Abstract
Objective:
A cough persisting beyond eight weeks is referred as chronic cough (CC) and is a common symptom of many respiratory conditions and non-respiratory conditions. The role of a speech language pathologist (SLP) in CC is emerging and this study aimed to profile the awareness and practice patterns of SLPs practicing in India.
Study design:
Cross-sectional study.
Method:
An online survey was used to profile the assessment, treatment and counselling practices in CC among SLPs working in India. It sought to identify the awareness levels among SLPs regarding their role and availability of behavioural interventions for CC. Only SLPs who dealt with CC could complete the entire survey while other SLPs, filled regarding awareness and availability of behavioural interventions.
Results:
127 eligible responses obtained from SLPs working across clinical settings in India were analysed. 75.59% (n=96) of them had not seen patients with CC in their career. 47.24% (n=60) of them were aware that behavioural interventions were available for CC. Thirty-one SLPs completed the entire survey and their practice patterns indicated that few clinicians used cough-specific protocols while largely relying on voice and swallowing related assessment and treatment for CC.
Conclusion:
This survey the lack of awareness of SLPs’ role in CC and that their practices are dominated by existing procedures for voice and swallowing disorders. Increasing the awareness of SLP’s role in CC may increase the caseload of patients referred and expand the SLP’s scope of practice. Development of guidelines in CC practice and inclusion in coursework/curriculum are future considerations.
Keywords: chronic cough, refractory, practice patterns, healthcare, scope of practice
Introduction
Cough is a common symptom of many respiratory conditions such as chronic obstructive pulmonary disease (COPD), upper airway cough syndrome (UACS), asthma, and reflux diseases [1,2]. Other non-respiratory conditions and triggers, such as drug-induced cough hypersensitivity, environmental/ occupational irritants, and foreign bodies, are also linked with cough [3–5]. A cough complaint lasting more than eight weeks is called “chronic cough (CC)” [6]. Adults and children with CC are assessed and optimally treated according to standard guidelines recommended by healthcare bodies such as The American College of Chest Physicians (CHEST) [7,8] and the European Respiratory Society (ERS) [9]. Performing lung function evaluations such as spirometry, or pulmonary function tests are essential to rule out any underlying respiratory conditions before defining CC as idiopathic. However, when the cough persists beyond eight weeks, with an unidentified etiology, a normal chest X-ray, and does not respond to medical treatment for the common causes, it is labelled “refractory chronic cough (RCC)” [2,10–12] or “unexplained chronic cough (UCC)” [8,11,13].
Many terminologies are used to refer to such clinical presentations, however, recent literature has sought the broad concept of ‘cough hypersensitivity’ or ‘neurogenic laryngeal hypersensitivity’ to understand RCC/ UCC [3,14,15]. Patients present with laryngeal symptoms of hypertussia and allotussia due to increased sensitivity in the neural pathways which triggers cough [16,17]. Patients undergo multiple clinic visits, assessment procedures, and treatment trials before being diagnosed with RCC/UCC and suffer from its consequences. This type of cough need not necessarily be associated with an underlying lower airway disease but could be reflective of laryngeal hypersensitivity [16]. Patients tend to have laryngeal dysfunctions such as hoarseness, throat clearing, globus sensation, itch, and tickle, which may be mistaken for symptoms of lower airway disease. Patients also experience deterioration in their physical well-being [4,18] and quality of life in social contexts, work life, and leisure [18–21]. Socioeconomic distress resulting from their perpetuating cough has also been documented [22].
CC is usually managed by medical and pharmacological interventions by ruling out common aetiologies as dictated by protocols [8,9]. The need for additional therapy to manage CC is well-founded, and research has highlighted the role of non-pharmacological interventions for CC [4,23,24]. Behavioural interventions for CC have emerged in the last two decades, usually provided by speech language pathologists (SLPs) or physiotherapists [24–28]. The role of speech language pathology and physiotherapy in the management of CC has gained attention with the advent of such behavioural interventions. These include breathing exercises, vocal hygiene and hydration, cough suppression strategies, patient education, and counselling [24–28]. The principles of these interventions were borrowed from the context of voice disorder management [17,29]. The components of patient education, vocal hygiene, and breathing exercises target reducing laryngeal irritation and improving vocal function [29]. The effectiveness of these behavioural programmes has been tested in the CC population [25,28,30,31] and were found to provide quick relief [32]. Other benefits of these behavioural programmes are their cost-effectiveness and significant improvement in quality of life [22,25,28,30].
Behavioural interventions are often recommended at later stages of treatment, more as a last resort after several rounds of pharmacological trials [31,33]. The delay in referral could be attributed to the lack of awareness of the role of the SLP in CC among physicians [34]. The CHEST guidelines recommend a trial of speech pathology treatment for UCC [8]. The ERS guidelines mention nonpharmacological therapy for patients with CC [9]. The American Speech and Hearing Association (ASHA) has included CC in its scope of practice under potential aetiology for communication disorders under ‘disorders of aerodigestive tract function’ [35]. In contrast, the Rehabilitation Council of India (RCI), which governs speech and hearing professionals in India, has not included CC in its scope of practice [36]. This may be due to the lack of awareness of CC among Indian SLPs. There are no published documents (position statements, review papers, guidelines) on speech pathology or behavioural management on CC in India. CC is not included in the under- or post-graduate curriculum in India. The evidence-based literature for speech pathology treatment for CC suggests a possible expansion in the scope of practice of SLPs, which is possibly emerging in India.
Although CC is within the scope of practice of SLPs, very few have awareness and exposure to work in this speciality. The level of knowledge and clinical expertise in CC may not be extensive or uniform across SLPs practicing in India. However, with increasing awareness among professionals and sufficient evidence-base from Western literature [25,28,30,32] the client load of CC seen by SLPs is bound to increase manifold. This survey was designed to understand the practice patterns of the few SLPs working in India with CC population. We aimed to investigate the following: 1) knowledge and awareness levels of Indian SLPs in the assessment and management of CC, 2) identify the proportion of SLPs dealing with CC in India, and 3) practice protocols of CC followed by the few SLPs working with CC in India.
Method
This survey was approved by the Institutional Ethics Committee of Kasturba Medical College, Manipal Academy of Higher Education, Mangalore (IECKMCMLR-11/2022/451).
Step 1: Development and validation of the survey
Literature on CC assessment and treatment by SLPs and physiotherapists was identified and used as references to develop this survey questionnaire [24,25,27,28,30,32]. An initial version of the questionnaire was developed by the first author to collect information on current practice trends in the assessment and management of CC among SLPs practicing in India. The questions focussed on demographics, clientele, symptoms, assessment, treatment, and complementary and alternative medicine (CAM) practices for patients with CC. Close-ended questions were used to collect quantitative data (demographics, clientele, symptoms, and aetiology), and open-ended questions were used to gather qualitative perspectives on assessment/treatment/CAM. Additional probes or follow up questions, mostly open-ended, were also used in the survey.
The fourth author, with a clinical experience of 10 years in the field of voice and swallowing disorders, reviewed the survey questions and suggested modifications such as adding other relevant questions and altering the question structure/type. Differences in opinions were discussed and resolved by consensus. The questionnaire was again reviewed by the fifth author (clinical experience of 15 years in the field of voice and swallowing disorders), who was given a review form to provide inputs regarding the survey. Based on the recommendations provided in the review form, the final version of the survey questionnaire was generated. A content validation form was prepared using the systematic approach for content validation [37], which provides acceptable cut-off scores. Two SLPs validated the final version, which received a content validity index score of 0.96. This score was higher than the recommended acceptable cut-off value [37].
The developed 28-item survey questionnaire was converted to an online version by uploading it to Google Forms. It contained six sections: brief information about the survey and consent, demographics, screening based on awareness of the topic, assessment-related data, treatment-related data, counselling, and CAM. Consent to participate in the survey was obtained from the respondents in the first section and was directed to submission if not consented. Similarly, in the third section, if CC was not within the scope of the clinician, the survey was directed to a few questions on awareness about CC, followed by submission of the form. Only SLPs who worked with CC completed the entire survey. The online version of the survey was checked for ease and completion duration by running a trial with the contributing authors and ten undergraduate speech-language pathology students. The time taken to complete the entire survey was around ten minutes.
Step 2 – Administration of the survey
The survey was circulated through email lists and social media, thus adopting a convenience sampling method. Professionals working in India were targeted by selecting email addresses from the Indian Speech and Hearing Association (ISHA) database, which has more than 3000 registered SLPs. However, not all practicing SLPs in India are registered with ISHA; hence, the surveys were circulated through social media for greater reach. The responses were collected between November 2022 and January 2023. The first author sent two reminder emails/messages to ensure more responses.
Eligibility criteria
The inclusion criteria were set as follows: a) should be a practicing SLP in India (as this study aimed to understand the awareness and practice patterns among SLPs in India), b) must have a minimum experience of one year (to avoid responses from undergraduate students), and c) must consent to participate in the survey. The exclusion criteria considered were SLPs practicing abroad or participants with no or less than one year of clinical experience.
Data analysis
The results of this survey included answers to both closed- and open-ended questions. Quantitative variables were analysed using descriptive statistics (mean and standard deviations). The answers to the open-ended questions were grouped based on similar response categories for a given question. Initial grouping was performed by the first author & cross-checked by the fifth author. If there was a difference in opinion, it was discussed until both authors agreed on the grouping category. These were then summarized using frequency–percentage analysis, depicted as percentage of responses grouped under response categories. The Jamovi software (version 2.3) (The Jamovi Project, 2022) was used to perform the statistical analyses.
Results
One hundred and fifty-two SLPs filled out the survey, of which twenty-five responses were excluded based on the eligibility criteria and consent. Only responses from SLPs working in India with at least one year of working experience were included. This has been depicted as a flowchart in Figure 1 (considering one round of emails sent). The findings have been reported in the following sub-sections as per the six sections of the survey.
Figure 1.
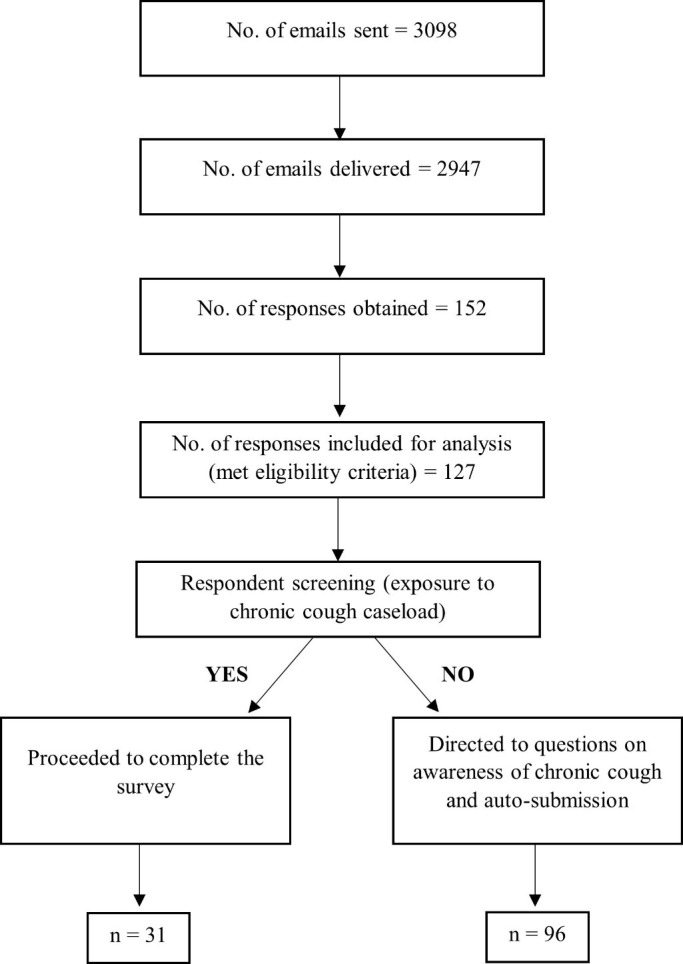
Survey administration and included responses depicted as a flowchart.
Consent
In the first section of the survey, the respondent’s consent to partake in the study was obtained. If the respondent indicated an unwillingness to participate in the survey, the form was configured to auto-submit. Three respondents did not agree to participate in this survey and were thus excluded from the analysis.
Demographic data
The demographic section of the survey collected information on age, gender, years of experience, the city of work, and clinical work settings. Responses from SLPs practicing abroad (n=21) or with less than 1 year clinical experience (n=1) were excluded. A final one hundred and twenty-seven responses were subjected to analysis. The mean age, gender distribution, and years of clinical experience of the respondents are shown in Table 1. The clinical work settings of the respondents yielded two hundred and four item responses. These spanned across private set-ups (34.80%, n=71), hospitals (27.45%, n=56), training institutes/colleges (23.53%, n=48), home-based set-ups (8.82%, n=18) and schools (3.92%, n=8). Additionally, three respondents mentioned online services (0.98%, n=2) and a government-related setting (0.49%, n=1).
Table 1.
Demographic information of respondents.
| Demographic information of 127 SLPs | |||
|---|---|---|---|
| Demographic data | Gender | Total respondents | |
| Males | Females | ||
| N (%) | 26 (20.5%) | 101 (79.5%) | 127 (100%) |
| Age (in years) (Mean±SD) [Range] |
33.65±6.11 [23–47] |
30.11±7.19 [22–53] |
30.84±7.11 [22–53] |
| Years of overall clinical experience (Mean±SD) [Range] |
10.26±5.14 [1–22] |
7.35±6.78 [1–35] |
7.95±6.57 [1–35] |
| Years of clinical experience in voice (Mean±SD) [Range] |
8.03±4.97 [1–20] |
5.25±5.63 [1–27] |
5.82±5.59 [1–27] |
| Demographic information of respondents 31 SLPs who worked with chronic cough population | |||
| N (%) | 10 (32.26%) | 21 (67.74%) | 31 (100.00%) |
| Age (Mean±SD) (in years) [Range] |
33.80±5.78 [25–47] |
30.66±7.88 [22–50] |
31.67±7.33 [22–50] |
| Years of overall clinical experience (Mean±SD) [Range] |
9.60±4.81 [3–20] |
8.04±7.40 [1–28] |
8.54±6.63 [1–28] |
| Years of clinical experience in voice (Mean±SD) [Range] |
7.80±5.11 [2–20] |
5.61±5.63 [1–22] |
6.32±5.48 [1–22] |
Note. SD, standard deviation.
Respondents screening
This section covered three questions, one each on CC caseload, awareness of behavioural interventions for managing CC, and the professionals involved in the same. The first question on caseload identified SLPs who dealt with the CC population based on their clinical practice. Ninety-six respondents (75.59%) had not seen patients with CC in their career and thus they were not directed to other sections of the survey. However, they could answer the remaining two questions before the form was auto-submitted. As a result, only thirty-one respondents (24.41%) proceeded to complete the entire survey.
Although most did not deal with this population, 47.24% (n=60) of the respondents were aware that behavioural interventions were available for CC. Interestingly among these 60 respondents, 73.33% (n=44) were working in a hospital and/or training institute. An array of healthcare professionals was listed by the SLPs when asked to mention the professionals who provided behavioural interventions for CC based on their knowledge and experience. Two hundred and sixty-six item responses were obtained from the participants, and this distribution is depicted in Figure 2. Fourteen (5.26%) of them reported no knowledge of the professionals involved in behavioural interventions. The frequently reported professionals were SLPs (25.56%, n=68), otorhinolaryngologists/ENTs (23.68%, n=63), and pulmonologists (16.92%, n=45).
Figure 2.
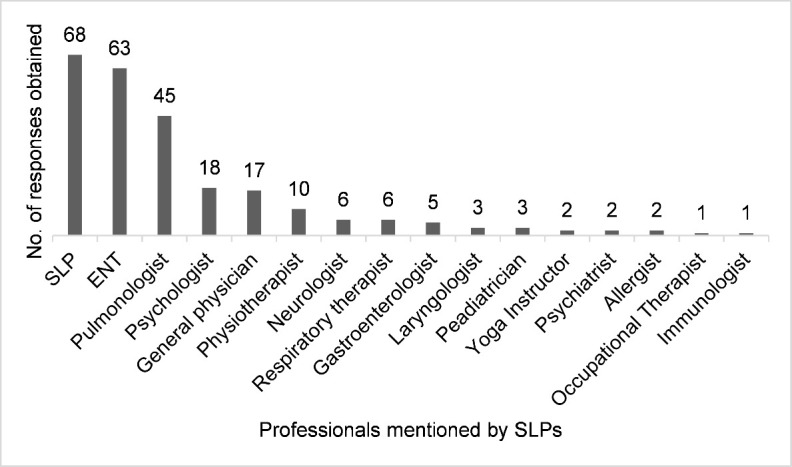
The professionals involved in the management of chronic cough as reported by all 127 SLPs.
Respondents screened for further analysis
For the upcoming sections, thirty-one completed surveys were analysed. It included responses from twenty-one female (67.74%) and ten male (32.26%) respondents. The mean age, gender distribution, and years of clinical experience of these respondents are reported in Table 1.
Assessment related data
This section addressed seven questions on clientele-related data, referrals, signs and symptoms, etiology, and assessment procedures. The inquiries on clientele data revealed that 74.19% (n=23) of them assessed patients with CC, whereas 25.81% (n=8) did not. It is possible that these eight SLPs did not use cough specific procedures for evaluation but proceeded to intervention based on the patient’s case history. The percentage of patients with CC dealt by these SLPs is illustrated in Figure 3. Most SLPs (67.74%, n=21) saw 1–2 patients monthly. For the question on referral source, sixty-one item responses were received which was predominantly from ENTs/otorhinolaryngologists (44.26%, n=27), pulmonologists (21.31%, n=13), primary care physicians (14.75%, n=9), and allergists (9.84%, n=6), among others. Two questions were on signs and symptoms presented by patients with CC. The SLPs were asked to specify how often their patients reported complaints of voice change or hoarseness, with response options ranging from always to never. The frequency of voice complaints was documented as follows: “very often” (45.16%, n=14), “sometimes” (41.94%, n=13) and “always” (12.90%, n=4). The question on “symptoms reported by patients other than cough”, generated one hundred and fifty item responses, as depicted in Table 2. One SLP indicated that they had never encountered patients with such complaints. These responses reflect the symptoms as reported by the patients with CC who were seen by the SLPs.
Figure 3.
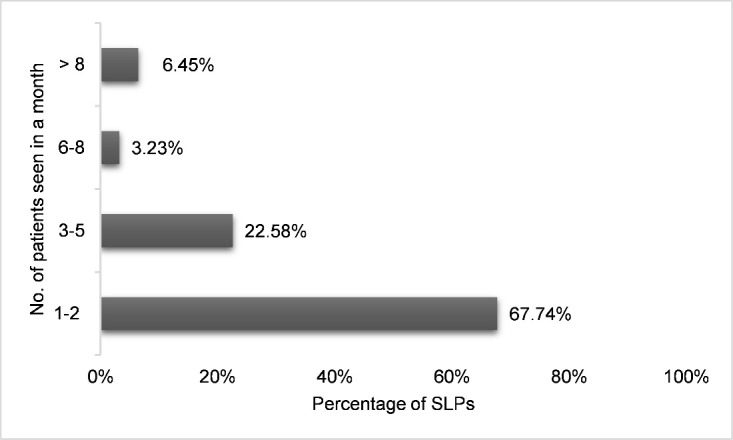
Chronic cough caseload per month of the 31 SLPs who completed the survey.
Table 2.
Common symptoms reported by patients with chronic cough as encountered by the 30 SLPs.
| Symptoms | Number of responses | Percentage of item responses of 30 SLPs |
|---|---|---|
| Voice change | 27 | 18.00% |
| Breathlessness | 24 | 16.00% |
| Tiredness | 20 | 13.33% |
| Pain/discomfort | 20 | 13.33% |
| Impaired work life | 19 | 12.67% |
| Sleep disturbances | 13 | 8.67% |
| Poor social life | 13 | 8.67% |
| Sleep apnea | 7 | 4.67% |
| Vocal fatigue | 2 | 1.33% |
| Low volume of voice | 1 | 0.67% |
| More effort in speaking | 1 | 0.67% |
| Voice trails off | 1 | 0.67% |
| Throat clearing | 1 | 0.67% |
| Poor food intake | 1 | 0.67% |
Eighty-two item responses were obtained for the open-ended question on common etiologies of CC. One SLP chose not to respond to this question. Most reported causes were lung-related pathologies (14.46%, n=12), vocal pathologies (12.05%, n=10) gastroesophageal reflux disease (GERD; 10.84%, n=9), and asthma (9.64%, n=8) among others.
The SLPs were enquired about the tools, procedures, or questionnaires used in evaluation of CC. This yielded sixty-three item responses, with four participants not revelaing their assessment practices. Instrumental procedures related to voice (26.87%, n=18) and swallowing (5.97%, n=4), subjective measures (16.42%, n=11), case history (14.93%, n=10), and patient-reported measures (11.94%, n=8) were frequently carried out by the SLPs. Few SLPs reported using cough-specific questionnaires/checklists (5.97%, n=4). Table 3 shows the detailed breakdown of these responses.
Table 3.
Procedures and tools carried out by the 27 SLPs for assessment of chronic cough.
| Procedures/Tools | Number of responses | Percentage of item responses of 27 SLPs |
|---|---|---|
| Instrumental measures – voice related (endoscopy, stroboscopy, acoustic analysis, aerodynamic measures, EGG) | 18 | 28.57% |
| Instrumental measures – swallowing related (FEES & VFS) | 4 | 6.35% |
| Perceptual voice analysis & MPT | 11 | 17.46% |
| History/Informal assessment | 10 | 15.87% |
| PROM (VFI, VHI, VR-QoL) | 8 | 12.70% |
| Cough-related assessment | 4 | 6.35% |
| Swallowing related assessment | 3 | 4.76% |
| Voice assessment | 2 | 3.17% |
| EMST | 1 | 1.59% |
| Therapeutic trials | 1 | 1.59% |
| Cranial Nerve evaluation | 1 | 1.59% |
Note. FEES,Flexible Endoscopic Evaluation of Swallowing; VFS, Video Fluoroscopy, EGG, Electroglottography; MPT, Maximum Phonation Time; PROM, Patient-Reported Outcome Measures; VFI, Vocal Fatigue Index; VHI, Voice Handicap Index; VR-QoL, Voice-Related Quality of Life; EMST, Expiratory Muscle Strength Training.
Treatment-related data
The section on management practices consisted of four questions. Among the thirty-one analysed responses, 67.74% (n=21) provided treatment for CC. The next question on treatment options used by the SLPs elicited fifty-one item responses. The same ten respondents who answered “No” to the previous question, responded “Not applicable” to this question. The techniques followed by the remaining SLPs are detailed in Table 4.
Table 4.
Treatment techniques used by the 21 SLPs for managing chronic cough.
| Treatment techniques | Number of responses | Percentage of item responses of 21 SLPs |
|---|---|---|
| Vocal hygiene | 10 | 19.61% |
| Voice therapy | 8 | 15.69% |
| Breathing exercises | 8 | 15.69% |
| Relaxation exercises | 5 | 9.80% |
| Swallowing/dysphagia therapy | 4 | 7.84% |
| Cough Suppression Strategies | 4 | 7.84% |
| Steam inhalation | 3 | 5.88% |
| Medications | 3 | 5.88% |
| EMST/Respiratory training | 2 | 3.92% |
| Psychoeducational counselling | 1 | 1.96% |
| Diet changes | 1 | 1.96% |
| Cognitive Behavioural Therapy | 1 | 1.96% |
| Referral to Otorhinolaryngology | 1 | 1.96% |
Note. EMST, Expiratory Muscle Strength Training.
SLPs delivered a varying number of behavioral therapy sessions, ranging from one session to more than six sessions. Ten respondents (32.26%) answered “Not applicable” to this question. The options chosen by the respondents are as follows: more than 6 sessions (19.35%, n=6), 1–2 sessions (16.13%, n=5), 3–4 sessions (16.13%, n=5), 5–6 sessions (12.90%, n=4), and as per patient needs (3.45%, n=1).
The final question on “the number of times you ask your patients to perform exercises or follow strategies at home” resulted in thirty-six cumulative item responses. Eight respondents (22.22%) reported “Not applicable”. The most documented answers were 3 times a day (22.22%, n=8), and whenever the patient experiences cough (13.89%, n=5). This was followed by 2 times a day and patient needs (each 8.33%, n=3) and 2–3 or 3–5 times or every day (each 5.56%, n=2). Other answers were 5 times/day, 2–6 times/day, and 10–15 minutes/session (each 2.78%, n=1).
Counselling & CAM
This section had two questions on components of counselling and four questions on CAM. A significant majority of thirty SLPs (96.77%) counselled their patients about cough and its effects. Twenty-seven (87.10%) SLPs also counselled on how to avoid the persistent cough while four (12.90%) did not. To understand how SLPs aligned with utilizing CAM in treatment, they were asked if they recommended CAM to their patients. Fifteen SLPs (48.39%) responded affirmatively, stating “Yes, I believe that it may augment medications” while thirteen (41.94%) SLPs opted “No, strictly traditional methods only”. One reported an integrated approach (3.23%) while two SLPs (6.45%) answered “Not applicable” to this question.
The CAM approaches mostly recommended by SLPs comprised the following - home remedies (19.57%, n=9), yoga (10.87%, n=5), steam inhalation (8.70%, n=4), homeopathy (4.35%, n=2), and lifestyle changes (4.35%, n=2) among others. Self-reports of patients seeking remedies or alternative approaches yielded forty-one item responses from twenty-two SLPs (70.97%). Majorly reported approaches included home remedies, yoga, ayurveda, and steam inhalation, among others. It is important to note that this information was recalled by SLPs as reported by their patients.
Discussion
This survey determined to gather data from three distinct aspects: i) assessing the awareness among SLPs about CC, ii) identifying the proportion of SLPs working with CC and, iii) understanding the clinical practice patterns of Indian SLPs involved in assessing and treating CC. Notably, this is the first survey conducted among SLPs in India on CC and the findings indicate that it is emerging as an new area of practice. Considering that the topic explored in this survey was relatively unfamiliar to SLPs, there is a possibility that those without prior knowledge did not partake in the survey as it involved questions about an unfamiliar caseload. Thus, the survey appears to have primarily attracted participation of only a handful of SLPs who specifically worked with the targeted clientele.
Awareness and respondent screening
The initial sub-section of the survey targeted to find how many clinicians were working with patients with CC and whether they were aware of behavioural interventions available. While most of the respondents’ clientele did not include patients with CC, a considerable number were familiar with the feasibility of behavioural interventions for CC. Numerous professionals from various disciplines were mentioned as service providers for this behavioural intervention. However, the responses were based on the clinician’s knowledge and experience, as this subject is not addressed in the curriculum during undergraduate or post-graduate degree courses. From these responses, it could be interpreted that SLPs were aware of behavioural interventions for CC but did not regard it within their scope of practice. This clearly showed that there is a lack of awareness of CC among SLPs, particularly about their role in assessing and managing it. This survey can serve as a steppingstone for future studies exploring this area of CC.
Assessment related data
The decreased CC caseload of SLPs could be due limited referrals from physicians owing to the insufficient knowledge of behavioural interventions, despite guideline recommendations [34]. This can be corroborated with findings from literature that patients are referred to speech language pathology late, after several investigations and treatments for their CC [31,32]. Physicians may have reservations about how such treatments work, which has been indicated as a possibility for the delay in referral [31].
Speech pathology intervention was specified for UCC in CHEST panel and ERS guidelines [8,22]. A 2019 Indian consensus statement on cough, recommended referral to a “specialist” when the cough persists after rigorous methodical testing and patients have not benefitted from medical treatment [38]. This consensus statement has guidelines for cough of all origins but does not include information on RCC/UCC. Furthermore, it does not specify the field of the specialist or provide stepwise decision making regarding this consultation. However, a recent consensus statement on managing cough has provided definitions for UCC and RCC, and a recommendation of a trial speech therapy management for UCC [10]. This shows that awareness on the role of SLPs in managing CC has grown among physicians in the past four years. Physicians may prefer to suggest speech pathology treatment when they suspect the etiology to be laryngeal hypersensitivity than other causes [34]. In the following years, this awareness may potentially increase referrals to SLPs. This solidifies the need for SLPs to better equip themselves with the knowledge and training of CC to provide clinical services for this cough phenotype.
SLP respondents indicated that their patients with CC regularly reported voice complaints, such as hoarseness or a change in voice. This is not surprising as earlier studies have also reported on the co-occurrence of laryngeal abnormalities such as vocal cord dysfunction, paradoxical vocal fold movement, and voice hoarseness in patients with CC [26,27,39,40]. Cough is known to affect everyday activities, and the common complaints reported by patients to SLPs in this survey are similar to findings from the literature [41]. The physical symptoms encompassed breathlessness, tiredness, pain or discomfort, and sleep disturbances/ apnoea. Other studies have identified additional symptoms, such as vomiting, retching, hernias, and headaches, leading to physical exhaustion/tiredness [17,42]. SLPs reported that the work life of their patients was impaired though details were not provided. Literature shows loss of job, frequent absences from work, embarrassment during meetings, and poor concentration and attention as some of the work-related complications faced by patients with CC [41–43]. SLPs frequently reported poor social life among their patients; however, specific case scenarios were not disclosed. Previous studies have highlighted social isolation due to the embarrassment of coughing in public spaces or social situations. Other compromising issues faced by patients included interference with lifestyle and leisure [42,43]. Respondents of this survey did not report psychological issues among their patients but abundant reports on depression, increased anxiety, fatigue, disrupted mood, and emotional distress are available [17,43–45].
While numerous causes are attributed to CC, the triad conditions - UACS, asthma, and GERD - have been reported as the most common etiologies [46–49]. The outcomes of this survey indicated GERD and asthma as predominant causes, along with lung-related disorders and vocal pathologies. SLPs possibly linked CC with dysphagia/voice, because for assessment, many relied on instrumental and subjective measures used in voice and/or swallowing evaluations. A scoping review on clinical assessment methods of SLPs for CC also reported that voice related measures were frequently used [50]. Only a minority of SLPs used cough related procedures, such as assessing cough triggers, cough symptoms, and quality of life and standardized cough-related checklists like Cough Symptom Index (CSI), Cough Quality of Life Questionnaire (CQLQ), Newcastle Laryngeal Hypersensitivity (NLH) questionnaire. The usage of such questionnaires is recommended in literature [51,52]. Interestingly, one response indicated attempting therapeutic trials, as recommended by the CHEST panel and ERS guidelines [8,22]. Unique responses obtained from respondents comprised performing auscultations and using Expiratory Muscle Strength Training (EMST) devices. These findings indicate that practice patterns of CC are evolving in India. SLPs predominantly used already available materials and adjunctly used cough-specific tools if they were aware.
Treatment-related data
Ten SLPs did not provide treatment or reveal their treatment techniques, but substantial variations were evident in the responses obtained from the other respondents. SLPs predominantly indulged in techniques borrowed or adapted from voice therapy literature for treating CC [29]. This could be because both coughing and voicing mechanisms share similar anatomy. Coughing can be as harmful as phonotraumatic behaviours like screaming or talking loudly [39]. Coughing may create laryngeal irritation and dryness, thus, exacerbating the cough problem. The laryngeal structures addressed through voice treatment assist in suppressing cough, even if the physiology behind this is not exactly understood. This might be because targeting the underlying vocal pathology consequently leads to an improvement in the cough-related complaints [29].
Strategies provided by clinicians revolved around reducing laryngeal irritation, a major cause that triggers persistent cough [29]. This included giving breathing exercises, vocal hygiene tips, relaxation techniques, cough suppression strategies, steam inhalation, and dietary changes. Cough triggers originating in the laryngeal area can possibly be controlled through suitable vocal hygiene practices which minimize laryngeal irritation [39]. In some cases, patients with CC may experience physical tension or stiffness of the head, neck, or upper chest areas. They may engage in clavicular breathing or maintain abnormal postures at rest or during speech [29,39]. Clinicians possibly preferred breathing exercises to address such issues to promote relaxation of the stiff muscles of the throat, neck, and shoulders [5]. Apart from these, few clinicians reported using specific techniques to target the cough behaviour (cough suppression strategies, pursed lip breathing, psychoeducational counselling). These strategies for cough suppression or control are quite prevalent within the CC literature [25,28,30].
Most SLPs provided behavioural therapy between one to six sessions, and one SLP reported offering flexible number of sessions. Literature shows that patients are usually treated over a span of 1–2-months, across three-four sessions, although this may range between 1–7 sessions. [31,32,53]. Studies recommend that deciding the number of sessions should be based on the patient's needs and learning ability [29,54]. There was a great variability in the dosages prescribed by the SLPs for the treatment exercises or strategies. A particular treatment program for CC, provides comprehensive information on the dosage, practice conditions, and hierarchy for each exercise included [54].
Counselling & CAM
Most clinicians counselled their patients about cough, its implications, and how to avoid it. Typically, treatment programs for CC include a component on “psychoeducation” or “patient education/ counselling”. These are intended to cover aspects such as - differences between a medical and a behavioural approach, accepting a behavioural treatment, helping patients perceive their cough as a controllable factor and overcome it [24,25,28,54]. Patients are educated about the larynx, laryngeal well-being, identifying cough triggers, making lifestyle changes, and stress management.
Nearly half of the SLPs who completed the survey acknowledged the augmentative effects of complementary and alternative medicinal approaches on CC. The other half adhered strictly to traditional methods or opted not to not reveal their opinions. This suggests that SLPs are willing to try different modalities as much as they confine to their beliefs. There might be more willingness to endorse CAM if efficacy for treating cough is demonstrated [55]. SLPs who advocated CAM, mostly suggested home remedies, steam inhalation, and yoga. Similarly, patients self-reported using CAM such as home remedies, ayurveda, and yoga. A study on online forums showed that patients sought home remedies when conventional methods did not relieve their cough [56]. Home remedies are usually concoctions of a single or many herbal ingredient(s), each with a property that alleviates cough symptoms. These may be antitussive, anti-inflammatory, antibacterial, or mucolytic [57] in nature.
Limitations and future considerations
The major limitation of this survey would be its relatively small sample size. Although one hundred and fifty-two responses were received, only thirty-one completed responses could be analysed. The interpretations presented in this article reflect the practices of few SLPs and not representative of all SLPs in India. These findings cannot be generalized or applied across different settings. Nonetheless, this was anticipated as many SLPs in India are not working with chronic cough. Thus, this preliminary survey highlighted the very idea it intended to - lack of awareness of CC and their role in assessing and treating CC, among SLPs in India. As for the grouping strategy followed for survey responses, categories were grouped as deemed appropriate and this could have led to some bias and thus, subsequently led to broader interpretations. Another potential limitation is the interpretation of survey responses that had binary options or open-ended questions which did not receive detailed answers. These study findings and recent advances in cough consensus statements in India should prompt contemplating behavioural management for CC. Further, CC needs to be included in the curriculum for the under- and post-graduation courses of speech language pathology. Conducting workshops and continuing education programs on CC will facilitate ongoing learning among practicing clinicians. This will enable knowledge and clinical training in CC for both speech pathology students and graduate clinicians.
Conclusion
The findings of this survey showcase the status of CC as perceived by SLPs in India. It is emerging as an area of practice among Indian SLPs. The key takeaways from this survey are: first, there is a lack of awareness regarding SLPs’ role in assessing and treating CC. Second, very few SLPs deal with this population and their practices are dictated by their experience and existing procedures. There is a need for creating awareness on CC among SLPs in India, wherein working with chronic refractory cough is not yet a routine part of clinical practice. These findings may guide clinicians to develop knowledge through self-learning, continuing education programs, and workshops. Practice protocols for speech pathology treatment for CC in India may be devised in the foreseeable future if necessary measures are taken towards increasing awareness and clinical training. This will empower SLPs to facilitate the mental and physical well-being of patients with CC, thereby contributing to the overall healthcare system.
APPENDIX.
Please answer the following questions, considering patients with cough who DO NOT have any swallowing related (aspiration/penetration) complaints.
-
Kindly indicate your willingness to participate - Do you consent to participate in this survey?
Yes
No
Age:
Gender:
Are you currently working in India?
Mention the city you are currently practicing in:
Please mention your overall clinical experience (in years):
Please mention your clinical experience working in voice & disorders (in years):
-
Please mention your clinical practice setting:
Private practice
Hospital
Training institute/college
Schools
Others: _____
-
Does your caseload include patients with chronic cough?
Yes
No
-
Are you aware that behavioural interventions exist for managing chronic cough?
Yes
No
-
Based on your practice & experience, mention the professionals involved in providing behavioural management for chronic cough?
(Respondents who answered ‘No’ to Q9, were directed to submit the survey after answering Q10 & 11; whereas if they answered ‘ Yes’, they could proceed to complete the survey)
-
Does your clinical practice involve assessment of patients with chronic cough?
Yes
No
-
Approximately how many patients with chronic cough do you see in a month?
1–2
3–5
6–8
>8
NA
-
Select the professionals who refer cough patients to you? (Choose all that apply)
ENT
Allergist
Pulmonologist
Primary care physician
Others: _____
-
Do your patients with chronic cough, also complain of voice change or hoarseness?
Always
Very often
Sometimes
Rarely
Never
Please list the most common etiologies/medical conditions among the patients with chronic cough you encounter?
-
What are the other symptoms reported by your patients with chronic cough apart from cough? (Choose all that apply)
Tiredness
Breathlessness
Sleep disturbances
Voice change
Pain/ Discomfort
Impaired work life
Poor social life
Others: _____
Please mention the assessment procedures you generally carry out for a patient with chronic cough. Kindly list all tools, procedures or questionnaires you may use in your practice:
-
Do you provide treatment for patients with chronic cough?
Yes
No
If YES, please mention the treatment options you choose for your patients with chronic cough.
-
How many sessions do you typically provide therapy for a patient with chronic cough?
1–2
3–4
5–6
>6
NA
Kindly mention the number of times (frequency) you ask your patients to perform exercises or follow strategies at home (e.g. 5 times a day/whenever they are experiencing cough/ throughout the day)?
-
Do you counsel your patients about cough and its effects?
Yes
No
-
Do you also counsel on how to avoid the persistent cough?
Yes
No
-
Do you recommend your patients to try complementary and alternative methods (CAM) to manage their cough, such as yoga, pranayama, ayurveda, etc.?
Yes, it may augment medications/therapy
No, strictly traditional methods only
Other opinions (Please state them)
If yes, what are some of the CAM you recommend to your patient? Please list them.
Do any of your patients’ self-report on use of CAM for their cough complaints?
Please state the commonly reported CAM measures used by your patients.
Footnotes
Authors' contributions: Y.V., V.A. and R.K.B. were involved in study conceptualization and design. Y.V. developed the initial version of the survey, which was reviewed and edited by D.G. and R.K.B. The survey was circulated by Y.V. The formal data analysis was done by Y.V. and R.K.B and they drafted the first version of the manuscript. Y.V., R.K.B, D.G. were involved in editing the manuscript for content and clarity. The prepared manuscript was reviewed by V.A., S.K., and D.G. All authors approved the final manuscript.
Ethics approval and consent to participate: This survey was approved by the Institutional Ethics Committee of Kasturba Medical College, Manipal Academy of Higher Education, Mangalore (IECKMCMLR-11/2022/451).
Conflict of interest: The authors have no conflicts of interest to declare.
Publisher’s note: all claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Funding: The first author received grant-in-aid (Dr. T.M.A.Pai Scholarship) instituted by Manipal Academy of Higher Education, Manipal, for her full-time PhD.
Availability of data and material
Data available on request from the corresponding author.
References
- 1.Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. The Lancet. 2008;371:1364–74. doi: 10.1016/S0140-6736(08)60595-4. [DOI] [PubMed] [Google Scholar]
- 2.Irwin RS, Madison MJ. The diagnosis and treatment of cough. Crit Care Med. 2000;343:1715–21. doi: 10.1056/NEJM200012073432308. [DOI] [PubMed] [Google Scholar]
- 3.Chung KF, McGarvey L, Song W-J, Chang AB, Lai K, Canning BJ, et al. Cough hypersensitivity and chronic cough. Nat Rev Dis Primer. 2022;8:1–21. doi: 10.1038/s41572-022-00370-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perotin JM, Launois C, Dewolf M, Dumazet A, Dury S, Lebargy F, et al. Managing patients with chronic cough: challenges and solutions. Ther Clin Risk Manag. 2018;14:1041–51. doi: 10.2147/TCRM.S136036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Visca D, Beghè B, Fabbri LM, Papi A, Spanevello A. Management of chronic refractory cough in adults. Eur J Intern Med. 2020;81:15–21. doi: 10.1016/j.ejim.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irwin RS, French CL, Chang AB, Altman KW, Adams TM, Altman KW, et al. Classification of Cough as a Symptom in Adults and Management Algorithms: CHEST Guideline and Expert Panel Report. Chest. 2018;153:196–209. doi: 10.1016/j.chest.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang AB, Oppenheimer JJ, Irwin RS, Adams TM, Altman KW, Azoulay E, et al. Managing Chronic Cough as a Symptom in Children and Management Algorithms: CHEST Guideline and Expert Panel Report. Chest. 2020;158:303–29. doi: 10.1016/j.chest.2020.01.042. [DOI] [PubMed] [Google Scholar]
- 8.Gibson PG, Wang G, McGarvey L, Vertigan AE, Altman KW, Birring SS. Treatment of Unexplained Chronic Cough: CHEST Guideline and Expert Panel Report. Chest. 2016;149:27–44. doi: 10.1378/chest.15-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morice A, Millqvist E, Bieksiene K, Birring S, Dicpinigaitis P, Ribas C, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55:1–20. doi: 10.1183/13993003.01136-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chamberlain Mitchell S, Birring SS, Garrod R. Nonpharmacological interventions for refractory chronic cough patients: Systematic review. Lung. 2014;192:75–85. doi: 10.1007/s00408-013-9508-y. [DOI] [PubMed] [Google Scholar]
- 11.Desai PP, Thomas PK, Abhayankar N, Vora A, Jaggi V, Jog P, et al. INDIan Consensus on the mAnagemenT of cOugh at pRimary care setting (INDICATOR) J Assoc Physicians India. 2023;71:62–77. doi: 10.5005/japi-11001-0275. [DOI] [PubMed] [Google Scholar]
- 12.Pacheco A, Cobeta I, Wagner C. Refractory Chronic Cough: New Perspectives in Diagnosis and Treatment. Arch Bronconeumol Engl Ed. 2013;49:151–7. doi: 10.1016/j.arbres.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Irwin LK, Kelchner L, Kathy Groves-Wright C, Suzanne Boyce C. Perceptual Evaluation of Voice Quality of Individuals with Dysphagia and Dysphonia [Internet] 2006. Available from: http://rave.ohiolink.edu/etdc/view?acc_num=ucin1148416348.
- 14.Ahmad SR, Iyer VN. The Evolving Clinical Practice of Chronic Cough. Mayo Clin Proc. 2022;97:1164–75. doi: 10.1016/j.mayocp.2022.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Varelas EA, Hwang C, Brown S, Chang J, Sataluri M, Kirke D, et al. Standardized Behavioral Treatment Improves Chronic Cough. J Voice. 2023 doi: 10.1016/j.jvoice.2022.11.017. S0892199722003691. [DOI] [PubMed] [Google Scholar]
- 16.Sundar KM, Stark AC, Hu N, Barkmeier-Kraemer J. Is laryngeal hypersensitivity the basis of unexplained or refractory chronic cough? ERJ Open Res. 2021;7:00793-2020. doi: 10.1183/23120541.00793-2020. Available from: https://openres.ersjournals.com/content/7/1/00793-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vertigan A, Haines J, Slovarp L. An Update on Speech Pathology Management of Chronic Refractory Cough. J Allergy Clin Immunol Pract. 2019;7:1756–61. doi: 10.1016/j.jaip.2019.03.030. [DOI] [PubMed] [Google Scholar]
- 18.Young EC, Smith JA. Quality of life in patients with chronic cough. Ther Adv Respir Dis. 2010;4:49–55. doi: 10.1177/1753465809358249. [DOI] [PubMed] [Google Scholar]
- 19.Birring SS, Prudon B, Carr AJ, Singh SJ. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ) Thorax. 2003;58:339–43. doi: 10.1136/thorax.58.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sathar NP, Bhat J. Profiling selected speech characteristics in individual with chronic cough [Master’s Dissertation] Kasturba Medical College, Mangalore, Manipal Academy of Higher Education; Manipal, India: 2021. [Google Scholar]
- 21.Solomon CG, Smith JA, Woodcock A. Clinical Practice Chronic Cough. N Engl J Med. 2016;375:1544–51. doi: 10.1056/NEJMcp1414215. [DOI] [PubMed] [Google Scholar]
- 22.Slovarp L, Jetté M, Gillespie A, Reynolds J, Barkmeier-Kraemer J. Evaluation and Management Outcomes and Burdens in Patients with Refractory Chronic Cough Referred for Behavioral Cough Suppression Therapy. Lung. 2021;199:263–71. doi: 10.1007/s00408-021-00442-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morice A, McGarvey L. Clinical Cough II: Therapeutic Treatments and Management of Chronic Cough. In: Fan Chung K, Widdicombe J, editors. Pharmacol Ther Cough. Berlin, Heidelberg: Springer; 2009. pp. 277–95. [DOI] [PubMed] [Google Scholar]
- 24.Patel AS, Watkin G, Willig B, Mutalithas K, Bellas H, Garrod R, et al. Improvement in health status following cough-suppression physiotherapy for patients with chronic cough. Chron Respir Dis. 2011;8:253–8. doi: 10.1177/1479972311422547. [DOI] [PubMed] [Google Scholar]
- 25.Chamberlain Mitchell S, Garrod R, Clark L, Douiri A, Parker SM, Ellis J, et al. Physiotherapy, and speech and language therapy intervention for patients with refractory chronic cough: a multicentre randomised control trial. Thorax. 2017;72:129–36. doi: 10.1136/thoraxjnl-2016-208843. [DOI] [PubMed] [Google Scholar]
- 26.Murry T, Branski RC, Yu K, Cukier-Blaj S, Duflo S, Aviv JE. Laryngeal sensory deficits in patients with chronic cough and paradoxical vocal fold movement disorder. The Laryngoscope. 2010;120:1576–81. doi: 10.1002/lary.20985. [DOI] [PubMed] [Google Scholar]
- 27.Ryan NM, Vertigan AE, Gibson PG. Chronic cough and laryngeal dysfunction improve with specific treatment of cough and paradoxical vocal fold movement. Cough. 2009;5:1–8. doi: 10.1186/1745-9974-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vertigan A, Theodoros D, Gibson P, Winkworth A. Efficacy of speech pathology management for chronic cough: a randomised placebo controlled trial of treatment efficacy. Thorax. 2006;61:1065–9. doi: 10.1136/thx.2006.064337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vertigan A, Theodoros D, Winkworth A. Chronic cough: A tutorial for speech-language pathologists. J Med Speech-Lang Pathol. 2007;15:189–206. [Google Scholar]
- 30.Ribeiro VV, Lopes LW, de Medeiros CMA, da Silva ACF, de Medeiros Neto AH, Behlau M. Effectiveness of the Therapy Program for Management of Chronic Cough: Preliminary Data From a Randomized Clinical Trial. Am J Speech Lang Pathol. 2022;31:1611–20. doi: 10.1044/2022_AJSLP-21-00381. [DOI] [PubMed] [Google Scholar]
- 31.Slovarp L, Vertigan A. Most patients with idiopathic chronic cough can benefit from a cough-suppression treatment provided by SLPs. But such treatment is often delayed if given at all. Why? ASHA Lead. 2019:50–6. [Google Scholar]
- 32.Slovarp L, Loomis BK, Glaspey A. Assessing referral and practice patterns of patients with chronic cough referred for behavioral cough suppression therapy. Chron Respir Dis. 2018;15:296–305. doi: 10.1177/1479972318755722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chamberlain Mitchell S, Ellis J, Ludlow S, Pandyan A, Birring SS. Non-pharmacological interventions for chronic cough: the past, present and future. Pulm Pharmacol Ther. 2019;56:29–38. doi: 10.1016/j.pupt.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Demirjian NL, Lever A, Yip H. Identifying Practice Gaps Among Otolaryngology Providers for the Treatment of Chronic Cough. OTO Open. 2024;8:e143. doi: 10.1002/oto2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Speech-Language-Hearing Association. Scope of practice in speech-language pathology [Internet] 2016. [cited 2023 Jun 14]; Available from: www.asha.org/policy/
- 36.Rehabilitation Council of India (RCI) Scope of Practice in Audiology and Speech-Language Pathology. 2016. [cited 2023 Jun 14]; Available from: https://www.ishaindia.org.in/pdf/Scope_of_Practice.pdf.
- 37.Yusoff MSB. ABC of Content Validation and Content Validity Index Calculation. Educ Med J. 2019;11:49–54. [Google Scholar]
- 38.Guleria R, Dhar R, Mahashur A, Ghoshal A, Jindal S, Talwar D, et al. Indian Consensus on Diagnosis of Cough at Primary Care Setting. J Assoc Physicians India. 2019;67:92–8. [PubMed] [Google Scholar]
- 39.Goland H, Thompson C. Cough management: the speech-language pathologist’s role in the treatment of chronic cough. In: Carroll TL, editor. Chronic Cough. San Diego, CA: Plural Publishing; 2019. pp. 143–72. [Google Scholar]
- 40.Vertigan A, Kapela S, Gibson P. Chronic cough in Vocal Cord Dysfunction: Description of a clinical entity. Respir Med. 2020;168:105990. doi: 10.1016/j.rmed.2020.105990. [DOI] [PubMed] [Google Scholar]
- 41.Brignall K, Jayaraman B, Birring SS. Quality of Life and Psychosocial Aspects of Cough. Lung. 2008;186:55–8. doi: 10.1007/s00408-007-9034-x. [DOI] [PubMed] [Google Scholar]
- 42.French CL, Irwin RS, Curley FJ, Krikorian CJ. Impact of Chronic Cough on Quality of Life. Arch Intern Med. 1998;158:1657–61. doi: 10.1001/archinte.158.15.1657. [DOI] [PubMed] [Google Scholar]
- 43.Dailey SH, Mai JP. Chronic Cough. San Diego, CA 92123: Plural Publishing Inc; 2019. Overview of chronic cough and its impact on health care; pp. 1–20. [Google Scholar]
- 44.Hulme K, Deary V, Dogan S, Parker SM. Psychological profile of individuals presenting with chronic cough. ERJ Open Res. 2017;3:00099. doi: 10.1183/23120541.00099-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McGarvey LP, Carton C, Gamble LA, Heaney LG, Shepherd R, Ennis M, et al. Prevalence of psychomorbidity among patients with chronic cough. Cough. 2006;2:4. doi: 10.1186/1745-9974-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Blasio F, Virchow JC, Polverino M, Zanasi A, Behrakis PK, Kilinç G, et al. Cough management: A practical approach. Cough. 2011;7:1–12. doi: 10.1186/1745-9974-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McGarvey LP. Does idiopathic cough exist? Lung. 2008;186:78–81. doi: 10.1007/s00408-007-9048-4. [DOI] [PubMed] [Google Scholar]
- 48.Morice A. Epidemiology of cough. In: Chung KF, Widdicombe JG, Boushey HA, editors. Cough Causes Mech Ther Victoria. Australia: Blackwell Publishing Ltd; 2003. pp. 11–6. [Google Scholar]
- 49.Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:59S–62S. doi: 10.1378/chest.129.1_suppl.59S. [DOI] [PubMed] [Google Scholar]
- 50.Dornelas R, Casmerides MCB, da Silva RC, Victória dos Anjos Souza M, Pereira LT, Ribeiro VV, et al. Clinical Parameters of the Speech-Language Pathology Assessment of the Chronic Cough: A Scoping Review. J Voice. 2022. Available from: https://www.sciencedirect.com/science/article/pii/S0892199721004380. [DOI] [PubMed]
- 51.Boulet L-P, Coeytaux RR, McCrory DC, French CT, Chang AB, Birring SS, et al. Tools for Assessing Outcomes in Studies of Chronic Cough. Chest. 2015;147:804–14. doi: 10.1378/chest.14-2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cho PSP, Birring SS, Fletcher HV, Turner RD. Methods of Cough Assessment. J Allergy Clin Immunol Pract. 2019;7:1715–23. doi: 10.1016/j.jaip.2019.01.049. [DOI] [PubMed] [Google Scholar]
- 53.Chamberlain Mitchell S, Garrod R, Birring SS. Cough suppression therapy: Does it work? Pulm Pharmacol Ther. 2013;26:524–7. doi: 10.1016/j.pupt.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 54.Ribeiro VV, Lopes LW, Behlau M. Presentation of the Therapy Program for Management of Chronic Cough. CODAS. 2021;33:1–5. doi: 10.1590/2317-1782/20202020057. [DOI] [PubMed] [Google Scholar]
- 55.Shisler R, Basilakos A. Hot or Not?: A Survey Regarding Knowledge and Use of Complementary and Alternative Practices in Speech-Language Pathology. Contemp Issues Commun Sci Disord. 2014;41:235–51. [Google Scholar]
- 56.Sinha A, Porter T, Wilson A. The Use of Online Health Forums by Patients With Chronic Cough: Qualitative Study. J Med Internet Res. 2018;20:e19. doi: 10.2196/jmir.7975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Widdicombe J, Ernst E. Pharmacol Ther Cough. Berlin, Heidelberg: Springer; 2009. Clinical Cough V: Complementary and Alternative Medicine: Therapy of Cough; pp. 321–42. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the corresponding author.


