Abstract
Introduction
The COVID-19 pandemic necessitated a major expansion in telemedicine use. The continued use of telemedicine post-pandemic has the potential to enhance healthcare use for people at risk for sub-optimal healthcare access and utilization, such as patients with previous preventable hospitalization. This study analyzed the association between pre-pandemic preventable hospitalizations (PPHs) and telemedicine use during the pandemic.
Methods
This retrospective cohort study uses Medicaid administrative claims data (01/2018–06/2022) for patients of a large Federally Qualified Health Center in Arizona that implemented telemedicine in March 2020. Bivariate and multivariable generalized estimating equations were used to analyze the relationship between the outcome and predictor variables. We also analyze racial/ethnic and primary language disparities in telemedicine use among those with PPH and report the average predicted probability.
Results
There was a statistically significant relationship between telemedicine use and PPH even after adjusting for comorbidity severity (OR:1.85; CI: 1.74, 1.96). Analyses restricted to those who had PPHs showed an seven-percentage point difference in the predicted probability of telemedicine use between non-Hispanic White individuals and Asian/Pacific Islanders, the group with the lowest probability of telemedicine use among our study sample.
Conclusion
Telemedicine is a unique tool that can be leveraged by interventions that aim to optimize healthcare use among those with a history of preventable hospitalizations. However, the lack of targeted interventions to identify and address barriers to telemedicine use among minoritized groups could limit the impact of such interventions and widen disparities.
Keywords: Telemedicine, preventable hospitalization, ambulatory care-sensitive hospitalization, FQHC, disparities
Introduction
Preventable hospitalization also known as ambulatory care-sensitive hospitalization (ACSH) is indicative of sub-optimal preventative care and is a marker of healthcare access and the quality of health services in a given community.1–4 Defined as hospital stays that can be prevented by optimal preventive care,2–4 preventable hospitalizations are often due to acute ambulatory care-sensitive conditions (ACSCs) (urinary tract infection, bacterial pneumonia, dehydration) or chronic ACSCs (diabetes short and long-term complications, chronic obstructive lung disease, hypertension, congestive heart failure, angina, and asthma) as identified by the Agency for Healthcare Research and Quality.1,5 Preventable hospitalizations accounted for 12.9% of all non-obstetric hospitalizations and $33.7 billion in hospital costs in 2017, 6 the most recent year for which there are national estimates. The burden of these hospitalizations on individuals and society has significant practice and policy implications, particularly for underserved populations, who have higher preventable hospitalization prevalence3,7; many of whom also receive care in safety-net settings.
Safety-net clinics, such as Federally Qualified Health Centers (FQHC), play a significant role in ensuring access to primary care for many low-income, Medicaid-enrolled, and uninsured patients. Funded by the Health Resources & Services Administration (HRSA), FQHCs provide primary care services in underserved areas, serving many minoritized racial/ethnic populations, and populations who are often at high risk for sub-optimal healthcare use. Prior work shows that Medicaid-insured individuals are at higher risk for preventable hospitalizations compared to privately insured individuals.6,8,9 Other researchers have noted that non-Hispanic Black and Hispanic individuals have a higher likelihood of preventable hospitalizations compared to non-Hispanic White individuals,10–12 even when stratified by sex and age. 13 For instance, the rate of preventable hospitalizations for chronic conditions among non-Hispanic Black people in 2017 was 2.5 times the rate among non-Hispanic White people (2198 vs 874.6/100,000); the rate among Hispanic people was 992/100,000. 10 Similarly, in studies restricted to Medicaid-insured individuals, the prevalence of these hospitalizations is higher among non-Hispanic Black individuals compared to their non-Hispanic White counterparts. 12 These trends indicate a need for newer approaches to optimize healthcare use among populations at risk for preventable hospitalizations.
Telemedicine has long been proposed as a novel tool to improve population health, especially for those at risk for inadequate healthcare use and poor health outcomes.14,15 Since the COVID-19 pandemic-related telemedicine expansion, practice, and policy discourse regarding the role of this unique digital tool in addressing disparate healthcare use and health outcomes has intensified. Telemedicine could improve healthcare utilization among underserved individuals with previous preventable hospitalizations by reducing previously identified barriers to healthcare use, such as transportation barriers, lack of childcare, or work schedules that conflict with appointment availability and associated financial strain.16,17 Thus, this tool could be leveraged by interventions that aim to optimize healthcare use among those with a history of preventable hospitalizations.
Studies examining the association between telemedicine and preventable hospitalizations have reported mixed findings. Evidence from a pre-pandemic study reported a decreased likelihood of preventable hospitalizations among patients living with diabetes who used telemedicine, compared to their counterparts who did not use telemedicine. 18 Friedman et al. noted that telemedicine familiarity was associated with decreased inpatient and emergency department utilization for certain preventable hospitalizations post-disaster. 19 However, Li and colleagues noted that primary care practices with high telehealth use had greater preventable hospitalization rates compared with practices with lower rates of telehealth use during the COVID-19 pandemic. 20 Missing from the literature is how patients with pre-pandemic preventable hospitalizations (PPHs) have engaged with telemedicine during the pandemic era. It is also not clear whether there are disparities in telemedicine use across racial and/or ethnicity or primary language exist among this subpopulation. This understanding could aid stakeholders exploring the feasibility of interventions that leverage telehealth to improve healthcare use and potentially reduce preventable hospitalizations among those at risk for these hospitalizations. It is also crucial to identify whether social determinants of health such as race/ethnicity and primary language affect telemedicine use among this sub-group as this could guide interventions to increase telemedicine use.
This study aims to fill this gap by analyzing the relationship between telemedicine use and preventable hospitalizations among Medicaid enrollees of a large safety-net academic center with 12 FQHCs. We analyze disparities in telemedicine use among those with a prior preventable hospitalization across race/ethnicity and primary language.
Methods
Data source
This study employs a retrospective cohort study design, using linked January 2018–June 2022 Arizona Medicaid insurance enrollment, demographics, and claims data files. The demographic data contained information on race, ethnicity, primary language, sex, age, and marital status. The claims file contained diagnosis information as well as the visit date.
Study sample
The study sample was adult (≥18 years) Medicaid-insured patients of a safety-net academic health center with 12 FQHCs and four hospitals that implemented telemedicine in March 2020. The inclusion criteria were (a) Medicaid-enrolled (b) having at least one claim before the pandemic (January 2018 and February 2020), (c) having at least one outpatient claim during the pandemic, and (d) adult (≥18 years). The unit of analysis was person-year. The final sample size was 135,303.
Measures
The outcome measure was the visit modality for primary care visits during the pandemic (March 2020–June 2022). Visit modality was categorized as no telemedicine visit [0] or telemedicine visit [1]). The primary predictors of interest were prior preventable hospitalization (January 2018–February 2020). We conducted analyses for preventable hospitalizations for chronic and acute conditions combined and separately. The conditions were identified and defined using ICD-10 codes from the database. In line with the AHRQ designation, the chronic conditions, also known as chronic ACSCs, included angina, asthma, congestive heart failure, chronic obstructive pulmonary disease, diabetes complications, hypertension, and convulsions/epilepsy. Acute ACSC included aspiration, cellulitis, constipation, dehydration and gastroenteritis, ear, nose, and throat infections, gangrene, gastroesophageal reflux disease, iron deficiency anemia, influenza, nutritional deficiencies, pelvic inflammatory disease, perforated/bleeding ulcers, pneumonia and other acute lower respiratory tract infections, tuberculosis and other vaccine-preventable infections, and urinary tract infection/pyelonephritis. 1 Control variables were race/ethnicity, primary language, age, sex, number of days enrolled in Medicaid, marital status, year fixed effects, and comorbidity severity. Comorbidity severity was defined using the Charlson comorbidity index, a weighted index that predicts 10-year mortality by accounting for the number and severity of comorbid diseases, derived using the SAS user-written code.21–23
Race/ethnicity and primary language were the primary predictors for the analyses exploring determinants of telemedicine use among those with previous preventable hospitalizations.
Statistical analyses
We calculated descriptive statistics and examined differences by telehealth utilization using Pearson's χ2 test and t-tests for categorical and continuous variables, respectively. We also analyzed differences in telemedicine use by history of PPH. To account for the longitudinal nature of the data, we used generalized estimating equations (GEEs) with a logit link. We estimate three models: bivariate model with only PPH s as the predictor (model 1), multivariable model adjusting for all covariates except the Charlson comorbidity index (model 2), and multivariable model adjusting for the Charlson comorbidity index (model 3). We then analyzed the relationship between race/ethnicity, primary language, and telemedicine use among those with PPH using GEE models and report the predicted probability. All analyses were conducted using STATA/MP version 16.1. Statistical significance was assessed at α = .05 level. This study was approved by the Arizona State University Institutional Review Board (#00016056).
Results
Descriptive analyses
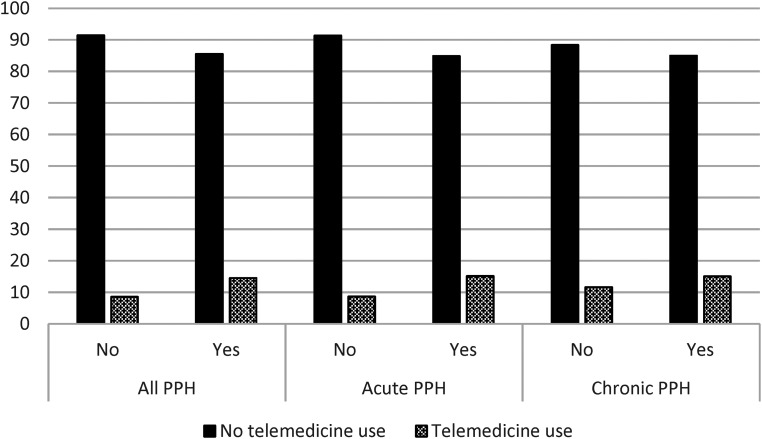
Table 1 shows summary statistics of the study sample. Non-Hispanic Whites comprised about 32% of the study sample while non-Hispanic Blacks, Native Americans, Asians, and Hispanics comprised approximately 17%, 4%, 3%, and 43%, respectively. English was the primary language for approximately 84% of the study sample while Spanish was the primary language for about 15% of the study sample. Only about 17% of outpatient claims for primary care were for telemedicine visits during the first year of the study period (2020) with a decline to 10% used in 2022. About 9% of claims for those who did not have a PPH were for telemedicine compared to 15% for those who had a PPH (Figure 1).
Table 1.
Descriptive characteristics of study sample (n = 135,303).
| All | No telehealth use | Telehealth use | p-value | |
|---|---|---|---|---|
| n(%) | n(%) | n(%) | ||
| Total | 115,739 (86.58) | 17,942 (13.42) | ||
| Sex | <0.0001 | |||
| Male | 53,532 (39.56) | 45,624 (85.23) | 7908 (14.74) | |
| Female | 81,771 (60.44) | 71,495 (87.43) | 10,276 (12.57) | |
| Race/ethnicity | <0.0001 | |||
| Non-Hispanic White | 43,845 (32.41) | 35,868 (81.81) | 7977 (18.19) | |
| Non-Hispanic Black | 23,166 (17.12) | 20,009 (86.37) | 3157 (13.63) | |
| Native American | 5843 (4.32) | 4918 (84.17) | 925 (15.83) | |
| Asian/Pacific/Islander | 3995 (2.95) | 3665 (91.74) | 330 (8.26) | |
| Hispanic | 58,454 (43.20) | 52,659 (90.09) | 5795 (9.91) | |
| Age (Years) | <0.0001 | |||
| 18–40 | 59,285 (43.82) | 50,456 (85) | 8829 (15) | |
| 41–64 Years | 58,980 (43.59) | 50,565 (86) | 8415 (14) | |
| ≥65 Years | 16,898 (12.64) | 16,098(94) | 940 (6) | |
| Marital status | <0.0001 | |||
| Married | 6971 (5.15) | 6229 (89.36) | 742 (10.64) | |
| Single | 44,670 (33.01) | 37,607 (84.19) | 7063 (15.81) | |
| Widow/widower | 915 (0.68) | 872 (95.30) | 43 (4.70) | |
| Unknown/unspecified | 82,747 (61.16) | 72,411 (87.51) | 10,336 (12.49) | |
| Language | <0.0001 | |||
| English | 113,123 (83.61) | 96,053 (85.00) | 17,070 (15) | |
| Spanish | 20,222 (14.95) | 19,256 (95.00) | 966 (5) | |
| Other | 1958 (1.45) | 1810 (92) | 148 (8) | |
| Year | <0.0001 | |||
| 2020 | 47,717 (35.27) | 39,659 (83.11) | 8058 (16.89) | |
| 2021 | 48,879 (36.13) | 42,592 (87.14) | 6287 (12.86) | |
| 2022 | 38,707 (28.61) | 34,868 (90.08) | 3839 (9.92) | |
| Mean (Std. dev.) | Mean (Std. dev.) | Mean (Std. dev.) | ||
| Charlson comorbidity index | 0.23 (0.52) | 0.24 (0.53) | 0.15 (0.43) | <0.0001 |
| Number of days enrolled in Medicaid | 305.51 (87.38) | 303.35 (88.46) | 322.39 (78.07) | <0.0001 |
Figure 1.
Descriptive analysis of telemedicine use by pre-pandemic preventable hospitalization.
Regression analyses
On bivariate analyses (Table 2), there were greater odds of telemedicine use for primary care visits among those who had a pre-pandemic prior preventable hospitalization (OR: 1.94; 95% CI:1.83, 2.06), compared to those who did not have a prior preventable hospitalization. This relationship remained statistically significant when controlling for covariates excluding the Charlson comorbidity index (OR:1.80; CI: 1.70, 1.92). Controlling for the Charlson comorbidity index did not explain this relationship (OR:1.85; CI: 1.74, 1.96). These results were consistent on stratification by type of ACSH (acute and chronic).
Table 2.
Regression analyses of the relationship between telemedicine use and prior preventable hospitalizations (n = 135, 303).
| All preventable hospitalizations | Acute conditions | Chronic conditions | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Preventable hospitalization | |||||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.94 (1.83, 2.06)*** | 1.80 (1.70, 1.92) *** | 1.85 (1.74, 1.96) *** | 1.98 (1.89, 2.09) *** | 1.80 (1.71, 1.90) *** | 1.82 (1.73, 1.92) *** | 1.40 (1.34, 1.45) *** | 1.54 (1.48, 1.61) *** | 1.61 (1.55, 1.69) *** |
| Charlson comorbidity index | 0.79 (0.76, 0.82) *** | 0.80 (0.77, 0.83) *** | 0.76 (0.73, 0.79) *** | ||||||
| Race/ethnicity | |||||||||
| Non-Hispanic White | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| Non-Hispanic Black | 0.69 (0.65, 0.73) *** | 0.70 (0.66, 0.74) *** | 0.70 (0.66, 0.74) *** | 0.70 (0.67, 0.75) *** | 0.68 (0.64, 0.72) *** | 0.68 (0.65, 0.72) *** | |||
| Native American | 0.81 (0.74, 0.89) *** | 0.82 (0.75, 0.90) *** | 0.82 (0.75, 0.90) *** | 0.83 (0.76, 0.91) *** | 0.79 (0.72, 0.87) *** | 0.80 (0.73, 0.88) *** | |||
| Asian/Pacific Islander | 0.53 (0.45, 0.61) *** | 0.53 (0.46, 0.61) *** | 0.53 (0.46, 0.62) *** | 0.54 (0.46, 0.62) *** | 0.53 (0.46, 0.61) *** | 0.53 (0.46, 0.62) *** | |||
| Hispanic | 0.60 (0.57, 0.63) *** | 0.61 (0.58, 0.64) *** | 0.60 (0.58, 0.63) | 0.61 (0.58, 0.64) | 0.60 (0.57, 0.63) | 0.61 (0.58, 0.64) | |||
| Age (Years) | |||||||||
| 18–40 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| 41–64 Years | 0.93 (0.89, 0.97) *** | 0.96 (0.92, 1.00) | 0.95 (0.92, 0.99) * | 0.99 (0.95, 1.03) | 0.86 (0.82, 0.89) *** | 0.88 (0.84, 0.92) *** | |||
| ≥65 Years | 0.39 (0.35, 0.42) *** | 0.41 (0.38, 0.45) *** | 0.41 (0.37, 0.44) *** | 0.43 (0.40, 0.47) *** | 0.34 (0.31, 0.37) *** | 0.36 (0.33, 0.39) *** | |||
| Sex | |||||||||
| Male | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| Female | 0.88 (0.85, 0.92) *** | 0.87 (0.84, 0.91) *** | 0.86 (0.83, 0.90) *** | 0.85 (0.82, 0.89) *** | 0.91 (0.87, 0.95) *** | 0.90 (0.86, 0.94) *** | |||
| Primary Language | |||||||||
| English | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| Spanish | 0.42 (0.38, 0.46) *** | 0.43 (0.39, 0.47) *** | 0.42 (0.39, 0.46) *** | 0.43 (0.39, 0.47) *** | 0.40 (0.37, 0.44) *** | 0.41 (0.38, 0.45) *** | |||
| Other | 0.62 (0.50, 0.77) *** | 0.61 (0.49, 0.76) *** | 0.61 (0.49, 0.76) *** | 0.61 (0.49, 0.75) *** | 0.66 (0.53, 0.82) *** | 0.65 (0.53, 0.81) *** | |||
| Marital status | |||||||||
| Married | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| Single | 1.17 (1.05, 1.30) ** | 1.16 (1.05, 1.29) ** | 1.16 (1.05, 1.29) ** | 1.16 (1.04, 1.28) ** | 1.18 (1.07, 1.31) ** | 1.18 (1.06, 1.30) ** | |||
| Widow/ widower | 0.63 (0.42, 0.94) * | 0.64 (0.43, 0.95) * | 0.63 (0.43, 0.94) * | 0.64 (0.43, 0.96) * | 0.62 (0.42, 0.93) * | 0.63 (0.42, 0.94) * | |||
| Unspecified | 0.93 (0.84, 1.03) | 0.93 (0.84, 1.03) | 0.94 (0.85, 1.04) | 0.93 (0.84, 1.03) | 0.94 (0.85, 1.04) | 0.94 (0.85, 1.04) | |||
| Number of days enrolled in Medicaid | 1.00 (1.00, 1.00) *** | 1.00 (1.00, 1.00) *** | 1.00 (1.00, 1.00) *** | 1.00 (1.00, 1.00) *** | 1.00 (1.00, 1.00) *** | 1.00 (1.00, 1.00) *** | |||
| Year | |||||||||
| 2020 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |||
| 2021 | 0.75 (0.73, 0.77) *** | 0.75 (0.73, 0.77) *** | 0.75 (0.73, 0.77) *** | 0.75 (0.72, 0.77) *** | 0.75 (0.73, 0.77) *** | 0.75 (0.73, 0.77) *** | |||
| 2022 | 1.06 (0.95, 1.18) | 1.04 (0.93, 1.16) | 1.06 (0.95, 1.18) | 1.04 (0.93, 1.16) | 1.07 (0.96, 1.20) | 1.05 (0.94, 1.17) | |||
***p < 0.001; **p < 0.01; *p < 0.5.
Average predicted probability
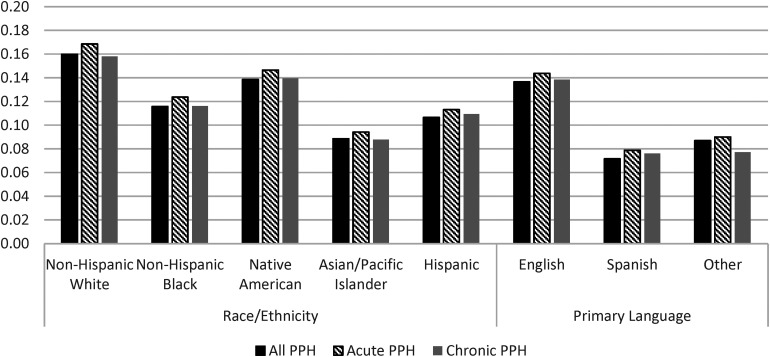
Figure 2 shows that among those who had a PPH, non-Hispanic White individuals had the highest predicted probability of using telemedicine during the pandemic (predicted probability: 0.16) followed by Native Americans (probability: 0.14), non-Hispanic Black (predicted probability: 0.12), Hispanic (predicted probability: 0.11), and Asian/Pacific Islanders (predicted probability: 0.09). Those whose primary language was English had the highest predicted probability of telemedicine use (predicted probability: 0.14) followed by those in the other category (predicted probability: 0.9) and then Hispanic patients (predicted probability: 0.7). These results were consistent when preventable hospitalizations were stratified by acute and chronic conditions
Figure 2.
Average predicted probability of race/ethnicity and primary language on telemedicine use among those with a pre-pandemic preventable hospitalization (PPH)*. * Predicted probability results from multivariable models adjusted for race/ethnicity, primary language, age, sex, number of days enrolled in Medicaid, marital status, year fixed effects, and comorbidity severity.
Discussion
In this study, we examined associations between a history of PPH and telemedicine use during the pandemic among Medicaid-insured patients of a safety-net academic health center with multiple FQHCs. To the best of our knowledge, this is one of the first studies to focus on this relationship among Medicaid-enrolled FQHC patients. We found that less than 1 in 5 of the study sample used telemedicine for an outpatient visit during the first year of the pandemic, with a persistent decline to about 1 in 10 in 2022. We also found that previous preventable hospitalization was associated with an increased likelihood of telemedicine use for outpatient visits. We found evidence of disparities in telemedicine use across race/ethnicity and primary language among those with a previous preventable hospitalization. Studies like this are informative, highlighting the role of telemedicine in optimizing healthcare use among underserved populations at risk for preventable hospitalizations. This study also underscores opportunities for practice and policy discussions and interventions to leverage this tool in a way that does not exacerbate disparities.
Our findings of increased odds of telemedicine use among Medicaid-insured individuals with PPH highlight the critical role that telemedicine could play in improving preventative healthcare visits for this subpopulation. This study presents evidence suggesting that individuals who have experienced preventable hospitalizations may become more proactive in seeking medical care through remote channels. This could be attributed to a desire to avoid repeated hospitalizations, minimize inconveniences, and enhance overall health management. 20 In addition, telemedicine could alleviate previously identified barriers such as transportation barriers, financial barriers related to transportation, tight work schedules, and lack of childcare that contribute to sub-optimal healthcare use. 17 Telemedicine use could also reduce travel burden barriers for patients living in medically underserved areas with limited provider availability. 20 The index study findings provide encouraging insight into the feasibility of using telehealth interventions to enhance health-seeking behavior and healthcare use among patients at risk for preventable hospitalizations.
It is however crucial to point out that low rates of telemedicine use among our study sample are an indication that proactive measures are needed to increase telemedicine use to ensure that the benefits of this tool are equally experienced across sub-groups. Further, analyses restricted to patients with a previous preventable hospitalization found a decreased probability of telemedicine use among minoritized racial and ethnic groups and those who did not speak English as a primary language. Previous studies that have explored telemedicine use during the COVID-19 pandemic have also reported a decreased likelihood of telemedicine use among minoritized patients and those whose primary language is not English.20,24–29 These disparities are worrisome given that minoritized populations often face a higher burden of chronic conditions as well as barriers to healthcare use that can be reduced by telemedicine use30–32 The decreased use of telemedicine could therefore exacerbate disrupted care continuity, which is more prevalent among minoritized individuals, further leading to preventable hospitalizations and increased healthcare costs. 33
Although disparate access to technology, such as smartphones, computers, and reliable internet, also known as the digital divide, is on a steady decline; minoritized individuals continue to be disproportionately affected by this phenomenon. 34 This divide could hinder the ability of this subpopulation to engage with telemedicine platforms, limiting their access to virtual care. Additionally, telemedicine platforms might not adequately address language preferences or cultural sensitivities, leading to communication barriers that might deter minoritized individuals from seeking virtual care. This could also be the explanation for our finding of decreased likelihood of telemedicine use among those whose primary language was not English. Limited digital literacy among minoritized individuals could also contribute to the disparities noted in our study.35,36 It is also possible that minoritized individuals might prefer in-person visits or could mistrust virtual visits, hence exhibiting a preference for in-person clinic visits. Future studies are needed to understand telemedicine use preference as well as identify and address barriers to telemedicine use among patients with previous preventable hospitalizations.
The COVID-19 pandemic-related policy changes that allowed for increased implementation and/or expansion of telemedicine and the resultant uptake by patients suggest that telemedicine is here to stay. However, the expansion has also highlighted the limitations of telemedicine use in clinical care and the need for research aimed at identifying best practices for telemedicine use in clinical care across disease conditions. The persistent disparities in telemedicine use will limit the generalizability of such findings and any associated guidelines and potentially exacerbate health and healthcare inequities. It is therefore critical to understand the reasons for low telemedicine use among underserved populations with a history of sub-optimal preventative care use.
Several limitations should be considered when reviewing these findings. First, our study is limited to Medicaid-insured patients of a single, although large, multisite academic safety-net healthcare system of a single state and therefore might not be generalizable to other healthcare settings. Second, our use of claims data limits our ability to control for other factors that could contribute to telemedicine use among our study sample. Third, data limitations did not allow us to delineate between audio-only and audio-visual visits, an important factor when considering telemedicine use. Fourth, our study is limited by the study period that ends in June 2023. Future studies using more recent data are needed to understand whether the observed patterns have persisted. Fifth, we cannot imply causality given the cross-sectional nature of our data.
Our study has noteworthy strengths. First, our study provides insights into the use of telemedicine among patients with a history of sub-optimal preventative care use, as well as disparities in telemedicine use among this subpopulation. Second, prior studies usually classify Native Americans in the “other” category due to limited observations; however, the high proportion of Native Americans in our study allowed us to look at this group independently and has strengthened our contribution to the literature. Third, our use of administrative claims data reduces the likelihood of measurement error due to self-reports.
In conclusion, the escalating telemedicine adoption among patients highlights technology's transformational impact on healthcare delivery. Our study findings indicate that interventions that seek to leverage telemedicine to optimize healthcare use and health outcomes among patients with a PPH should strive to identify and address barriers to telemedicine use among minoritized patients and those whose primary language is not English.
Acknowledgments
The Arizona Health Care Cost Containment System (AHCCCS) claims and encounter data used in this study were provided by the Arizona State University, Center for Health Information Research (CHiR).
Footnotes
Contributorship: COO: conceptualization, data analyses, and initial draft; LJ: data curation; LN, SY, and OA: reviewed multiple drafts for interpretation and intellectual content; MD reviewed for intellectual content.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Arizona State University College of Health Solutions Jumpstart grant (PG15125). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation or approval of the manuscript; and decision to submit the manuscript for publication.
Ethical approval: This study was approved by the Arizona State University Institutional Review Board.
Guarantor: Chinedum O. Ojinnaka takes full responsibility for the article, including for the accuracy and appropriateness of the reference list.
ORCID iD: Chinedum O Ojinnaka https://orcid.org/0000-0002-4535-5820
References
- 1.Agency for Healthcare Research and Quality. AHRQ Quality Indicators Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions, 2001. https://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf. Accessed 03/26/2019.
- 2.Purdy S, Griffin T, Salisbury C, et al. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009; 123: 169–173. [DOI] [PubMed] [Google Scholar]
- 3.Billings J, Zeitel L, Lukomnik J, et al. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993; 12: 162–173. [DOI] [PubMed] [Google Scholar]
- 4.Basu J, Friedman B, Burstin H. Primary care, HMO enrollment, and hospitalization for ambulatory care sensitive conditions: a new approach. Med Care 2002; 40: 1260–1269. [DOI] [PubMed] [Google Scholar]
- 5.Torio CM and Andrews RM. Geographic variation in potentially preventable hospitalizations for acute and chronic conditions, 2005–2011. 2014 Sep. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-. Statistical Brief #178. Available from: https://www.ncbi.nlm.nih.gov/books/NBK253887/.
- 6.McDermott KW and Jiang HJ. Characteristics and costs of potentially preventable inpatient stays, 2017. 2020 Jun 16. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-. Statistical Brief #259. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559945/. [PubMed]
- 7.Biello KB, Rawlings J, Carroll-Scott A, et al. Racial disparities in age at preventable hospitalization among U.S. Adults. Am J Prev Med 2010; 38: 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang CF, Pope RA. Potentially avoidable hospitalizations in Tennessee: analysis of prevalence disparities associated with gender, race, and insurance. Public Health Rep 2009; 124: 127–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boersma P, Black LI, Ward BW. Prevalence of multiple chronic conditions among US adults, 2018. Prev Chronic Dis 2020; 17: E106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDermott KW, Jiang HJ. Characteristics and Costs of Potentially Preventable Inpatient Stays, 2017: Statistical Brief# 259. In:2020. [PubMed]
- 11.Laditka JN, Laditka SB. Insurance status and access to primary health care: disparate outcomes for potentially preventable hospitalization. J Health Soc Policy 2004; 19: 81–100. [DOI] [PubMed] [Google Scholar]
- 12.Chopra I, Wilkins TL, Sambamoorthi U. Ambulatory care sensitive hospitalizations among medicaid beneficiaries with chronic conditions. Hospital Practice (1995) 2016; 44: 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laditka JN, Laditka SB, Mastanduno MP. Hospital utilization for ambulatory care sensitive conditions: health outcome disparities associated with race and ethnicity. Soc Sci Med 2003; 57: 1429–1441. [DOI] [PubMed] [Google Scholar]
- 14.Pérez-Stable EJ, Jean-Francois B, Aklin CF. Leveraging advances in technology to promote health equity. Med Care 2019; 57(Suppl 6, Suppl 2): S101–s103. [DOI] [PubMed] [Google Scholar]
- 15.Gruman JC. Making health information technology sing for people with chronic conditions. Am J Prev Med 2011; 40(Suppl 2): S238–S240. [DOI] [PubMed] [Google Scholar]
- 16.Gage-Bouchard EA. Social support, flexible resources, and health care navigation. Soc Sci Med 2017; 190: 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013; 38: 976–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jia H, Chuang HC, Wu SS, et al. Long-term effect of home telehealth services on preventable hospitalization use. J Rehabil Res Dev 2009; 46: 557–566. [DOI] [PubMed] [Google Scholar]
- 19.Friedman RSC, Carpenter DM, Shaver JM, et al. Telemedicine familiarity and post-disaster utilization of emergency and hospital services for ambulatory care sensitive conditions. Am J Prev Med 2022; 63: e1–e9. [DOI] [PubMed] [Google Scholar]
- 20.Li KY, Ng S, Zhu Z, et al. Association between primary care practice telehealth use and acute care visits for ambulatory care-sensitive conditions during COVID-19. JAMA Netw Open 2022; 5: e225484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173: 676–682. [DOI] [PubMed] [Google Scholar]
- 23.Coorbidty C. Charlson Comorbidity Index, http://mchp-appserv.cpe.umanitoba.ca/Upload/SAS/_CharlsonICD10.sas.txt. Published n.d. Accessed 04.12.2024.
- 24.Chen EM, Andoh JE, Nwanyanwu K. Socioeconomic and demographic disparities in the use of telemedicine for ophthalmic care during the COVID-19 pandemic. Ophthalmology 2022; 129: 15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriguez JA, Betancourt JR, Sequist TD, et al. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021; 27: 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare 2023; 29(1): 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adepoju OE, Chae M, Ojinnaka CO, et al. Utilization gaps during the COVID-19 pandemic: racial and ethnic disparities in telemedicine uptake in Federally Qualified Health Center clinics. J Gen Intern Med 2022; 37(5): 1191–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arora A, Fekieta R, Nouri Z, et al. Trends in utilization of electronic consultations associated with patient payer and language among US academic medical centers during the COVID-19 pandemic. JAMA Netw Open 2022; 5: e2224628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiong G, Greene NE, Lightsey H, et al. Telemedicine use in orthopaedic surgery varies by race, ethnicity, primary language, and insurance Status. Clin Orthop Relat Res 2021; 479: 1417–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quiñones AR, Botoseneanu A, Markwardt S, et al. Racial/ethnic differences in multimorbidity development and chronic disease accumulation for middle-aged adults. PLoS One 2019; 14: e0218462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang N, Fujimoto J, Karliner L. Evaluation of a primary care-based post-discharge phone call program: keeping the primary care practice at the center of post-hospitalization care transition. J Gen Intern Med 2014; 29: 1513–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bindman AB, Cox DF. Changes in health care costs and mortality associated with transitional care management services after a discharge among medicare beneficiaries. JAMA Intern Med 2018; 178: 1165–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc 2003; 51: 556–557. [DOI] [PubMed] [Google Scholar]
- 34.Eberly LA, Khatana SAM, Nathan AS, et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic: bridging or opening the digital divide? Circulation 2020; 142: 510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cunha AS, Pedro AR, Cordeiro JV. Facilitators of and barriers to accessing hospital medical specialty telemedicine consultations during the COVID-19 pandemic: systematic review. J Med Internet Res 2023; 25: e44188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eruchalu CN, Pichardo MS, Bharadwaj M, et al. The expanding digital divide: digital health access inequities during the COVID-19 pandemic in New York City. J Urban Health 2021; 98: 183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]