Abstract
The COVID-19 pandemic has highlighted the need for research about communicating with populations who have limited English proficiency in the United States during infectious disease outbreaks. These populations have experienced significantly worse health outcomes during emergencies, including the COVID-19 pandemic, and evidence-based risk communications are critical to protecting their health. To support improved development of emergency communications for these communities, we conducted a scoping review that examined the extent of research available, with an intent to identify which communications topics are covered in the literature and where research gaps exist. Following the JBI framework, with reporting guided by the PRISMA extension for scoping reviews, 6 electronic databases were systematically searched in October 2022. The inclusion criteria for articles selected were: data collected between 2009 and 2022, published in English, and focused on communications pertaining to emergency infectious disease outbreaks (eg, H1N1 influenza, Zika virus, COVID-19) for populations with limited English proficiency. Of 2,049 articles identified through the search, 31 met the inclusion criteria and were selected for review. We identified major limitations in the evidence base: a majority of studies were conducted only among Spanish speakers or during the COVID-19 pandemic, and most used qualitative or nonrandom samples. Most studies documented basic language barriers in communications, but there was little exploration of more nuanced barriers, such as cultural relevance or social context. Ahead of future outbreaks, more research is urgently needed to examine the information landscapes of populations with limited English proficiency, to inform the development of more effective communications strategies from public health institutions and others.
Keywords: Limited English proficiency, Public health communication, COVID-19, Public health preparedness/response, Risk communication, Infectious disease outbreaks, Vulnerable populations
Introduction
People with limited English proficiency (LEP) make up nearly one-tenth of the US population, ages 5 years and older.1 Historically, they have disproportionately faced a host of circumstances that contributed to inequities in health broadly, including lower income, lower educational attainment, lower health literacy, and less access to health insurance or healthcare. They have also been more likely to live in crowded or unstable housing situations and work in high-risk settings, compared with other populations. They are more likely to be older, and thus face related health issues as well as cognitive decline. Further, they have experienced both racial/ethnic discrimination and discrimination based on immigration status.2–7 These circumstances have carried particular negative health consequences during the COVID-19 pandemic, including higher rates of severe illness and death, as well as lower uptake of preventive behaviors.2,3,8–11
Effective emergency risk communication plays a critical role in people’s ability to protect themselves in emergency infectious disease outbreaks.12–15 However, guidelines for public health agencies and others to develop effective communications for people with LEP have been substantially constrained due to a lack of robust evidence available about the communication experiences and needs of people with LEP in the context of emergency infectious disease outbreaks, including COVID-19 and a range of other outbreaks.4,11,16 While some studies suggest that populations with LEP generally have different media consumption habits, use different channels of information, and have different levels of trust than those proficient in English, their communication needs in public health emergencies since the proliferation of social media are much less well understood.13,17,18 There is a lack of data on the preferences of populations with LEP regarding trust in information sources, communication channels, or formats, and a lack of data fully describing barriers to accessing accurate information.13 Instead, most published research to date has focused on racial and ethnic minority populations broadly (eg, the general US Hispanic/Latino population), and has rarely included data on the unique needs of communicating with populations with LEP.3,4,12,13,15
There is a need for an updated perspective on risk communication for communities with LEP because even the research about broad media usage is older, and the communications landscape has transformed dramatically in recent years. The growth of the internet, along with rising smartphone use, has reshaped how people communicate with each other and seek information.13,19 Social media use has facilitated the spread of information with unprecedented speed, reach, and penetration.20,21 This has particular consequences for information during the COVID-19 pandemic, as misinformation has been easily spread on the internet. As a result, the World Health Organization decried in February 2020 that the COVID-19 pandemic has been accompanied by a massive “infodemic” (ie, an overabundance of information, including misinformation).22 While there is a broad literature base on the importance of social media, internet, broadband, and smartphone use,13,19,20 it is still not well understood how these technologies have played a role during the COVID-19 pandemic for people with LEP. Such research can be used to optimally support emergency response, resilience, or preparedness.
Understanding the contours, boundaries, and limitations of existing literature focused on the communication and information experiences of people with LEP in infectious disease outbreaks is essential to building a stronger foundation of research and, ultimately, better communication strategies to support populations with LEP. While prior reviews have examined healthcare experiences or risk communications of populations with LEP in different contexts, none have synthesized knowledge on risk communications pertaining to infectious disease outbreaks.13,23,24 To address this gap, we conducted a review of existing evidence to clarify what elements are well addressed and where additional work is needed.
Methods
Given how little is known about emergency risk communications for people with LEP, we used the JBI scoping review methodology25 to examine the extent, range, and nature of relevant, published research. We followed this methodology (building upon Arksey and O’Malley26 and Levac et al27), with reporting based on the PRISMA extension for scoping reviews checklist28 (see Supplemental Table S1, www.liebertpub.com/doi/suppl/10.1089/hs.2023.0050 ). No review protocol was registered a priori. This review was conducted in 5 stages: (1) identify research questions, (2) identify relevant studies, (3) screen studies, (4) extract and synthesize data, and (5) present results.
Identify Research Questions
To help support a research base that can ground future communication approaches for people with LEP during infectious disease outbreaks, we anchored our review to answer 2 central research questions: (1) What topics about communications pertaining to emergency infectious disease outbreaks for populations with LEP in the United States are currently covered in the literature? (2) What key gaps exist?
Identify Relevant Studies
We aimed to conduct a comprehensive review of published studies on this subject. We therefore defined populations with LEP broadly, following US Census Bureau parameters to include those who do not speak English very well. However, we also expanded beyond those parameters to include, for example, studies of those who prefer languages other than English, those who rely on non-English sources of information, monolingual non-English speakers, and English language learners. We also considered a broad scope of communications, which might include any information that people send or receive through traditional and social media, community outreach efforts, community leaders, and by word of mouth. To focus on the most relevant communications landscape, we considered all emergency infectious disease outbreaks or planning since the last pandemic (H1N1) in 2009. This allowed for the inclusion of literature derived from a range of outbreaks, providing insights from variable features—such as mode of transmission, populations most vulnerable to severe illness, and scale—while still including only outbreaks that occurred in times reasonably considered part of a more modern communications era, when the internet and social media played a strong role. Finally, we searched for articles that included primary data collection and were available in English, as the results aim to inform emergency communication efforts by public health agencies, which primarily use English as a working language in the United States. In addition, to ensure the quality of research conducted through the peer review process, we restricted our search to only peer-reviewed published studies and excluded gray literature from this review.
The literature search was developed and conducted by a research librarian who searched 6 relevant indexed databases: MEDLINE (Ovid), Embase (Elsevier), CINAHL Complete (EBSCO), Global Health (EBSCO), APA Psyc-Info (EBSCO), and Web of Science Core Collection (Clarivate). The first round of the search was conducted on October 20, 2022. To ensure a comprehensive set of articles, a second round was conducted on November 10, 2022, in which the research librarian ran a search from the reference lists of the articles included in the first search. Search terms aimed to cast a wide net in line with our conceptualization. The search therefore included multiple terms used for people with LEP, a variety of communication or information types, and different types of emergency infectious disease outbreaks. Supplemental Table S2 contains the full search string parameters, adapted to each database searched.
To identify relevant articles within the results of this broad search, we developed inclusion criteria prior to screening, and we developed clarifying exclusion criteria after an initial review of the literature. The full list of inclusion and exclusion criteria is available in Supplemental Table S3.
Screen Studies
After records were identified in the first-round search conducted on October 20, 2022, duplicates were removed. Records were then uploaded to Covidence (www.covidence.org)—a systematic review management platform—for a 2-stage screening process. Two authors independently screened articles by title and abstract review. To avoid bias, their decisions were not revealed to each other until all assigned titles and abstracts had been read. To err on the side of caution, if studies could not be clearly excluded based on the titles and abstracts alone, they were carried forward to the second stage (full-text review). When disagreements between reviewing coauthors occurred, consensus was reached through discussion. Articles selected for full-text screening were then independently reviewed by 2 authors to determine whether the articles met the full inclusion criteria. From the second-round search conducted on November 10, 2022, the librarian uploaded additional, deduplicated records to Covidence for screening, and 2 authors repeated the 2-stage screening procedures on the second set of articles. All procedures resulted in a final sample of relevant articles.
Extract and Synthesize Data
We stored the final sample of articles in Zotero for analysis. We analyzed the articles according to the following core components: research method used, language that populations spoke, and type of disease outbreak. In addition, we used thematic analysis to identify and code the content of communication addressed in each article.23,29 Themes about communication content were drawn from the US Centers for Disease Control and Prevention Crisis and Emergency Risk (CERC) framework,14 which aims to help communicators at health departments communicate during emergency infectious disease outbreaks. Themes included: documentation of language barriers in communications on emergency infectious disease outbreaks, information channels used for emergency infectious disease outbreaks, sources trusted for emergency infectious disease outbreak information, and other barriers and facilitators that shape receptivity to information. Two authors validated all information extracted from articles.
Results
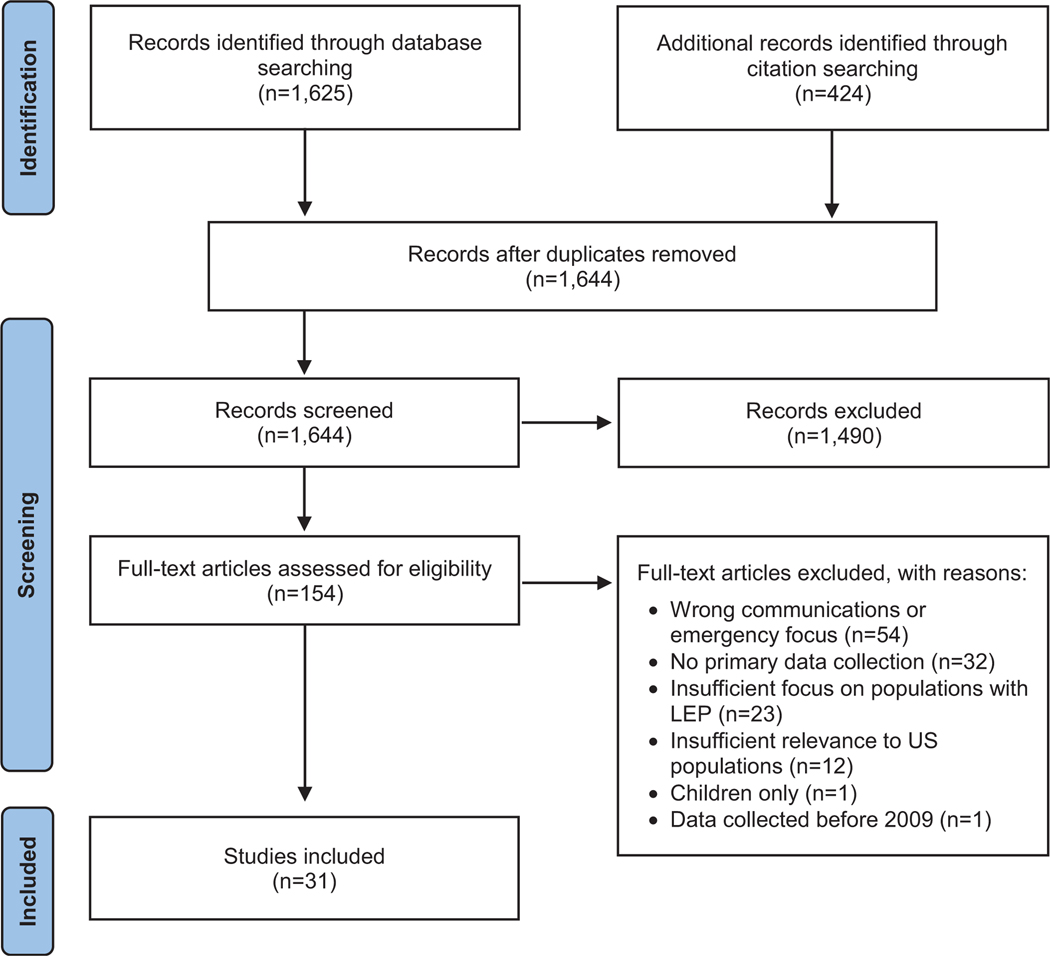
The literature search yielded 1,625 articles in the initial search and 424 articles in the subsequent search of references in articles from the initial search. After duplicates were removed, 1,644 articles were screened out during the first stage (title and abstract screening), leaving 154 studies to be screened for eligibility in the second stage (full-text screening). Full-text screening eliminated a further 123 studies, leaving 31 (28 from the initial search and 3 from the reference search) deemed appropriate for inclusion in the final sample.30–60 The screening process is displayed in the Figure. A detailed presentation of each article is available in Supplemental Table S4. The 31 articles in the final sample were categorized by the core features described in the next section.
Figure.
Flow diagram of data search and results. The flowchart, adapted from the Moher et al61 PRISMA statement, as cited in the Tricco et al28 PRISMA extension for scoping reviews, displays the workflow for screening and assessing articles for eligibility. “Records screened” includes articles screened at the title and abstract stage. “Records excluded” indicates the number of articles excluded in the title and abstract screening stage. Abbreviation: LEP, limited English proficiency.
Core Features
Population
About half (n=15) of the 31 studies focused on the experiences or needs of populations with LEP directly (Table 1). Five studies focused primarily on institutions or groups who work with people with LEP and examined the experiences or needs of people with LEP. Three studies focused on the experiences or needs of institutions or groups who communicate with populations with LEP, about communicators’ experiences or needs. Eight studies focused on communication materials available for people with LEP.
Table 1.
Overview of Core Features and Communication Content of Articles (N=31)
| Core Features | Applicable Studies n (%) |
|---|---|
|
| |
| Population of focus and research method | |
| Studies primarily of populations with LEP about their own needs/experiences (n=15) | |
| Qualitative methods | 6 (19.4) |
| Mixed methods | 1 (3.2) |
| Survey – not nationally representative | 5 (16.1) |
| Survey – nationally representative | 3 (9.7) |
| Studies primarily of institutions or groups who work with populations with LEP about the needs/experiences of populations with LEP (n=5) | |
| Qualitative methods | 3 (9.7) |
| Mixed methods | 2 (6.5) |
| Studies primarily of institutions or groups who communicate to populations with LEP about communicators’ needs/experiences (n=3) | |
| Qualitative methods | 1 (3.2) |
| Survey of community/public health workers | 2 (6.5) |
| Studies of communications materials (n=8) | |
| Mixed methods | 1 (3.2) |
| Impact evaluation of communication intervention | 2 (6.5) |
| Content analysis | 5 (16.1) |
|
| |
| Language of population with LEP studied | |
| Spanish | 20 (64.5) |
| Chinese (Mandarin or Cantonese) | 2 (6.5) |
| Portuguese | 1 (3.2) |
| Swahili | 1 (3.2) |
| Unspecified non-English language preference or multilinguala | 8 (25.8) |
|
| |
| Emergency infectious disease outbreak type | |
| COVID-19 | 21 (67.7) |
| H1N1 influenza or pandemic influenza | 4 (12.9) |
| Zika | 1 (3.2) |
| Mumps | 1 (3.2) |
| General/unspecified emergency infectious disease outbreak type | 4 (12.9) |
|
| |
| Communication content | |
| Did barrier exist by virtue of whether non-English language materials were available | 18 (58.1) |
| Information channels used by populations with LEP | 18 (58.1) |
| Trust in sources of emergency infectious disease outbreak information | 16 (51.6) |
| Other barriers/facilitators shaping information receptivity | 16 (51.6) |
Note: Percentages may add up to more than 100% if articles covered multiple types of non-English languages or multiple communications/information types. Numbers may not add up to 100% due to rounding.
Unspecified non-English preference or multilingual may include studies where the language was specified, but implications of the results were not separately reported by language group.
Abbreviation: LEP, limited English proficiency.
Language
The majority (n=20) of studies examined Spanish speakers or Spanish-language materials. Only 12 studies examined non-Spanish-speaking populations or non-Spanish-language-materials: 2 focused on Chinese speakers, 1 each on Portuguese and Swahili speakers, as well as 8 studies that examined unspecified non-English preference or multilingual groups. This means that the study results relevant to this review were not separated by language group.
Emergency Infectious Disease Outbreak
The majority (n=21) of studies were conducted on the COVID-19 pandemic. Only 10 studied emergency infectious disease outbreaks other than COVID-19: H1N1 influenza or pandemic influenza (n=4), Zika virus (n=1), a mumps outbreak (n=1), and emergency infectious disease outbreaks generally that did not specify the outbreak type (n=4).
Communication Content
Documentation of Language Barriers in Communications More than half (n=18) of the studies in this scoping review included assessments of the language barriers that exist in communications on emergency infectious disease outbreaks (Table 2). Nine of these studies assessed information availability and whether emergency information is less available or contains less information in non-English languages than in English during emergency infectious disease outbreaks. Two studies assessed whether populations with LEP need non-English language information. Five studies examined public health and healthcare workers’ needs regarding non-English language training in order to communicate with populations with LEP. An additional 4 studies discussed language barriers on sending or receiving emergency information during outbreaks.
Table 2.
Overview of Relevant Findings Related to Communications for Populations with Limited English Proficiency in Emergency Infectious Disease Outbreaks
| Categories | Relevant Findings | Language of Population With Limited English Proficiency Studied |
|---|---|---|
| Documentation of language barriers in communications on emergency infectious disease outbreaks (n=18 studies) | Less availability of non-English emergency information (n=9)33,35,45,53–57,60 | Spanish, Swahili, multilingual |
| Need for non-English information (n=2)45,48 | Spanish, Swahili | |
| Public health/healthcare workers’ training/skills needs (n=5)38,39,44,46,50 |
Portuguese, Spanish, multilingual | |
| Language discussed as barrier to sending/receiving emergency information (n=4)36,42,44,47 | Spanish | |
| Information channels used for emergency infectious disease outbreaks (n=18 studies) | Traditional media (n=11): television, radio, newspapers (local, national, and international)30,31,35,37,40,45,46,48,49,51,52 | Chinese, Portuguese, Spanish, Swahili, multilingual |
| Internet/social media (n=11): internet,31,40,45,51,52 social media30,40,43,45,46,49,58,59 | Chinese, Portuguese, Spanish, Swahili, multilingual | |
| Friends/family (n=8): friends/family,30,31,35,45,51,52 social networks/community members30,40,41,45 | Chinese, Spanish, Swahili, multilingual | |
| Healthcare providers (n=6): healthcare providers,30,31,37,51,52 specifically federally qualified health centers47 | Chinese, Spanish, multilingual | |
| Community-based and religious organizations (n=6): nonprofit organizations, community-based organizations or community centers,30,31,40 specifically including Ventanilla de Salud,42 refugee programs,35 churches40,45 | Chinese, Spanish, Swahili | |
| Officials or public figures (n=4): public health agencies,30 governor49 or other elected officials,30,31 public health systems or hotlines,31 firefighters40 | Chinese, Spanish | |
| Other (n=7): health educators37; emergency SMS (text) alerts, phone calls, mobile phone applications, or email31,40,49,51; door-to-door40; police departments37; schools31,40; workplaces45,50 | Chinese, Spanish, Swahili, multilingual | |
| Trust in sources of emergency infectious disease outbreak information (n=16 studies) | Trust in sources of information (n=14) | |
| Media (n=3): television,45,52 journalists32 | Spanish, Swahili | |
| Internet/social media (n=4): internet,34,52 social media46,49 | Portuguese, Spanish, multilingual | |
| Friends/family (n=2): friends, family, social networks30,48 | Chinese, Spanish | |
| Healthcare providers (n=6): healthcare providers,30,41,48,52,60 traditional medicine practitioners,30 medical interpreters40 | Chinese, Spanish, multilingual | |
| Community-based and religious organizations (n=7): staff at community-based organizations60 and specific programs (Ventanilla de Salud42 and the Rochester Healthy Community Partnership43), faith groups/religious leaders,30,41,48,60 community stakeholders48 | Spanish, multilingual | |
| Officials or public figures (n=3): public health agencies/departments,30 elected officials,30 government generally33,41 | Chinese, Spanish, multilingual | |
| Other (n=3): social services,41 translated mail handouts,34 schools,41 phone calls,34 texting,49 emailing49 | Spanish, multilingual | |
| Other areas studied (n=6): misinformation (n=4)42,46,51,60; general trust/mistrust in information (n=2)31,45 | Portuguese, Spanish, multilingual; Chinese, Swahili | |
| Other barriers and facilitators that shape receptivity to information, beyond trust (n=16 studies) | Cultural factors that shape receptivity to information (n=8): differences in vaccine willingness,33 whether cultural needs were considered or met,34,38,42–44,47,60 public health workers expressed interest in training on cultural competency or cultural sensitivity38,44 | Portuguese, Spanish, multilingual, |
| Literacy/health literacy as a barrier to communication (n=5)33,44,47,54,55 |
Spanish | |
| Quality of information/user experience (n=4): hospital websites,55 health department websites,56,57 contact tracing calls36 | Spanish, multilingual | |
| Other areas studied (n=8): concerns about immigration, being undocumented, or fear of deportation related to the emergency infectious disease outbreak (n=5)35,44,46,47,60; stigma, “othering,” or discrimination (n=3)30,47,60 | Portuguese, Spanish, multilingual; Chinese, Spanish |
Information Channels Used for Emergency Infectious Disease Outbreaks
In addition, the majority (n=18) of studies in this review examined information channels used by populations with LEP for emergency infectious disease outbreaks. Eleven examined which traditional media sources people with LEP use for information in emergency infectious disease outbreaks, including local, national, and international radio, television, and newspapers. Eleven studies examined the internet or social media. Other sources examined were friends/family (n=8 studies), healthcare providers (n=6 studies), community-based and religious organizations (n=6 studies), and officials or public figures (n=4 studies), as well as other modes including health educators, emergency SMS (text) alerts, phone calls, mobile phone applications, emails, door-to-door outreach, police departments, schools, and workplaces.
Trust in Sources of Emergency Infectious Disease Outbreak Information
Sixteen studies included findings on trust in information or sources of information during emergency infectious disease outbreaks. Despite the broad number of trusted sources identified by individual studies, there was little overlap in media or social sources mentioned across studies. For example, only 4 studies mentioned trust in the internet or social media, 3 studies mentioned trust in traditional media, and 2 studies mentioned trust in family, friends, or social networks. The greatest areas of overlap across studies were mentions of healthcare providers or community- or faith-based organizations as trusted sources of information. Seven studies mentioned trust in staff at community- or faith-based organizations or in specific community health programs. Six studies mentioned trust in healthcare providers, including traditional medicine practitioners and medical interpreters. Three studies mentioned trust in officials or public figures, including public health agencies and elected officials. Other sources of information mentioned in the context of trust were social services, translated mail handouts, schools, phone calls, or emails. In addition, 4 studies assessed misinformation, while 2 assessed general trust and mistrust in information.
Barriers and Facilitators Beyond Trust That Shape Receptivity to Information
About half (n=16) of the studies documented barriers and facilitators beyond trust that shaped receptivity to information during emergency infectious disease outbreaks among populations with LEP. Half of those (n=8) examined cultural factors that shaped receptivity to information on behaviors like vaccination. These included studies that assessed whether cultural needs, including communications sensitive to religious beliefs, immigration issues, or dialects, had been considered or met (n=7), and studies that reported public health workers’ interest in cultural competency or sensitivity training (n=2). Five studies examined literacy or health literacy as a barrier to communication, and 4 studies examined the quality of information available or the user experience with hospital websites, health department websites, and contact tracing calls. In addition, a small number of studies examined the social and structural context that might make it difficult to get information in an emergency. Five studies examined concerns about immigration, being undocumented, or fear of deportation, while 3 studies assessed stigma, “othering,” or discrimination.
Discussion
Key Topics Identified and Implications for Research and Practice
This scoping review revealed the paucity of research on the communication experiences and information landscape of people with LEP during infectious disease outbreaks. Only 31 relevant studies have been published since 2009, and the articles that have been published are extremely limited in scope. Most focus exclusively on Spanish speakers, while other populations with LEP have 1, or at most 2, articles focused on their experience. Even studies focused on Spanish speakers used primarily qualitative methods, which may provide a certain richness in insights but have limited capacity to provide representative findings. Further, most articles are about experiences during the COVID-19 pandemic, which may be timely but provide little opportunity to understand how information needs may vary in outbreaks of different scales.
Beyond these limitations in study availability and design, results showed 2 additional constraints specific to communications development. First, while the literature published since 2009 includes several studies documenting information that is available to populations with LEP (eg, Spanish-language information on websites), few covered what information was actually used or preferred by these populations. Moreover, despite the proliferation of internet and social media use in the past 2 decades, only 11 studies mentioned social media or internet use, while still fewer documented concerns about trust or misinformation in these sources. Most of the available literature covered media sources broadly and did not attempt to systematically rank or list news sources used or preferred by populations with LEP. This lies in stark contrast to readily available research documenting the news sources used, trusted, and preferred by the general (primarily English-speaking) US population.62,63
Second, discussion of barriers to accessing and using communication materials was extremely limited. Most studies simply documented the inadequate availability of materials in concordant languages and thus showed that even basic translation has been a major barrier to communicating with US populations who speak a language other than English. While this is important to document, few went beyond to examine other barriers to effective communication like the quality of materials in languages other than English. Moreover, even studies including measures of quality were limited to assessing readability and user experience, in effect judging non-English materials by the same metrics as English materials. Largely missing from the literature are assessments of the quality of communication materials, with the added lens of whether materials are culturally relevant for populations with LEP. In addition, few studies examined trusted sources, with little overlap in sources discussed. Importantly, there was also little evidence examining more complex inhibitors of information seeking, understanding, and use. There was little discussion of experiences of discrimination or stigma, cultural responsiveness, and/or concerns about deportation or immigration among populations with LEP, and how these experiences related to how they accept and process emergency risk communications. For instance, cultural stigma from the origins of COVID-19 has been a major source of discrimination and concern among the broader Asian American community in the United States, but only 1 study examined how this impacted Asian adults’ receptivity to COVID-19 information.30
Finally, results from this scoping review revealed challenges with the sampling frames and foci of existing studies that constrain the utility of their findings. On one hand, several studies did not focus on populations with limited English proficiency specifically, but rather they had a broader focus on Spanish-speaking, Latino, or immigrant populations.32,33,48,60 For example, in some studies, not all participants had LEP, and/or the findings were not separately reported between participants with LEP and those proficient in English. On the other hand, several studies included only those findings relevant to specific subsets of populations with LEP, like pregnant women tested for Zika virus infection,52 migrant and seasonal farmworkers,36,47 refugees,35,45 and older adults living alone with cognitive impairment during the COVID-19 pandemic.51 Thus, findings from many of the studies in this field may not be directly generalizable to broader populations with LEP without more careful consideration. Further, none examined the heterogeneity of experiences within language groups (eg, how Puerto Ricans’ communication experiences differed from those of Mexican Americans).
Future research is needed to create a more robust foundation of evidence that can support communication strategy and development efforts to prepare for and respond to emergency infectious disease outbreaks for populations with LEP. Additional studies are needed that go beyond documenting the extent to which materials are translated, and that go into more depth about how well materials are translated, adapted, and developed, as well as examine less obvious challenges such as cultural responsiveness. National healthcare standards on culturally and linguistically appropriate services may provide a parallel framework useful for consideration in the context of infectious disease outbreaks.64 Cultural differences are essential to tease out—recognizing that there is huge diversity within a given language group. More research is needed on trusted sources, as well as how to build and maintain trust at different inflection points in longer-term emergency infectious disease outbreaks such as COVID-19, fully accounting for historical racism and xenophobia. Finally, the scope of future research needs to be more appropriately designed with a more comprehensive and clear focus on people with LEP, while using methods that are generalizable to larger populations with LEP and across different outbreak types.
Limitations
This scoping review has important limitations. Although the review is based on evidence retrieved from 6 search databases, the search strategy could have resulted in the inclusion of additional relevant articles if different search terms or databases had been used. The search strategy also excluded gray literature, which could have important implications for practice. The definition of LEP differed across studies analyzed, and people who make up the larger population with LEP in the United States are diverse, limiting the generalizability of some findings. Studies with findings that were not specific to emergency infectious disease outbreaks (eg, studies of hurricanes, fires, medical emergencies, other natural disasters) or studies with results not specific to the United States (eg, studies of Spanish-language tweets) were excluded. Although this approach was aligned with the overall purpose of the scoping review, in effect it may have excluded other literature informing communications with communities with LEP in noninfectious disease outbreak contexts that could have broad relevance to emergency settings. In addition, since a scoping review was conducted instead of a systematic review, the authors did not compare the quality of evidence across studies, and thus are not able to evaluate study quality or methods.
Conclusion
This scoping review on communications for and with US populations with LEP pertaining to emergency infectious disease outbreaks found that there has been a paucity of peer-reviewed research published since the H1N1 pandemic in 2009. Ahead of future outbreaks, more high-quality studies are urgently needed to address the following areas in particular. Future studies should (1) examine other language groups, in addition to Spanish; (2) examine other outbreak types beyond just COVID-19; (3) use study designs with quantitative methods and random, representative samples where possible; (4) go beyond documenting information availability and also examine which information is used or preferred by populations with LEP; (5) examine more nuanced barriers to communication beyond language translation, including cultural relevance and social context; and (6) report findings according to individual languages or level of English proficiency rather than reporting only about larger groups that include people with LEP. Building a stronger research base in this area will help ensure public health agencies can build a more robust communications infrastructure with relevant strategies and materials ahead of future emergency infectious disease outbreaks.
Supplementary Material
Acknowledgments
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC), any other portion of the Government of the United States, or Harvard TH Chan School of Public Health (HSPH). The study was conducted through a direct contract to HSPH from the CDC, “Evidence for Translating Views to Action: Understanding Information Needs and Communication Channels Among Limited English Proficiency Populations to Inform Emergency Communication Recommendations for Infectious Disease Outbreaks” (Contract #75D30118C03566).
Contributor Information
Mary G. Findling, Harvard Opinion Research Program, Department of Health Policy and Management.
Hannah L. Caporello, Harvard Opinion Research Program, Department of Health Policy and Management.
Rebekah I. Stein, Harvard Opinion Research Program, Department of Health Policy and Management.
Carrie G. Wade, Research and Instruction Librarian, Countway Library of Medicine, Harvard Medical School, Boston, MA..
Keri M. Lubell, US Centers for Disease Control and Prevention, Atlanta, GA..
Lisa Briseño, US Centers for Disease Control and Prevention, Atlanta, GA..
Gillian K. SteelFisher, Harvard Opinion Research Program, Department of Health Policy and Management.
References
- 1.US Census Bureau. 2021. American Community Survey. Table B16001: Language spoken at home by ability to speak English for the populations 5 years and over Accessed September 11, 2023. https://data.census.gov/table?q=B16001:+LANGUAGE+SPOKEN+AT+HOME+BY+ABILITY+TO+SPEAK+ENGLISH+FOR+THE+POPULATION+5+YEARS+AND+OVER&g=0100000US&tid=ACSDT5Y2021.B16001
- 2.Truman BI, Tinker T, Vaughan E, et al. Pandemic influenza preparedness and response among immigrants and refugees. Am J Public Health. 2009;99(suppl 2):S278–S286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hutchins SS, Fiscella K, Levine RS, Ompad DC, McDonald M. Protection of racial/ethnic minority populations during an influenza pandemic. Am J Public Health. 2009;99(suppl 2): S261–S270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andrulis DP, Siddiqui NJ, Gantner JL. Preparing racially and ethnically diverse communities for public health emergencies. Health Aff (Millwood). 2007;26(5):1269–1279. [DOI] [PubMed] [Google Scholar]
- 5.Clark E, Fredricks K, Woc-Colburn L, Bottazzi ME, Weatherhead J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Negl Trop Dis. 2020;14(7):e0008484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quandt SA, LaMonto NJ, Mora DC, Talton JW, Laurienti PJ, Arcury TA. COVID-19 pandemic among immigrant Latinx farmworker and non-farmworker families: a rural–urban comparison of economic, educational, healthcare, and immigration concerns. New Solut J. 2021;31(1):30–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKee MM, Paasche-Orlow MK. Health literacy and the disenfranchised: the importance of collaboration between limited English proficiency and health literacy researchers. J Health Commun. 2012;17(suppl 3):S7–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021;4(1):e2036462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rozenfeld Y, Beam J, Maier H, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. 2020;19(1):126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ingraham NE, Purcell LN, Karam BS, et al. Racial and ethnic disparities in hospital admissions from COVID-19: determining the impact of neighborhood deprivation and primary language. J Gen Intern Med. 2021;36(11):3462–3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ortega P, Martínez G, Diamond L. Language and health equity during COVID-19: lessons and opportunities. J Health Care Poor Underserved. 2020;31(4):1530–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beckjord EB, Stern S, Meredith LS, et al. Enhancing Emergency Preparedness, Response, and Recovery Management for Vulnerable Populations. Task 3: Literature Review. Santa Monica, CA: RAND Health; 2008. https://www.rand.org/pubs/working_papers/WR581.html [Google Scholar]
- 13.Berg SH, O’Hara JK, Shortt MT, et al. Health authorities’ health risk communication with the public during pandemics: a rapid scoping review. BMC Public Health. 2021;21(1): 1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Centers for Disease Control and Prevention. CERC: Messages and Audiences. 2018 update. Atlanta: CDC; 2018. https://emergency.cdc.gov/cerc/ppt/CERC_Messages_and_Audiences.pdf [Google Scholar]
- 15.Vaughan E, Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Public Health. 2009;99(suppl 2):S324–S332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quinn SC. Crisis and emergency risk communication in a pandemic: a model for building capacity and resilience of minority communities. Health Promot Pract. 2008; 9(4 suppl):S18–S25. [DOI] [PubMed] [Google Scholar]
- 17.Clayman ML, Manganello JA, Viswanath K, Hesse BW, Arora NK. Providing health messages to Hispanics/Latinos: understanding the importance of language, trust in health information sources, and media use. J Health Commun. 2010;15(suppl 3):S252–S263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rowel R, Sheikhattari P, Barber TM, Evans-Holland M. Introduction of a guide to enhance risk communication among low-income and minority populations: a grassroots community engagement approach. Health Promot Pract. 2012;13(1):124–132. [DOI] [PubMed] [Google Scholar]
- 19.Chou WYS, Hunt YM, Beckjord EB, Moser RP, Hesse BW. Social media use in the United States: implications for health communication. J Med Internet Res. 2009;11(4):e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Merchant RM, Lurie N. Social media and emergency preparedness in response to novel coronavirus. JAMA. 2020; 323(20):2011–2012. [DOI] [PubMed] [Google Scholar]
- 21.Rosenberg H, Syed S, Rezaie S. The Twitter pandemic: the critical role of Twitter in the dissemination of medical information and misinformation during the COVID-19 pandemic. CJEM. 2020;22(4):418–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Novel coronavirus (2019-nCoV) situation report – 13: data as reported by 2 February 2020. Accessed September 11, 2023. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200202-sitrep-13-ncov-v3.pdf
- 23.Yeheskel A, Rawal S. Exploring the ‘patient experience’ of individuals with limited English proficiency: a scoping review. J Immigr Minor Health. 2019;21(4):853–878. [DOI] [PubMed] [Google Scholar]
- 24.Hipper TJ, Davis R, Massey PM, et al. The disaster information needs of families of children with special healthcare needs: a scoping review. Health Secur. 2018;16(3):178–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. Chapter 11: Scoping reviews. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. Adelaide, Australia: JBI; 2020. Updated July 26, 2022. Accessed September 11, 2023. 10.46658/JBIMES-20-12 [DOI] [Google Scholar]
- 26.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 27.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. [DOI] [PubMed] [Google Scholar]
- 29.Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Effect. 2012;4(3): 409–429. [Google Scholar]
- 30.SteelFisheK, CaporellL, LubelM, et al. Getting critical information during the COVID-19 pandemic: experiences of Spanish and Chinese speakers with limited English proficiency. Health Secur. 2022;20(4):273–285. [DOI] [PubMed] [Google Scholar]
- 31.Yip MP, Ong B, Painter I, Meischke H, Calhoun B, Tu SP. Information-seeking behaviors and response to the H1N1 outbreak in Chinese limited-English proficient individuals living in King County, Washington. Am J Disaster Med. 2009;4(6):353–360. [PubMed] [Google Scholar]
- 32.Gomez-Aguinaga B, Oaxaca AL, Barreto MA, Sanchez GR. Spanish-language news consumption and Latino reactions to COVID-19. Int J Environ Res Public Health. 2021;18(18): 9629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quinn SC, Kumar S, Freimuth VS, Kidwell K, Musa D. Public willingness to take a vaccine or drug under Emergency Use Authorization during the 2009 H1N1 pandemic. Biosecur Bioterror. 2009;7(3):275–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evola CM, Repas SJ, Dickman J, et al. Perceptions of theSARS-CoV2 pandemic: a small comparative survey analysis between language preference populations in a United States community health center. Pathog Glob Health. 2023;117(2): 203–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gautham I, Albert S, Koroma A, Banu S. Impact ofCOVID-19 on an urban refugee population. Health Equity. 2021;5(1):718–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Limaye N, Ninesling B, Marcelin F, et al. COVID-19 pandemic response in a migrant farmworker community: excess mortality, testing access and contact tracing in Immokalee, Florida. Ann Glob Health. 2022;88(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Witrago E, Perez MA. Preparing for an influenza pandemic: policy implications for rural Latino populations. J Health Care Poor Underserved. 2011;22(3 suppl):S58–S71. [DOI] [PubMed] [Google Scholar]
- 38.D’Ambrosio L, Huang CE, Sheng Kwan-Gett T. Evidence-based communications strategies: NWPERLC response to training on effectively reaching limited English-speaking (LEP) populations in emergencies. J Public Health Manag Pract. 2014;20(suppl 5):S101–S106. [DOI] [PubMed] [Google Scholar]
- 39.El-Khayat Y, Franco N, Miller L. Community conversations about COVID-19. Med Ref Serv Q. 2022;41(3):223–235. [DOI] [PubMed] [Google Scholar]
- 40.Ike BR, Calhoun R, Angulo AS, Meischke H, Senturia KD. Medical interpreters and bilingual school staff: potential disaster information conduits? J Emerg Manag. 2015;13(4): 339–348. [DOI] [PubMed] [Google Scholar]
- 41.Kozo J, Wooten W, Porter H, Gaida E. The Partner Relay Communication Network: sharing information during emergencies with limited English proficient populations. Health Secur. 2020;18(1):49–56. [DOI] [PubMed] [Google Scholar]
- 42.Vilar-Compte M, Gaitán-Rossi P, Félix-Beltrán L, Bustamante AV. Pre-COVID-19 social determinants of health among Mexican migrants in Los Angeles and New York City and their increased vulnerability to unfavorable health outcomes during the COVID-19 pandemic. J Immigr Minor Health. 2022;24(1):65–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wieland ML, Asiedu GB, Njeru JW, et al. Community-engaged bidirectional crisis and emergency risk communication withimmigrant and refugee populations during theCOVID-19 pandemic. Public Health Rep. 2022;137(2):352–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koeller S, Meyer D, Shearer MP, Hosangadi D, Snyder M, Nuzzo JB. Responding to a mumps outbreak impacting immigrants and low–English-proficiency populations. J Public Health Manag Pract. 2020;26(2):124–130. [DOI] [PubMed] [Google Scholar]
- 45.Mahoney D, Obure R, Billingsley K, Inks M, Umurutasate E, Baer RD. Evaluating understandings of state and federal pandemic policies: the situation of refugees from the Congo wars in Tampa, Florida. Hum Organ. 2020;79(4):271–280. [Google Scholar]
- 46.Priebe Rocha L, Rose R, Hoch A, et al. The impact of theCOVID-19 pandemic on the Brazilian immigrant community in the U.S: results from a qualitative study. Int J Environ Res Public Health. 2021;18(7):3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schoch-Spana M, Bouri N, Rambhia KJ, Norwood A. Stigma, health disparities, and the 2009 H1N1 influenza pandemic: how to protect Latino farmworkers in future health emergencies. Biosecur Bioterror. 2010;8(3):243–254. [DOI] [PubMed] [Google Scholar]
- 48.Balasuriya L, Santilli A, Morone J, et al. COVID-19 vaccine acceptance and access among Black and Latinx communities. JAMA Netw Open. 2021;4(10):e2128575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moyce S, Velazquez M, Claudio D, et al. Exploring a rural Latino community’s perception of the COVID-19 pandemic. Ethn Health. 2021;26(1):126–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Osakwe ZT, Osborne JC, Samuel T, et al. All alone: a qualitative study of home health aides’ experiences during the COVID-19 pandemic in New York. Am J Infect Control. 2021;49(11):1362–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Portacolone E, Chodos A, Halpern J, et al. The effects of the COVID-19 pandemic on the lived experience of diverse older adults living alone with cognitive impairment. Gerontologist. 2021;61(2):251–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodriguez M, Danvers AA, Sanabia C, Dolan SM. Educational behaviors of pregnant women in the Bronx during Zika’s International emerging epidemic: “First mom ... and then I’d Google. And then my doctor.” BMC Pregnancy Childbirth. 2021;21:719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Capurro D, Chaudhuri S, Turner AM. The online availability of multilingual health promotion materials produced by local health departments: an information assessment. Stud Health Technol Inform. 2015:216:380–385. [PubMed] [Google Scholar]
- 54.Fulmer AA, Abboud GA, Wallace LS. Health literacy characteristics of over-the-counter rapid antigen COVID-19 test materials. Res Soc Adm Pharm. 2022;18(12):4124–4128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Higashi RT, Sweetenham JW, Israel AD, Tiro JA. COVID-19 communication from seven health care institutions in north Texas for English- and Spanish-speaking cancer patients: mixed method website study. JMIR Cancer. 2021;7(3):e30492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kusters IS, Dean JM, Gutierrez AM, Sommer M, Klyueva A. Assessment of COVID-19 website communication in languages other than English by local health departments in the United States. Health Commun. 2023;38(8):1519–1529. [DOI] [PubMed] [Google Scholar]
- 57.Kusters IS, Gutierrez AM, Dean JM, Sommer M, Klyueva A. Spanish-language communication of COVID-19 information across US local health department websites. J Racial Ethn Health Disparities. 2023;10(5):2482–2489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marcell L, Dokania E, Navia I, et al. One Vax Two Lives: asocial media campaign and research program to address COVID-19 vaccine hesitancy in pregnancy. Am J Obstet Gynecol. 2022:227(5):685–695.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ramos AK, Duysen E, Carvajal-Suarez M, Trinidad N. Virtual outreach: using social media to reach Spanish-speaking agricultural workers during the COVID-19 pandemic. J Agromed. 2020;25(4):353–356. [DOI] [PubMed] [Google Scholar]
- 60.Kerrigan D, Mantsios A, Karver TS, et al. Context and considerations for the development of community-informed health communication messaging to support equitable uptake of COVID-19 vaccines among communities of color in Washington, DC. J Racial Ethn Health Disparities. 2023; 10(1):395–409. (First published online February 3, 2022.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liedke J, Gottfried J. U.S. adults under 30 now trust information from social media almost as much as from national news outlets. Pew Research Center. Published October 27, 2022. Accessed September 11, 2023. https://www.pewresearch.org/fact-tank/2022/10/27/u-s-adults-under-30-now-trust-information-from-social-media-almost-as-much-as-fromnational-news-outlets/ [Google Scholar]
- 63.Forman-Katz N, Matsa KE. News platform fact sheet. Pew Research Center. Published September 20, 2022. Accessed September 11, 2023. https://www.pewresearch.org/journalism/fact-sheet/news-platform-fact-sheet/ [Google Scholar]
- 64.Department of Health and Human Services Office of Minority Health. National Culturally and Linguistically Appropriate Services standards. Accessed October 10, 2023. https://thinkculturalhealth.hhs.gov/clas/standards
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.