Abstract
Background:
Traumatic middle cerebral artery (MCA) pseudoaneurysms following minor head trauma are rare.
Case Description:
We report a case of a 76-year-old man who presented with a traumatic acute subdural hematoma and subarachnoid hemorrhage (SAH) from a ruptured distal right MCA pseudoaneurysm treated with evacuation of the hematoma, resection of the pseudoaneurysm, and an MCA-to-MCA bypass.
Conclusion:
Although traumatic pseudoaneurysms of the distal intracranial vessels are rare, patients with traumatic SAH would benefit from vascular imaging. Treatment of pseudoaneurysms of distal intracranial vessels may be treated with vessel occlusion or trapping/excision of aneurysm with revascularization.
Keywords: Middle cerebral artery, Pseudoaneurysm, Subdural hematoma, Trauma
INTRODUCTION
Ruptured traumatic intracranial pseudoaneurysms following closed-head injuries are rare, highly fatal, and require immediate surgical intervention.[1-3,5] Fewer than 1% of cerebral aneurysms are traumatic intracranial pseudoaneurysms, most often occurring in the internal carotid artery after major head trauma.[1,2,6,8] Traumatic middle cerebral artery (MCA) pseudoaneurysms following seemingly trivial head trauma are even more remarkable and subsequently scantly documented in the literature.[1-4,6,7] We present a case of ruptured traumatic MCA pseudoaneurysm following a closed-head injury treated with direct MCA-to-MCA bypass and excision of the ruptured pseudoaneurysm.
CASE REPORT
A 76-year-old man with a medical history significant for atrial fibrillation being managed with apixaban and chronic kidney disease stage 3 presented to the emergency department (ED) with headache, left hemiparesis, slight left facial droop, and altered mental status after an unwitnessed fall with head strike on the day of admission without skull fracture. Computed tomography (CT) of the head demonstrated an acute 18 mm right subdural hematoma (SDH) with subarachnoid hemorrhage (SAH), causing an 8 mm midline shift [Figure 1]. Preoperative CT angiography (CTA) of the head showed a 4 mm distal right MCA pseudoaneurysm adjacent to the SDH [Figure 1]. The patient was administered andexanet alfa to reverse the anticoagulation and taken emergently to the operating room for evacuation of the SDH and repair of the pseudoaneurysm.
Figure 1:
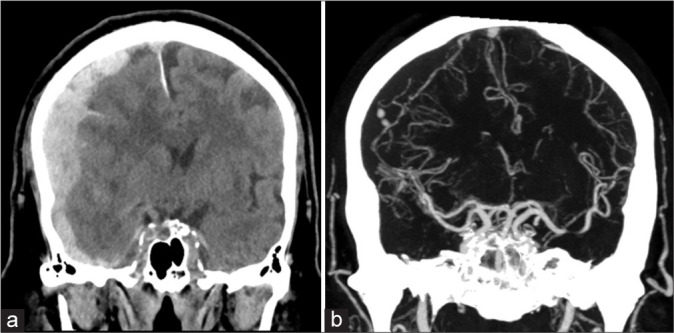
(a) Preoperative non-contrast coronal head computed tomography (CT) demonstrates right holohemispheric acute subdural hematoma and subarachnoid hemorrhage with midline shift. (b) Preoperative coronal CT angiography demonstrates a 4 mm distal right middle cerebral artery pseudoaneurysm adjacent to the subdural hematoma.
A frontotemporal craniotomy was performed, and the SDH was evacuated with no evidence of skull fracture noted. Removal of the hematoma exposed an area of platelet plug overlying the pseudoaneurysm that had disrupted the arachnoid membrane [Figure 2]. There was a clear disruption of the vessel wall with no aneurysmal dilation to suggest a preexisting aneurysm [Figure 2]. Temporary clips were placed proximal and distal to the pseudoaneurysm, and the area of vessel injury was resected to a clean edge [Figure 2]. An end-to-end anastomosis was performed using 10-0 nylon sutures. Administration of indocyanine green dye confirmed good patency of the anastomosis [Figure 2]. The patient was extubated immediately after surgery and, by postoperative day 1, demonstrated significant improvement in the left hemiparesis and headaches. Immediate postoperative head CT showed improvement in midline shift and previously noted SDH, as well as patency of the involved MCA branch [Figure 3]. On postoperative day 6, he was discharged to inpatient rehabilitation.
Figure 2:
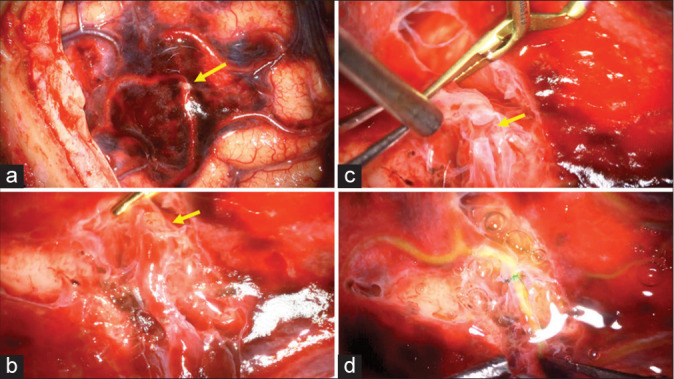
Intraoperative images showing (a) a platelet plug (arrow) disrupting the arachnoid membrane corresponding to the pseudoaneurysm, (b) The disrupted middle cerebral artery with a platelet plug (arrow) after removal of the overlying arachnoid. (c) The pseudoaneurysm (arrow) was resected to a clean edge proximally and distally. (d) Demonstration of good patency throughout the anastomosis after administration of indocyanine green dye.
Figure 3:
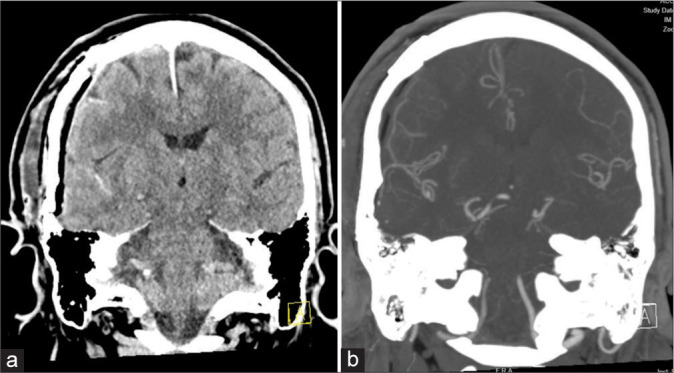
Postoperative coronal computed tomography (CT) and CT angiography show (a) improvement in both midline shift and subdural hematoma and (b) resection of pseudoaneurysm with patent distal middle cerebral artery.
DISCUSSION
Traumatic pseudoaneurysms are most commonly caused by head trauma.[1,2,8] Compared to extracranial arteries, intracranial arteries lack external elastic lamina and have comparatively thicker internal elastic lamina, leading them to be thinner and stiffer than extracranial arteries and subsequently more vulnerable to injury.[8] It has been proposed that traumatic pseudoaneurysms occur at points where the surface vessels are either strongly adherent to the dura or supply small dural branches and, with potentially abrupt accelerative or decelerative forces secondary to head trauma, lead to lacerations in the artery.[5] In a review of 28 cases of MCA pseudoaneurysms, 72.4% of traumatic MCA pseudoaneurysms ruptured, with 43.5% of patients experiencing a delayed rupture.[1] The average time from trauma to rupture was 4.7 days.[1] Of these 28 cases, the majority of the lacerations occurred in the cortical branches, and 43.5% of cases had no skull fracture.[1]
Digital subtraction angiography (DSA) is the gold standard for diagnosing intracranial pseudoaneurysms, given the low sensitivity of CTA and magnetic resonance angiography (MRA) for small aneurysms.[7] In addition, vessel imaging immediately after trauma may not demonstrate evidence of traumatic pseudoaneurysms, which can manifest in a delayed state, resulting in false-negative results.[1,6-8] For example, a 23-year-old male injured in a motorcycle accident presented to the ED with a Glasgow Coma Scale of 7 and thick SAH with no vascular lesions detected on the initial 3D CTA.[6] A brain MRA showed progressive M1 stenosis, suggesting traumatic SAH-induced vasospasm, and a repeat CTA 20 days after admission revealed a small M2 aneurysm. Four days after this finding, the pseudoaneurysm ruptured, and the patient developed hemiparesis and new SAH requiring emergent superficial temporal artery-M2 bypass with trapping of the ruptured pseudoaneurysm.[6] As such, although initial workup for vascular abnormalities may be negative on initial diagnostic imaging, in cases where thick SAH follows head trauma, delayed imaging is recommended to detect late-emerging pseudoaneurysms and allow for immediate surgical intervention.[6-8] At present, there is no standardized time interval for repeat angiograms to detect delayed-onset traumatic pseudoaneurysms following head trauma established in the literature.[8]
As in the case mentioned above, most ruptured traumatic MCA pseudoaneurysms follow major trauma, with very few instances of ruptured traumatic MCA pseudoaneurysms from minor head trauma resulting in SDH.[1-3,7] One such case involves a 75-year-old man who suffered a head strike against a floor mat, initially maintaining consciousness, only to deteriorate 13 hours later. Similar to the case we present herein, this patient presented with altered mental status and hemiparesis with a CT scan revealing SDH and trace SAH in the Sylvian fissure due to a ruptured MCA pseudoaneurysm.[3] The clinical course to follow was also similar to our case, with the patient making a sufficient recovery after surgical intervention to evacuate the SDH and extirpation of the aneurysm followed by rehabilitation.[3] Similarly, another ruptured MCA pseudoaneurysm case following minor head trauma involved a 79-year-old male who presented to the ED with altered mental status 2 weeks after a mechanical fall with a head strike.[7] CT revealed a 3 mm left frontoparietal SDH with 5 mm of midline shift to the right; no skull fracture was noted.[7] Three days after presentation, the patient developed right-sided weakness and expressive aphasia with contrast MRI revealing an expansion of the SDH to 10 mm and DSA demonstrating a 6 mm cortical MCA pseudoaneurysm.[7] Cases such as these further emphasize the need for serial neurovascular evaluation and consideration of traumatic pseudoaneurysms in the differential diagnoses of patients with acute neurological deterioration after seemingly trivial closed-head injuries.[2,3,7,8]
Trapping traumatic pseudoaneurysms with or without bypass revascularization is a definitive surgical treatment for intracranial pseudoaneurysms with associated acute hematomas.[4] However, endovascular treatments for traumatic pseudoaneurysms are rapidly evolving as an alternative to open surgical management.[2,7] Current endovascular options for traumatic pseudoaneurysms include parent vessel occlusion, coil embolization, stentassisted/balloon-assisted coiling, and covered stents.[4] However, preserving branch arteries remains challenging.[4] To avoid irreversible complications, super-selective balloon occlusion tests to account for essential side branches or perforating arteries should be performed before deploying a covered stent or before performing a vessel occlusion.[4]
CONCLUSION
Although traumatic pseudoaneurysms of the distal intracranial vessels are rare, patients with traumatic SAH would benefit from vascular imaging. Pseudoaneurysms of distal intracranial vessels may be treated with vessel occlusion or trapping/excision of the aneurysm with revascularization.
Footnotes
How to cite this article: Tirado S, Bass DI, Feroze A, Johnston B, Bi WL, Du R. Ruptured traumatic pseudoaneurysm of the middle cerebral artery following minor trauma treated with an MCA-MCA bypass: A case report. Surg Neurol Int. 2024;15:247. doi: 10.25259/SNI_373_2024
Contributor Information
Selena-Rae Tirado, Email: stirado1@bwh.harvard.edu.
David I. Bass, Email: dbass2@bwh.harvard.edu.
Abdullah Feroze, Email: aferoze@bwh.harvard.edu.
Benjamin Johnston, Email: bjohnston2@mgb.org.
Wenya Linda Bi, Email: wbi@bwh.harvard.edu.
Rose Du, Email: rdu@bwh.harvard.edu.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Horiuchi T, Nakagawa F, Miyatake M, Iwashita T, Tanaka Y, Hongo K. Traumatic middle cerebral artery aneurysm: Case report and review of the literature. Neurosurg Rev. 2007;30:263–7. doi: 10.1007/s10143-007-0073-9. [DOI] [PubMed] [Google Scholar]
- 2.Larson PS, Reisner A, Morassutti DJ, Abdulhadi B, Harpring JE. Traumatic intracranial aneurysms. Neurosurg Focus. 2000;8:e4. doi: 10.3171/foc.2000.8.1.1829. [DOI] [PubMed] [Google Scholar]
- 3.Murakami M, Kakita K, Hosokawa Y. Ruptured traumatic aneurysm after trivial injury mimicking acute spontaneous subdural hematoma--case report. Neurol Med Chir (Tokyo) 2003;43:130–3. doi: 10.2176/nmc.43.130. [DOI] [PubMed] [Google Scholar]
- 4.Shi Y, Gao Y, Liu Y, Cui W, Zhou G, Wang L, et al. Treatment of traumatic intracranial pseudoaneurysms: A single-center experience. Front Neurol. 2021;12:690284. doi: 10.3389/fneur.2021.690284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith DR, Kempe LG. Cerebral false aneurysm formation in closed head trauma; case report. J Neurosurg. 1970;32:357–9. doi: 10.3171/jns.1970.32.3.0357. [DOI] [PubMed] [Google Scholar]
- 6.Somiya D, Sakamoto Y, Maeda K, Takasu S, Takemoto M, Choo J, et al. Ruptured proximal middle cerebral artery traumatic pseudoaneurysm treated with bypass-assisted trapping surgery: A case report. Surg Neurol Int. 2023;14:263. doi: 10.25259/SNI_344_2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varma S, Banh L, Smith P. Traumatic aneurysm of the cortical middle cerebral artery. BMJ Case Rep. 2017;2017:bcr2017219301. doi: 10.1136/bcr-2017-219301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zheng Y, Lu Z, Shen J, Xu F. Intracranial pseudoaneurysms: Evaluation and management. Front Neurol. 2020;11:582. doi: 10.3389/fneur.2020.00582. [DOI] [PMC free article] [PubMed] [Google Scholar]


