Abstract
To explore the clinical characteristics of patients infected with SARS-CoV-2 nationwide, especially the effect factors of asymptomatic infection and disappearance of clinical symptoms. A total of 66,448 COVID-19 patients in China who have been diagnosed by nucleic acid test or rapid antigen test were surveyed online (December 24, 2022 to January 16, 2023). Our cross-sectional study used descriptive analyses and binary Logistics regression model to assess the correlation between the clinical characteristics and relative factors, including age, gender, pre-existing conditions, reinfection, vaccination and treatment. A total of 64,515 valid questionnaires were collected. Among included participants, 5969 of which were asymptomatic. The symptoms were mainly upper respiratory symptoms, including dry and itchy throat (64.16%), sore throat (59.95%), hoarseness (57.90%), nasal congestion (53.39%). In binary Logistics regression model, we found that male, no pre-existing conditions, reinfection and vaccination have positive correlations with the appearance of asymptomatic COVID-19 patients. In Cox proportional-hazards regression model, considering all clinical symptoms disappeared in 14 days as outcome, we found that ≤ 60 years old, male, no pre-existing conditions, vaccination and adopted treatment have positive correlations with rapid amelioration of clinical symptoms in COVID-19 patients. The clinical symptoms of the participants were mainly upper respiratory symptoms which were according with the infection of Omicron variant. Factors including age, gender, pre-existing conditions and reinfection could influence the clinical characteristics and prognosis of COVID-19 patients. Importantly, vaccination has positive significance for the prevention and treatment of COVID-19. Lastly, the use of Chinese medicine maybe beneficial to COVID-19 patients, however, reasonable guidance is necessary.
Keywords: Clinical characteristics, Related factors, COVID-19, Cross-sectional study, Regression model
Subject terms: Risk factors, Infectious diseases, Signs and symptoms, Epidemiology
Introduction
Coronavirus disease 2019 (COVID-19), caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1, has spread widely in more than 200 countries and regions worldwide at present. As of January 31, 2023, there were 753,479,439 confirmed cases worldwide, including 6,812,798 deaths, have been reported to WHO2. COVID-19 has caused significant and far-reaching impact on the global economy, society, public health, and has become a catastrophic public health crisis worldwide. Since the outbreak of COVID-19 in China in December 2019, its high pathogenicity and high infectivity have seriously affected our daily life. Meanwhile, on November 9, 2021, the SARS-CoV-2 B.1.1.529 variant named Omicron was detected for the first time in South Africa, which has become the main circulating strain worldwide. The Omicron variant is characterized by rapid transmission, strong concealability, significant immune escape, besides, most infection were asymptomatic or mild cases3,4. Obvious study has shown that vaccine effectiveness against symptomatic disease caused by the Omicron variant is substantially lower than with the delta variant5. However, Emerging clinical data have demonstrated that vaccine protection is more preserved against severe outcomes than against infection in the Omicron era6.
SARS-CoV-2 became widespread in China from November to December, 20227, and we have made major adjustments to the prevention and control strategy since December 7, 20228. The new measures allow at-home quarantine of asymptomatic and mild cases, reduce the frequency and scale of mass testing. Since the policy adjustment, as of 24:00 on December 23, 2022, the cumulative number of reported confirmed cases has increased from 354,0179 to 393,06710. Due to the residents with suspected SARS-CoV-2 infections gradually adopted the use of RAT (rapid antigen test) for health surveillance at home and without reporting to community health departments and medical institutions, it is difficult to fully understand the clinical characteristics of SARS-CoV-2 patients at present. Therefore, we conducted this online questionnaire to record the sociodemographic characteristics, clinical symptoms, adopted prevention and treatment, prognosis and outcome of patients infected with SARS-CoV-2 in China at present, which is conducive to providing high-quality evidence for further optimization of epidemic prevention and control measures.
Methods
This study involving human participants were reviewed and approved by the Dongzhimen Hospital, Beijing University of Chinese Medicine (No. 2023DZMEC-009). Informed consent was obtained from participants before the study. All research was performed in accordance with the Declaration of Helsinki11.
Study design
We included data through professional questionnaire survey platform (www.wenjuan.com) online in China from December 24, 2022 to January 16, 2023. The participants were required positive test result of COVID-19, no matter NAT (nucleic acid test) or RAT, with or without clinical symptoms related to COVID-19. We adopted the snowball sampling method. The links or QR codes of online questionnaire were sent by researchers to their personal WeChat contacts, groups and moments for dissemination. Participants were also encouraged to forward the questionnaire links. WeChat is the most widely used social media platform in China, with more than 1 billion users. The dissemination of questionnaires through WeChat platform can effectively guarantee the spread range of questionnaires. All participants were anonymous and filled out voluntarily and information in the questionnaire that may reveal personal identity was hidden when reporting the results. Besides, all survey data was collected and managed by researchers familiar with the use, confidentiality, and data management of online questionnaires. Each questionnaire has unique ID number.
The orientation of the questionnaire and the classification of questions were discussed at the panel. Experts involved in respiratory, emergency, infection, psychology, and statistics were invited to demonstrate the rationality of the questionnaire. Before the distribution of questionnaire, we carried out a preliminary survey, finally determined and completed the online distribution of the questionnaire. The problems mainly include 4 categories: (1) Sociodemographic characteristics and general characteristics (age, sex, career, etc.). (2) Infection-related characteristics (time of contact, time of attack, time of diagnosis, method of diagnosis, symptomatic or not, symptom characteristics and duration, etc.). (3) Adopted prevention and intervention measures (situation of vaccination, situation of the use of Chinese herbal medicine, Chinese patent medicine, western drug and other non-drug therapies, etc.). (4) Final outcome (whether all clinical symptoms disappeared and their duration). All the information above were described clearly and normatively, which ensure consistent understanding and reporting. The questionnaire takes about 5–10 min to complete.
Data cleaning process
After the recruitment, we exported the data into Excel file format. Before analysis, we checked the overall quality of data, carried out data cleaning, which aimed to summarize problems such as filling errors, omissions and misfilling. If the filling time is less than 1 min, or there are major logic mistakes, doubtful authenticity that cannot confirmed from the respondents, we will eliminate all these questionnaires. As for the omissions and misfilling of part questions, if there was no serious logic error and we cannot confirm from respondents, we would eliminate the data with problems and retain the rest of the data.
Statistical analysis
Data analysis was completed by SPSS 24.0, all categorical variables were presented by absolute value and percentage. Besides, binary Logistics regression model would be used to analyze the correlation between each factor and the appearance of asymptomatic infection. We defined asymptomatic infection as laboratory-confirmed COVID-19 cases that did not exhibit any clinical symptoms, including fever, upper respiratory symptoms, pneumonia, fatigue, headache, myalgia, dehydration, or gastrointestinal dysfunction, at the time of testing, besides, those continued to exhibit no clinical symptoms during at least 7 days of follow-up after testing would also be considered as asymptomatic infection12. Meanwhile, in the symptomatic participants, whether all clinical symptoms disappeared would be taken as outcome, and the record time was 14 days. If the symptoms had not been cured at the moment of filling out questionnaire and the duration was less than 14 days, this data would be considered as censored data. Relevant factors affecting the duration of clinical symptom remission were sorted out as covariates, including age, gender, reinfection, vaccination conditions and the presence of pre-existing conditions. Cox proportional-hazards regression model would be used to analyze the correlation between each factor and the outcome, besides, we fully considered the mutual influence of each factor, and conducted adjustment analysis of each covariate. As for the self-assessed mental conditions, Mann–Whitney U test was used to evaluate the differences in mental conditions of participants in each period. All P values were from 2-sided tests and results were deemed statistically significant at p < 0.05.
Ethics approval and consent to participate
This study involving human participants were reviewed and approved by the Dongzhimen Hospital, Beijing University of Chinese Medicine (No. 2023DZMEC-009).
Results
A total of 66,448 patients with confirmed SARS-CoV-2 infection participated in the online questionnaire survey, of which 1933 (2.91%) participants were excluded after discussion due to less than 1 min to fill in questionnaire, major logical mistakes, and lack of confirmation from the respondents. Among the remaining 64,515 participants, 66 (0.10%) had unclear career information, 564 (0.87%) did not clearly fill in infection-related conditions and treatment, which were partially eliminated.
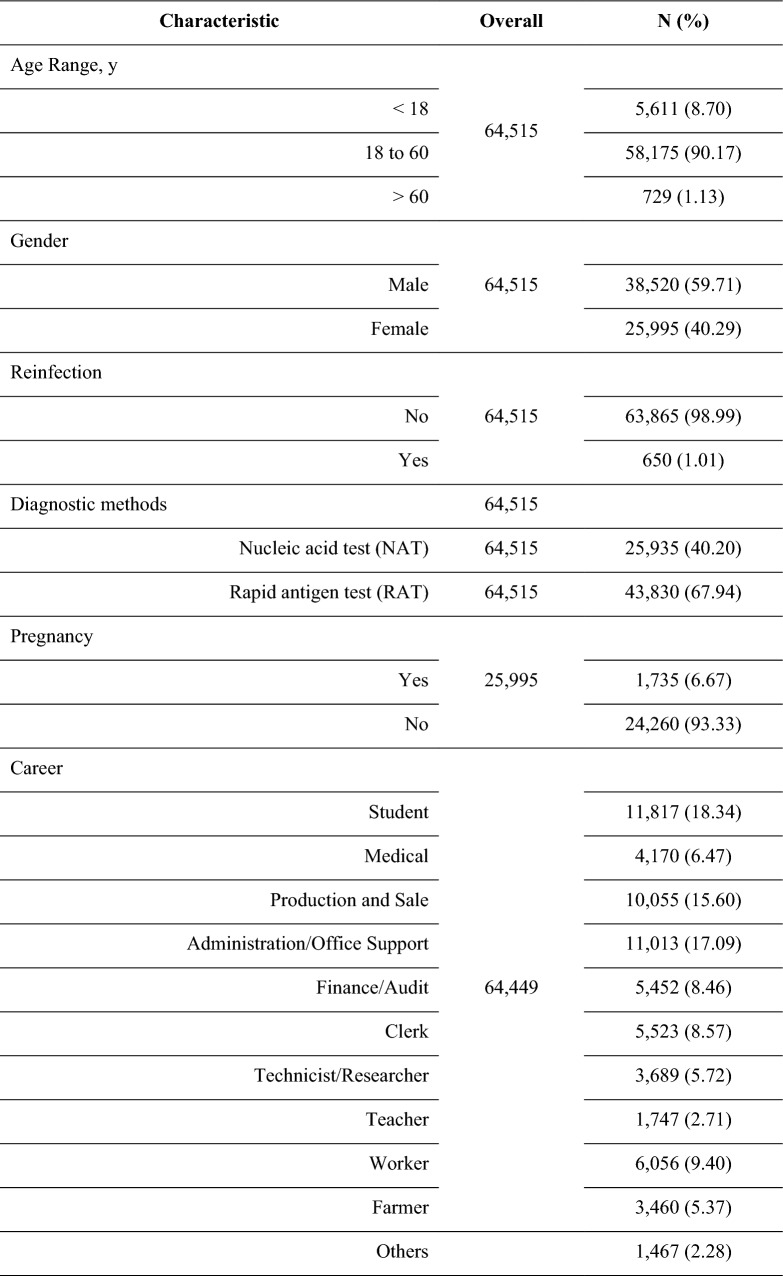
In this study, majority of participants were 18 to 60 years old (90.17%; 63,865/64,515), with slightly more male participants (59.71%; 38,520/64,515), and a small group of female participants were pregnancy during infection (6.67%; 1735/25,995). Most participants were first infected (98.89%; 47,512/64,515), and few reinfections (1.01%; 650/64,515). All participants were confirmed through RAT (67.94%; 43,830/64,515) or NAT (40.20%; 25,935/64,515). The largest group of participants were student (18.34%; 11,817/64,449). In terms of reporting pre-existing conditions, part of participants reported a history of healthy conditions (32.91%; 21,233/64,515), most of which are cardiovascular and cerebrovascular disease (16.87%; 10,884/64,515), respiratory disease (8.59%; 5542/64,515) and endocrine system disease (6.21%; 4005/64,515). In terms of prevention, majority of participants had completed three doses of COVID-19 vaccine (85.83%; 55,370/64,515). In term of the treatment, part of participants had adopted Chinese herbal medicine (37.52%; 23,994/63,951), majority of participants had adopted Chinese patent medicine (79.34%; 50.740/63,951) and western drugs (83.43%;53,353/63,951), but a small group of participants only took regular rest without intervention (9.95%; 6552/63,951). Most treatment recommendations were derived from medical orders (34.21%; 21,877/63,951), personal experience (34.15%; 21,840/63,591) and consulting health care provider (33.21%; 21,241/63,951) (Table 1).
Table 1.
Characteristics of study population.
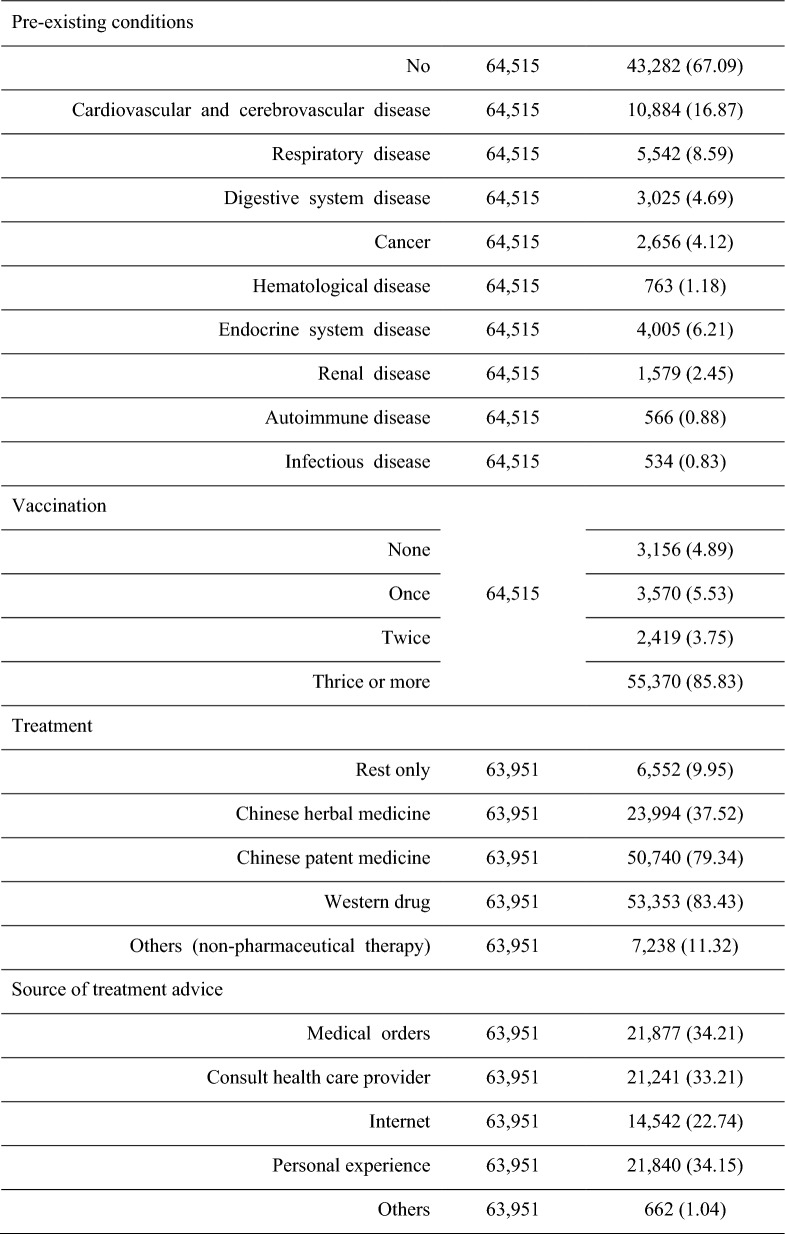
Characteristics of clinical symptom evolution
Asymptomatic infection accounted for a small proportion of the participants in this study (9.33%; 5969/63,951). The majority of participants still had clinical symptoms at the moment of filling in the questionnaire (55.99%; 35,809/63,951). Among the participants who had been cured, most of which achieved complete cured within 7 days (69.82%; 17,793/22,173), and a few patients achieved complete cured more than 14 days (1.38%; 306/22,173). There were 4 symptoms that were reported more than 50% in this study, including dry and itchy throat (64.16%; 37,203/57,982), sore throat (59.95%; 34,762/57,982), hoarseness (57.90%; 33,574/57,982), nasal obstruction (53.39%; 30,954/57,982) (Table 2). The dynamic changes of clinical symptoms recorded in this study over a period of 14 days are shown (Table 3 and Fig. 1).
Table 2.
Characteristics of conditions about the infection.
| Characteristic | Overall | N (%) |
|---|---|---|
| Duration of symptoms | ||
| No symptom | 63,951 | 5969 (9.33) |
| Not cured yet | 35,809 (55.99) | |
| 1d | 1045 (1.63) | |
| 2d | 4085 (6.39) | |
| 3d | 1709 (2.67) | |
| 4d | 1611 (2.52) | |
| 5d | 4452 (6.96) | |
| 6d | 1922 (3.01) | |
| 7d | 658 (1.03) | |
| 8d | 3850 (6.02) | |
| 9d | 414 (0.65) | |
| 10d | 385 (0.60) | |
| 11d | 1106 (1.73) | |
| 12d | 180 (0.28) | |
| 13d | 14 (0.02) | |
| 14d | 436 (0.68) | |
| > 14d | 306 (0.48) | |
| Symptoms | ||
| Dry and itchy throat | 57,982 | 37,203 (64.16) |
| Sore throat | 57,982 | 34,762 (59.95) |
| Hoarseness | 57,982 | 33,574 (57.90) |
| Nasal obstruction | 57,982 | 30,954 (53.39) |
| Runny nose (clear) | 57,982 | 27,812 (47.97) |
| Runny nose (turbid) | 57,982 | 20,694 (35.69) |
| Sneeze | 57,982 | 23,101 (39.84) |
| Dry cough | 57,982 | 24,362 (42.02) |
| Cough white sputum | 57,982 | 19,162 (33.05) |
| Cough yellow sputum | 57,982 | 17,028 (29.37) |
| Blood-stained sputum | 57,982 | 17,628 (30.40) |
| Thirst | 57,982 | 17,855 (30.79) |
| Fear of cold | 57,982 | 22,824 (39.36) |
| Fever | 57,982 | 22,501 (38.80) |
| Sweat | 57,982 | 20,193 (34.83) |
| Headache | 57,982 | 22,254 (38.38) |
| Dizziness | 57,982 | 17,031 (29.37) |
| Nausea | 57,982 | 13,645 (23.53) |
| Vomit | 57,982 | 11,645 (20.08) |
| Abdominal pain | 57,982 | 10,393 (17.92) |
| Diarrhea | 57,982 | 11,188 (19.30) |
| Dry eyes | 57,982 | 11,305 (19.50) |
| Blurred vision | 57,982 | 9,906 (17.08) |
| Hypogustia | 57,982 | 12,672 (21.86) |
| Hyposmia | 57,982 | 13,308 (22.95) |
| General fatigue | 57,982 | 17,471 (30.13) |
| Muscle soreness | 57,982 | 16,677 (28.76) |
| Sleep difficulties | 57,982 | 14,065 (24.26) |
| Anorexia | 57,982 | 13,265 (22.88) |
| Depression | 57,982 | 10,128 (17.47) |
Table 3.
Symptoms of enrolled 63,951 SARS-CoV-2 patients in 14 days.
| Symptoms | Participants, N (%) | ||||||
|---|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | |
| Dry throat and itchy throat | 21,164 (33.09) | 18,138 (28.36) | 17,073 (26.70) | 9474 (14.81) | 7315 (11.44) | 6698 (10.47) | 3562 (5.57) |
| Throat pain | 15,604 (24.40) | 17,501 (27.37) | 17,078 (26.70) | 10,158 (15.88) | 7974 (12.47) | 7280 (11.38) | 3687 (5.77) |
| Hoarseness | 11,900 (18.61) | 13,384 (20.93) | 11,726 (18.34) | 8358 (13.07) | 6926 (10.83) | 6412 (10.03) | 3586 (5.61) |
| Nasal obstruction | 11,885 (18.58) | 14,263 (22.30) | 14,577 (22.79) | 9279 (14.51) | 7886 (12.33) | 7362 (11.51) | 3855 (6.03) |
| Runny nose(clear) | 10,368 (16.21) | 12,282 (19.21) | 12,456 (19.48) | 7521 (11.76) | 6685 (10.45) | 6397 (10.00) | 3467 (5.42) |
| Runny nose(turbid) | 7608 (11.90) | 8604 (13.45) | 8586 (13.43) | 5300 (8.29) | 4925 (7.70) | 4783 (7.48) | 2472 (3.87) |
| Sneeze | 8288 (12.96) | 9902 (15.48) | 9923 (15.52) | 6018 (9.41) | 5504 (8.61) | 5293 (8.28) | 2479 (3.88) |
| Dry cough | 8120 (12.70) | 10,633 (16.63) | 10,967 (17.15) | 6856 (10.72) | 6454 (10.09) | 6316 (9.88) | 3183 (4.98) |
| Cough white sputum | 6411 (10.02) | 7793 (12.19) | 7340 (11.48) | 5028 (7.86) | 5021 (7.85) | 4834 (7.56) | 2639 (4.13) |
| Cough yellow sputum | 5521 (8.63) | 6984 (10.92) | 7134 (11.16) | 4488 (7.02) | 4258 (6.66) | 4204 (6.57) | 2075 (3.24) |
| Sputum contains blood | 5234 (8.18) | 5690 (8.90) | 5126 (8.02) | 3357 (5.25) | 3242 (5.07) | 3081 (4.82) | 1477 (2.31) |
| Thirst | 6708 (10.49) | 8395 (13.13) | 8231 (12.87) | 4595 (7.19) | 4401 (6.88) | 4286 (6.70) | 1937 (3.03) |
| Fear of cold | 8631 (13.50) | 9801 (15.33) | 7774 (12.16) | 4397 (6.88) | 3786 (5.92) | 3653 (5.71) | 1607 (2.51) |
| Fever | 9988 (15.62) | 12,770 (19.97) | 11,802 (18.45) | 4906 (7.67) | 3781 (5.91) | 3571 (5.58) | 1428 (2.23) |
| Sweat | 5890 (9.21) | 7585 (11.86) | 6353 (9.93) | 3830 (5.99) | 3437 (5.37) | 2950 (4.61) | 1406 (2.20) |
| Headache | 8689 (13.59) | 10,811 (16.91) | 10,052 (15.72) | 4787 (7.49) | 4027 (6.30) | 3457 (5.41) | 1597 (2.50) |
| Dizziness | 6914 (10.81) | 8781 (13.73) | 8565 (13.39) | 4224 (6.61) | 3749 (5.86) | 3621 (5.66) | 1599 (2.50) |
| Nausea | 5450 (8.52) | 6543 (10.23) | 6184 (9.67) | 3257 (5.09) | 2965 (4.64) | 2885 (4.51) | 1369 (2.14) |
| Vomit | 4701 (7.35) | 5157 (8.06) | 5141 (8.04) | 2725 (4.26) | 2563 (4.01) | 2469 (3.86) | 1179 (1.84) |
| Abdominal pain | 4245 (6.64) | 4440 (6.94) | 4368 (6.83) | 2583 (4.04) | 2379 (3.72) | 2293 (3.59) | 1179 (1.84) |
| Diarrhea | 4176 (6.53) | 5002 (7.82) | 4968 (7.77) | 2804 (4.38) | 2631 (4.11) | 2557 (4.00) | 1228 (1.92) |
| Dry eyes | 4717 (7.38) | 5287 (8.27) | 5162 (8.07) | 2827 (4.42) | 2638 (4.13) | 2575 (4.03) | 1327 (2.08) |
| Blurred vision | 4008 (6.27) | 4512 (7.06) | 4494 (7.03) | 2437 (3.81) | 2257 (3.53) | 2225 (3.48) | 1134 (1.77) |
| Hypogustia | 4706 (7.36) | 5763 (9.01) | 5703 (8.92) | 3581 (5.60) | 3422 (5.35) | 3356 (5.25) | 1764 (2.76) |
| Hyposmia | 4209 (6.58) | 5219 (8.16) | 5305 (8.30) | 3346 (5.23) | 3309 (5.17) | 2845 (4.45) | 1739 (2.72) |
| General fatigue | 7446 (11.64) | 9543 (14.92) | 9066 (14.18) | 4972 (7.77) | 4492 (7.02) | 4286 (6.70) | 2096 (3.28) |
| Muscle soreness | 7241 (11.32) | 9181 (14.36) | 8589 (13.43) | 4166 (6.51) | 3557 (5.56) | 3394 (5.31) | 1462 (2.29) |
| Sleep difficulties | 5204 (8.14) | 6212 (9.71) | 6143 (9.61) | 3267 (5.11) | 2884 (4.51) | 2477 (3.87) | 1389 (2.17) |
| Anorexia | 5620 (8.79) | 7158 (11.19) | 6914 (10.81) | 3688 (5.77) | 3391 (5.30) | 3256 (5.09) | 1561 (2.44) |
| Depression | 4436 (6.94) | 5346 (8.36) | 5087 (7.95) | 2698 (4.22) | 2492 (3.90) | 2381 (3.72) | 1191 (1.86) |
| Day 8 | Day 9 | Day 10 | Day 11 | Day 12 | Day 13 | Day 14 | |
|---|---|---|---|---|---|---|---|
| Dry throat and itchy throat | 2792 (4.37) | 2423 (3.79) | 1122 (1.75) | 680 (1.06) | 632 (0.99) | 366 (0.57) | 218 (0.34) |
| Throat pain | 2829 (4.42) | 2455 (3.84) | 1158 (1.81) | 678 (1.06) | 654 (1.02) | 322 (0.50) | 165 (0.26) |
| Hoarseness | 2720 (4.25) | 2437 (3.81) | 1146 (1.79) | 665 (1.04) | 639 (1.00) | 350 (0.55) | 172 (0.27) |
| Nasal obstruction | 3171 (4.96) | 2714 (4.24) | 1255 (1.96) | 758 (1.19) | 734 (1.15) | 349 (0.55) | 235 (0.37) |
| Runny nose(clear) | 2803 (4.38) | 2481 (3.88) | 1188 (1.86) | 690 (1.08) | 651 (1.02) | 352 (0.55) | 232 (0.36) |
| Runny nose(turbid) | 2223 (3.48) | 2010 (3.14) | 882 (1.38) | 571 (0.89) | 555 (0.87) | 244 (0.38) | 135 (0.21) |
| Sneeze | 2273 (3.55) | 2064 (3.23) | 857 (1.34) | 557 (0.87) | 487 (0.76) | 273 (0.43) | 160 (0.25) |
| Dry cough | 3137 (4.91) | 2694 (4.21) | 1175 (1.84) | 861 (1.35) | 806 (1.26) | 436 (0.68) | 309 (0.48) |
| Cough white sputum | 2490 (3.89) | 2202 (3.44) | 1041 (1.63) | 774 (1.21) | 669 (1.05) | 400 (0.63) | 295 (0.46) |
| Cough yellow sputum | 1999 (3.13) | 1752 (2.74) | 747 (1.17) | 536 (0.84) | 495 (0.77) | 239 (0.37) | 159 (0.25) |
| Sputum contains blood | 1513 (2.37) | 1290 (2.02) | 546 (0.85) | 363 (0.57) | 347 (0.54) | 161 (0.25) | 100 (0.16) |
| Thirst | 1845 (2.89) | 1633 (2.55) | 646 (1.01) | 473 (0.74) | 454 (0.71) | 212 (0.33) | 148 (0.23) |
| Fear of cold | 1509 (2.36) | 1345 (2.10) | 561 (0.88) | 370 (0.58) | 365 (0.57) | 167 (0.26) | 96 (0.15) |
| Fever | 1327 (2.08) | 1252 (1.96) | 468 (0.73) | 318 (0.50) | 322 (0.50) | 143 (0.22) | 79 (0.12) |
| Sweat | 1413 (2.21) | 1255 (1.96) | 513 (0.80) | 351 (0.55) | 350 (0.55) | 144 (0.23) | 82 (0.13) |
| Headache | 1552 (2.43) | 1253 (1.96) | 548 (0.86) | 342 (0.53) | 348 (0.54) | 160 (0.25) | 100 (0.16) |
| Dizziness | 1539 (2.41) | 1357 (2.12) | 551 (0.86) | 387 (0.61) | 364 (0.57) | 190 (0.30) | 116 (0.18) |
| Nausea | 1274 (1.99) | 1134 (1.77) | 482 (0.75) | 328 (0.51) | 318 (0.50) | 149 (0.23) | 89 (0.14) |
| Vomit | 1149 (1.80) | 1074 (1.68) | 413 (0.65) | 296 (0.46) | 271 (0.42) | 129 (0.20) | 54 (0.08) |
| Abdominal pain | 1116 (1.75) | 1019 (1.59) | 415 (0.65) | 271 (0.42) | 258 (0.40) | 125 (0.20) | 78 (0.12) |
| Diarrhea | 1159 (1.81) | 1065 (1.67) | 422 (0.66) | 271 (0.42) | 254 (0.40) | 126 (0.20) | 65 (0.10) |
| Dry eyes | 1170 (1.83) | 1073 (1.68) | 448 (0.70) | 290 (0.45) | 268 (0.42) | 154 (0.24) | 96 (0.15) |
| Blurred vision | 1067 (1.67) | 977 (1.53) | 427 (0.67) | 281 (0.44) | 271 (0.42) | 137 (0.21) | 93 (0.15) |
| Hypogustia | 1604 (2.51) | 1387 (2.17) | 593 (0.93) | 398 (0.62) | 376 (0.59) | 194 (0.30) | 129 (0.20) |
| Hyposmia | 1606 (2.51) | 1359 (2.13) | 608 (0.95) | 406 (0.63) | 389 (0.61) | 203 (0.32) | 136 (0.21) |
| General fatigue | 1937 (3.03) | 1647 (2.58) | 789 (1.23) | 527 (0.82) | 485 (0.76) | 290 (0.45) | 214 (0.33) |
| Muscle soreness | 1374 (2.15) | 1211 (1.89) | 489 (0.76) | 338 (0.53) | 329 (0.51) | 178 (0.28) | 111 (0.17) |
| Sleep difficulties | 1229 (1.92) | 1126 (1.76) | 486 (0.76) | 327 (0.51) | 297 (0.46) | 177 (0.28) | 104 (0.16) |
| Anorexia | 1467 (2.29) | 1259 (1.97) | 545 (0.85) | 382 (0.60) | 349 (0.55) | 188 (0.29) | 117 (0.18) |
| Depression | 1116 (1.75) | 987 (1.54) | 445 (0.70) | 296 (0.46) | 60 (0.09) | 158 (0.25) | 98 (0.15) |
Figure 1.
Symptoms of enrolled COVID-19 patients in 14 days.
Characteristics of self-assessed mental conditions in each period of infection
In this study, we initially investigated the self-assessed mental conditions of the participants in each period of infection. Before infection (64.07%; 40,973/63,951), infection confirmed (64.07%; 40,973/63,951), and after infection, (67.76%; 43,331/63,951). The number of participants who self-reported no mental disorders increased gradually, and the difference between the period of infection was statistically significant (p < 0.01) (Table 4).
Table 4.
Mental conditions (self-assessed) in each period.
| Mental disorders (Anxiety or Depression) | Overall | N (%) | p value |
|---|---|---|---|
| Before infection | 63,951 | Reference | |
| None | 39,346 (61.53) | ||
| Slight | 11,775 (18.41) | ||
| Moderate | 11,129 (17.40) | ||
| Severe | 1701 (2.66) | ||
| Infection confirmed | 63,951 | < 0.01* | |
| None | 40,973 (64.07) | ||
| Slight | 9937 (15.54) | ||
| Moderate | 10,812 (16.91) | ||
| Severe | 2229 (3.49) | ||
| After infection | 63,951 | < 0.01* | |
| None | 43,331 (67.76) | ||
| Slight | 10,099 (15.79) | ||
| Moderate | 8394 (13.13) | ||
| Severe | 2127 (3.33) |
*Mann–Whitney U test was used to evaluate the differences in mental conditions of participants in each period. Comparing with the period of before infection, the mental condition of participants during the period of infection confirmed and after infection had shown significantly changing. (p < 0.01).
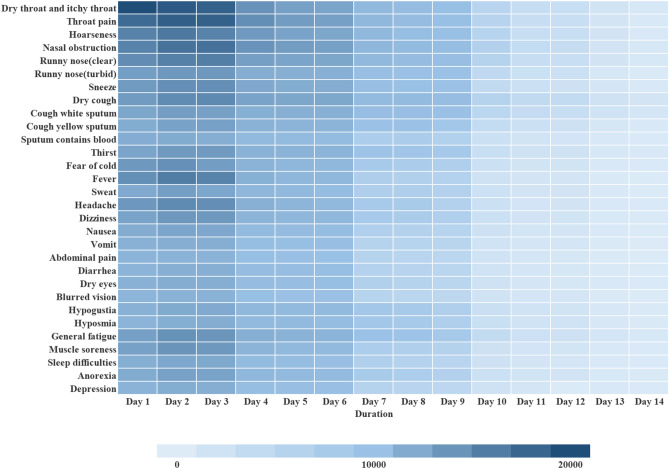
Associations between covariates and appearance of asymptomatic infection
A total of 5969 asymptomatic infections were reported. A binary Logistics regression model was used to analyze the correlation between each factor and the appearance of asymptomatic infections. Factors included age, gender, pre-existing conditions, reinfections and vaccination as covariates. We not only independently analyzed the correlation between each single factor and the appearance of asymptomatic infection, but also fully considered the mutual influence of each factor, and carried out the adjustment analysis of each covariate (Fig. 2).
Figure 2.
Correlation between covariates and appearance of asymptomatic infection*. *The correlation between all covariates and appearance of asymptomatic infection was estimated with the use of a binary Logistics regression model. The higher the hazard ratio, the greater the association between the listed characteristic and appearance of asymptomatic infection. CI denotes confidence interval.
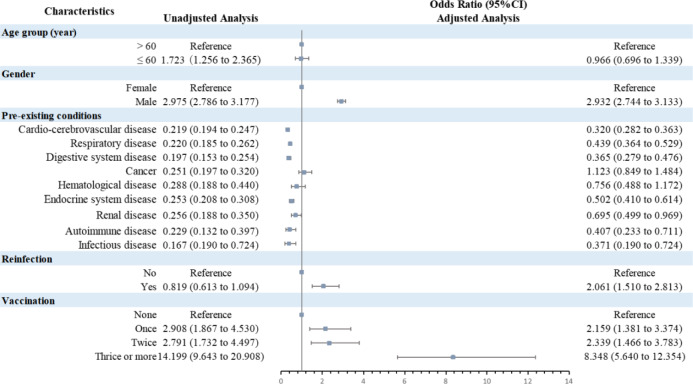
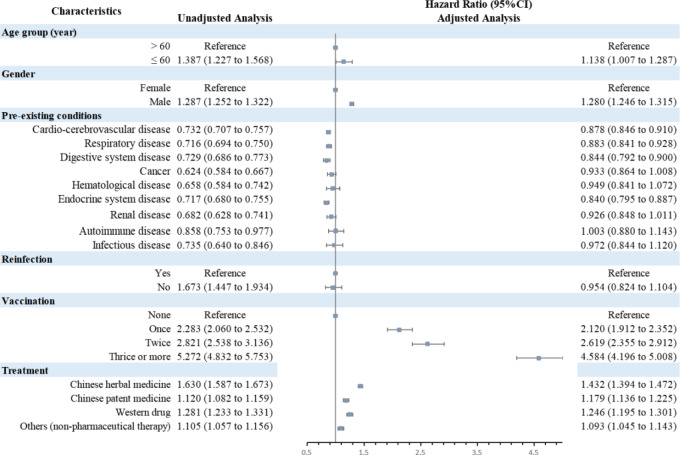
Associations between covariates and disappearance of clinical symptoms
In this study, a total of 57,982 participants reported significant clinical symptoms, and the characteristics of symptom evolution were recorded from 1 to 14 days after infection. Therefore, we defined disappearance of symptoms as the outcome and analyzed the correlation between each factor and outcome through a multivariate Cox proportional-hazards regression model. Factors included age, gender, pre-existing conditions, reinfection, vaccination and treatment as covariates. We not only independently analyzed the correlation between each single factor and the outcome, but also fully considered the mutual influence of each factor, and carried out the adjustment analysis of each covariate (Fig. 3).
Figure 3.
Correlation between covariates and disappearance of clinical symptoms*. *The correlation between all covariates and amelioration of clinical symptoms was estimated with the use of a multivariate Cox proportional-hazards regression model. The higher the hazard ratio, the greater the association between the listed characteristic and amelioration of clinical symptoms. CI denotes confidence interval.
Discussion
In this study, more than half of the participants were not cured at the time they filled out the questionnaire. The clinical symptoms mainly showed as upper respiratory symptoms, including dry and itchy throat, sore throat, hoarseness and nasal obstruction. Besides, other symptoms such as chills, fever, headache and fatigue were also common. One study found that comparing with patients who suffered from SARS-CoV-2 Delta variant, patents infected with Omicron variant were more likely to show sore throat and hoarseness, rather than hyposmia and eyes pain13. The symptoms of patients in this study are generally consistent with the common characteristics of Omicron infection reported presently. Most participants who had been cured in this study achieved amelioration in 1 week. However, we still need to pay attention to the potential risk of “long COVID”. Previous studies showed that over 30% of COVID-19 patients (including asymptomatic cases) and approximately 80% of hospitalized patients with COVID-19 may experience post-COVID symptoms14,15. What we need to focus is that most “long-COVID” symptoms would appear after cured, and these symptoms could persist for 3 months or even more16. The main symptoms of “long-COVID” are fatigue, headache, attention disorder, hair loss and breathing difficulty, which are different from that in acute infection period17–21. These characteristics provide essential reference for further observation in our follow-up study.
Considering the combined effects of numerous factors on the clinical characteristics of COVID-19 patients, we analyzed the correlations between age, gender, pre-existing conditions, reinfection, vaccination and the appearance of asymptomatic infections, besides, the improvement of clinical symptoms, which is one significant strength of this study. We found that asymptomatic infections were more likely to occur in those who were males, without pre-existing conditions, reinfected and fully vaccinated. Meanwhile, the factors including over 60 years, females, pre-existing conditions and no vaccination could impact the early recovery of COVID-19. Besides, these factors could also influence each other. In this study, over 30% of the participants reported pre-existing conditions, which is detrimental to early recovery. As independent factor, each pre-existing condition could impact the appearance of asymptomatic patients and the rapid amelioration of symptoms in COVID-19 patients. Considering interactions of other factors, patients who had suffered from cardio-cerebrovascular disease, respiratory disease, digestive system disease and endocrine system disease were still correlation with the adverse impact of clinical characteristics and prognosis. One study with a large sample of 61,414,470 individuals in England found that type 1 and type 2 diabetes were both independently associated with a significant increased odds of in-hospital death with COVID-1922. Meanwhile, COVID-19 may increase the burden of pre-existing conditions. Studies had found increasing risk of cardio-cerebrovascular disease after acute infection of COVID-19, which showed significant burden within 1 year23,24. As for reinfection, current study found that the risk of reinfection and hence hospitalization in recovered individuals remains low in 20 months, vaccination could further reduce these risks25. In this study, the reinfection group accounted for a very low proportion, and asymptomatic infection was more likely to occur than that in first infection group. Meanwhile, after interactive adjustment of various factors, we have found that there is no correlation between reinfection and rapid amelioration. Thus, this condition still needs to be alerted. As for gender, current evidence suggests that sexual dimorphism in COVID-19 has potential implications, the severity and mortality of COVID-19 is higher in males than that in females, whereas females might be at increased risk of reinfection and development of long COVID26. Combined with our study, males were more likely to occur asymptomatic infections, and females were more difficult to achieve amelioration of symptoms rapidly than males. However, whether it means more risk of “long COVID” should be confirmed in longer follow-up. As for vaccination, over 95% of the participants in this study received at least one dose vaccine of SARS-CoV-2, and over 80% of the participants completed three or more doses of vaccine. Results show clearly that vaccination is positively correlated with the appearance of asymptomatic infection and the rapid amelioration of symptoms, besides, positive effect of booster injection is also showed in this study. Sufficient evidence have shown that vaccination could significantly reduce risks of hospitalization, severity and mortality, besides, the booster vaccination could further reduce the risk of infection and the severity of COVID-1927–29. Therefore, in the following of prevention and control, vaccination is still a link that needs continuous attention.
The mental conditions of patients before and after infection are also essential in this study. The WHO has warned unequivocally that the COVID-19 pandemic is a major potential risk for a surge in mental health disorders30. An study demonstrates that the increasing problems of mental disorder during COVID-19 pandemic is closely related to the disease, growth of confirmed cases and severity of control measures31. Comparing the self-assessed mental conditions of the participants before infection, moment of confirmed and after infection, we found that the overall mental condition showed a gradual improvement trend over time. However, part of participants became severe anxiety and depression at the moment of infection confirmed, which, combined with existing research, may be related to the short-term increasing of confirmed cases and the fear that the prognosis of the disease is unknown31. Nevertheless, with the advance of time, people with severe anxiety and depression showed a downward trend again. These characteristics can not only reflect the influence of this disease in mental condition, but also serve as one potential reference to evaluate whether the adjustment of prevention and control policy is reasonable.
Lastly, majority of participants received treatment in this study, including Chinese herbal medicine, Chinese patent medicine, western drugs and other non-pharmaceutical therapy. Each treatment was independently conducive to the rapid amelioration of clinical symptoms. Considering the interaction of other factors, participants in this study could also profit through treatment. One meta-analysis found that Integrated Medicine showed better effects than western medicine independently and did not increase adverse drug reactions in the treatment of COVID-1932. What we should be focused is that in addition to medical orders, most treatment were based on “consult health care provider” and “personal experience”, which may be related to the widespread dissemination of this questionnaire in medical institutions and medical universities. However, we should still be alert to the risk of medicine abuse and repeated medication. Therapy without guidance and prescription from formal medical institution may pose more potential risks that we should pay more attention.
Limitations and strengths
Firstly, this study recruit participants through WeChat platform based on online questionnaire survey, which made it difficult for part group to participate effectively, including elderly, children, disabled. Besides, populations with severe cases, adverse events and dead population cannot participate in online questionnaire survey. Moreover, most asymptomatic patients would not conduct NAT or RAT without relative symptoms, which may lead to an underestimation of the prevalence of asymptomatic patients. Factors above could lead to the limitations of participating populations, which would influence the overall reflection of clinical characteristics. Secondly, this study lacked physicochemical indicators, besides, relied on self-reports of clinical symptoms from participants rather than assessment from clinicians, which may led to limitations in objective assessment of disease. Thirdly, the questionnaire neglected to collect the educational level and literacy of the study participants. In self-reports, this information is crucial for assessing the potential impact of participant understanding on the accuracy and completeness of the reported data. We would solve this problem through further follow-up.
Despite above limitations, we also have strengths. Firstly, this study extensively collected numerous samples of COVID-19 patients nationwide and recorded the characteristics of symptom changes of within 2 weeks in detail, which was helpful to further understand the clinical characteristics of COVID-19 presently. Secondly, we analyzed the correlation between age, gender, reinfection, pre-existing conditions, vaccination and the appearance of asymptomatic infections, besides, the amelioration of symptoms, which may help guide us to adopt more targeted prevention and control measures for corresponding populations. Lastly, we we preliminarily explored the effect of different treatment on the amelioration of symptoms in COVID-19 patients, providing a reference for the specific clinical studies of COVID-19 in the future.
Conclusion
In this cross-sectional study, the clinical symptoms of the participants were mainly upper respiratory symptoms, which are according with symptoms after infected with Omicron variant of SARS-CoV-2. Meanwhile, relevant factors including age, gender, pre-existing conditions, reinfection and vaccination could influence the clinical characteristics and rapid amelioration of symptoms in COVID-19 patients, which reminds us to further optimize the prevention and treatment measure of COVID-19. Importantly, vaccination has positive significance for the prevention and treatment of COVID-19, which is conducive to the appearance of asymptomatic patients and rapid amelioration of clinical symptoms. Therefore, strategy of vaccinating everyone should still be keep focused in the subsequent policy. Lastly, the use of Chinese medicine is beneficial to the amelioration of symptoms in COVID-19 patients, however, reasonable guidance is necessary. In summary, we need to strengthen early identification of clinical symptoms, actively promote the vaccination procedure of COVID-19 vaccine, and do a good job of prognostic follow-up.
Author contributions
Dr Kaige Zhang, Xiaoying Zhong, Xiaodan Fan, Dongdong Yu and Zhuo Chen had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Dr Kaige Zhang, Xiaoying Zhong, Xiaodan Fan, Dongdong Yu and Zhuo Chen contributed equally as co-first authors. Kaige Zhang, Xiaoying Zhong, Xiaodan Fan, Dongdong Yu, Zhuo Chen, Liangzhen You and Hongcai Shang designed this study; Kaige Zhang, Xiaoying Zhong, Xiaodan Fan, Dongdong Yu and Zhuo Chen conducted research, analyzed the data collectively; Kaige Zhang wrote the main manuscript text; Xiaoying Zhong prepared all figures; Xiaodan Fan created the online questionnaire; Liangzhen You and Hongcai Shang were in charge of supervision; All authors reviewed and approved the final version of the paper.
Funding
This work was supported by the Funds Entrusted by the State Administration of Traditional Chinese Medicine (NO.GZY-KJS-2021-055) and Young backbone personnel project by Beijing University of Chinese Medicine Dongzhimen Hospital.
Data availability
The data and materials are available in Key Laboratory of Chinese Internal Medicine of Ministry of Education, Dongzhimen Hospital, Beijing University of Chinese Medicine and could be obtained only with the approval of the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Liangzhen You, Email: youliangzh@126.com.
Hongcai Shang, Email: shanghongcai@foxmail.com.
References
- 1.Mehra, M. R., Desai, S. S., Kuy, S., Henry, T. D. & Patel, A. N. Cardiovascular disease, drug therapy, and mortality in Covid-19. N. Engl. J. Med.382(25), e102. 10.1056/NEJMoa2007621 (2020). 10.1056/NEJMoa2007621 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Coronavirus disease (COVID19) situation dashboard. Accessed January 31, 2023. https://covid19.who.int
- 3.Callaway, E. & Ledford, H. How bad is Omicron? What scientists know so far. Nature600(7888), 197–199. 10.1038/d41586-021-03614-z (2021). 10.1038/d41586-021-03614-z [DOI] [PubMed] [Google Scholar]
- 4.Pulliam, J. R. C. et al. Increased risk of SARS-CoV-2 reinfection associated with emergence of Omicron in South Africa. Science376(6593), eabn4947. 10.1126/science.abn4947 (2022). 10.1126/science.abn4947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andrews, N. et al. Covid-19 vaccine effectiveness against the Omicron (B11529) variant. N. Engl. J. Med.386(16), 1532–1546. 10.1056/NEJMoa2119451 (2022). 10.1056/NEJMoa2119451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarah, A. B. et al. Estimated effectiveness of COVID-19 vaccines against Omicron or Delta symptomatic infection and severe outcomes. JAMA Netw Open5(9), e2232760 (2022). 10.1001/jamanetworkopen.2022.32760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fang, H., Zhang, N., Hou X., et al. Investigation of traditional Chinese medicine syndromes in patients with mild symptoms of 2019-ncov infection caused by Omicron variant [J/OL]. Beijing Chinese medicine: 2023:1–5. http://kns.cnki.net/kcms/detail/11.5635.R.20230117.1437.006.html
- 8.On further optimization of disease prevention and control measures to carry out the new crown pneumonia notice (zone spreading mechanism of hair [2022] no. 113). Accessed December 07, 2022. http://www.gov.cn/xinwen/2022-12/07/content_5730443.htm
- 9.Update on the epidemic situation of novel coronavirus pneumonia as of 24:00 on December 7. Accessed December 08, 2022. http://www.nhc.gov.cn/xcs/yqtb/202212/cf3fb59d2e394ce2b89b5e18c60f5143.shtml
- 10.Update on the outbreak of novel coronavirus pneumonia as at 2pm on December 23. Accessed December 24, 2022. http://www.nhc.gov.cn/xcs/yqtb/202212/cb666dbd11864171b6586887c964791c.shtml
- 11.WMA declaration of Helsinki—Ethical principles for medical research involving human subjects. Accessed June 12, 2024. https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ [PubMed]
- 12.Sah, P. et al. Asymptomatic SARS-CoV-2 infection: A systematic review and meta-analysis. Proc. Natl. Acad. Sci. USA118(34), e2109229118 (2021). 10.1073/pnas.2109229118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez-Leon, S. et al. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep.11(1), 16144. 10.1038/s41598-021-95565-8 (2021). 10.1038/s41598-021-95565-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tenforde, M. W. et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network-United States, March–June 2020. MMWR Morb. Mortal. Wkly. Rep.69(30), 993–998. 10.15585/mmwr.mm6930e1 (2020). 10.15585/mmwr.mm6930e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang, C. et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet397(10270), 220–232. 10.1016/S0140-6736(20)32656-8 (2021). 10.1016/S0140-6736(20)32656-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: A systematic review and meta-analysis. Brain Behav. Immun.101(1), 93–135. 10.1016/j.bbi.2021.12.020 (2022). 10.1016/j.bbi.2021.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Townsend, L. et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. Plos One15, 11 (2020). 10.1371/journal.pone.0240784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peter, R. S. et al. Post-acute sequelae of covid-19 six to 12 months after infection: Population based study. BMJ379, e071050. 10.1136/bmj-2022-071050 (2022). 10.1136/bmj-2022-071050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mizrahi, B. et al. Long covid outcomes at one year after mild SARS-CoV-2 infection: Nationwide cohort study. BMJ380, e072529. 10.1136/bmj-2022-072529 (2023). 10.1136/bmj-2022-072529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Subramanian, A. et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat. Med.28(8), 1706–1714. 10.1038/s41591-022-01909-w (2022). 10.1038/s41591-022-01909-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall, V. et al. Protection against SARS-CoV-2 after Covid-19 vaccination and previous infection. N. Engl. J. Med.386(13), 1207–1220. 10.1056/NEJMoa2118691 (2022). 10.1056/NEJMoa2118691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barron, E. et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A whole-population study. Lancet Diabetes Endocrinol.8(10), 813–822. 10.1016/S2213-8587(20)30272-2 (2020). 10.1016/S2213-8587(20)30272-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xie, Y., Xu, E., Bowe, B. & Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med.28(3), 583–590. 10.1038/s41591-022-01689-3 (2022). 10.1038/s41591-022-01689-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ellul, M. A. et al. Neurological associations of COVID-19. Lancet Neurol.19(9), 767–783. 10.1016/S1474-4422(20)30221-0 (2020). 10.1016/S1474-4422(20)30221-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nordstrom, P., Ballin, M. & Nordstrom, A. Risk of SARS-CoV-2 reinfection and COVID-19 hospitalisation in individuals with natural and hybrid immunity: A retrospective, total population cohort study in Sweden. Lancet Infect, Dis.22(6), 781–790. 10.1016/S1473-3099(22)00143-8 (2022). 10.1016/S1473-3099(22)00143-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bechmann, N. et al. Sexual dimorphism in COVID-19: Potential clinical and public health implications. Lancet Diabetes Endocrinol.10(3), 221–230. 10.1016/S2213-8587(21)00346-6 (2022). 10.1016/S2213-8587(21)00346-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haas, E. J. et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: An observational study using national surveillance data. Lancet397(10287), 1819–1829. 10.1016/S0140-6736(21)00947-8 (2021). 10.1016/S0140-6736(21)00947-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vasileiou, E. et al. Interim findings from first-dose mass COVID-19 vaccination roll-out and COVID-19 hospital admissions in Scotland: A national prospective cohort study. Lancet397(10285), 1646–1657. 10.1016/S0140-6736(21)00677-2 (2021). 10.1016/S0140-6736(21)00677-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jorgensen, S. C. J. et al. Maternal mRNA covid-19 vaccination during pregnancy and delta or omicron infection or hospital admission in infants: Test negative design study. BMJ380, e074035. 10.1136/bmj-2022-074035 (2023). 10.1136/bmj-2022-074035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Organization WH. Mental health and psychosocial considerations during the COVID-19 outbreak (2020).
- 31.Salanti, G. et al. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: A systematic review and dose-response meta-analysis. Ann. Intern. Med.175(11), 1560–1571. 10.7326/M22-1507 (2022). 10.7326/M22-1507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu, M. et al. Efficacy and safety of integrated traditional Chinese and Western Medicine for Corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. Pharmacol. Res.158, 104896. 10.1016/j.phrs.2020.104896 (2020). 10.1016/j.phrs.2020.104896 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and materials are available in Key Laboratory of Chinese Internal Medicine of Ministry of Education, Dongzhimen Hospital, Beijing University of Chinese Medicine and could be obtained only with the approval of the corresponding author.