Dear Editor,
By 2040, one in three Japanese people will be at least 65 years old, and the country will become a super-aging society, which is unprecedented worldwide. Therefore, a consensus on safe dental care using local dental anesthetics must be established for older individuals with underlying diseases. As defined by the World Health Organization, adults aged ≥ 65 years are at risk for systemic diseases such as cardiovascular disease. Adrenaline, a component of local dental anesthetics, as a vasoconstrictor, may affect cardiovascular conditions [1]. Therefore, adrenaline exposure should be minimized in patients with cardiovascular diseases such as hypertension, ischemic heart disease, and obstructive hypertrophic cardiomyopathy [2]. In this commentary article, a method for diluting adrenaline in dental local anesthetics is presented, which can improve safety while maintaining efficacy.
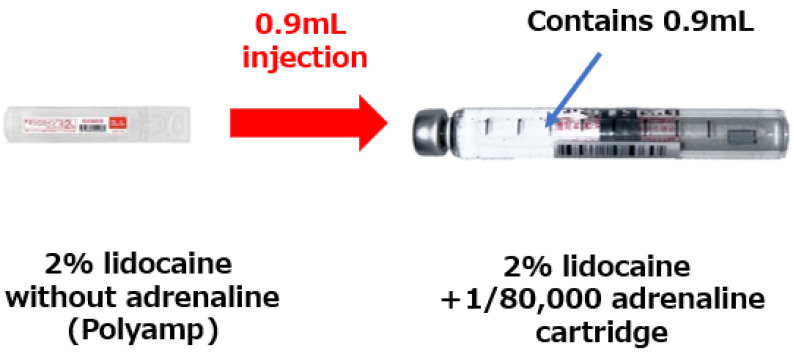
In Japan, the standard concentration of adrenaline in commercially available local dental anesthetic cartridges is 1:80,000 (1/80,000, A80). Therefore, in some cases, dentists dilute the adrenaline in local anesthetics such as lidocaine for use in patients with the aforementioned cardiovascular diseases without changing the overall amount of lidocaine (Fig. 1). In previous case reports, adrenaline was used at a concentration of 1:160,000 (A160) by dilution with half of A80 in dental surgery (tooth extractions) performed under local anesthesia in older patients or those with hypertension [3]. In such patients, circulatory changes should be avoided to the maximum possible extent. There is a separate method of administering local anesthetics with and without vasoconstrictors, but care must be taken to avoid misinjection due to mixing of the drugs and miscalculation of the dosage. Therefore, there is a method of diluting adrenaline before administration so that the number of local anesthetics used and the amount of vasoconstrictor administered can be immediately determined. This article introduces the adrenaline dilution method, which is gradually gaining popularity in Japan.
Fig. 1. Injection of 0.9 mL of 2% lidocaine without adrenaline into a 0.9 mL cartridge (2% lidocaine + 1/80,000 adrenaline).
Three combinations of local dental anesthetics and vasoconstrictors are available in Japan: lidocaine + adrenaline, propitocaine (prilocaine) + felypressin, and mepivacaine + no vasoconstrictors. Three percent propitocaine (prilocaine) with 0.03 IU/mL felypressin may be appropriate for patients who cannot tolerate tachycardia [1]. However, lidocaine + adrenaline is mainly used in most dental clinics in Japan.
The advantages of diluting adrenaline by half are not only limited to the avoidance of circulatory fluctuations. In an experimental animal model, 2% lidocaine containing 1:200,000 (A200) adrenaline achieved stable hemodynamic parameters (mean arterial pressure and heart rate) compared to 2% lidocaine with A80, while showing similar local anesthetic and hemostatic effects [2]. In a clinical study involving third molar extractions in healthy adults, the anesthetic effects of A200 and A80 were not different; however, the hemodynamic parameters after anesthesia were markedly higher with A80 [4]. Therefore, dilution of adrenaline by half can stabilize the vital signs while maintaining anesthetic and hemostatic effects, which is beneficial for dental surgery in patients with unstable hemodynamics.
In Japan, local anesthesia for dental treatment is often administered using special glass cartridges. When adrenaline is diluted twofold, it can be diluted using a disposable plastic syringe and injected directly into the patient. However, this method has certain disadvantages, such as the inability to connect to a disposable dental ultrafine needle (30–33G), poor operability during infiltration anesthesia, and the inability to aspirate during block anesthesia. Therefore, the following method is recommended. After discarding half of the cartridge (1:80,000 adrenaline + 2% lidocaine), the total adrenaline in the cartridge can be diluted by filling it with 2% lidocaine without adrenaline. At the same time, this method requires drilling at least two holes in the rubber stopper; therefore, we must be careful not to create a coring. Coring occurs when a piece of rubber is scraped off upon the insertion of a needle into a rubber stopper, and the rubber is mixed with the drug solution. This occurs with propofol and rocuronium, which are frequently used for sedation and general anesthesia, but not with dental local anesthetics [5]. Thus, a thin needle must be used, and the rubber plug should be vertically pierced when diluting the adrenaline in the cartridge.
In patients with circulatory problems, dilution with attention to the above points (e.g., coring) would further improve safety during dental procedures using local anesthetics. Investigations are underway to identify methods for dilution with half of the adrenaline, taking coring into consideration. In addition, a more straightforward dilution method is being studied for dentists in general dental clinics who do not specialize in dental anesthesia.
Footnotes
DECLARATIONS OF INTEREST: The authors declare no conflicts of interest regarding the publication of this letter.
- Takutoshi Inoue: Conceptualization, Writing – original draft, Writing – review & editing.
- Toru Yamamoto: Conceptualization, Writing – review & editing.
References
- 1.Kyosaka Y, Owatari T, Inokoshi M, Kubota K, Inoue M, Minakuchi S. Cardiovascular comparison of 2 types of local anesthesia with vasoconstrictor in older adults: a crossover study. Anesthesia Prog. 2019;66:133–144. doi: 10.2344/anpr-66-02-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karm MH, Kim M, Park FD, Seo KS, Kim HJ. Comparative evaluation of the efficacy, safety, and hemostatic effect of 2% lidocaine with various concentrations of epinephrine. J Dent Anesth Pain Med. 2018;18:143–149. doi: 10.17245/jdapm.2018.18.3.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inokoshi M, Soeda Y, Akiyama Y, Ueda K, Kubota K, Minakuchi S. Fully digital workflow for the fabrication of three-dimensionally printed surgical splints for preventing postoperative bleeding: a case report. Int J Environ Res Public Health. 2022;19:12773. doi: 10.3390/ijerph191912773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karm MH, Park FD, Kang M, Kim HJ, Kang JW, Kim S, et al. Comparison of the efficacy and safety of 2% lidocaine HCl with different epinephrine concentration for local anesthesia in participants undergoing surgical extraction of impacted mandibular third molars A multicenter, randomized, double-blind, crossover, phase IV trial. Medicine (Baltimore) 2017;96:e6753. doi: 10.1097/MD.0000000000006753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chotikawanich T, Kammee T, Khantee S. The impact of needle size and angle on rubber coring after multiple puncturing of multi-dose propofol vial rubber stoppers. Heliyon. 2022;8:e09389. doi: 10.1016/j.heliyon.2022.e09389. [DOI] [PMC free article] [PubMed] [Google Scholar]