Abstract
This study was to translate the Pieper–Zulkowski pressure ulcer knowledge test (PZ‐PUKT) into Traditional Chinese and evaluate its psychometric properties as well as identify the predictors of knowledge on pressure injury. The PZ‐PUKT was translated into Traditional Chinese (TC‐PZ‐PUKT), and its content validity was evaluated. A total of 296 nurses participated in this study and completed the 72‐item TC‐PZ‐PUKT online. The reliability of the TC‐PZ‐PUKT was analysed by evaluating its internal consistency and test–retest reliability. Hierarchical regression was used to determine factors associated with TC‐PZ‐PUKT scores. Content validity was achieved with a score of 0.986. Internal consistency was observed to be reliable, with a Cronbach's alpha of 0.858. The mean knowledge score on the TC‐PZ‐PUKT was 72.5%, with a 1‐week test–retest reliability of r = 0.849. Education level, certification as a wound specialist and self‐learning through reading articles, books or guidelines on pressure injury were significantly associated with TC‐PZ‐PUKT scores. The TC‐PZ‐PUKT is a valid and reliable tool. Education level, certification as a wound specialist and self‐learning regarding pressure injury are related to knowledge of pressure injury.
Keywords: education, knowledge of pressure injury, pressure injury, questionnaire
1. INTRODUCTION
Pressure injury is a major healthcare problem. A meta‐analysis reported that the overall prevalence and cumulative incidence of pressure injury ranged from 0.47% to 31.2% and from 3.7% to 27%, respectively. 1 Current guidelines for prevention and treatment of pressure injury include 22 recommendations and good practice statements. 2 Training programs can enhance nurses' knowledge, visual discrimination ability and clinical judgement regarding pressure injury. 3 The effectiveness of such training programs can be evaluated using the pressure injury classification system 4 and knowledge questionnaires, such as the pressure ulcer assessment test 5 and the Pieper–Zulkowski pressure ulcer knowledge test (PZ‐PUKT). 6
In 2014, Pieper and Zulkowski developed a 72‐item tool for assessing pressure ulcer knowledge, that is, the PZ‐PUKT, by referencing clinical practice guidelines for the prevention and treatment of pressure ulcers and Wound, Ostomy, and Continence Nurses Society guidelines for the prevention and management of pressure ulcers. 6 The PZ‐PUKT demonstrated strong reliability and validity 6 and has been translated into multiple languages, including Brazilian Portuguese, 7 Portuguese, 8 Turkey 9 and simple Chinese. 10 A cutoff score of 60% or higher on the PZ‐PUKT indicates a satisfactory overall level of knowledge regarding pressure injury. 11
A previous study used the PZ‐PUKT to investigate the knowledge of pressure injury among nurses working in an intensive care unit, where the corrected rate for knowledge of pressure injury was 51.66% (standard deviation [SD] = 5.97). The study determined that nurses with 5 years of experience had more knowledge regarding pressure injury, as indicated by higher scores, than did nursing staff with more than 20 years of experience. 12 Another study reported that the corrected rates of pressure injury knowledge significantly differed among nurses of different job categories and that scores were negatively associated with nurses' age and years of nursing practice. 10
Based on the langue culture difference form simple Chinese, this study translated the PZ‐PUKT into Traditional Chinese (TC‐PZ‐PUKT) and examined its validity and reliability. In addition, we investigated the association between nurses' knowledge regarding pressure injury and their years of clinical nursing experience. Moreover, we explored whether nurses' self‐learning behaviour regarding pressure injuries could enhance their knowledge on this topic.
2. MATERIALS AND METHODS
2.1. Translation of the PZ‐PUKT and content validity assessment
The PZ‐PUKT comprises 72 items and assesses three domains: prevention (31 items), staging (21 items) and wound care (20 items). 1 After receiving approval from Drs. Barbara Pieper and Karen Zulkowski, we translated the PZ‐PUKT into Traditional Chinese. On this test, each correct response is assigned a score of 1, and incorrect or ‘I don't know’ responses are assigned a score of 0. The total score ranges from 0 to 72, with the score then converted to a percentage value ranging from 0 to 100.
2.1.1. Forward translation
We translated the PZ‐PUKT from English into Traditional Chinese by using Brislin's translation model. 2 In the initial phase, two bilingual registered nurses who were proficient in English conducted a forward translation of the PZ‐PUKT into Traditional Chinese. Subsequently, a meeting was conducted to discuss any inconsistencies in the translation, and the first edition of the TC‐PZ‐PUKT was produced. In a second consensus meeting, three clinical nurses evaluated the first edition of the TC‐PZ‐PUKT in terms of its clarity and how easily nurses would be able to understand it in a clinical setting. The feedback from the three nurses confirmed that the Traditional Chinese version was comprehensible, and consequently, the second edition of the TC‐PZ‐PUKT was finalized.
2.1.2. Backward translation
The third step involved back translation, where the second edition of the TC‐PZ‐PUKT was independently translated back into English by two English‐speaking experts who were familiar with Chinese. Subsequently, the translated version was reviewed by clinical nurses to ensure semantic accuracy.
2.1.3. Evaluation of content validity
To assess the content validity of the TC‐PZ‐PUKT, a group of seven experts, comprising a nursing professor; two international wound, ostomy and continence nurses; two nursing administration supervisors; one clinical nurse and a chief surgeon, evaluated the questionnaire. The assessment criteria included the relevance of the questions to the research topic, the appropriateness of the question content and the semantic clarity of the descriptions. A content validity index was used to measure content validity, with each item scored on a 4‐point Likert scale (1 = irrelevant, 2 = weakly relevant, 3 = strongly relevant and 4 = absolutely relevant). Any content with a score of lower than 3 was revised based on the experts' suggestions.
2.2. Participants and data collection
We used an online questionnaire to collect data and assess knowledge of pressure injuries from August to September 2021. Clinical nurses or nursing practitioners who were able to answer the online questionnaire were considered eligible for participation. Individuals were excluded if they were unable to participate in the retest, which was scheduled for 1 week after the first test. We recruited 300 participants, and 100 were randomly selected to complete the retest after 1 week. The characteristics such as age, sex, education level, job category, nursing practice setting, years in nursing practice and certification as a wound specialist were collected. The learning behaviours related to pressure injury knowledge within the past from participants were also collected in this study. This study was approved by the institutional review board (Hualien Tzu Chi Hospital Research Ethics Committee No. IRB110‐087‐B).
2.2.1. Internal consistency reliability
To assess internal consistency reliability, correlations among the 72 items of the TC‐PZ‐PUKT scale were analysed, and the results were evaluated using Cronbach's α. Values exceeding 0.70 were considered to indicate acceptable internal consistency reliability. 3
2.2.2. Test–retest reliability
We determined the test–retest reliability of the 72‐item TC‐PZ‐PUKT by measuring the percentage of correct responses for each item on the pretest and on the retest. We evaluated the test–retest reliability for the total score and the domains of prevention, staging and wound care. Correlation coefficients were calculated, and weighted kappa values were used to estimate test–retest reliability. The interclass correlation coefficients ranged from 0 to 1, with levels considered acceptable (0.50–0.75), confident (0.75–0.90) and perfect (>0.90). 4
2.3. Statistical analysis
Data were retrieved from an online Excel file and analysed using SPSS, version 17.0 (Statistical Package for the Social Sciences, Chicago, IL, USA). The TC‐PZ‐PUKT scores for the prevention, staging and wound care domains and the total scores were calculated as percentages. Descriptive statistics, presented as means and percentages, were used in analyses. We analysed the internal consistency reliability, test–retest reliability, content validity and concurrent validity. Hierarchical regression was performed to identify factors related to knowledge of pressure injury. The significance level was set at p < 0.05.
3. RESULTS
Of the 300 participants, data were unavailable for 4. Thus, we included 296 participants in our analysis. In terms of demographics, the average age of the participants was 38.5 (SD = 9.9) years, and 95.6% of the participants were women, 70.9% held baccalaureate degrees, 86.5% were registered nurses, 13.5% were nursing practitioners, 90.0% worked in hospitals, 34.1% had more than 20 years of nursing experience and 15.9% were certified as wound specialists (Table 1).
TABLE 1.
Demographic characteristics of participants (N = 296).
| Variables | Mean | SD |
|---|---|---|
| Age | 38.5 | 9.9 |
| n | % | |
|---|---|---|
| Sex | ||
| Male | 13 | 4.4 |
| Female | 283 | 95.6 |
| Education level | ||
| Associate | 40 | 13.5 |
| Baccalaureate | 210 | 70.9 |
| Master's or doctorate | 46 | 15.5 |
| Job category | ||
| Registered nurse | 256 | 86.5 |
| Nursing practitioner | 40 | 13.5 |
| Nursing practice setting | ||
| Hospital | 269 | 90.9 |
| Long‐term care facility | 11 | 3.7 |
| Home care setting | 16 | 5.4 |
| Years in nursing practice | ||
| <1 year | 12 | 4.1 |
| 1–5 years | 44 | 14.9 |
| 5–10 years | 39 | 13.2 |
| 10–15 years | 53 | 17.9 |
| 15–20 years | 47 | 15.9 |
| >20 years | 101 | 34.1 |
| Certification as a wound specialist | 47 | 15.9 |
The content validity analysis of the TC‐PZ‐PUKT revealed that items 10, 19, 20, 54 and 64 required minor modifications to achieve equivalence. A review by five experts revealed the final version to have an average score of 4 for clarity of wording, resulting in a content validity index value of 0.986.
For internal consistency reliability, the Cronbach's alpha was determined to be 0.858. For the test–retest reliability of the TC‐PZ‐PUKT, significant reliability was noted for the total score and the scores of the prevention, staging and wound care domains (r = 0.849, 0.768, 0.662 and 0.793, respectively; all p < 0.001).
For learning behaviours related to pressure injury knowledge, this study indicates that 47.6% had listened to a lecture on the topic in the past year; 49.7% had read an article, a book or guidelines on pressure injury in the past year; and 70.3% of the participants had sought information online regarding pressure injuries in the past year.
Junior nurses (with <1 year of nursing practice) had the lowest corrected scores on the TC‐PZ‐PUKT in the prevention, staging and wound care domains and lowest total scores; the average values (SD) were 75.5 (13.1), 61.1 (8.1), 55.4 (8.4) and 65.7 (7.3), respectively (Figure 1).
FIGURE 1.
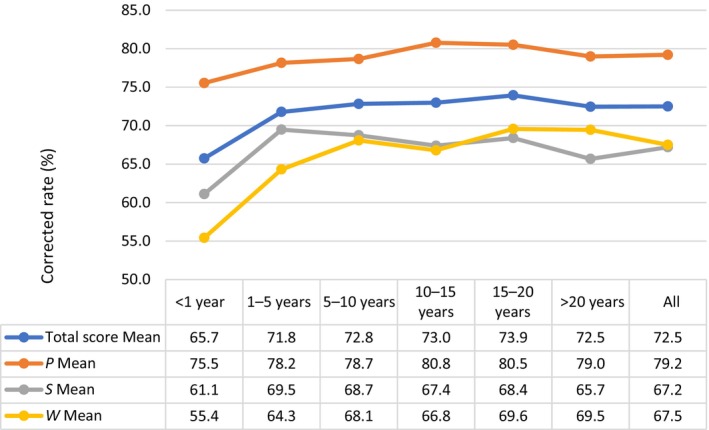
Trends in corrected rates of pressure injury knowledge and years of clinical practice. (P = prevention, S = staging, W = wound care domans).
Table 2 lists the results of two‐step hierarchical regression analysis. The first step of the analysis identified education level (β = 0.11, p = 0.031), job category (β = 0.07, p = 0.192), years in nursing practice (β = −0.09, p = 0.071) and certification as a wound specialist (β = 0.55, p < 0.001) as significant predictors of knowledge on pressure injury (R 2 = 0.31, p < 0.001). The second step of the analysis identified having listened to a lecture on pressure injury in the past year (β = 0.06, p = 0.317); having read an article, a book or guidelines on pressure injuries in the past year (β = 0.16, p = 0.006); and having listened to a lecture on pressure injuries in the past year (β = 0.05, p = 0.294) as significant predictors of knowledge on pressure injuries (R 2 = 0.36, p < 0.001). These factors explained 4% of the variance in knowledge on pressure injuries (ΔR 2 = 0.04, p < 0.001).
TABLE 2.
Hierarchical regression analysis for knowledge on pressure injury (N = 269).
| Variables | Step 1 | Step 2 | ||||
|---|---|---|---|---|---|---|
| β | t | p‐Value | β | t | p‐Value | |
|
Education level (0: Associate; 1: Baccalaureate; 2: Master's or Doctorate) |
0.11 | 2.17 | 0.031 | 0.10 | 2.09 | 0.038 |
|
Job category (0: Registered nurse; 1: Nursing practitioner) |
0.07 | 1.31 | 0.192 | 0.07 | 1.53 | 0.128 |
|
Years in nursing practice (0: <1 year; 1: 1–5 years; 2: 5–10 years; 3: 10–15 years; 4: 15–20 years; 5: >20 years) |
−0.09 | −1.81 | 0.071 | −0.07 | −1.30 | 0.195 |
|
Certification as wound specialist (0: no; 1: yes) |
0.55 | 10.92 | <0.001 | 0.47 | 8.94 | <0.001 |
| Listened to a lecture on pressure injury within the past year | 0.06 | 1.00 | 0.317 | |||
| Read an article, a book or guidelines on pressure injury within the past year | 0.16 | 2.74 | 0.006 | |||
| Sought information about pressure injuries on the web within the past year | 0.05 | 1.05 | 0.294 | |||
| R 2 | 0.31 | 0.36 | ||||
| ΔR 2 | – | 0.04 | ||||
| F/p | 32.89/<0.001 | 22.65/<0.001 | ||||
| ΔF/Δp | – | 10.24/<0.001 | ||||
4. DISCUSSION
This study revealed the TC‐PZ‐PUKT to have satisfactory internal consistency reliability for clinical nurses. In addition, we assessed the test–retest reliability of the TC‐PZ‐PUKT for the three domains of prevention, staging and wound care. Our findings revealed satisfactory correlation coefficients ranging from 0.6 to 0.8. Education level; certification as a wound specialist and self‐learning through reading articles, books or guidelines on pressure injury were identified as significant predictors of PZ‐PUKT scores. The PZ‐PUKT is a comprehensive tool for evaluating healthcare professionals' knowledge of pressure injury. 5 Training programs on pressure injury can enhance nurses' competencies, and measurement tools can be used to assess outcomes in clinical judgement and knowledge. 6
The quality of care for pressure injury is influenced by prevention and wound care skills, which are affected by knowledge, attitude and practice. 7 Various instruments, such as the PUKT and the pressure ulcer knowledge assessment tool, have been used to assess nurses' wound care knowledge, and these measures were determined to be valid and reliable. 8 However, strong evidence is not always available for all wound types and clinical situations, leading healthcare professionals to frequently rely on practical recommendations provided in consensus guidelines for clinical care. 8 , 9 The PZ‐PUKT is a valid measurement tool developed by Pieper and Zulkowski with reference to guidelines for pressure injury care. 1
A systematic literature review indicated that the PZ‐PUKT is among the most used, most effective, and most reliable tools for measuring nurses' knowledge of pressure injury. 8 The PZ‐PUKT has also been validated and has been used to assess healthcare workers' knowledge on pressure injury in Brazil, China, and the Philippines. 10 , 11 The Cronbach's alpha coefficient of the PUKT ranges from 0.35 to 0.91, 12 , 13 whereas the Kuder–Richardson formula scores range from 0.80 to 0.83. 14 , 15 In the current study, the TC‐PZ‐PUKT has 0.858 Cronbach's alpha for internal consistency reliability and with test–retest reliability in total score, prevention, staging and wound care domains (r = 0.849, 0.768, 0.662 and 0.793, respectively; all p < 0.001).
This study assessed nurses' knowledge on pressure injury, revealing an overall mean correct rate of 72.5%, which is higher than that reported in previous studies. 11 , 16 In this study, 47.6% and 49.7% of participants had listened to a lecture or read an article, a book or guidelines on pressure injury in the past year; moreover, 70.3% of the participants had sought information online regarding pressure injuries in the past year. In the result of regression also showed that the learning behaviour ‘Read an article, a book or guidelines on pressure injury within the past year’ is significantly related to the score of TC‐PZ‐PUKT. In this study, 15.5% of the participants had a PhD education level, and 34.15% had more than 20 years' nursing working experience, which may cause the higher TC‐PZ‐PUKT score than other reference.
For the domains of TC‐PZ‐PUKT, the nurses tended to have higher scores in the prevention domain and lower scores in the wound care domain. Studies have indicated that nurses with more knowledge on pressure injury are more likely to engage in effective prevention behaviours, which highlights the importance of providing accurate knowledge in changing nurses' behaviours. 8 , 17 Furthermore, nurses with higher education levels and specialized wound care training tend to have substantially higher scores of pressure injury knowledge. 18 , 19 , 20 Therefore, some studies have suggested that hospitals offer pressure injury prevention education programs or require nurses to participate in relevant training to improve their knowledge as a means of encouraging better pressure injury prevention practices. 21 , 22 , 23
The PZ‐PUKT can be completed in 20–30 min and can be easily completed when clear instructions are provided. 1 To prevent fatigue among participants as they answer the 72 questions, a system should be used that automatically saves their progress on the questionnaire; this would enable them to rest and then resume the questionnaire and thereby reduce the risk of skewed results. Moreover, limitations showed that the study's findings may not be generalizable to all nursing populations since the sample was limited to clinical nurses and nursing practitioners in a specific region. The cultural and educational background of nurses in other regions might influence the results differently. Otherwise, the data on learning behaviours related to pressure injury knowledge were self‐reported by the participants, which may introduce bias. Participants might overestimate or underestimate their engagement in self‐learning activities, affecting the accuracy of the findings.
For the clinical implication, the findings demonstrate that the Traditional Chinese version of the PZ‐PUKT is a reliable and valid tool for assessing nurses' knowledge on pressure injuries. The results indicate strong internal consistency (Cronbach's alpha = 0.858) and satisfactory test–retest reliability. The study highlights the importance of higher education levels, certification as wound specialists and self‐learning in improving pressure injury knowledge. Implementing the TC‐PZ‐PUKT in clinical practice can enhance targeted educational programs, thereby improving nurses' competencies in pressure injury prevention and management, ultimately leading to better patient outcomes.
5. CONCLUSIONS
This study translated the PZ‐PUKT into Traditional Chinese and analysed its internal consistency. The findings of content validity, concurrent validity, internal consistency and test–retest reliability analyses were satisfactory. We further assessed the scores on the TC‐PZ‐PUKT across three domains with a focus on the influence of having wound care or additional nursing qualifications. The TC‐PZ‐PUKT can be administered in countries that use Traditional Chinese to facilitate further research on healthcare professionals' knowledge on pressure injury and to develop educational programs.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENTS
The authors wish to thank all participants for their time.
Chao W‐Y, Hsu M‐Y, Chen S‐R, et al. Traditional Chinese‐version reliability test of the Pieper‐Zulkowski pressure ulcer knowledge: Psychometric and assessment. Int Wound J. 2024;21(8):e70017. doi: 10.1111/iwj.70017
DATA AVAILABILITY STATEMENT
Data sharing not applicable—no new data generated.
REFERENCES
- 1. Pieper B, Zulkowski K. The Pieper‐Zulkowski pressure ulcer knowledge test. Adv Skin Wound Care. 2014;27(9):413‐420. [DOI] [PubMed] [Google Scholar]
- 2. Brislin RW. The wording and translation of research instruments. In: Lonner WJ, Berry JW, eds. Field methods in cross‐cultural research. Sage Publications, Inc; 1986:137‐164. [Google Scholar]
- 3. Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. Oxford University Press; 2015. [Google Scholar]
- 4. Schuster C, Measurement P. A note on the interpretation of weighted Kappa and its relations to other rater agreement statistics for metric scales. Educ Psychol Meas. 2004;64(2):243‐253. [Google Scholar]
- 5. Moharramzadeh H, Heidarzadeh M, Aghamohammadi‐Kalkhoran M. Investigating the psychometric properties of the Pieper‐Zulkowski pressure ulcer knowledge test among nurses in Iran. Adv Skin Wound Care. 2021;34(3):1‐6. [DOI] [PubMed] [Google Scholar]
- 6. Kim G, Park M, Kim K. The effect of pressure injury training for nurses: a systematic review and meta‐analysis. Adv Skin Wound Care. 2020;33(3):1‐11. [DOI] [PubMed] [Google Scholar]
- 7. Alshahrani B, Middleton R, Rolls K, Sim J. Critical care nurses' knowledge and attitudes toward pressure injury prevention: a pre and post intervention study. Intensive Crit Care Nurs. 2023;79:103528. [DOI] [PubMed] [Google Scholar]
- 8. Kielo E, Suhonen R, Ylönen M, Viljamaa J, Wahlroos N, Stolt M. A systematic and psychometric review of tests measuring nurses' wound care knowledge. Int Wound J. 2020;17(5):1209‐1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fernández‐Araque A, Martinez‐Delgado M, Jiménez J‐M, López M, Castro MJ, Gila EC. Assessment of nurses' level of knowledge of the management of chronic wounds. Nurse Educ Today. 2024;134:106084. [DOI] [PubMed] [Google Scholar]
- 10. Miller DM, Neelon L, Kish‐Smith K, Whitney L, Burant CJ. Pressure injury knowledge in critical care nurses. J Wound Ostomy Cont Nurs. 2017;44(5):455‐457. [DOI] [PubMed] [Google Scholar]
- 11. Nie W, Tang J, Zulkowski K, Wang L, Zan T. Psychometric properties of the Chinese version of the Pieper‐Zulkowski pressure ulcer knowledge test in nursing practice: a cross‐sectional survey. Adv Skin Wound Care. 2020;33(5):1‐7. [DOI] [PubMed] [Google Scholar]
- 12. Pieper B, Mattern J. Critical care nurses' knowledge of pressure ulcer prevention, staging and description. Ostomy Wound Manag. 1997;43(2):22‐26, 28, 30. [PubMed] [Google Scholar]
- 13. Pieper B, Mott M. Nurses' knowledge of pressure ulcer prevention, staging, and description. Adv Wound Care. 1995;8(3):34, 38, 40 passim. [PubMed] [Google Scholar]
- 14. Charalambous C, Koulouri A, Roupa Z, Vasilopoulos A, Kyriakou M, Vasiliou M. Knowledge and attitudes of nurses in a major public hospital in cyprus towards pressure ulcer prevention. J Tissue Viability. 2019;28(1):40‐45. [DOI] [PubMed] [Google Scholar]
- 15. Tulek Z, Polat C, Ozkan I, Theofanidis D, Togrol RE. Validity and reliability of the Turkish version of the pressure ulcer prevention knowledge assessment instrument. J Tissue Viability. 2016;25(4):201‐208. [DOI] [PubMed] [Google Scholar]
- 16. Tomova‐Simitchieva T, Akdeniz M, Blume‐Peytavi U, Lahmann N, Kottner JJG. The epidemiology of pressure ulcer in germany: systematic review. Gesundheitswesen. 2018;81(6):505‐512. [DOI] [PubMed] [Google Scholar]
- 17. Thomas DC, Nain RA. Dataset on nurses' knowledge, attitude and practice in pressure injury prevention at Sabah, Malaysia. Data Brief. 2023;48:109193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. De Meyer D, Verhaeghe S, Van Hecke A, Beeckman D. Knowledge of nurses and nursing assistants about pressure ulcer prevention: a survey in 16 Belgian hospitals using the PUKAT 2.0 tool. J Tissue Viability. 2019;28(2):59‐69. [DOI] [PubMed] [Google Scholar]
- 19. Grešš Halász B, Bérešová A, Tkáčová Ľ, Magurová D, Lizáková Ľ. Nurses' knowledge and attitudes towards prevention of pressure ulcers. Int J Environ Res Public Health. 2021;18(4):1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Khojastehfar S, Ghezeljeh TN, Haghani S. Factors related to knowledge, attitude, and practice of nurses in intensive care unit in the area of pressure ulcer prevention: a multicenter study. J Tissue Viability. 2020;29(2):76‐81. [DOI] [PubMed] [Google Scholar]
- 21. Ebi WE, Hirko GF, Mijena DA. Nurses' knowledge to pressure ulcer prevention in public hospitals in Wollega: a cross‐sectional study design. BMC Nurs. 2019;18(1):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saleh MY, Papanikolaou P, Nassar OS, Shahin A, Anthony D. Nurses' knowledge and practice of pressure ulcer prevention and treatment: an observational study. J Tissue Viability. 2019;28(4):210‐217. [DOI] [PubMed] [Google Scholar]
- 23. Ünver S, Fındık ÜY, Özkan ZK, Sürücü ÇJ. Attitudes of surgical nurses towards pressure ulcer prevention. J Tissue Viability. 2017;26(4):277‐281. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable—no new data generated.


