Abstract
Purpose
Little is known about cognitive complaints (self-reported problems in cognitive functioning) in patients with Obstructive Sleep Apnea (OSA). We compared the prevalence and severity of cognitive complaints in patients with untreated OSA to patients with neurological and respiratory diseases. We also studied risk factors for cognitive complaints across these diseases, including OSA.
Methods
We used a convenience sample to compare untreated OSA patients (N = 86) to patients with stroke (N = 166), primary brain tumor (N = 197) and chronic obstructive pulmonary disease (COPD, N = 204) on cognitive complaints (Cognitive Failure Questionnaire, CFQ), anxiety and depression (Hospital Anxiety and Depression Scale, HADS) and cognitive impairments using neuropsychological tests. We combined all patient groups (OSA, stroke, brain tumor and COPD) and studied potential risk factors (demographic variables, anxiety, depression and cognitive impairments) for cognitive complaints across all patient groups using regression analysis.
Results
The prevalence of cognitive complaints was higher in OSA patients and complaints of forgetfulness and distractibility were more severe compared to stroke and primary brain tumor patients, but similar to or lower than COPD patients. Regression analysis for the combined sample of all patient groups showed that cognitive complaints were most strongly associated with symptoms of anxiety and depression.
Conclusion
A high rate of OSA reported clinically significant cognitive complaints, comparable to other respiratory and neurological patients. Symptoms of anxiety and depression are important risk factors for cognitive complaints in patients with various neurological and respiratory diseases. Future studies should examine the relation between anxiety, depression and cognitive complaints in patients with OSA.
Keywords: Brain tumor, Cognitive complaints, Cognitive functioning, Cognitive impairments, Obstructive sleep apnea, Pulmonary diseases, Stroke
Introduction
Obstructive Sleep Apnea (OSA) is a sleep disorder characterized by intermittent obstruction of the airway during sleep. OSA is associated with cognitive impairments as verified with neuropsychological testing [1]. Causes for cognitive impairments in OSA are multifactorial and include disruption of sleep and nighttime blood gas abnormalities (hypoxemia). More recent studies show that fragmented sleep and hypoxemia may be insufficient to cause cognitive impairments [2–4]. These studies show that comorbid conditions, such as overweight, hypertension, stroke, diabetes and emotional problems may worsen or even be the primary cause of cognitive impairments [5, 6]. Impairments in cognition in OSA might therefor be similar to or have overlap with those other medical diseases [5]. OSA is often treated with continuous positive airway pressure (CPAP). While CPAP improves cognition, residual cognitive impairments may persist post-treatment [6, 7].
Fundamentally different from objectively tested cognitive impairments are cognitive complaints. These are subjective self-reported problems in cognitive functioning (with or without objective cognitive impairment). Cognitive complaints are concerns patients express about their daily life cognitive functioning and are an important reason patients seek medical help for their cognition. They can be assessed relatively easily through an interview or by validated questionnaires. Evaluating cognitive complaints alongside objective cognitive impairments is crucial, as they correlate to overall well-being [8], other self-reported outcomes [9, 10], and absence from work due to sickness [11].
Cognitive complaints are common in patients with neurological diseases, such as stroke [12], and brain tumors [10], and respiratory diseases, such as chronic obstructive pulmonary disease (COPD) [13]. The limited studies in untreated OSA indicate more severe concentration problems compared to healthy controls [14]. To our best knowledge, no study has compared the prevalence and severity of cognitive complaints in patients with untreated OSA to other patients with neurological or respiratory diseases.
Associated with cognitive complaints include/are symptoms of anxiety and depression [15], objective cognitive impairments [9], and a chronic (versus acute) phase of the disorder [16]. Here, the acute phase typically refers to the early onset of symptoms (days to weeks) whereas the chronic phase refers to the months or years in which symptoms remain relatively stable. Given the chronic nature of OSA, and that it is often accompanied by depression, anxiety symptoms [17], and objective cognitive impairments [18], it is expected that cognitive complaints in OSA may be as prevalent and severe as those in patients with other diseases.
To test this hypothesis, we performed a retrospective study using available datasets on cognitive complaints in patients with OSA, stroke, primary brain tumors and COPD. We are aware that some of these medical diseases share comorbidities, such as hypertension or even OSA. However, our purpose is not to determine the unique contribution of OSA on cognitive complaints in various diseases but to compare cognitive complaints between untreated OSA patients and patients with other neurological and respiratory diseases, regardless of underlying pathophysiological causes of cognitive complaints or shared comorbidities. Additionally, we studied potential risk factors (sociodemographic characteristics, anxiety and depression symptoms and cognitive impairments) for cognitive complaints across all four patient groups.
Methods
Participants
OSA patients were recruited from the sleep units of two general hospitals in the Netherlands (VieCuri Medical Center, Venlo; and Reinier de Graaf Hospital, Delft). OSA diagnosis followed the clinical guidelines of the adult OSA taskforce of the American Academy of Sleep Medicine: apnea/hypopnea-index (AHI) of ≥ 15 or AHI of ≥ 5 according to a polysomnography (PSG) with significant daytime symptoms [19]. Patients were assessed before they started treatment.
We compared OSA patients (N = 86) to three separate medical diseases (these three groups were previously recruited for other studies). These were patients three months after a stroke without major communication difficulties (N = 166) [20] and patients three months after surgery for a primary brain tumor: low grade glioma (N = 85) [21], or meningioma (N = 112) [9]. All neurological patients were recruited at the general hospital where they received their treatment. Our third group comprised patients suffering from COPD (N = 204) [22]. They were recruited at a tertiary center for pulmonary rehabilitation. The majority of these patients had severe to very severe airway obstruction global initiative for chronic obstructive lung disease stage of III–IV based on pulmonary function parameter [23]. Exclusion criteria for OSA, stroke, COPD and brain tumor patients were a history of a psychiatric or (other) neurological disorder and the use of medication/substances impacting cognition. All studies were conducted in accordance with the declaration of Helsinki and approved by nationally certified medical ethical committees (OSA: NL37795.068.11; stroke: NL21642.008.08; low grade glioma + meningioma: NL41351.008.12; COPD: NL33713.008.10).
Measures
Sociodemographic characteristics
Data on age, sex and educational level were collected for all patient groups. Educational level was rated according to the Dutch Verhage system: a 7-point scale similar to the International Standard Classification of Education [24], but adapted to the Dutch educational system.
Cognitive complaints
Cognitive complaints were assessed using the Cognitive Failure Questionnaire (CFQ) [25]. The CFQ is a validated and reliable instrument that assesses the severity of everyday cognitive complaints in the last three months and consists of 25 items. Every item is rated on a 5-point Likert-scale (ranging from “never” to “very often”). Higher scores indicate a higher severity of everyday cognitive complaints. Scores were classified as clinically significant if they were one standard deviation above the mean for a healthy Dutch norm sample (> 68) [26].
Rast and colleagues found a stable factor structure of the CFQ across different ages in a Dutch population consisting of three subscales: “forgetfulness” (sum of 8 items, score range 0–32), “distractibility” (sum of 8 items, score range 0–32) and “false-triggering” (sum of 8 items, score range 0–32) [27]. The subscale forgetfulness contains items related to memory slips. The subscale distractibility contains items related to attentional misses, such as absentmindedness. The subscale false-triggering contains items related to blunders or slips in thinking or motor actions. If one item was missing on any of the CFQ subscales it was replaced by the average score of the same subscale. If more than one item was missing on any of the CFQ subscales that subscale was labeled as missing (see Fig. 1).
Fig. 1.
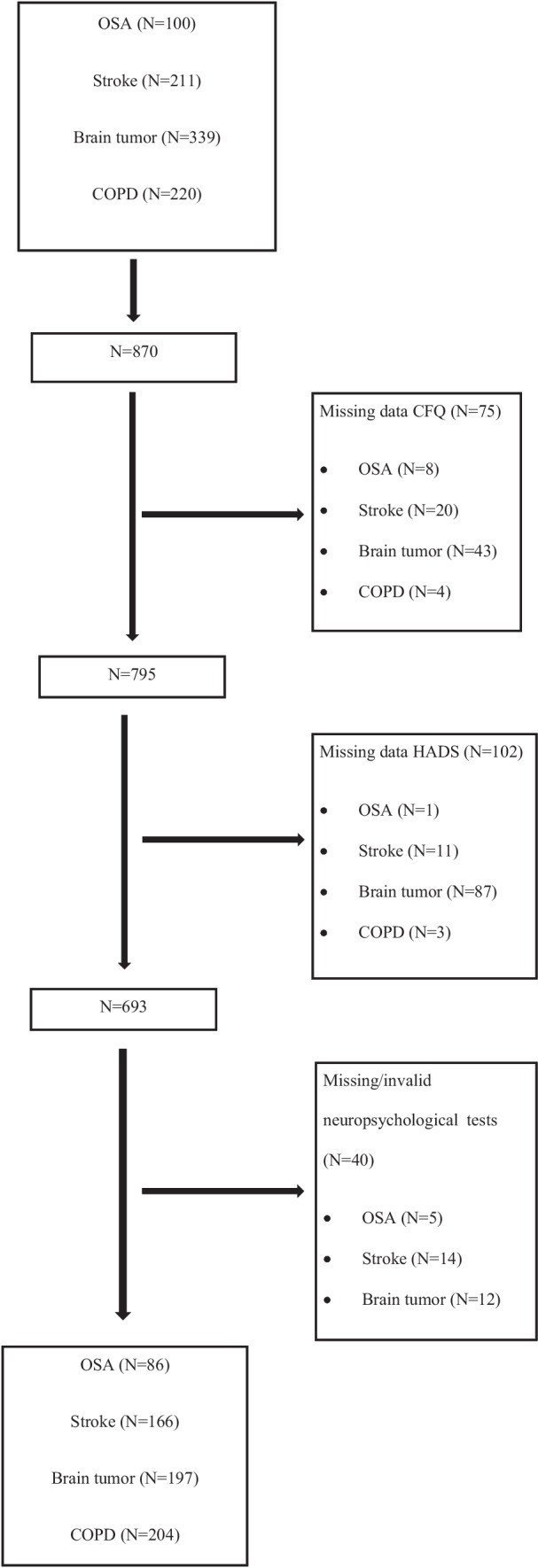
Flow chart of inclusion
Depression and anxiety symptoms
Depression and anxiety symptoms were measured using the depression (sum of 7 items, score range 0–21) and anxiety subscales (sum of 7 items, score range 0–21) of the Hospital Anxiety and Depression Scale (HADS), a reliable and validated questionnaire for mood problems in a medical setting [28]. If one item was missing on any of the HADS subscales the average score of the subscale replaced it. If more than one item was missing on any of the two subscales, the subscale was labeled as missing (see Fig. 1). A score of 8 or higher on either of the subscales indicates clinical symptoms of depression or anxiety.
Cognitive impairments
Neuropsychological tests were used to assess cognitive performance. We defined cognitive impairments using the Cognitive Impairment Non-Dementia (CIND) criteria [29]. These criteria were selected because previous studies have shown CIND criteria to be useful in defining cognitive impairments in various medical diseases [30]. According to these criteria, a cognitive domain is impaired if the norm-corrected Z-score is below -1.65 after adjusting for age, sex and educational level (the lowest 5% of the normal population). For brain tumor patients, scores were also corrected for practice effects [31], as this group had already taken the same tests three months prior. See Table 1 for all cognitive tests and scores per domain used for the different patient groups.
Table 1.
Cognitive tests and scores used per cognitive domain for all patientgroups
| Cognitive domain | Test | Scores used* | Patientgroup |
|---|---|---|---|
| Verbal memory | RAVLT-DR [49] | Total number of correct responses on delayed recall | OSA |
| WMS-PA-DR [35] | Total number of correct responses on delayed recall | Stroke | |
| CNSVS-VM [50] | Total number of correct responses on delayed recall | Brain tumor, COPD | |
| Cognitive flexibility | CNSVS-CF [50] | Total number of correct responses and errors on the Shifting Attention Test and the number of commission errors of the Stroop test | OSA, brain tumor, COPD |
| SCWT [36] | Interference score: based on the time to complete the interference part of the SCWT corrected for an estimated time based on the naming part of the SCWT test | Stroke | |
| Processing speed | CNSVS-PS [50] | Number of correct responses minus the number of errors on the Symbol Digit Coding test (an adaptation of the pen-and-paper Digit Symbol Substitution Test) | OSA, brain tumor, COPD |
| WAIS-SDST [35] | number of correctly coded symbols | Stroke |
*All scores were corrected for age, sex and educational level using available Dutch norm groups, except for WMS-PA-DR and WAIS-SDST, for these scores only age corrected norm scores were available
CNSVS-CF = Central Nervous System Vital Signs Cognitive Flexibility Domain, CNSVS-PS = Central Nervous System Vital Signs Processing Speed Domain, CNSVS-VM = Central Nervous System Vital Signs Verbal Memory Domain, RAVLT-DR = Rey Auditory Verbal Leaning Test Delayed Recall, SCWT = Stroop Color Word Test, WAIS-SD = Wechsler Adult intelligence Scale III Symbol Digit Substitution Test, WMS-PA-DR = Wechsler Memory Scale III Paired Association Delayed Recall
Verbal memory
In OSA patients, verbal memory was measured using the delayed recall score (total number of correct responses) of the Dutch version of the Rey Auditory Verbal Learning Test (RAVLT-DR) [32]. For COPD and brain tumor patients, the Verbal Memory domain score of Central Nervous System Vital Signs (CNSVS-VM) was used [33]. The CNSVS is a computerized neurocognitive test battery developed as a routine clinical screening instrument. This verbal memory test is based on an adaptation of the Rey Auditory Verbal Learning Test [34] and is recognition-based. Correct responses are summed to generate the composite Verbal Memory domain score. In stroke patients, the delayed recall score (total number of correct responses) of the Verbal Paired Association subtest of the Wechsler Memory Test (WMS-PA-DR) third edition [35] was used. For WMS-PA-DR only age- (not sex and educational level) corrected norms were available.
Cognitive flexibility
In OSA, COPD and brain tumor patients, cognitive flexibility was measured using the Cognitive Flexibility domain of Central Nervous System Vital Signs (CNSVS-CF) [31]. The score on this domain is based on the total number of correct responses and errors on the Shifting Attention Test (a measure of cognitive flexibility) and the number of commission errors of the Stroop test (a computerized version of the pen-and-paper Stroop Color Word Test, SCWT). In stroke patients, the interference score of the pen-and-paper SCWT was used as a measure for cognitive flexibility [36]. The SCWT consists of a reading, naming and interference part. The interference score was based on the time to complete the interference part corrected for an estimated time based on the naming part of the test [37].
Processing speed
In OSA, COPD and brain tumor patients processing speed was measured using the Processing Speed domain of Central Nervous System Vital Signs (CNSVS-PS) [31]. The score of this domain is based on the number of correct responses minus the number of errors on the Symbol Digit Coding test (an adaptation of the pen-and-paper Digit Symbol Substitution Test). In stroke patients, processing speed was measured using the pen-and-paper Digit Symbol Substitution Test of the Wechsler Adult Intelligence Scale (WAIS-DSST) third edition [35]. The score is based on the number of correctly coded symbols. For WAIS-DSST only age- (not sex and educational level) corrected norms were available.
Statistical analysis
Patients with untreated OSA were compared to patients with stroke, brain tumor and COPD on sociodemographic variables (age, sex and educational level), prevalence of cognitive complaints (percentage of patients with significant elevated total CFQ scores), severity of cognitive complaints (scores on CFQ subscales for forgetfulness, distractibility and false triggering), anxiety and depression symptoms (scores on HADS) and cognitive impairments (impaired scores on tests for verbal memory, cognitive flexibility and processing speed). For continuous variables we used independent samples t-tests and for categorical variables Chi-square tests.
We combined all patient groups and performed separate multiple linear regression analyses for the three CFQ subscales. As predictors we used age, sex, educational level, HADS depression, HADS anxiety and cognitive impairments. Standardized regression coefficients (β) were used to indicate the strength of the associations. We only examined component measures if the overall multivariate effect was significant. Two-sided p-values are reported and a p-value < 0.05 was considered to indicate statistical significance. P-values were adjusted using false discovery rates with the Benjamini–Hochberg method to correct for multiple testing [38]. All statistical analyses were performed using SPSS 24.0.0.0 software for Windows (IBM Corp, 2017).
Results
Participants
Figure 1 shows the inclusion flow chart for all included patient groups. We included a total of 870 patients of whom 170 had missing questionnaires cores (CFQ and/or HADS) and 40 had missing or invalid scores on the neuropsychological tests. In our analyses we were therefor able to include 86 OSA, 166 stroke, 197 brain tumor and 204 COPD patients.
Patient and sociodemographic characteristics
Table 2 shows the patient characteristics of the four patient groups. OSA severity ranged from mild to severe (AHI range 5.2—101.2) with a median of 16.2 and interquartile range of 21.5. OSA patients were significantly more often male than any of the other patients (all p’s < 0.04). OSA patients were significantly younger than stroke and COPD patients (all p’s < 0.001), but did not differ in age from brain tumor patients (p = 0.21). Furthermore, OSA patients had, on average, a significantly higher educational level than stroke (p = 0.01) and COPD patients (p < 0.001) while they did not differ on this variable from the brain tumor patients (p = 0.24).
Table 2.
Demographic variables, cognitive complaints, depression, anxiety and cognitive impairments
| Range | OSA | Stroke | p-value1 | Brain tumor | p-value1 | COPD | p-value1 | |
|---|---|---|---|---|---|---|---|---|
| N = 86 | N = 166 | N = 197 | N = 204 | |||||
| Demographics | ||||||||
| Sex (% female) | 0–100 | 21% | 34%* | .04 | 66%*** | < .001 | 52% | < .001 |
| Age | > 18 | 50.0 (10.2) | 64.1 (12.6)*** | < .001 | 52.3 (13.3) | .21 | 61.3 (8.6) | < .001 |
| Education | 1–7 | 5.3 (1.0) | 4.6 (1.4)* | .01 | 5.0 (1.2) | .24 | 4.1 (1.2) | < .001 |
| AHI | > 5 | 24.5 (19.7) | na | na | na | na | na | |
| Cognitive complaints | ||||||||
| CFQ significant cognitive complaints (%) | 0–100 | 30.2% | 17.5%* | .04 | 13.8%** | < .01 | 22.7% | .22 |
| CFQ forgetfulness | 0–32 | 13.3 (5.1) | 11.4 (5.2)* | .01 | 11.1 (5.7)** | < .01 | 13.2 (4.4) | .83 |
| CFQ distractibility | 0–32 | 11.6 (4.8) | 9.4 (5.0)** | < .01 | 8.9 (5.1)*** | < .001 | 11.8 (4.0) | .84 |
| CFQ false triggering | 0–32 | 8.3 (4.9) | 6.8 (4.4)* | .03 | 6.8 (4.6)* | .03 | 8.9 (4.1) | .34 |
| Depression and anxiety | ||||||||
| HADS depression score | 0–21 | 5.3 (3.5) | 5.2 (3.8) | .80 | 3.6 (3.1)*** | < .001 | 7.1 (3.9) | < .001 |
| HADS clinical symptoms depression(%) | 0–100 | 29.1% | 30.1% | .86 | 9.6%*** | < .001 | 44,1% | .03 |
| HADS anxiety score | 0–21 | 5.9 (3.3) | 4.7 (3.9)* | .04 | 4.6 (3.7)* | .02 | 7.3 (4.3) | .01 |
| HADS clinical symptoms anxiety (%) | 0–100 | 29.1% | 21.1% | .21 | 18.8% | .08 | 50.0% | < .01 |
| Cognitive impairments | ||||||||
| Verbal memory (%) | 0–100 | 24.0% | 8.7%* | .01 | 26.9% | .57 | 14.5% | .09 |
| Cognitive flexibility (%) | 0–100 | 30.2% | 2.4%*** | < .001 | 23.4% | .14 | 25.4% | .23 |
| Processing speed (%) | 0–100 | 8.2% | 19.3% | .06 | 17.8% | .10 | 26.4% | .01 |
AHI = Apnea/Hypopnea Index, CFQ = Cognitive Failure Questionnaire, HADS = Hospital Anxiety Depression Scale, na = not applicable,
1compared to OSA, * < .05, ** < .01, *** < .001
Cognitive complaints
In OSA 30.2% reported significant cognitive complaints (total CFQ score of more than one standard deviation above the mean of Dutch norms (see Table 2)). This percentage was significantly higher than in patients with stroke (p = 0.04) and with a brain tumor (p < 0.01), but did not differ compared to COPD patients (p = 0.22). OSA patients also reported a higher mean on the CFQ subscales for forgetfulness, distractibility and false triggering than stroke and brain tumor patients did (all p’s < 0.03, see Table 2). OSA and COPD patients did not differ in mean scores on any of the CFQ-subscales (all p’s > 0.34).
Depression and anxiety symptoms
In OSA patients, 29.1% reported clinical symptoms of depression (HADS depression) and 29.1% reported clinical symptoms of anxiety (HADS anxiety). These numbers were significantly lower compared to COPD patients for both clinical symptoms of depression and anxiety (all p’s < 0.03). OSA patients reported a higher number of clinical symptoms of depression compared to brain tumor patients (p < 0.001). For clinical symptoms of anxiety no differences were found between OSA and brain tumor patients (p = 0.08). No differences were also found between OSA and stroke for the number of patients with clinical symptoms of depression and anxiety (all p’s > 0.21).
OSA patients had a significantly higher overall score on HADS depression and anxiety than brain tumor patients (all p’s < 0.05), but a significantly lower overall score on HADS depression and anxiety than COPD patients (all p’s < 0.05). Compared to stroke patients, OSA patients scored significantly higher on HADS-anxiety (p < 0.05), but there was no difference on HADS-depression (p = 0.80).
Cognitive impairments
In OSA patients, 24% had an impairment in verbal memory, 30% in cognitive flexibility and 8% in processing speed (see Table 2). A significantly higher proportion of OSA patients had an impairment in verbal memory and cognitive flexibility (all p’s < 0.05) compared to stroke patients, but there was no significant difference for processing speed (p = 0.06). A significantly lower number of OSA patients had a cognitive impairment in processing speed compared to COPD (p < 0.05), with no significant differences for verbal memory and cognitive flexibility (all p’s > 0.09). OSA patients also did not significantly differ in the proportions of cognitive impairments on any domain compared to brain tumor patients (all p’s > 0.10).
Risk factors for cognitive complaints
For all three subscales of the CFQ we performed separate multivariate regression analyses (see Table 3). We entered age, sex, education, HADS depression score, HADS anxiety score and cognitive impairments in verbal memory, cognitive flexibility and processing speed as candidate predictors. All three models were significant (CFQ forgetfulness: F (8,651) = 13.5, p < 0.001, CFQ distractibility: F (8,651) = 19.6, p < 0.001, CFQ false triggering: F (8,651) = 14.5, p < 0.001), with R2’s of 0.14 for CFQ forgetfulness, 0.20 for CFQ distractibility and .15 for CFQ false triggering.
Table 3.
Multilinear regression analyses for all three CFQ subscales in the total sample
| CFQ forgetfulness N = 652 |
CFQ distractibility N = 652 |
CFQ false triggering N = 652 |
||||
|---|---|---|---|---|---|---|
| Variables | Standardized ß | p-value | Standardized ß | p-value | Standardized ß | p-value |
| Sex | .06 | .21 | -.09* | < .05 | .12** | .001 |
| Age | .00 | .96 | -.09* | < .05 | .00 | .96 |
| Education | .04 | .42 | -.08 | .10 | -.01 | .83 |
| HADS depression score | .25*** | < .001 | .20*** | < .001 | .18*** | < .001 |
| HADS anxiety score | .16** | .001 | .26*** | < .001 | .21*** | < .001 |
| Verbal memory impairment | .07 | .13 | .06 | .21 | .08 | .09 |
| Cognitive flexibility impairment | -.06 | .21 | -.05 | .28 | -.03 | .46 |
| Processing speed impairment | -.04 | .42 | -.09* | < .05 | -.05 | .28 |
CFQ = Cognitive Failure Questionnaire, HADS = Hospital Anxiety and Depression Scale, OSA = Obstructive Sleep Apnea,
* < .05, ** < .01, *** < .001
For our combined sample of all patient groups we found that a higher score on CFQ forgetfulness (i.e. more severe complaints of forgetfulness) was associated with a higher score on HADS depression (ß = 0.25) and a higher score on HADS anxiety (ß = 0.16).
A higher score on CFQ distractibility (i.e. more severe complaints of distractibility) was associated with a higher score on HADS depression (ß = 0.20) and HADS anxiety (ß = 0.26). A lower score on CFQ distractibility (i.e. less severe complaints of distractibility) was associated with female sex (ß = -0.09), a younger age (ß = -0.09) and an impairment in processing speed (ß = -0.09).
A higher score on CFQ false triggering (i.e. more severe complaints of false triggering) was associated with a higher score on HADS depression (ß = 0.18), a higher score on HADS anxiety (ß = 0.21) and female sex (ß = 0.12),
Discussion
To our knowledge, this is the first study comparing cognitive complaints in patients with untreated OSA to such complaints of patients with neurological or respiratory diseases. A high rate of our OSA sample reported clinically significant cognitive complaints (30.2%). Previous studies have shown that cognitive complaints are more prevalent in OSA compared to healthy controls [39, 40]. Our prevalence numbers are somewhat lower than what has been reported in previous studies (59% for memory complaints [40] and 69% for concentration complaints [41]). However, these studies used a single yes/no question to assess cognitive complaints. We do not know the percentages with similar reports of memory or concentration complaints in the healthy population. Because we used a validated questionnaire with norm-referenced cut-off scores, our prevalence numbers only include clinically significant cognitive complaints, not just any cognitive complaint also prevalent in the general population. This may explain why previous studies have found a higher prevalence of cognitive complaints in OSA.
The prevalence and severity of cognitive complaints in OSA were at least comparable to our sample of patients with other neurological and respiratory diseases. Cognitive complaints in OSA were even more prevalent and severe compared to our sample of neurological patients (stroke, brain tumor). We did not expect this last finding. There are four possible explanations for this. Firstly, patients with communication difficulties were excluded from the stroke group, likely excluding stroke patients with more severe cognitive complaints. Secondly, the datasets we used for stroke and brain tumors assessed patients three months after an acute neurological event (stroke, brain surgery). Patients at this stage of their disease may have not yet been confronted enough with cognitive failures to adequately report them [20]. Thirdly, after an acute medical event (such as stroke or brain tumor) patients may shift their evaluation of their health standards. Gratitude about their health may overshadow cognitive complaints [42]. Fourtly, we included OSA patients in the diagnostic phase at a sleep center. This sample probably has a bigger focus on and incentive to report cognitive complaints, compared to OSA patients that did not seek for help at a sleep center. Therefor the finding that OSA patients report more cognitive complaints than neurological patients need to be interpreted with caution. Current findings can only be generalized to OSA patients attending a sleep clinic and the prevalence and severity of cognitive complaints in our neurological sample might be an underestimation compared to the overall population of stroke and brain tumor patients.
For the combined sample (OSA, stroke, brain tumor and COPD together) cognitive complaints were most strongly associated with symptoms of depression and anxiety. This corresponds to results of previous cross-sectional studies in stroke [15], glioma [10], meningioma [9] and various other diseases [43]. Because our data is also cross-sectional the nature of this relation is unclear: cognitive complaints may be a sign of anxiety or depression, cognitive complaints may cause anxiety of depression or an unknown disease factor (such as fatigue or pain) may cause all three. Studies do show, however, that treating a depressive disorder reduces cognitive complaints [44]. This, together with our findings, implies that patients with cognitive complaints need to be screened for anxiety and depression. And if patients fit the criteria of a depressive disorder treatment for it will likely improve cognitive complaints.
A limitation of our study is that the medical diseases we included may share comorbidities, and there may be overlap between patient groups in the possible causes for cognitive complaints. For instance, OSA is also prevalent in stroke [45] and COPD [46] and OSA increases the risk for a primary brain tumor [47]. All included patient groups share comorbidities such as hypertension and diabetes mellitus. Unfortunately, the stroke, COPD and brain tumor patients we included were not screened for OSA. Also, data on comorbidities such as hypertension or diabetes mellitus was not available for all patient groups. However, for all patient groups we did exclude patients with psychiatric disorders, (other) neurological disorders and use of medication or substances that impact cognition. Therefore, we believe that the included patient groups are a good representation of patients in clinical practice with common comorbidities, but excluding comorbidities that have a large impact on cognition.
We were able to compare cognitive complaints in patients with untreated OSA to patients with other diseases using a well-validated questionnaire (CFQ). We also used well-established instruments to assess cognitive impairments. Almost all test scores were adjusted using age, sex and education corrected norms. This was done so we could compare across diseases, who inherently differ in age, sex and educational level. Although neuropsychological tests were often comparable across patient groups (e.g. a computerized adaptation versus a paper-and-pencil version of a test), it was not possible to use exactly the same tests (and norm scores) for all patient groups. We should therefore be careful when making comparisons between OSA and the other patient groups on cognitive impairments. This is most notable for stroke patients. For stroke patients a relatively easier and less sensitive verbal memory test was used compared to the patients with untreated OSA (WMS-PA-DR for stroke versus RAVLT-DR for OSA). WMS-PA-DR is less likely to pick up a verbal memory impairment than RAVLT-DR [48].
Conclusions
Cognitive complaints are as prevalent and severe in patients with OSA as in patients with neurological diseases (stroke, primary brain tumors) and respiratory diseases (COPD). For all patient groups combined (OSA, stroke, brain tumor and COPD) symptoms of anxiety and depression were important risk factors for cognitive complaints. Our results underscore the importance of screening for symptoms of anxiety and depression in patients who express cognitive complaints. Future studies in OSA should examine the relation between cognitive complaints, anxiety, depression and cognitive impairments to assess which OSA patients are at risk for cognitive complaints.
Acknowledgements
The authors would like to thank all the patients that participated in the study. We would like to thank the people involved in the data collection at the sleep center of VieCuri Medical Center in Venlo and Reinier de Graaf Hospital in Delft (OSA sample), Elisabeth TweeSteden hospital in Tilburg (brain tumor and stroke sample), Rehabilitation Center Leijpark in Tilburg and Maxima Medical Center in Veldhoven (for our stroke sample), Pulmonary Rehabilitation Center Schoondonck Revant in Breda (for our COPD sample). We would also like to thank the researchers involved in the original studies for their contribution to this paper: Mariëlle van Rijsbergen and Paul de Kort (stroke), Geert-Jan Rutten (LGG, Men), Sophie van der Linden (low grade glioma), Sophie Rijnen (meningioma), Dirk van Ranst and Carlijn Campman (COPD).
Abbreviations
- AHI
Apnea/Hypopnea Index
- CNSVS
Central Nervous System Vital Signs
- CNSVS-CF
Central Nervous System Vital Signs Cognitive Flexibility
- CNSVS-PS
Central Nervous System Vital Signs Processing Speed
- CNSVS-VM
Central Nervous System Vital Signs Verbal Memory
- CFQ
Cognitive Failure Questionnaire
- COPD
Chronic Obstructive Pulmonary Disease
- CPAP
Continuous Positive Airway Pressure
- ESS
Epworth Sleepiness Scale
- HADS
Hospital Anxiety Depression Scale
- OSA
Obstructive Sleep Apnea
- RAVLT-DR
Rey Auditory Verbal Learning Test Delayed Recall
- SCWT
Stroop Color Word Test
- WAIS-DSST
Wechsler Adult Intelligence Scale Digit Symbol Substitution Test
- WMS-PA-DR
Wechsler Memory Test Verbal Paired Association Delayed Recall
Authors contribution
All authors contributed to the study conception and design. Data collection and analysis were performed by Tim Vaessen. The first draft of the manuscript was written by Tim Vaessen and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, ornot-for-profit sectors.
Data availability
This study is based on the combined analysis of previously reported studies. With respect to data availability, we refer to the publications on the respective datasets. For the datasets of OSA the informed consent at the time of data collection does not allow data to be made available outside.
Declarations
All authors have seen and approved this manuscript.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Consent
All participants gave their informed consent prior to their inclusion in the study.
Competing interests
S. Overeem consulted for Jazz Pharmaceuticals, Takeda, UCB Pharma and Bioproject, all paid to institution, and none related to the present work. The other authors report no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rosenzweig I, Glasser M, Polsek D, Leschziner GD, Williams SCR, Morrell MJ (2015) Sleep apnoea and the brain: a complex relationship. Lancet Respir Med 3(5):404–414. 10.1016/S2213-2600(15)00090-9 10.1016/S2213-2600(15)00090-9 [DOI] [PubMed] [Google Scholar]
- 2.Aloia MS, Arnedt JT, Davis JD, Riggs RL, Byrd D (2004) Neuropsychological sequelae of obstructive sleep apnea-hypopnea syndrome: A critical review. J Int Neuropsychol Soc 10(5):772–785. 10.1017/S1355617704105134 10.1017/S1355617704105134 [DOI] [PubMed] [Google Scholar]
- 3.Olaithe M, Skinner TC, Hillman D, Eastwood PE, Bucks RS (2015) Cognition and nocturnal disturbance in OSA: the importance of accounting for age and premorbid intelligence. Sleep Breath 19(1):221–230. 10.1007/S11325-014-1000-2 10.1007/S11325-014-1000-2 [DOI] [PubMed] [Google Scholar]
- 4.Devita M, Montemurro S, Ramponi S et al (2017) Obstructive sleep apnea and its controversial effects on cognition. J Clin Exp Neuropsychol 39(7):659–669. 10.1080/13803395.2016.1253668 10.1080/13803395.2016.1253668 [DOI] [PubMed] [Google Scholar]
- 5.Olaithe M, Bucks RS, Hillman DR, Eastwood PR (2018) Cognitive deficits in obstructive sleep apnea: Insights from a meta-review and comparison with deficits observed in COPD, insomnia, and sleep deprivation. Sleep Med Rev 38:39–49. 10.1016/J.SMRV.2017.03.005 10.1016/J.SMRV.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 6.Vardanian M, Ravdin L (2022) Cognitive Complaints and Comorbidities in Obstructive Sleep Apnea. Sleep Med Clin 17(4):647–656. 10.1016/j.jsmc.2022.07.009 10.1016/j.jsmc.2022.07.009 [DOI] [PubMed] [Google Scholar]
- 7.Kylstra WA, Aaronson JA, Hofman WF, Schmand BA (2013) Neuropsychological functioning after CPAP treatment in obstructive sleep apnea: a meta-analysis. Sleep Med Rev 17(5):341–347. 10.1016/J.SMRV.2012.09.002 10.1016/J.SMRV.2012.09.002 [DOI] [PubMed] [Google Scholar]
- 8.Zuniga KE, Mackenzie MJ, Kramer A, Mcauley E (2016) Subjective memory impairment and well-being in community-dwelling older adults. Psychogeriatrics 16(1):20–26. 10.1111/PSYG.12112 10.1111/PSYG.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Lonkhuizen PJC, Rijnen SJM, van der Linden SD, Rutten GJM, Gehring K, Sitskoorn MM (2019) Subjective cognitive functioning in patients with a meningioma: Its course and association with objective cognitive functioning and psychological symptoms. Psychooncology 28(8):1654–1662. 10.1002/PON.5136 10.1002/PON.5136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gehring K, Taphoorn MJB, Sitskoorn MM, Aaronson NK (2015) Predictors of subjective versus objective cognitive functioning in patients with stable grades II and III glioma. Neurooncol Pract 2(1):20–31. 10.1093/NOP/NPU035 10.1093/NOP/NPU035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okonkwo O, Vance D, Antia L, et al. Service Utilization and Cognitive Complaints in Adults with HIV: Results from a Statewide Survey. 2008;7(2):175-19410.1080/15381500802006771
- 12.Van Rijsbergen MWA, Mark RE, De Kort PLM, Sitskoorn MM (2014) Subjective cognitive complaints after stroke: a systematic review. J Stroke Cerebrovasc Dis 23(3):408–420. 10.1016/J.JSTROKECEREBROVASDIS.2013.05.003 10.1016/J.JSTROKECEREBROVASDIS.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 13.Taylor CA, Bouldin ED, Greenlund KJ, Mcguire LC (2020) Comorbid Chronic Conditions Among Older Adults with Subjective Cognitive Decline, United States, 2015–2017. Innov Aging 4(1):1–10. 10.1093/GERONI/IGZ045 10.1093/GERONI/IGZ045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ulfberg J, Carter N, Talbäck M, Edling C (1996) Excessive daytime sleepiness at work and subjective work performance in the general population and among heavy snorers and patients with obstructive sleep apnea. Chest 110(3):659–663. 10.1378/CHEST.110.3.659 10.1378/CHEST.110.3.659 [DOI] [PubMed] [Google Scholar]
- 15.Nijsse B, van Heugten CM, van Mierlo ML, Post MWM, de Kort PLM, Visser-Meily JMA (2017) Psychological factors are associated with subjective cognitive complaints 2 months post-stroke. Neuropsychol Rehabil 27(1):99–115. 10.1080/09602011.2015.1065280 10.1080/09602011.2015.1065280 [DOI] [PubMed] [Google Scholar]
- 16.Tinson DJ, Lincoln NB (1987) Subjective memory impairment after stroke. Int Disabil Stud 9(1):6–9. 10.3109/02599148709166217 10.3109/02599148709166217 [DOI] [PubMed] [Google Scholar]
- 17.Bjorvatn B, Rajakulendren N, Lehmann S, Pallesen S. Increased severity of obstructive sleep apnea is associated with less anxiety and depression. J Sleep Res. 2018;27(6). 10.1111/JSR.12647 [DOI] [PubMed]
- 18.Bucks RS, Olaithe M, Rosenzweig I, Morrell MJ (2017) Reviewing the relationship between OSA and cognition: Where do we go from here? Respirology 22(7):1253–1261. 10.1111/RESP.13140 10.1111/RESP.13140 [DOI] [PubMed] [Google Scholar]
- 19.Epstein LJ, Kristo D, Strollo PJ et al (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5(3):263–276. 10.5664/jcsm.27497 10.5664/jcsm.27497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Rijsbergen MWA, Mark RE, De Kort PLM, Sitskoorn MM (2015) Prevalence and Profile of Poststroke Subjective Cognitive Complaints. J Stroke Cerebrovasc Dis 24(8):1823–1831. 10.1016/J.JSTROKECEREBROVASDIS.2015.04.017 10.1016/J.JSTROKECEREBROVASDIS.2015.04.017 [DOI] [PubMed] [Google Scholar]
- 21.Rijnen SJM, Kaya G, Gehring K et al (2019) Cognitive functioning in patients with low-grade glioma: effects of hemispheric tumor location and surgical procedure. J Neurosurg 133(6):1671–1682. 10.3171/2019.8.JNS191667 10.3171/2019.8.JNS191667 [DOI] [PubMed] [Google Scholar]
- 22.Campman C, Van Ranst D, Meijer JW, Sitskoorn M (2017) Computerized screening for cognitive impairment in patients with COPD. Int J COPD 12:3075–3083. 10.2147/COPD.S142871 10.2147/COPD.S142871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campman C, Van Ranst D, Meijer JW, Sitskoorn M (2017) Computerized screening for cognitive impairment in patients with COPD. Int J COPD 12:3075–3083. 10.2147/COPD.S142871 10.2147/COPD.S142871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United Nations Educational, Scientific and Cultural Organization. Accessed July 19, 2023. www.uis.unesco.org
- 25.Broadbent DE, Cooper PF, FitzGerald P, Parkes KR (1982) The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol 21(1):1–16. 10.1111/J.2044-8260.1982.TB01421.X 10.1111/J.2044-8260.1982.TB01421.X [DOI] [PubMed] [Google Scholar]
- 26.Elfferich MD, Nelemans PJ, Ponds RW, De Vries J, Wijnen PA, Drent M (2010) Everyday Cognitive Failure in Sarcoidosis: The Prevalence and the Effect of Anti-TNF-α Treatment. Respiration 80(3):212–219. 10.1159/000314225 10.1159/000314225 [DOI] [PubMed] [Google Scholar]
- 27.Rast P, Zimprich D, Van Boxtel M, Jolles J (2009) Factor structure and measurement invariance of the cognitive failures questionnaire across the adult life span. Assessment 16(2):145–158. 10.1177/1073191108324440 10.1177/1073191108324440 [DOI] [PubMed] [Google Scholar]
- 28.Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J Psychosom Res 52(2):69–77. 10.1016/S0022-3999(01)00296-3 10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 29.Van Den Berg E, Kessels RPC, De Haan EHF, Kappelle LJ, Biessels GJ (2005) Mild impairments in cognition in patients with type 2 diabetes mellitus: the use of the concepts MCI and CIND. J Neurol Neurosurg Psychiatry 76(10):1466–1467. 10.1136/JNNP.2005.062737 10.1136/JNNP.2005.062737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dove A, Shang Y, Xu W et al (2021) The impact of diabetes on cognitive impairment and its progression to dementia. Alzheimer’s and Dementia 17(11):1769–1778. 10.1002/alz.12482 10.1002/alz.12482 [DOI] [PubMed] [Google Scholar]
- 31.Rijnen SJM, Meskal I, Emons WHM et al (2020) Evaluation of Normative Data of a Widely Used Computerized Neuropsychological Battery: Applicability and Effects of Sociodemographic Variables in a Dutch Sample. Assessment 27(2):373–383. 10.1177/1073191117727346 10.1177/1073191117727346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Elst W, van Boxtel MPJ, van Breukelen GJP, Jolles J (2005) Rey’s verbal learning test: Normative data for 1855 healthy participants aged 24–81 years and the influence of age, sex, education, and mode of presentation. J Int Neuropsychol Soc 11(3):290–302. 10.1017/S1355617705050344 10.1017/S1355617705050344 [DOI] [PubMed] [Google Scholar]
- 33.Gualtieri CT, Johnson LG (2006) Reliability and validity of a computerized neurocognitive test battery. CNS Vital Signs Arch Clin Neuropsychol 21(7):623–643. 10.1016/J.ACN.2006.05.007 10.1016/J.ACN.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 34.Schmidt M. Rey Auditory Verbal Learning Test: A Handbook.; 1996. Accessed July 19, 2023. http://www.v-psyche.com/doc/Clinical%20Test/Rey%20Auditory%20Verbal%20Learning%20Test.docx
- 35.Tulsky D, Zhu J, Ledbetter M. WAIS-III WMS-III Technical Manual (Wechsler Adult Intelligence Scale & Wechsler Memory Scale). Published online 1997:350. Accessed July 19, 2023. http://www.amazon.com/WAIS-III-WMS-III-Technical-Wechsler-Intelligence/dp/0158981049
- 36.Lezak MD, Howieson DB, Bigler ED, Tranel D. Neuropsychological Assessment. 5th editio.; 2012.
- 37.Handboek neuropsychologische diagnostiek | Bouma, Mulder, Lindeboom, Schmand | 9789026517976 | Boom Psychologie. Accessed April 14, 2024. https://www.boompsychologie.nl/product/100-1785_Handboek-neuropsychologische-diagnostiek
- 38.Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J Roy Stat Soc: Ser B (Methodol) 57(1):289–300. 10.1111/J.2517-6161.1995.TB02031.X 10.1111/J.2517-6161.1995.TB02031.X [DOI] [Google Scholar]
- 39.Dwarakanath A, Ghosh D, Jamson S, Elliott M (2014) Evaluation of cognitive dysfunction using the cognitive failures questionnaire (CFQ), driving incidents and driving simulator (MiniUoLDS) outcome in obstructive sleep apnoea syndrome (OSAS) patients and controls. Eur Respiratory J. 44(Suppl 58).
- 40.Jennum P, Sjol A (1994) Self-assessed cognitive function in snorers and sleep apneics: An epidemiological study of 1, 504 females and males aged 30–60 years: The dan-monica ii study. Eur Neurol 34(4):204–208. 10.1159/000117039 10.1159/000117039 [DOI] [PubMed] [Google Scholar]
- 41.Ward Flemons W, Reimer MA (1998) Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am J Respir Crit Care Med 158(2):494–503. 10.1164/AJRCCM.158.2.9712036 10.1164/AJRCCM.158.2.9712036 [DOI] [PubMed] [Google Scholar]
- 42.van Gils P, van Heugten C, Sep S, Moulaert V, Hofmeijer J, Verbunt J (2022) A change of perspective? An explorative study on why patients may not subjectively report cognitive impairments after a cardiac arrest. Resuscitation 180:59–63. 10.1016/J.RESUSCITATION.2022.09.008 10.1016/J.RESUSCITATION.2022.09.008 [DOI] [PubMed] [Google Scholar]
- 43.Galioto R, Blum AS, Tremont G (2015) Subjective cognitive complaints versus objective neuropsychological performance in older adults with epilepsy. Epilepsy Behav 51:48–52. 10.1016/J.YEBEH.2015.06.035 10.1016/J.YEBEH.2015.06.035 [DOI] [PubMed] [Google Scholar]
- 44.Semkovska M, Knittle H, Leahy J, Rasmussen JR (2023) Subjective cognitive complaints and subjective cognition following electroconvulsive therapy for depression: A systematic review and meta-analysis. Aust N Z J Psychiatry 57(1):21–33. 10.1177/00048674221089231 10.1177/00048674221089231 [DOI] [PubMed] [Google Scholar]
- 45.Johnson KG, Johnson DC (2010) Frequency of Sleep Apnea in Stroke and TIA Patients: A Meta-analysis. J Clin Sleep Med 6(2):131–137. 10.5664/JCSM.27760 10.5664/JCSM.27760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shawon MSR, Perret JL, Senaratna CV, Lodge C, Hamilton GS, Dharmage SC (2017) Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: A systematic review. Sleep Med Rev 32:58–68. 10.1016/J.SMRV.2016.02.007 10.1016/J.SMRV.2016.02.007 [DOI] [PubMed] [Google Scholar]
- 47.Chen JC, Hwang JH (2014) Sleep apnea increased incidence of primary central nervous system cancers: a nationwide cohort study. Sleep Med 15(7):749–754. 10.1016/J.SLEEP.2013.11.782 10.1016/J.SLEEP.2013.11.782 [DOI] [PubMed] [Google Scholar]
- 48.Uttl B, Graf P, Richter LK (2002) Verbal Paired Associates tests limits on validity and reliability. Arch Clin Neuropsychol 17(6):567–581. 10.1016/S0887-6177(01)00135-4 10.1016/S0887-6177(01)00135-4 [DOI] [PubMed] [Google Scholar]
- 49.van der Elst W, van Boxtel MPJ, van Breukelen GJP, Jolles J (2005) Rey’s verbal learning test: normative data for 1855 healthy participants aged 24–81 years and the influence of age, sex, education, and mode of presentation. J Int Neuropsychol Soc 11(3):290–302. 10.1017/S1355617705050344 10.1017/S1355617705050344 [DOI] [PubMed] [Google Scholar]
- 50.Gualtieri CT, Johnson LG (2006) Reliability and validity of a computerized neurocognitive test battery. CNS Vital Signs Arch Clin Neuropsychol 21(7):623–643. 10.1016/J.ACN.2006.05.007 10.1016/J.ACN.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 51.Bucks RS, Olaithe M, Rosenzweig I, Morrell MJ (2017) Reviewing the relationship between OSA and cognition: Where do we go from here? Respirology 22(7):1253–1261. 10.1111/RESP.13140 10.1111/RESP.13140 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study is based on the combined analysis of previously reported studies. With respect to data availability, we refer to the publications on the respective datasets. For the datasets of OSA the informed consent at the time of data collection does not allow data to be made available outside.


