia. A nationwide retrospective cohort study including 4,602,264 hospital admissions3 showed a higher risk of both cardiovascular and noncardiovascular hospitalization at 6 months in AF compared to non-AF patients (28.4% vs 1.8% and 33.3% vs 9.7%, respectively).3 However, the study did not report reasons for hospitalization, as well as data on anticoagulation status of patients, and was conducted before the introduction of direct oral anticoagulants (DOACs) (1997-2009).
Hospital admission represents a relevant cost for health care system considering the high prevalence and incidence of the disease.4,5 These costs could be mitigated with an integrated care approach to AF management.5,6 A substudy of the Euro Heart Survey of AF performed on 2,995 patients from 5 countries7 showed that inpatient care and interventional procedures were the main drivers of costs, accounting for ≥70% of the total annual costs.7 Furthermore, a systematic review and meta-analysis performed on 37 studies showed that hospitalizations represented 50% to 70% of annual direct costs in AF patients in the United Kingdom.8
Nevertheless, few real-world prospective data are available about the incidence and characteristics of patients undergoing hospitalizations, especially in Western countries. In addition, there is still conflicting evidence on the effectiveness of anti-arrhythmic drugs for AF recurrences prevention.
Based on this, we investigated in the prospective ATHERO-AF (Atherosclerosis in Atrial Fibrillation) cohort the causes of hospitalization and the clinical characteristics of AF patients undergoing hospital admission focusing on predictors of cardiac- and AF-related hospitalizations, including anti-arrhythmic drugs.
Methods
Study cohort
We analyzed data of patients from the prospective ongoing observational ATHERO-AF cohort at Sapienza University of Rome. All patients were treated with oral anticoagulants, either vitamin K antagonists (VKAs) or DOACs. During the first clinical examination, a completed personal medical history was collected, including drug therapy and comorbidities. The choice of starting DOAC or VKA was at physician discretion and based on an informed shared decision with patients.
All patients signed an informed written consent at study entry. The study was approved by the local ethic committee of Sapienza University (No. 1306/2007) and it was conducted according to the Declaration of Helsinki.
Follow-up and definition of primary outcomes
Follow-up visits were performed by periodic clinical evaluations or by telephone calls if patients missed the visit on site. The primary end point was all-cause hospitalization, defined as every admission to the emergency department and/or hospital admission. Hospitalization was then classified as cardiac, respiratory, cancer, trauma, bleeding, cerebrovascular, infection, or surgery related. Among cardiac hospitalizations, we identified those related to (non-AF) arrhythmias, acute coronary syndromes, heart failure (HF), systemic embolism, hypertensive urgency, vascular/cardiac surgery, and AF-related. AF-related hospitalization was defined either as recurrence of AF in patients with paroxysmal AF or high ventricular rate symptomatic AF episodes for persistent/permanent AF patients.
Data on hospitalization were documented by clinical reports and discharge letters. For the analysis it was used only the first event that occurred in time and the confirmation of the primary event was made by a blinded commission which did not participate in patient recruitment and was not aware of the characteristics of the enrolled patients.
Statistical analysis
Categorical variables were reported as counts (percentage), and Pearson chi-squared test was used to compare proportions. Continuous variables were expressed as mean ± SD or median (IQR), depending on their distribution, which was assessed by the Kolmogorov-Smirnov test. Appropriate nonparametric tests (Mann-Whitney U test and Spearman rank correlation test) were employed for non-normal variables. Continuous variables with non-normal distribution were log-transformed for multivariable analysis.
We estimated the incidence of all-cause, cardiac- and AF-related hospitalizations and described the single causes of hospital admission. We then divided the cohort in two groups according to hospitalization status to describe clinical characteristics.
We performed separate survival models of multivariable Cox proportional hazards regression analysis using as covariates cardiovascular risk factors (age, sex, arterial hypertension, diabetes, previous myocardial infarction, chronic obstructive pulmonary disease [COPD], cancer, HF) and cardiovascular therapy (angiotensin-converting enzyme inhibitors/angiotensin receptor blocker [ACEI/ARB], nitrates, Vaughan Williams class Ic antiarrhythmics such as flecainide and propafenone, amiodarone, beta-blockers, calcium-channel blockers, digoxin, anticoagulants, and lipid-lowering therapy). We used the composite CHA2DS2-VASc score instead of single variables due to the relatively small number of events for the outcome of AF-related hospitalizations.
All tests were 2-tailed and the analyses were performed using computer software packages (SPSS-25.0, IBM). Values of P < 0.05 were considered as statistically significant.
Results
All-cause hospitalizations
We enrolled 2,782 patients with non-valvular AF, of whom 43.5% were women and a mean age of 74.6 ± 9.1 years (Supplemental Table 1). During a mean follow-up of 31 ± 26.8 months, 1,205 all-cause hospitalizations occurred (incidence rate [IR]: 12.9%/year; 95% CI: 12.1%-13.6%). Patients hospitalized were more frequently affected by arterial hypertension, diabetes, previous myocardial infarction, COPD, HF, history of cancer, and chronic kidney disease, having a higher mean of CHA2DS2-VASc and HAS-BLED score compared to the ones without hospitalizations (Supplemental Table 1). Furthermore, patients with all-cause hospitalization were more frequently treated with VKAs, ACE-I/ARBs, calcium channel blockers, nitrates, anti-arrhythmic drugs, and digoxin (Supplemental Table 1).
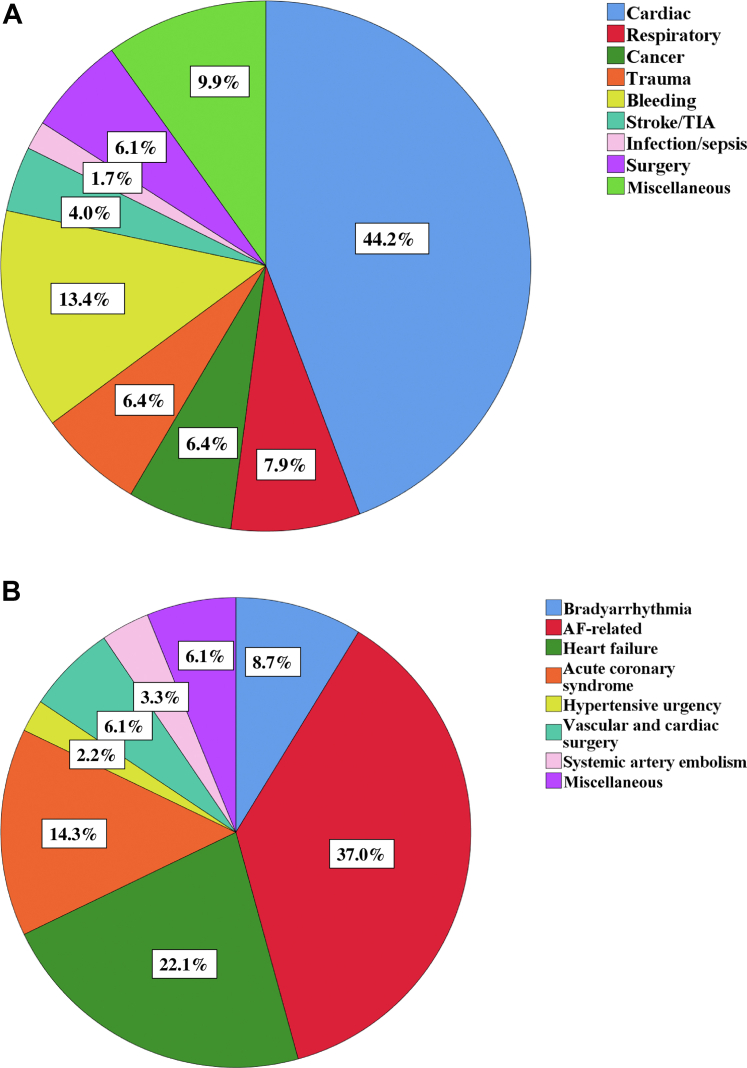
The most common causes of hospitalizations were for cardiac (44.2%), bleeding (13.4%), respiratory (7.9%), and stroke/transient ischemic attack causes (6.4%) (Figure 1A).
Figure 1.
Rate and Type of Hospitalization
Rate and type of hospitalization: all-cause (A) and cardiac (B).
Cardiac hospitalizations
Among hospitalizations, cardiac causes represented 1 out of 2 (IR: 5.7%/year; 95% CI: 5.2%-6.2%), and the most common causes (Figure 1B) were AF-related with 180 events (IR: 2.0%/year; 95% CI: 1.6%-2.2%) and HF-related with 119 events (IR: 1.3%/year; 95% CI: 1.1%-1.5%).
Patients with cardiac hospitalization (n = 533) were more likely to be affected by arterial hypertension, previous myocardial infarction, COPD, history of cancer, HF with a higher mean of CHA2DS2-VASc and HAS-BLED scores compared to those without hospitalizations (Table 1). Patients with cardiac hospitalization were more frequently treated at baseline with VKAs, lipid-lowering therapy, ACEI/ARBs, nitrates, anti-arrhythmic drugs, especially amiodarone, and digoxin compared to the ones who were not hospitalized (Table 1).
Table 1.
Population Characteristics According to Cardiovascular Hospitalization Occurrence
| Total Cohort (n = 2,782) | No Hospitalization (n = 1,577) | Cardiac Hospitalization (n = 533) | P Value | |
|---|---|---|---|---|
| Women | 43.5 | 43.9 | 41.1 | 0.288 |
| Age, y | 74.6 ± 9.1 | 74.7 ± 9.4 | 73.7 ± 8.7 | 0.035 |
| Permanent/persistent AF | 62.8 | 62.8 | 60.4 | 0.353 |
| Arterial hypertension | 86.7 | 85.5 | 90.1 | 0.006 |
| Diabetes | 21.3 | 19.6 | 22.9 | 0.106 |
| Previous stroke/TIA | 15.1 | 14.7 | 14.3 | 0.887 |
| Previous myocardial infarction | 17.1 | 15.5 | 20.1 | 0.019 |
| COPD | 15.1 | 12.5 | 18.1 | 0.002 |
| Cancer | 16.4 | 12.8 | 18.2 | 0.003 |
| Heart failure | 14.1 | 12.6 | 21.2 | <0.001 |
| CKD | 32.9 | 31.5 | 34.0 | 0.370 |
| CHA2DS2-VASc | 3.6 ± 1.5 | 3.5 ± 1.5 | 3.7 ± 1.6 | 0.015 |
| HAS-BLED | 2.3 ± 0.9 | 2.2 ± 0.8 | 2.4 ± 0.9 | <0.001 |
| Therapy | ||||
| DOAC | 33.1 | 39.1 | 20.6 | <0.001 |
| Lipid-lowering therapy | 39.3 | 38.2 | 43.7 | 0.024 |
| ACEI/ARBs | 62.7 | 59.8 | 67.5 | 0.002 |
| Beta-blockers | 44.8 | 45.3 | 46.9 | 0.580 |
| Calcium-channel blockers | 27.7 | 26.1 | 27.4 | 0.532 |
| Verapamil/diltiazem | 9.8 | 9.5 | 9.6 | 0.948 |
| Nitrates | 9.8 | 7.9 | 13.1 | 0.001 |
| Antiarrhythmics | 27.6 | 25.8 | 35.6 | <0.001 |
| Class Ic | 13.4 | 12.9 | 15.6 | 0.125 |
| Amiodarone | 14.4 | 13.4 | 20.5 | <0.001 |
| Digoxin | 13.6 | 12.5 | 17.4 | 0.004 |
| Hypoglycemic drugs | 16.6 | 15.2 | 17.6 | 0.193 |
| Diuretics | 43.6 | 42.7 | 46.3 | 0.157 |
| Proton pump inhibitor | 44.8 | 45.8 | 46.5 | 0.763 |
Values are % or mean ± SD.
ACEI/ARB = angiotensin-converting enzyme inhibitors/angiotensin receptor blockers; AF = atrial fibrillation; CKD = chronic kidney disease; COPD = chronic obstructive pulmonary disease; DOAC = direct oral anticoagulant; TIA = transient ischemic attack.
At multivariable Cox regression analysis (Table 2), cardiac hospitalization is directly associated with COPD (HR: 1.396; 95% CI: 1.110-1.757; P = 0.004), HF (HR: 1.364; 95% CI: 1.076-1.729; P = 0.010), and with the use of antiarrhythmics, both Vaughan Williams Class Ic agents, ie, propafenone and flecainide (HR: 1.385; 95% CI: 1.074-1.789; P = 0.012) and amiodarone (HR: 1.495; 95% CI: 1.197-1.868; P < 0.001), while the use of DOACs was inversely associated (HR: 0.586; 95% CI: 0.468-0.733; P < 0.001). A summary of hospitalization rates and causes were reported in the (Central Illustration).
Table 2.
Multivariable Cox Proportional Hazards Regression Analysis of Cardiac Hospitalization
| 95% CI |
||||
|---|---|---|---|---|
| HR | Low | High | P Value | |
| Age | 1.006 | 0.996 | 1.017 | 0.255 |
| Female | 0.936 | 0.781 | 1.123 | 0.478 |
| Arterial hypertension | 1.206 | 0.875 | 1.661 | 0.253 |
| Diabetes | 1.036 | 0.837 | 1.281 | 0.746 |
| Previous myocardial infarction | 1.189 | 0.926 | 1.527 | 0.174 |
| COPD | 1.396 | 1.110 | 1.757 | 0.004 |
| Cancer | 1.194 | 0.953 | 1.497 | 0.124 |
| Heart failure | 1.364 | 1.076 | 1.729 | 0.010 |
| ACEI/ARB | 1.002 | 0.817 | 1.229 | 0.984 |
| Nitrates | 0.997 | 0.757 | 1.314 | 0.983 |
| Class Ic antiarrhythmics | 1.386 | 1.074 | 1.789 | 0.012 |
| Amiodarone | 1.495 | 1.197 | 1.868 | <0.001 |
| Beta-blockers | 1.033 | 0.853 | 1.250 | 0.742 |
| Verapamil/diltiazem | 0.990 | 0.724 | 1.353 | 0.949 |
| Digoxin | 1,243 | 0.977 | 1.581 | 0.076 |
| DOAC vs VKA | 0.586 | 0.468 | 0.733 | <0.001 |
| Lipid-lowering therapy | 1.087 | 0.897 | 1.317 | 0.396 |
VKA = vitamin K antagonist; other abbreviations as in Table 1.
Central Illustration.
Incidence Rates of Hospitalisation in AF Patients
AF-related hospitalizations
Among cardiac hospitalizations, AF-related hospitalization (n = 180; IR: 2%/year; 95% CI: 1.6%-2.2%) was the most frequent cause. Patients with AF-related hospitalization were younger (71.5 ± 8.5 vs 74.7 ± 9.4; P < 0.001), with higher prevalence of cancer history, with lower rate of permanent/persistent AF, and lower mean CHA2DS2-VASc compared to AF patients without hospitalizations (Table 3). Furthermore, patients with AF-related hospitalizations were treated more commonly with ACE-I/ARBs, VKAs, and antiarrhythmics both Ic Vaughan Williams class and amiodarone.
Table 3.
Population Characteristics According to AF-Related Hospitalization
| No Hospitalization (n = 1,577) | AF-Related Hospitalization (n = 180) | P Value | |
|---|---|---|---|
| Women | 43.9 | 42.8 | 0.812 |
| Age, y | 74.7 ± 9.4 | 71.5 ± 8.5 | <0.001 |
| Permanent/persistent AF | 62.8 | 53.3 | 0.014 |
| Arterial hypertension | 85.5 | 88.9 | 0.210 |
| Diabetes | 19.6 | 17.2 | 0.455 |
| Previous stroke/TIA | 14.7 | 12.8 | 0.509 |
| Previous myocardial infarction | 15.5 | 11.7 | 0.167 |
| COPD | 12.5 | 13.3 | 0.785 |
| Cancer | 12.8 | 18.9 | 0.024 |
| Heart failure | 12.6 | 11.1 | 0.568 |
| CKD | 31.5 | 31.1 | 0.893 |
| CHA2DS2-VASc | 3.5 ± 1.5 | 3.2 ± 1.6 | 0.013 |
| HAS-BLED | 2.2 ± 0.8 | 2.2 ± 0.9 | 0.932 |
| Therapy | |||
| DOAC | 39.1 | 16.7 | <0.001 |
| Lipid-lowering therapy | 38.2 | 45.0 | 0.073 |
| ACEI/ARBs | 59.8 | 68.3 | 0.027 |
| Beta-blockers | 45.3 | 42.8 | 0.493 |
| Calcium-channel blockers | 26.1 | 27.2 | 0.727 |
| Verapamil/diltiazem | 9.5 | 13.3 | 0.101 |
| Nitrates | 7.9 | 8.3 | 0.876 |
| Antiarrhythmics | 25.8 | 43.9 | <0.001 |
| Class Ic | 12.9 | 22.8 | <0.001 |
| Amiodarone | 13.4 | 22.2 | <0.001 |
| Digoxin | 12.5 | 12.2 | 0.915 |
| Hypoglycemic drugs | 15.2 | 15.0 | 0.951 |
| Diuretics | 42.7 | 39.4 | 0.403 |
| Proton pump inhibitor | 45.8 | 45.0 | 0.844 |
Values are % or mean ± SD.
Abbreviations as in Table 1.
We performed a multivariable Cox regression analysis (Table 4) investigating whether paroxysmal and persistent/permanent pattern of AF could have different characteristic of hospitalization. Eighty-four AF-related hospitalizations occurred in paroxysmal AF patients (Table 4) and they were directly associated with Vaughan Williams Class Ic antiarrhythmics (HR: 1.861; 95% CI: 1.116-3.101; P = 0.017), not associated with amiodarone (HR: 1.045; 95% CI: 0.584-1.872; P = 0.881) and inversely associated with DOAC use (HR: 0.352; 95% CI: 0.206-0.602; P < 0.001). Ninety-six AF-related hospitalizations occurred in persistent/permanent AF patients (Table 4). In these patients, amiodarone (HR: 3.012; 95% CI: 1.835-4.943; P < 0.001), Vaughan Williams Class Ic antiarrhythmics (HR: 1.947; 95% CI: 10.69-3.548; P = 0.029), verapamil, and diltiazem use (HR: 2.067; 95% CI: 1.117-3.825; P = 0.021) were directly associated with AF-related hospitalizations, while DOAC use was inversely associated with them (HR: 0.318; 95% CI: 0.171-0.590; P < 0.001).
Table 4.
Multivariable Cox Regression Analysis of Factors Associated With AF-Related Hospitalization in Patients With Paroxysmal and Persistent/Permanent Atrial Fibrillation
| 95% CI |
||||
|---|---|---|---|---|
| HR | Low | High | P Value | |
| Paroxysmal AF (84 events) | ||||
| Amiodarone | 1.045 | 0.584 | 1.872 | 0.881 |
| Class Ic antiarrhythmics | 1.861 | 1.116 | 3.101 | 0.017 |
| Digoxin | 1.008 | 0.391 | 2.596 | 0.987 |
| Beta-blockers | 0.804 | 0.506 | 1.277 | 0.355 |
| Verapamil/diltiazem | 0.866 | 0.399 | 1.881 | 0.717 |
| DOAC (vs VKA) | 0.352 | 0.206 | 0.602 | <0.001 |
| Cancer | 1.199 | 0.687 | 2.091 | 0.524 |
| CHA2DS2-VASc score | 0.929 | 0.801 | 1.078 | 0.331 |
| Persistent/permanent AF (96 events) | ||||
| Amiodarone | 3.012 | 1.835 | 4.943 | <0.001 |
| Class Ic antiarrhythmics | 1.947 | 1.069 | 3.548 | 0.029 |
| Digoxin | 1.137 | 0.658 | 1.966 | 0.645 |
| Beta-blockers | 1.521 | 0.989 | 2.340 | 0.056 |
| Verapamil/diltiazem | 2.067 | 1.117 | 3.825 | 0.021 |
| DOAC (vs VKA) | 0.318 | 0.171 | 0.590 | <0.001 |
| Cancer | 1.802 | 1.057 | 3.070 | 0.030 |
| CHA2DS2-VASc score | 0.932 | 0.808 | 1.074 | 0.330 |
In these patients, cancer was associated with higher risk of AF-related hospitalizations (HR: 1.802; 95% CI: 0.157-3.070; P = 0.030).
Discussion
Our study shows a high incidence of hospitalization in elderly patients with AF treated with oral anticoagulants. Cardiovascular hospitalizations were mainly related to cardiac rather than thromboembolic events, with a substantial proportion of AF-related conditions. Our results suggest that anti-arrhythmic drugs are not effective in preventing AF recurrences or high-ventricular rate symptomatic episodes.
In this study, we found a rate of 12.9%/year of hospitalization. This incidence is slightly higher than a previous post hoc analysis of the ROCKET-AF (Rivaroxaban Once-daily oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation) trial in which the rate of all-cause hospitalization was 10.2% during 2 years of follow-up.9 Among all reasons for hospitalization in this trial, 47% were for noncardiovascular causes, 36% were for cardiovascular conditions, 4% were AF-related, and 12% for bleeding events.9 The rate of hospitalizations was lower in this study compared to our analysis despite an apparent higher complexity of patients, as shown by the high prevalence of HF (60%), diabetes (40%), and previous stroke (55%). Furthermore, in the ROCKET-AF study, most of the patients had permanent AF (81%) compared to 62.8% of our cohort. Of note, no data on anti-arrhythmic drugs were provided in this post hoc analysis. The lower observed rate of hospitalization could be due to the controlled setting of the clinical trial compared to the routine clinical practice, with closer monitoring of the patients.
Conversely, the risk of all-cause hospitalization in a large cohort of 20,172 AF patients from the Chinese AF registry10 was as high as 24.0 per 100 patient-years during a follow-up of 37.3 ± 20.4 months increasing with age: 18.3 in patients <65 years, 26.0 in 65 to 74 years, and 33.5 in patients ≥75 years.10 This rate of hospitalization is higher compared to our cohort, taking into account the younger age of patients (64 years with 50% aged <65 years), the lower proportion of persistent AF (35.9%), of hypertension (66.4%) of COPD (0.8%), and of chronic kidney disease (3.5%).10 One potential reason accounting for this different result may be the low proportion of patients taking oral anticoagulants, which was 63% (of whom only 16.2% were DOACs) compared to our patients who were all anticoagulated.10 No data on cancer were provided in Chinese AF registry.
An analysis from The Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) registry11 enrolled 9.484 patients, of whom 2,963 underwent hospitalization with a 20%/year rate of cardiovascular hospitalizations at 1 year. This rate is probably driven by the high cardiovascular risk profile of patients from the ORBIT-AF registry, with high prevalence of previous CAD (33% vs 17.1% of our cohort), HF (33% vs 14.1% of our cohort), and low use of anticoagulants (76.8%, of which 4.8% on DOAC [only dabigatran was administered]).11 The type of anti-arrhythmic drugs was not reported.
In our cohort, we found an IR of AF recurrence of 2.0%/year. These data are consistent with a previous study in which an IR of 1.62%/year of AF recurrence was observed in patients with AF.12
In the present study, we found that anti-arrhythmic drugs were associated with cardiac hospitalizations and AF-related hospitalizations. This evidence is in line with the Chinese AF registry in which the use of anti-arrhythmic drugs was associated with 38% higher risk of AF hospitalizations, although it was not specified single anti-arrhythmic drugs.10 In the ORBIT-AF study, anti-arrhythmic drugs were linked to an increased risk of cardiac hospitalization (HR: 1.30), without any specific analysis on single drugs.11
Altogether, these data suggest that anti-arrhythmic drugs are not effective in preventing cardiovascular hospitalization. A similar finding comes from ablation studies. For example, a high rate of AF recurrences was observed in a study performed on patients randomized to catheter ablation or anti-arrhythmic therapy showing that at 9 months, 66% of patients in the catheter ablation group compared to 16% of patients with anti-arrhythmic drugs experienced an AF recurrence.13 In addition, one randomized clinical trial performed on 200 patients with persistent AF undergoing catheter ablation by optimized pulmonary vein isolation showed that the addition of anti-arrhythmic drugs did not reduce the recurrence of atrial tachyarrhythmia during a median follow-up of 370 days.14 In the post hoc analysis of the CABANA (Catheter Ablation versus Antiarrhythmic Drug Therapy for Atrial Fibrillation) trial including 1,240 patients with AF treated with catheter ablation or anti-arrhythmic drugs,15 AF burden in ablation group was 6.3% against 14.4% in the anti-arrhythmic drugs group at 12 months.15
In a systematic review and meta-analysis including six randomized clinical trials16 with 2,667 AF patients undergoing catheter ablation, the short-term use of anti-arrhythmic drugs was associated with a reduction in early AF recurrence compared to no treatment, but it did not decrease the risk of late AF recurrence.16 Finally, a recent consensus suggested that rhythm control has no morbidity or mortality benefit compared with ventricular rate control in elderly AF patients.17
Given these observations, the management of AF has evolved toward a more holistic and integrated care approach,18 as recommended in guidelines.19 Indeed, adherence to an integrated care approach based on the ABC (Atrial fibrillation Better Care) pathway has been associated with a reduction in mortality, stroke, bleeding, and hospitalizations rates.20 This is particularly important given the associated multimorbidity, polypharmacy, and clinical complexity seen in AF populations which have implications for risk and management.21,22
Study Limitations and strengths
Our study has some limitations. First, we performed an observational prospective cohort study, and we can establish only associations between risk factors and outcomes and not a causal relationship. For this reason, further interventional studies are needed. Secondly, we enrolled an Italian single-center cohort and our results could not be applied to patients belonging to other countries or ethnicities. Finally, for our analysis, we used only the first hospitalization occurring during follow-up. We acknowledge that the analysis of recurrent hospitalizations may provide additional prognostic information. However, also after a single hospitalization, the natural history of AF may change with a great impact on quality of life and disease’s perception. Indeed, the knowledge of characteristics of patients facing a first hospitalization, also according to different treatments may provide useful information for health care resource allocation and clinical management of AF patients.
Our study has also some strengths. Previous studies on this topic had a retrospective design, while our analysis is carried out in a prospective observation. Conversely to previous studies, patients included in the present study were taking oral anticoagulants. We obtained clinical records detailing the cause for hospital admission to confirm and classify the type of hospitalization. Finally, we provided detailed information on individual anti-arrhythmic drugs.
Conclusions
A significant proportion of elderly AF patients underwent hospitalizations for both cardiovascular and noncardiovascular causes. The use of anti-arrhythmic drugs was associated with an increased risk of cardiovascular and AF-related hospitalization. Our results suggest that prescription of these drugs should be carefully considered and reserved to symptomatic patients with frequent AF recurrences.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: Elderly patients with AF frequently undergo hospitalizations for both cardiovascular and noncardiovascular causes.
COMPETENCY IN PATIENT CARE: The most common causes of hospitalization are cardiac and are frequently AF- and HF-related.
TRANSLATIONAL OUTLOOK 1: The AF patients’ therapy should be optimized to reduce the risk of cardiac and noncardiac complications, especially AF- and HF-related and adverse drugs effect.
TRANSLATIONAL OUTLOOK 2: The use of anti-arrhythmic drugs was associated with an increased risk of AF-related hospitalization suggesting a scarce effect of these drugs in preventing AF episodes. Therefore, their use should be carefully considered and may be reserved for symptomatic patients with frequent AF recurrences.
Funding support and author disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables, please see the online version of this paper.
Contributor Information
Daniele Pastori, Email: daniele.pastori@uniroma1.it.
ATHERO-AF Study Group:
Tiziana Di Stefano, Elio Sabbatini, Patrizia Iannucci, Alberto Befani, Ilaria Maria Palumbo, and Emanuele Valeriani
Supplementary data
References
- 1.Wong C.X., Brooks A.G., Leong D.P., Roberts-Thomson K.C., Sanders P. The increasing burden of atrial fibrillation compared with heart failure and myocardial infarction: a 15-year study of all hospitalizations in Australia. Arch Intern Med. 2012;172:739–741. doi: 10.1001/archinternmed.2012.878. [DOI] [PubMed] [Google Scholar]
- 2.Magnussen C., Niiranen T.J., Ojeda F.M., et al. Sex Differences and Similarities in atrial fibrillation Epidemiology, risk factors, and mortality in Community cohorts: results from the BiomarCaRE Consortium (Biomarker for cardiovascular risk Assessment in Europe) Circulation. 2017;136:1588–1597. doi: 10.1161/CIRCULATIONAHA.117.028981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christiansen C.B., Olesen J.B., Gislason G., Lock-Hansen M., Torp-Pedersen C. Cardiovascular and non-cardiovascular hospital admissions associated with atrial fibrillation: a Danish nationwide, retrospective cohort study. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burdett P., Lip G.Y.H. Atrial fibrillation in the UK: predicting costs of an emerging epidemic recognizing and forecasting the cost drivers of atrial fibrillation-related costs. Eur Heart J Qual Care Clin Outcomes. 2022;8:187–194. doi: 10.1093/ehjqcco/qcaa093. [DOI] [PubMed] [Google Scholar]
- 5.Pastori D., Farcomeni A., Pignatelli P., Violi F., Lip G.Y. ABC (atrial fibrillation Better care) pathway and healthcare costs in atrial fibrillation: the ATHERO-AF study. Am J Med. 2019;132:856–861. doi: 10.1016/j.amjmed.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Camacho E.M., Lip G.Y.H. Estimating the impact of implementing an integrated care management approach with Atrial fibrillation Better Care (ABC) pathway for patients with atrial fibrillation in England from 2020-2040. Eur Heart J Qual Care Clin Outcomes. 2023;10:326–333. doi: 10.1093/ehjqcco/qcad055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ringborg A., Nieuwlaat R., Lindgren P., et al. Costs of atrial fibrillation in five European countries: results from the Euro Heart Survey on atrial fibrillation. Europace. 2008;10:403–411. doi: 10.1093/europace/eun048. [DOI] [PubMed] [Google Scholar]
- 8.Wolowacz S.E., Samuel M., Brennan V.K., Jasso-Mosqueda J.G., Van Gelder I.C. The cost of illness of atrial fibrillation: a systematic review of the recent literature. Europace. 2011;13:1375–1385. doi: 10.1093/europace/eur194. [DOI] [PubMed] [Google Scholar]
- 9.DeVore A.D., Hellkamp A.S., Becker R.C., et al. Hospitalizations in patients with atrial fibrillation: an analysis from ROCKET AF. Europace. 2016;18:1135–1142. doi: 10.1093/europace/euv404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong Z., Du X., Lu S., et al. Incidence and predictors of hospitalization in patients with atrial fibrillation: results from the Chinese atrial fibrillation registry study. BMC Cardiovasc Disord. 2021;21:146. doi: 10.1186/s12872-021-01951-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steinberg B.A., Kim S., Fonarow G.C., et al. Drivers of hospitalization for patients with atrial fibrillation: results from the outcomes registry for Better informed treatment of atrial fibrillation (ORBIT-AF) Am Heart J. 2014;167:735–742.e2. doi: 10.1016/j.ahj.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kisheva A., Yotov Y. Risk factors for recurrence of atrial fibrillation. Anatol J Cardiol. 2021;25:338–345. doi: 10.14744/AnatolJCardiol.2020.80914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilber D.J., Pappone C., Neuzil P., et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303:333–340. doi: 10.1001/jama.2009.2029. [DOI] [PubMed] [Google Scholar]
- 14.Demolder A., O'Neill L., El Haddad M., et al. No effect of Continued antiarrhythmic drug treatment on Top of optimized pulmonary vein isolation in patients with persistent atrial fibrillation: results from the POWDER-AF2 trial. Circ Arrhythm Electrophysiol. 2023;16 doi: 10.1161/CIRCEP.123.012043. [DOI] [PubMed] [Google Scholar]
- 15.Poole J.E., Bahnson T.D., Monahan K.H., et al. Recurrence of atrial fibrillation after catheter ablation or antiarrhythmic drug therapy in the CABANA trial. J Am Coll Cardiol. 2020;75:3105–3118. doi: 10.1016/j.jacc.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen W., Liu H., Ling Z., et al. Efficacy of short-term antiarrhythmic drugs Use after catheter ablation of atrial fibrillation-A systematic review with meta-analyses and trial Sequential analyses of randomized controlled trials. PLoS One. 2016;11 doi: 10.1371/journal.pone.0156121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dan G.A., Martinez-Rubio A., Agewall S., et al. Antiarrhythmic drugs-clinical use and clinical decision making: a consensus document from the European heart rhythm association (EHRA) and European Society of Cardiology (ESC) Working group on cardiovascular Pharmacology, endorsed by the heart rhythm Society (HRS), Asia-Pacific heart rhythm Society (APHRS) and International Society of cardiovascular Pharmacotherapy (ISCP) Europace. 2018;20:731–732an. doi: 10.1093/europace/eux373. [DOI] [PubMed] [Google Scholar]
- 18.Lip G.Y.H. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol. 2017;14:627–628. doi: 10.1038/nrcardio.2017.153. [DOI] [PubMed] [Google Scholar]
- 19.Chao T.F., Joung B., Takahashi Y., et al. 2021 focused Update consensus guidelines of the Asia Pacific heart rhythm Society on stroke prevention in atrial fibrillation: Executive summary. Thromb Haemost. 2022;122:20–47. doi: 10.1055/s-0041-1739411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Romiti G.F., Pastori D., Rivera-Caravaca J.M., et al. Adherence to the 'atrial fibrillation Better care' pathway in patients with atrial fibrillation: impact on clinical outcomes-A systematic review and meta-analysis of 285,000 patients. Thromb Haemost. 2021;122:406–414. doi: 10.1055/a-1515-9630. [DOI] [PubMed] [Google Scholar]
- 21.Grymonprez M., Petrovic M., De Backer T.L., Steurbaut S., Lahousse L. The impact of polypharmacy on the effectiveness and Safety of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Thromb Haemost. 2023;124:135–148. doi: 10.1055/s-0043-1769735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng Y., Li S., Liu X., Lip G.Y.H., Guo L., Zhu W. Effect of oral anticoagulants in atrial fibrillation patients with polypharmacy: a meta-analysis. Thromb Haemost. Published online July 3, 2023 doi: 10.1055/s-0043-1770724. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.