Abstract
Objective: To evaluate the efficacy of laparoscopic choledocholithotomy with either an indwelling T-tube or primary suture in treating cholecystolithiasis complicated by choledocholithiasis. Methods: We conducted a retrospective analysis of 133 patients with cholecystolithiasis complicated by choledocholithiasis treated at Inner Mongolia Aerospace Medical Baogang Hospital from March 2020 to March 2023. Patients were divided into a control group (laparoscopic choledocholithotomy with T-tube placement) and an observation group (laparoscopic choledocholithotomy with primary suture). We compared general and surgery-related data between groups. Factors correlated with favorable postoperative outcomes were identified using univariate and multivariate logistic regression analyses. Results: The observation group exhibited significantly shorter surgical times, faster intestinal function recovery, reduced postoperative hospital stays, and lower total hospitalization costs compared to the control group (all P < 0.05). No significant differences were observed in postoperative total bilirubin (TBIL), aspartate aminotransferase (AST), or alanine aminotransferase (ALT) levels between the groups (all P > 0.05). Both primary suture technique and the absence of postoperative complications were independent predictors of favorable outcomes. Conclusion: Laparoscopic choledocholithotomy with primary suture is associated with shorter operation times, reduced medical costs, decreased hospitalization duration, and quicker gastrointestinal recovery compared to the traditional T-tube approach. This method is safe and feasible, provided clinicians are well-versed in its indications.
Keywords: Laparoscopic choledocholithotomy, indwound T-tube, primary suture, cholecystolithiasis
Introduction
Gallstone disease is prevalent in hepatobiliary surgery, with an incidence of approximately 10% to 20% in adults [1-3]. Notably, 10% to 15% of these patients also develop common bile duct stones [4]. A study by Park et al. followed 594 patients with common bile duct stones managed conservatively over a period of 0 to 4 years, revealing that 25.3% experienced complications such as cholangitis and bile duct obstruction [5]. In contrast, the complication rate for those undergoing stone clearance was 12.7% (OR=0.44, 95% CI: 0.35-0.55). The risk of adverse outcomes escalates with the size of the stone. Specifically, stones smaller than 4 mm carry a 6% risk of complications, while the risk increases to 9% for larger stones (OR=0.52, 95% CI: 0.34-0.79) [6]. Thus, prompt removal of common bile duct stones through endoscopic or surgical interventions is crucial, even in asymptomatic cases, to minimize complication risks and improve patient quality of life.
Increasingly, clinicians are favoring direct suturing of the common bile duct post-choledochal stone extraction [7,8]. This one-stage suturing approach facilitates early resumption of gastrointestinal activities, dietary intake, and mobility, enhancing postoperative recovery and reducing risks such as lung infections or lower limb thrombosis associated with prolonged bed rest. Moreover, it obviates the need for a second hospitalization for tube removal, thereby cutting costs and significantly improving patient convenience. Evidence suggests that the routine use of T-tubes post-laparoscopic choledochotomy may not offer clinical benefits and could lead to complications, thereby diminishing the advantages of laparoscopic interventions [9-12]. A systematic review and meta-analysis supports the superiority of one-stage bile duct suturing over T-tube placement in terms of efficacy and safety for eligible patients [13]. The one-stage suture technique for choledochotomy, a novel approach detailed in recent studies, involves a single incision in the common bile duct for stone removal, followed by immediate suture closure. This method is quicker and potentially reduces postoperative complications compared to conventional multi-step techniques [14]. Currently, there is no consensus on the preferred method post-laparoscopic common bile duct exploration (LCBDE): one-stage suture versus T-tube drainage. Practices vary among physicians and medical institutions globally, reflecting a lack of standardized guidelines.
This study aims to compare clinical outcomes of different surgical approaches following laparoscopic choledocholithotomy plus LCBDE in patients with gallbladder and common bile duct stones. The findings are intended to assist clinicians in making informed surgical decisions and to contribute to the standardization of treatment protocols.
Methods and materials
Patient selection and study design
In this retrospective analysis, 133 patients diagnosed with cholecystolithiasis complicated by choledocholithiasis were evaluated at Inner Mongolia Aerospace Medical Baogang Hospital from March 2020 to March 2023. Based on the therapeutic approach, patients were divided into two groups: 64 patients who underwent laparoscopic choledocholithotomy with T-tube placement (control group), while another 69 underwent the same procedure followed by primary suture (observation group). This study received approval from the Ethics Committee of Inner Mongolia Aerospace Medical Baogang Hospital.
Inclusion and exclusion criteria
Inclusion criteria: (1) Patients who underwent laparoscopic choledocholithotomy [15]. (2) Age ≥ 18 years. (3) Complete clearance of all stones, with no residual stones. (4) Common bile duct diameter ≥ 8 mm. (5) All procedures were performed laparoscopically without any additional incisions. (6) Complete clinical data available for each patient.
Exclusion criteria: (1) Patients with complex intrahepatic bile duct stones. (2) Severe comorbidities including cardiovascular and cerebrovascular diseases, diabetes, hypertension, hepatorenal syndrome, and severe thyroid disorders. (3) Presence of malignant tumors, systemic infections, or autoimmune diseases. (4) Females who were pregnant or lactating. (5) Severe inflammation of the common bile duct preventing laparoscopic access. (6) Inadequate common bile duct diameter for choledochoscopic intervention. (7) Postoperative pathological findings indicative of gallbladder or bile duct cancer. (8) Obstruction of the distal common bile duct detected during intraoperative choledochoscopy. (9) Absence of concurrent intraoperative cholecystectomy. (10) Incomplete patient clinical data.
Methods
In this group, patients underwent laparoscopic choledocholithotomy with T-tube insertion using a T-tube (Product ID: 1009387, Shanghai Bikang Medical Equipment Co., Ltd.). After successful induction of anesthesia, the patient was positioned supine on the operating table. The operative field was sterilized with iodophor and draped using four small sheets, two medium sheets, followed by a large sheet. Surgical instruments were connected, and the abdomen was prepared for entry. An incision was made 1 cm below the navel, and the abdominal cavity was insufflated with CO2 gas to maintain an intra-abdominal pressure of 12-14 mmHg.
Trocar placement followed the initial incision. The abdominal cavity was inspected laparoscopically to rule out any intestinal injuries from trocar insertion, and three additional trocars were positioned. Adhesions around the gallbladder were dissected using an ultrasonic scalpel, and both the anterior and posterior triangles were carefully separated to expose the cystic duct and artery. These were clipped and severed with the ultrasonic knife.
The anterior wall of the common bile duct was lifted, and an incision was made at its upper part using an electrosurgical hook. A choledochoscope was inserted to visualize and remove stones using a stone retrieval basket. The bile duct was then flushed. Depending on the diameter of the bile duct, an appropriately sized T-tube was placed. The choledochotomy was sutured closed, and a drainage tube was placed in the hepatorenal recess, exiting through the right anterior axillary line and secured in place.
The procedure concluded with securing the T-tube and transferring the patient to a general ward or intensive care unit based on their level of consciousness post-operatively.
In the observation group, patients underwent laparoscopic choledocholithotomy followed by primary suture. The preparatory steps prior to suturing the common bile duct were similar to those used for T-tube placement (Product ID: 1009387, Shanghai Bikang Medical Equipment Co., Ltd.). The common bile duct was sutured closed using absorbable sutures, the cystic duct was sealed with absorbable clips, and the gallbladder was removed using an ultrasonic scalpel.
To prevent postoperative abdominal adhesions, the abdominal cavity was irrigated with an anti-adhesion solution at the end of the surgery. An abdominal drainage tube was placed and secured on the right side. Postoperatively, patients were transferred to the general ward or intensive care unit based on their vital signs and level of consciousness.
Postoperative management included first-level nursing care, cardiac monitoring, administration of anti-inflammatory medications, pain relief, nutritional support, and rehydration. Symptomatic treatment was provided for postoperative symptoms such as pain and vomiting. The volume and color of the abdominal drainage were monitored, with the drainage tube being removed when output was consistently below 30 mL/day.
For those with an indwelling T-tube, the tube was secured to prevent displacement, and the drainage was monitored for any abnormalities. T-tube imaging was conducted approximately 7 days post-surgery to check for residual stones; if none were found, the T-tube was left in place for three weeks. Patients were discharged with the T-tube and returned for a follow-up imaging. If no stones were detected, the T-tube was removed.
Patients were encouraged to ambulate early to prevent complications such as deep vein thrombosis and pulmonary complications from prolonged immobility. Blood analysis and biochemistry tests were repeated three days post-operation to assess the patient’s ion balance and nutritional status.
Outcome measures
This section compares key metrics between the two patient groups, including demographic information (age, gender), preoperative comorbidities, stone characteristics (number and diameter of common bile duct stones), and surgical details (operation time, intraoperative blood loss). Postoperative data reviewed include gastrointestinal recovery time, timing of abdominal drainage tube removal, length of postoperative hospital stay, and total hospitalization costs. Additionally, clinical outcomes one week post-intervention, incidence of postoperative complications, and follow-up data after hospital discharge were analyzed.
Efficacy Evaluation Criteria [16]: Remarkable Effect: Complete resolution of upper abdominal tenderness, patient’s vital signs within normal ranges, and no residual stones on imaging.
Effective: Significant improvement in upper abdominal tenderness, vital signs mostly within normal ranges, and no residual stones on imaging.
Invalid: No improvement or worsening of upper abdominal tenderness, vital signs outside normal ranges, and presence of residual stones on imaging. Total efficacy rate = (markedly effective + effective)/cases × 100%.
Statistical analysis
Data were processed and analyzed using SPSS software version 27.0. The comparison of continuous variables among groups was performed using ANOVA, with post-hoc testing by the LSD-t method. Categorical data were compared using the chi-squared test, while ordinal data employed the rank-sum test. Pearson’s correlation test was used for correlation analysis. Factors influencing postoperative outcomes were evaluated using univariate and multivariate logistic regression analyses. A p-value of less than 0.05 was considered statistically significant.
Results
Comparison of clinical data between the two groups
No significant differences were observed in gender, age, body mass index, stone size, common bile duct diameter, number of stones, hypertension, diabetes, coronary heart disease, fatty liver, preoperative anemia, preoperative hypoalbuminemia, and history of abdominal and pelvic surgery within each group (all P > 0.05) (Table 1).
Table 1.
Comparison of clinical data between the two groups
| Observation group (n=69) | Control group (n=64) | Z/χ2 | P | |
|---|---|---|---|---|
| Age (years) | 50.57 (39.77-71.44) | 53.74 (33.41-73.44) | -1.214 | 0.264 |
| Sex | 0.612 | 0.484 | ||
| Male (n%) | 31 (%) | 33 (60.7%) | ||
| Female (n%) | 38 (%) | 31 (39.3%) | ||
| Body mass indexes | 24.10 (23.04-26.12) | 24.46 (22.98-26.71) | -0.034 | 0.847 |
| Stone size (cm2) | 6.50 (5.00-8.00) | 7 (5.00-10.00) | -1.926 | 0.074 |
| Common bile duct diameter (cm2) | 13.00 (11.00-13.00) | 12.00 (10.00-12.00) | -1.842 | 0.077 |
| Number of stones | 3.00 (1.00-3.00) | 3.00 (1.00-4.00) | -0.347 | 0.881 |
| Hypertension | 29 (42.03%) | 27 (42.19%) | 0.004 | 0.974 |
| Diabetes | 13 (18.84%) | 14 (21.88%) | 0.074 | 0.741 |
| Coronary heart disease | 13 (18.84%) | 7 (10.94%) | 0.714 | 0.369 |
| Fatty liver | 11 (15.94%) | 9 (14.06%) | 0.000 | 0.941 |
| Preoperative anemia | 13 (18.84%) | 7 (10.94%) | 0.457 | 0.541 |
| Preoperative hypoalbuminemia | 7 (10.14%) | 3 (4.69%) | 0.067 | 0.897 |
| History of abdominal and pelvic surgery | 8 (11.59%) | 1 (1.56%) | 1.897 | 0.147 |
Comparison of intraoperative and postoperative conditions between the two groups
The observation group experienced significantly shorter surgical time, intestinal function recovery time, postoperative hospitalization time, and total hospitalization cost compared to the control group (all P < 0.05). There were no significant differences in intraoperative bleeding volume and drainage tube removal time between the groups (P > 0.05) (Table 2).
Table 2.
Comparison of intraoperative and postoperative conditions between the two groups of patients
| Indicator | Observation group (n=69) | Control group (n=64) | Z/t | P |
|---|---|---|---|---|
| Surgical time (min) | 118.50 (111.00-142.00) | 156.00 (124.25-184.50) | -3.512 | 0.001 |
| Intraoperative bleeding volume (mL) | 21.00 (10.00-21.00) | 22.00 (11.00-22.00) | -0.784 | 0.425 |
| Intestinal function recovery time (Days) | 2.12±0.98 | 2.67±1.14 | 2.841 | 0.005 |
| Postoperative hospital stays (Days) | 7.00 (6.00-8.00) | 8.00 (3.00-9.00) | -6.654 | 0.004 |
| Removal time of drainage tube (Days) | 5.00 (4.00-7.00) | 6.00 (4.00-8.00) | -0.842 | 0.384 |
| Total hospitalization cost | 4.50 (3.84-4.98) | 5.21 (4.46-7.21) | -4.571 | 0.004 |
Comparison of biochemical indexes between the two groups
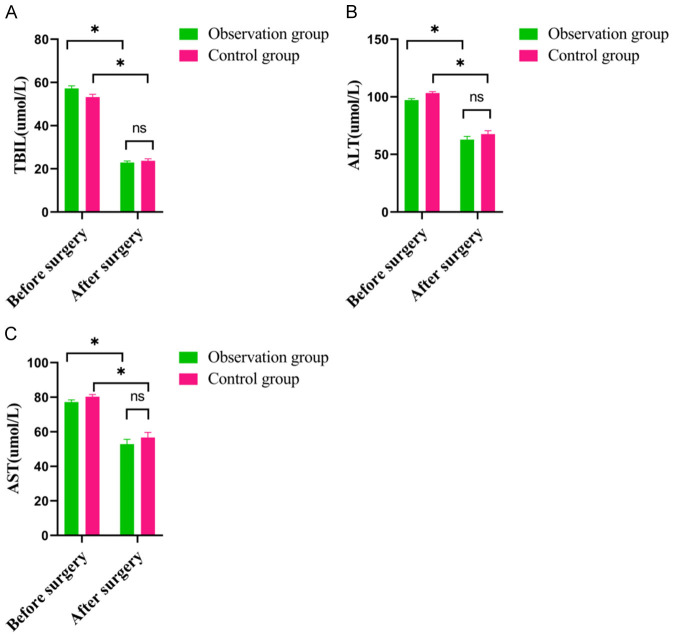
Serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and total bilirubin (TBIL) are presented in Figure 1. There were no significant differences in TBIL, ALT, and AST levels before surgery between the groups (all P > 0.05). However, these levels were significantly reduced post-surgery in both groups (P < 0.05), with no significant differences between the groups postoperatively (P > 0.05).
Figure 1.
Comparison of biochemical indexes between the two groups. A: TBIL; B: ALT; C: AST. TBIL: total bilirubin; AST: aspartate aminotransferase; ALT: alanine aminotransferase. *P < 0.05 indicating the difference is statistically significant.
Comparison of postoperative complications between the two groups
There were no severe complications such as biliary peritonitis, biliary bleeding, septic shock, or death in either group. Additionally, no significant differences were noted in bile leakage, residual stones in the common bile duct, incision infection, T-tube detachment, electrolyte disorder, incision fat liquefaction, or pulmonary infection between the groups (P > 0.05) (Table 3).
Table 3.
Comparison of postoperative complications between the two groups
| Indicator | Observation group (n=69) | Control group (n=64) | χ2 | P |
|---|---|---|---|---|
| Bile leakage | 7 (10.14%) | 1 (1.56%) | 1.847 | 0.124 |
| Residual stones in the common bile duct | 0 (0.00%) | 2 (3.13%) | 0.998 | 1.000 |
| Incision infection | 0 (0.00%) | 1 (1.56%) | 0.887 | 1.000 |
| T-tube detachment | 0 (0.00%) | 1 (1.56%) | 0.968 | 1.000 |
| Electrolyte disorder | 3 (4.35%) | 1 (1.56%) | 0.977 | 0.541 |
| Incision fat liquefaction | 3 (4.35%) | 1 (1.56%) | 0.909 | 0.471 |
| Pulmonary infection | 5 (7.25%) | 1 (1.56%) | 0.911 | 0.147 |
| Overall complications | 15 (21.74%) | 6 (9.38%) | 2.151 | 0.213 |
Comparison of clinical efficacy between the two groups
The total effective rate was 94.2% in the observation group, significantly higher than the 84.3% observed in the control group after a one-week intervention, with a statistically significant difference (χ2=8.165, P < 0.05) (Table 4).
Table 4.
Comparison of clinical efficacy between the two groups
| Group | Number of cases | Remarkable | Effective | Invalid | Total efficacy rate |
|---|---|---|---|---|---|
| Observation group | 69 | 35 (53.8%) | 30 (46.2%) | 4 (5.8%) | 65 (94.2%) |
| Control group | 64 | 28 (43.74%) | 26 (40.63%) | 10 (15.63%) | 54 (84.3%) |
| χ2 | - | 6.896 | 5.372 | 2.578 | 8.165 |
| P | - | 0.042 | 0.045 | 0.095 | 0.024 |
Univariate and multivariate regression analysis
Univariate analysis identified primary suture, drainage tube removal time, and absence of postoperative complications as factors correlated with favorable postoperative prognosis in patients with cholecystolithiasis complicated by choledocholithiasis (all P < 0.05). The Cox proportional hazards regression model indicated that primary suture and absence of postoperative complications were independent factors affecting favorable postoperative prognosis (Tables 5 and 6).
Table 5.
Univariate analysis
| OR (95% CI) | P | β | SE | Wals | |
|---|---|---|---|---|---|
| Age | |||||
| ≥ 65 | 1.751 (0.487-2.648) | 0.794 | 0.515 | 0.296 | 5.064 |
| < 65 | 1.000 | 0.984 | - | - | 13.546 |
| Gender | |||||
| Female | 1.364 (0.678-2.384) | 0.524 | 2.037 | 0.909 | 5.024 |
| Male | 1.000 | 0.556 | - | - | 11.981 |
| Fatty liver | 1.024 (0.988-1.248) | 0.109 | 0.661 | 0.226 | 8.514 |
| Preoperative anemia | 3.507 (0.824-2.259) | 0.119 | 0.891 | 0.484 | 0.149 |
| Preoperative hypoalbuminemia | 3.568 (0.607-9.608) | 0.113 | -0.459 | 0.801 | 0.324 |
| Hypertension | 0.814 (0.354-1.821) | 0.451 | 1.012 | 0.243 | 11.139 |
| Diabetes | 2.013 (1.712-4.925) | 0.334 | 1.002 | 0.223 | 9.930 |
| Coronary heart disease | 1.563 (0.748-3.488) | 0.172 | 0.989 | 0.119 | 9.928 |
| Primary suture | 3.927 (1.647-9.678) | 0.007 | 1.287 | 0.276 | 9.589 |
| Surgical time | 0.984 (0.324-1.249) | 0.827 | 2.038 | 0.283 | 8.498 |
| Intraoperative bleeding volume | 16.437 (6.829-29.279) | 0.942 | 2.009 | 0.210 | 7.398 |
| Intestinal function recovery time | 1.227 (0.677-2.358) | 0.342 | 0.641 | 0.106 | 10.514 |
| Postoperative hospital stays | 4.224 (0.298-12.791) | 0.234 | 0.791 | 0.354 | 8.349 |
| Total hospitalization cost | 2.632 (0.174-6.768) | 0.328 | 1.412 | 0.143 | 10.139 |
| Removal time of drainage tube | 1.548 (0.643-5.688) | 0.641 | 1.022 | 0.323 | 8.930 |
| Postoperative complication | 0.572 (0.437-1.782) | < 0.001 | 0.689 | 0.219 | 8.928 |
Table 6.
Multivariate regression analysis
| Factor | β | SE | Wals | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Primary suture | ||||||
| No | - | - | 3.546 | 0.059 | 1 | |
| Had | 0.515 | 0.296 | 15.064 | 0.023 | 4.568 | 1.647-9.678 |
| Removal time of drainage tube | ||||||
| No | - | - | 1.981 | 0.104 | 1 | |
| Had | 0.891 | 0.484 | 10.149 | 0.084 | 2.568 | 1.647-9.678 |
| Postoperative complication | ||||||
| No | - | - | 3.981 | 0.304 | 1 | |
| Had | 2.037 | 0.909 | 15.024 | 0.028 | 0.668 | 0.575-1.878 |
Discussion
With advances in medical technology and clinician experience, one-stage suturing after choledochotomy is increasingly employed in clinical settings [17]. Unlike T-tube placement, one-stage suturing allows earlier patient mobilization, though it demands stricter indications. Despite the lack of consensus on bile duct management post-laparoscopic choledochotomy and lithotripsy, recent evidence suggests that T-tube drainage offers no clinical benefit and is generally discouraged [18,19]. The safety and efficacy of direct one-stage suturing of the common bile duct have been supported by numerous national and international studies [20-24].
Increasingly, clinicians opt for direct one-stage suturing post-laparoscopic choledochotomy, which prevents bile leakage, facilitates quicker recovery of digestive functions, reduces hospitalization costs, and shortens surgery duration [25]. This approach aligns with the principles of enhanced recovery surgery and is suitable even for elderly patients. Comparative studies and meta-analyses have confirmed that one-stage suturing is as safe and effective as T-tube drainage, including in emergency procedures [26-28]. Moreover, long-term outcomes show lower rates of stone recurrence and no biliary strictures with one-stage suturing [29]. Therefore, one-stage suturing of the common bile duct after laparoscopic choledochotomy and lithotripsy is a safe and effective alternative to T-tube drainage.
Junsheng et al. [30] conducted six randomized controlled trials involving 604 patients with combined gallbladder and common bile duct stones, comparing one-stage suturing (307 patients) to T-tube drainage (297 patients). The results indicated that one-stage suturing reduced operative times, hospitalization costs, and the length of postoperative hospital stays. Additionally, there were no significant differences in the incidence of postoperative complications such as bile leakage and residual stones between the two groups. Analysis of data from 133 patients further supported that one-stage suturing was superior in reducing postoperative hospitalization time, operation time, hospitalization costs, and the time to recovery of intestinal function (P < 0.05).
The lack of a significant difference in intraoperative bleeding and postoperative drain removal time suggests comparable safety profiles for both methods. The primary advantage of one-stage suturing is the elimination of the need for T-tube cholangiography and hospital re-admissions for T-tube removal, thus reducing overall hospitalization costs. Earlier bile flow back to the intestine after one-stage suturing promotes quicker intestinal peristalsis, enabling patients to resume eating sooner and reducing anesthesia duration. This reduction in operation time decreases the risk of infection, postoperative thrombosis, and respiratory and cardiac complications, particularly beneficial for elderly patients with cardiovascular risks. Overall, the findings reveal no significant differences in the incidence of postoperative complications such as bile leakage, residual stones, T-tube detachment, and overall complications between the two groups.
Laparoscopic common bile duct exploration with stone extraction and primary T-tube closure effectively reduces bile leakage post-surgery in patients with gallbladder and common bile duct stones. This procedure utilizes a laparoscope to access the common bile duct, removes the stones, and secures the duct with a T-tube, which ensures proper closure and facilitates drainage during healing [31]. Addressing both gallbladder and common bile duct stones concurrently significantly diminishes the risks of complications like bile leakage and bile duct injuries.
However, this study has several limitations. Firstly, it relies on retrospective data, which may be incomplete or biased. The absence of randomization may introduce confounding variables, potentially affecting the validity of the results. Secondly, the study’s duration was limited, and it did not evaluate the long-term efficacy of the treatment. Lastly, being a single-center study with a small sample size could introduce selection bias. Future research should aim to expand the sample size and extend the duration of follow-up to more accurately assess the long-term outcomes.
Despite these limitations, primary suturing aligns with the principles of accelerated rehabilitation surgery. Compared to T-tube drainage, primary suturing offers shorter operative times, reduced medical costs, decreased hospitalization durations, and quicker gastrointestinal recovery. It is a safe and feasible option for clinicians, provided they are adept at its indications, offering significant clinical benefits to patients.
Disclosure of conflict of interest
None.
References
- 1.Grigor’eva IN, Romanova TI. Gallstone disease and microbiome. Microorganisms. 2020;8:835. doi: 10.3390/microorganisms8060835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haal S, Guman MSS, Bruin S, Schouten R, van Veen RN, Fockens P, Dijkgraaf MGW, Hutten BA, Gerdes VEA, Voermans RP. Risk factors for symptomatic gallstone disease and gallstone formation after bariatric surgery. Obes Surg. 2022;32:1270–1278. doi: 10.1007/s11695-022-05947-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gutt C, Schläfer S, Lammert F. The treatment of gallstone disease. Dtsch Arztebl Int. 2020;117:148–158. doi: 10.3238/arztebl.2020.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simon M, Hassan IN, Ramasamy D, Wilson D. Primary choledocholithiasis 15 years postcholecystectomy. Case Rep Med. 2020;2020:3265010. doi: 10.1155/2020/3265010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park CH. The management of common bile duct stones. Korean J Gastroenterol. 2018;71:260–263. doi: 10.4166/kjg.2018.71.5.260. [DOI] [PubMed] [Google Scholar]
- 6.Masuda S, Koizumi K, Shionoya K, Jinushi R, Makazu M, Nishino T, Kimura K, Sumida C, Kubota J, Ichita C, Sasaki A, Kobayashi M, Kako M, Haruki U. Comprehensive review on small common bile duct stones. World J Gastroenterol. 2023;29:1955–1968. doi: 10.3748/wjg.v29.i13.1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katayose Y, Yamamoto K, Takami K. Management of common bile duct stones. Nihon Shokakibyo Gakkai Zasshi. 2021;118:296–302. doi: 10.11405/nisshoshi.118.296. [DOI] [PubMed] [Google Scholar]
- 8.Mohseni S, Bass GA, Forssten MP, Casas IM, Martin M, Davis KA, Haut ER, Sugrue M, Kurihara H, Sarani B, Cao Y, Coimbra R. Common bile duct stones management: a network meta-analysis. J Trauma Acute Care Surg. 2022;93:e155–e165. doi: 10.1097/TA.0000000000003755. [DOI] [PubMed] [Google Scholar]
- 9.Pallaneeandee NK, Govindan SS, Zi Jun L. Evaluation of the common bile duct (CBD) diameter after laparoscopic cholecystectomy (LC) and laparoscopic common bile duct exploration (LCBDE): a retrospective study. Surg Laparosc Endosc Percutan Tech. 2023;33:62–68. doi: 10.1097/SLE.0000000000001135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Temara H, Morreau M, Waddell O, Maloney J, Jauffret B. How to perform laparoscopic common bile duct exploration through a transverse choledochotomy. ANZ J Surg. 2023;93:1017–1020. doi: 10.1111/ans.18349. [DOI] [PubMed] [Google Scholar]
- 11.Li G, Zhang J, Cai J, Yu Z, Xia Q, Ding W. Enhanced recovery after surgery in patients undergoing laparoscopic common bile duct exploration: a retrospective study. Medicine (Baltimore) 2022;101:e30083. doi: 10.1097/MD.0000000000030083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu B, Luo T, Yang T, Wang S, Meng H, Gong J, Zhou B, Zheng W, Song Z. Laparoscopic common bile duct exploration with primary closure is beneficial for patients with previous upper abdominal surgery. Surg Endosc. 2022;36:1053–1063. doi: 10.1007/s00464-021-08371-8. [DOI] [PubMed] [Google Scholar]
- 13.Rudiman R, Hanafi RV, Almawijaya, Halim F. Complications of biliary stenting versus T-tube insertion after common bile duct exploration: a systematic review and meta-analysis. PLoS One. 2023;18:e0280755. doi: 10.1371/journal.pone.0280755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu H, Wu L, Yuan R, Wang Y, Liao W, Lei J, Shao J. Learning curve for performing choledochotomy bile duct exploration with primary closure after laparoscopic cholecystectomy. Surg Endosc. 2018;32:4263–4270. doi: 10.1007/s00464-018-6175-3. [DOI] [PubMed] [Google Scholar]
- 15.De Silva HM, Howard T, Bird D, Hodgson R. Outcomes following common bile duct exploration versus endoscopic stone extraction before, during and after laparoscopic cholecystectomy for patients with common bile duct stones. HPB (Oxford) 2022;24:2125–2133. doi: 10.1016/j.hpb.2022.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Nadeem K, Tarar JM, Rashid M. Posterior first infundibular dissection: another safe approach in laparoscopic cholecystectomy. Pakistan Journal of Medical and Health Sciences. 2022;16:359–360. [Google Scholar]
- 17.Shen H, Sheng Y, Jiang H, Lu J, Wang Y. The feasibility of “one-stage and two classification” method to treat concomitant gallbladder stones and common bile duct stones. Chinese Journal of Hepatobiliary Surgery. 2017;23:526–529. [Google Scholar]
- 18.Chuang SH. Routine single-incision laparoscopic cholecystectomy and/or single-incision laparoscopic common bile duct exploration for elderly patients: an observational comparative study. J Am Coll Surg. 2022;235:S54. [Google Scholar]
- 19.Zhen W, Xu-Zhen W, Nan-Tao F, Yong L, Wei-Dong X, Dong-Hui Z. Primary closure versus T-tube drainage following laparoscopic common bile duct exploration in patients with previous biliary surgery. Am Surg. 2021;87:50–55. doi: 10.1177/0003134820947396. [DOI] [PubMed] [Google Scholar]
- 20.Wu D, Jin W, Zhang Y, An Y, Chen X, Chen W. Primary suture of the common bile duct: continuous or interrupted? J Laparoendosc Adv Surg Tech A. 2022;32:390–394. doi: 10.1089/lap.2021.0215. [DOI] [PubMed] [Google Scholar]
- 21.Lu J, Zhang X, Zeng C, Gu JT, Cai H. Clinical analysis of laparoscopic common bile duct primary suture and T-tube drainage in the treatment of common bile duct stones. J Laparoendosc Adv Surg Tech A. 2023;33:622–625. doi: 10.1089/lap.2022.0485. [DOI] [PubMed] [Google Scholar]
- 22.He Y, Cai Y, Tang H, Zhu L, Chen Q. Analysis of risk factors of bile leakage in patients after laparoscopic common bile duct exploration and primary suture. Int J Surg. 2017;44:733–736. [Google Scholar]
- 23.Lu W, Sun G, Bai J, Shi Y, Zhang D. Clinical research of laparoscopic common bile duct exploration with primary suture and T tube drainage in the management of choledocholithiasis. Int J Surg. 2019;46:667–673. [Google Scholar]
- 24.Ma X, Cai S. The outcome and safety in laparoscopic common bile duct exploration with primary suture versus T-tube drainage: a meta-analysis. Appl Bionics Biomech. 2023;2023:7300519. doi: 10.1155/2023/7300519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yin Y, He K, Xia X. Comparison of primary suture and T-tube drainage after laparoscopic common bile duct exploration combined with intraoperative choledochoscopy in the treatment of secondary common bile duct stones: a single-center retrospective analysis. J Laparoendosc Adv Surg Tech A. 2022;32:612–619. doi: 10.1089/lap.2021.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu T, Zhu K, Sun J, Liu C, Lin H, Zhang R. The clinical effect of primary duct closure and T-tube drainage: a propensity score matched study. Asian J Surg. 2023;46:3046–3051. doi: 10.1016/j.asjsur.2022.09.132. [DOI] [PubMed] [Google Scholar]
- 27.Liu W, Liu D, Liu J, Li K, Xu D, Wang Y, Tong X, Zheng Y, Jiang H. Primary closure versus T-tube drainage following laparoscopic common bile duct exploration in acute cholangitis cases. Int J Surg. 2017;44:240–243. [Google Scholar]
- 28.Sui X, Sui Z, Gu X, Ding M, Miao G. Primary closure combined with C-tube drainage through cystic duct after laparoscopic common bile duct exploration is safe and feasible for patients. Front Surg. 2022;9:972490. doi: 10.3389/fsurg.2022.972490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qi Y, Jin L, Lei K, Hao J, Zhao W, Gao X. Clinical analysis of laparoscopic common bile duct exploration with free T-tube in the treatment of common bile duct stones. Chin J Oper Proc Gen Surg (Electronic Edition) 2019;13:646–648. [Google Scholar]
- 30.Cao J, Chen M, Zhang B, Cai X. Is safe and efficient by intraoperative endoscopic nasobiliary drainage over primary closure of the common bile duct for cholecystolithiasis combined with common bile duct stones: a meta-analysis. Ann Oncol. 2019;12:1–12. [Google Scholar]
- 31.Zhu Y, Dong J, Yang S. A retrospective study on 1 152 patients with common bile duct stones. Chinese Journal of Hepatobiliary Surgery. 2019;25:579–581. [Google Scholar]