Abstract
Introduction
Laparoscopic cholecystectomy is a commonly performed surgical procedure and there are instances where complications may occur intraoperatively which can go undiagnosed or unreported and the patient can present at a later time with the manifestations of those complications. This study presents a case series comprising three instances of “ghost complications” following laparoscopic cholecystectomy, emphasizing the utmost significance of careful follow-up care and efficient communication to promptly recognize and manage any complications arising after the surgery.
Case presentation
Three cases of ghost complications post-biliary surgery are presented. These complications were initially overlooked or dismissed due to factors such as atypical symptom presentation and inadequate follow-up. The cases involve retained stones leading to secondary complications, bile leak masked by postoperative symptoms, and post-cholecystectomy syndrome mistaken for unrelated conditions.
Clinical discussion
Diagnosing ghost complications is challenging when symptoms diverge from the expected postoperative course. Meticulous clinical suspicion and interdisciplinary collaboration are crucial for accurate diagnoses and timely intervention. Effective communication between patients and surgeons is pivotal in ensuring appropriate management.
Conclusion
This study illuminates the concept of “ghost complications” after biliary surgery, highlighting challenges in their recognition and management. Through three distinct cases, the study underscores the significance of vigilant follow-up care, early symptom recognition, and open communication to prevent and address such complications. Transparent communication and meticulous monitoring are vital for enhancing patient outcomes and mitigating the occurrence of “ghost complications.”
Keywords: Biliary tract surgical procedures, Case report, Postoperative complications
Highlights
-
•
Case series on “ghost complications” in biliary surgery post-laparoscopic cholecystectomy, revealing unnoticed complications
-
•
Three cases are presented, involving missed complications such as retained stones and bile leak
-
•
Vigilant follow-up and early symptom recognition, and interdisciplinary collaboration is crucial to detect such complication
1. Introduction
Biliary surgery, such as laparoscopic cholecystectomy, is a standard procedure with generally low complication rates [1]. However, there are instances of unnoticed or undiagnosed complications, where patients remain unaware of these issues. Ghost surgery occurs when an undisclosed surgical assistant or another surgeon performs a procedure without the patient's knowledge, even if the consenting surgeon is not directly involved [2]. This study highlights the term “ghost complications” and reports three cases of pneumobilia as a ghost complication following laparoscopic cholecystectomy.
All cases received corrective surgeries, resulting in favorable outcomes during follow-up. By raising awareness about this phenomenon, healthcare professionals can better identify and manage such complications, ensuring improved patient care and safety. This case series has been reported in line with the PROCESS criteria [3].
2. Case series
2.1. Case one
A 25-year-old female presented to the Gastrointestinal (GI) unit of the hospital with a two-year history of yellowish scleral discoloration, dark urine, and light-colored stool. Her jaundice was progressive and associated with generalized body itching which had gotten more severe in the last three months before her presentation. She did not have any history of anorexia or weight loss. The patient had undergone a laparoscopic cholecystectomy that was converted to open cholecystectomy 12 years prior. The surgery lasted for approximately 3 h and required an abdominal drain in situ for 6 days postoperatively. She was unaware of the reasons for the conversion and had not been on regular follow-up.
At our hospital, on examination, she was icteric with scratch marks all over the body and had not demonstrated any other stigmata of liver disease. Her abdominal examination revealed a scar of Kocher's incision, with no other significant findings. Blood investigation revealed Total Bilirubin (TB) 7 mg/dL, Direct Bilirubin (DB) 5 mg/dL, Aspartate Aminotransferase (AST), 267 units/L Alanine Aminotransferase (ALT) 259 units/L, and Alkaline phosphatase (ALP) 832 IU/L. Ultrasonography revealed dilated intrahepatic and extrahepatic bile duct with hepatolithiasis at the confluence of the right and left hepatic duct and Magnetic Resonance Cholangiopancreatography (MRCP) confirmed the same findings with stricture at the Hepatic Hilum (Strasberg E2) (Fig. 1).
Fig. 1.
MRCP showing stricture at the hepatic hilum (Strasberg E2).
Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis revealed similar findings to MRCP with no associated vascular injury, no atrophy and hypertrophy complex, with the presence of pneumobilia in the intrahepatic biliary tree. During exploratory laparotomy, grossly all the viscera were normal. However, there was a retrocolic Roux Limb which was anastomosed with the common hepatic duct and the anastomotic site was completely stenosed. The anastomosis site was dismantled and choledochoscopic exploration of the biliary tract was done, hepatolithiasis was removed and the same Roux limb was used for revision Hepp-Couinaud Hepaticojejunostomy. The patient showed satisfactory outcomes during the follow-up after 16 months (Fig. 2).
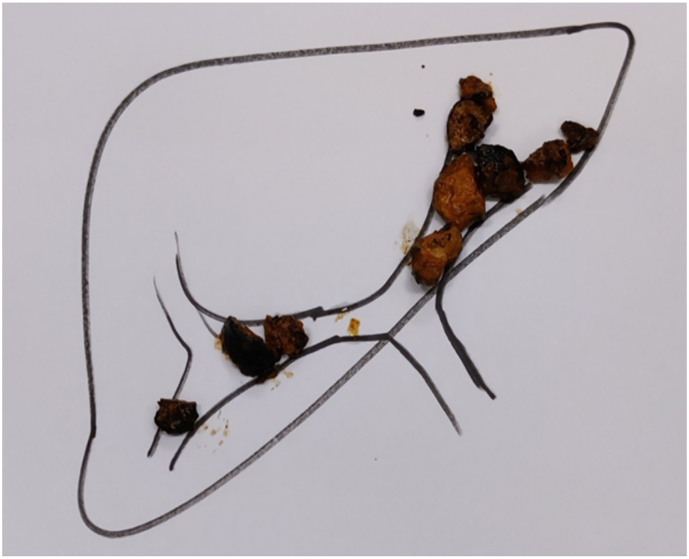
Fig. 2.
Hepatolithiasis found during the surgery.
2.2. Case two
A 51-year-old male was referred to the GI Surgical unit of the Hospital for Endoscopic Retrograde Cholangiopancreatography (ERCP) due to persistent symptoms. Three years prior, he began experiencing insidious right upper abdominal pain that was colicky and moderately severe. The pain was alleviated with mild analgesics and accompanied by intermittent vomiting containing food particles. The patient also exhibited yellowish scleral discoloration and experienced intermittent fever with chills and rigor during episodes of pain. Initially, the patient was managed for a suspected benign biliary stricture and received conservative treatment. However, despite eight hospital visits, multiple endoscopies, and repeated investigations, including MRCP, at other centers, the symptoms persisted. The patient also gave a history of a prior laparoscopy being converted to open cholecystectomy seven years ago. He was unaware of the reasons for the conversion and had not been on regular follow-up after surgery.
Upon evaluation at our center, the patient's LFTs were assessed which was suggestive of obstructive jaundice, and MRCP revealed a Strasberg E2 biliary stricture. Further imaging with CECT scans of the abdomen showed three suspicious laparoscopic clips around the common hepatic duct, along with evidence of pneumobilia, indicating the possibility of bilioenteric communications. Vascular injury and atrophy/hypertrophy complex were ruled out (Fig. 3).
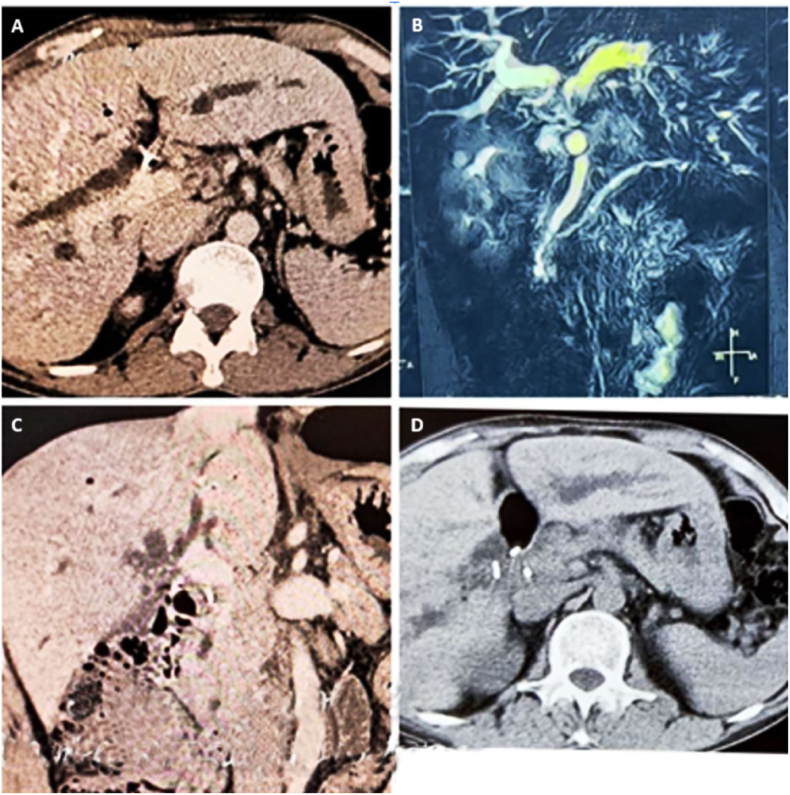
Fig. 3.
A. CECT Abdomen axial section portal venous phase showing dilated intrahepatic biliary radicles, pneumobilia, and surgical clip at hepatic hilum. B. Maximum intensity projection coronal section Magnetic Resonance Cholangiopancreatography showing dilated Intrahepatic biliary ducts with stricture at the level of Common hepatic duct. C. CECT abdomen coronal section portal venous phase showing dilated intrahepatic biliary radicals, pneumobilia, and surgical clips at common hepatic duct. D. CECT abdomen axial section delayed phase showing dilated intrahepatic biliary radicals and surgical clips with bowel loop at hepatic hilum.
The patient was then taken for laparotomy, where a retro-colic Roux limb of approximately 60 cm in length was identified. The hepaticojejunostomy site had a stricture with a diameter of approximately 5 mm, and a jejuno-jejunostomy was observed approximately 70 cm distal to the hepaticojejunostomy site (Fig. 4).
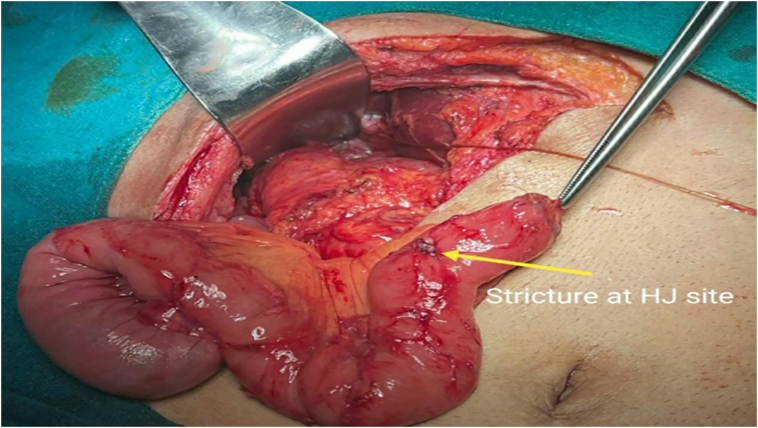
Fig. 4.
Intraoperative finding showing retrocolic Roux limb that was made during previous surgery with stricture at the HJ site.
Consequently, a redo-hepaticojejunostomy was performed using the same Roux limb. Choledocoscopic exploration of the biliary tree was conducted, sludge was removed, and a Hepp-Couinaud Hepaticojejunotomy was performed. The patient was discharged on the fifth postoperative day after the removal of the abdominal drain and has been doing well during the 14-month follow-up period.
2.3. Case three
A 37-year-old female presented to the GI Surgical Unit of the Hospital with complaints of mild epigastric pain and vague abdominal discomfort that had been alleviated with over-the-counter drugs for the past three months. The patient had no history of anorexia, weight loss, jaundice, or fever. Thirteen years prior, she had undergone an open cholecystectomy, but she was unaware of the reason for the procedure and had a normal postoperative course. During a routine ultrasound at another center, the patient was incidentally diagnosed with left-sided hepatolithiasis. Her liver function tests showed mild derangement. Further imaging with MRCP revealed a Huang Type III A biliary variant, while CECT demonstrated pneumobilia with sludge in the left hepatic duct and common hepatic duct. [4] Upper GI endoscopy revealed a suspicious choledochoduodenostomy adjacent to the papilla (Fig. 5).
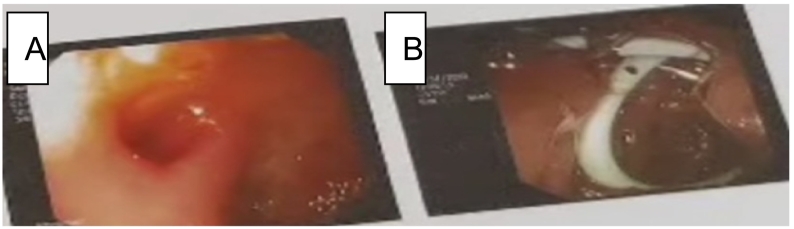
Fig. 5.
A - Image showing an endoscopic view of choledochoduodenostomy adjacent to the Ampulla of Vater that was made in previous surgery. B- Double J biliary pigtail stent after endoscopic balloon dilatation of the CHD stricture.
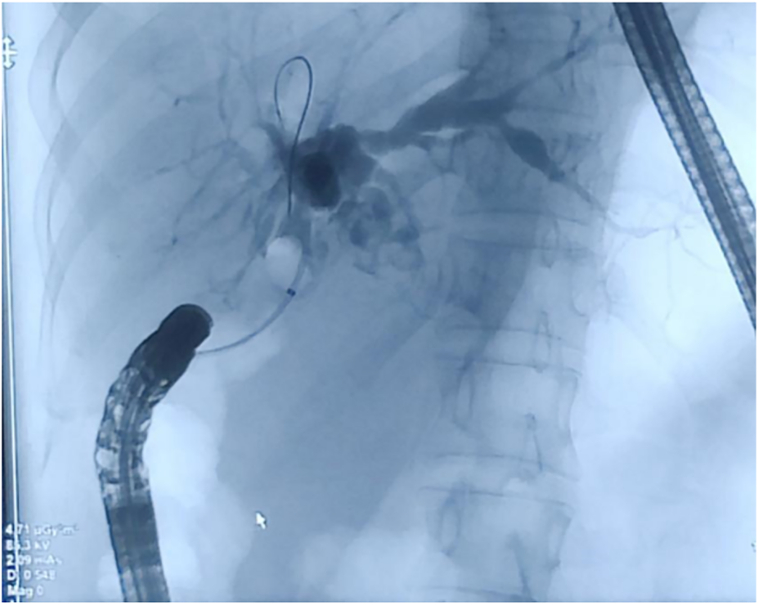
In the same session, an ERCP was performed, which showed a short Common Bile Duct (CBD) with slight narrowing at the mid-CBD level (Fig. 6).
Fig. 6.
Image of ERCP showing a very short segment of common bile duct with normal opacification of bilateral intrahepatic biliary radicles.
The narrow segment was dilated using a balloon, and sludge was extracted, clearing the common bile duct. The patient has been doing well during the nine-month follow-up period.
3. Discussion
These cases highlight the occurrence of ghost complications in biliary surgeries, where patients remain unaware of the complications until later presentations. Ghost complications can result from various factors, including incomplete documentation, inadequate follow-up care, and limited patient awareness. Communication gaps between surgeons and patients, as well as inadequate referral notes, can contribute to missed diagnoses and delayed management of these complications. All three patients in this case series were unaware of their complications and were not on regular follow-ups. The complications were only identified during subsequent surgeries. We can refer to such a phenomenon as “ghost complications,” which occur when patients experience complications from a previous surgery but remain unaware of them until they present with related consequences later on.
Laparoscopic cholecystectomy is a commonly performed surgery, and while it generally has a low complication rate, there are potential risks involved. Intraoperatively, laparoscopic surgeries might need to be converted to open cholecystectomy and this has reported rates of 1 % to 15 % [5,6]. Bile duct injury is one of the recognized complications with an incidence of 0.3 to 0.7 % [7]. Patients undergoing this surgery must be properly informed about the indications, potential complications, alternative treatment options, and the risk versus benefit analysis associated with the procedure.
Medicolegal issues and litigations are not uncommon after cholecystectomy. Patients who experience complications may face a challenging life with prolonged hospital stays, repeated visits, and additional surgeries, leading to a worsened quality of life. In a study, it was found that a significant number of patients were inadequately informed about the possibility of bile duct injury (BDI) during the surgical consent process. This lack of awareness can result in negative emotional states, such as low mood and low energy levels, repeated hospital visits, expenses, and difficulty treating as they are also unaware of the previous event during the surgery [8]. However, surgical repair has been shown to improve symptoms and provide relief for patients, decrease the cost of treatment and expenses, and prevent irreversible complications like secondary biliary cirrhosis [8].
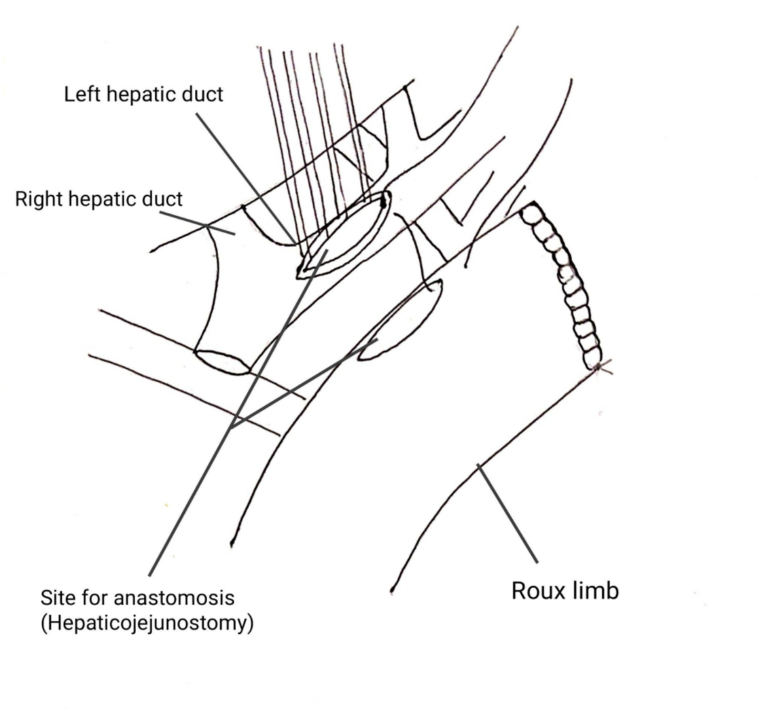
Hepp-Couinaud hepaticojejunostomy is a technique of wide, accurate, mucosa-to-mucosa end-to-side bilio-enteric anastomosis and is a common procedure done for bile duct injury and biliary stricture (Fig. 7) [10]. This procedure of biliary reconstruction can be complicated by stricture development and anastomotic leak which can negatively impact the quality of life of the patient [10]. Asymptomatic patients require follow-up every six months during the first year and annually thereafter, as complications can manifest later in life. Proper postoperative monitoring and timely management are crucial to ensure optimal patient outcomes [11].
Fig. 7.
Schematic diagram showing the Hepp-Couinaud approach.
(Adapted from Clavien P-A, Sarr MG, Fong Y, et al.: Atlas of Upper Gastrointestinal and Hepato-Pancreato-Biliary Surgery, 2nd Edition, Pg no. 707 [9].)
Surgeons involved in laparoscopic cholecystectomy may face the natural temptation to fix any complications immediately or perform early repairs to conceal the injury i.e. to ‘fix the leak then and there’. However, studies have shown that about 50 % of cases in the UK and 60–75 % in Canada and the USA involve an immediate or early repair approach [12]. When experienced hepatobiliary surgeons execute such strategies, positive outcomes are likely. Yet, if the repair is conducted by the same surgeon without sufficient expertise, the likelihood of complications and the need for reoperation increase significantly [12]. To address these issues and minimize complications, it is crucial to identify any injuries promptly and refer the patient to a specialized tertiary center with expert biliary surgeons. During the referral process, all pertinent details of the operative findings and events should be meticulously documented in the referral note or preferably conveyed via phone directly to the expert surgeon before transferring the patient.
It's essential to highlight that immediate repair performed by a non-biliary surgeon is prone to failure. The chances of success following repair by the surgeon responsible for the injury, rather than a biliary surgeon, are considerably lower—21 % compared to 95 % for a biliary surgeon [13]. In some cases, desperate attempts to identify the site of the biliary duct injury and subsequent unsuccessful repair attempts may exacerbate the injury, leading to higher ductal injury and additional vascular damage [11].
To prevent such situations, it is essential to emphasize proper training techniques for laparoscopic surgery, obtain detailed written informed consent from patients undergoing laparoscopic cholecystectomy, and consider early conversion to open surgery when necessary with careful, proper, and adequate postoperative monitoring. Effective communication and documentation play a vital role in preventing and managing ghost complications. All documents and communications related to the patient's care should be preserved for medicolegal purposes. Proper documentation of referral notes and communication between surgeons also contributes to optimal patient care and minimal complications after the surgery [14].
To minimize ghost complications, it is crucial to emphasize the importance of proper informed consent, comprehensive documentation, effective communication, and regular follow-up care. Surgeons should provide patients with detailed information about the surgery, potential complications, and available treatment options. Adequate referral notes, including complete operative findings and procedures, must be provided when referring patients to biliary centers. Additionally, maintaining meticulous documentation and preserving all communication records can be instrumental in managing any medicolegal issues that may arise.
4. Conclusions
Ghost complications can occur in biliary surgeries, often going unnoticed or undiagnosed until later presentations. It is imperative to obtain proper informed consent, ensuring that patients are fully aware of potential complications. Open and transparent communication between surgeons and patients, as well as detailed documentation, are crucial to prevent and manage ghost complications effectively. Proper documentation of referral notes and communication between surgeons also contributes to optimal patient care.
Patient consent
Written informed consent was obtained from the patients for the publication of this case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Patient anonymity is maintained throughout this manuscript, and consent was obtained for publication from the patient. Ethical approval is not required for case series.
Funding
No sources of funding.
Guarantor
Uttam Laudari, U., Laudari, Department of Surgery, Kathmandu University School of Medical Sciences, Dhulikhel, 45210, Nepal.
Research registration number
-
1.
Name of the registry: NA
-
2.
Unique identifying number or registration ID: NA
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NA.
CRediT authorship contribution statement
Uttam Laudari: Concept, manuscript preparation, edit and review.
Ashlesha Chaudhary: Manuscript preparation, edit and review.
Suzit Bhusal: Manuscript preparation, edit and review.
Baibhav Bhatta: Manuscript preparation, edit and review.
Aashutosh Chaudhary: Manuscript preparation, edit and review.
Bala Ram Malla: Manuscript preparation, edit and review.
Declaration of competing interest
The authors have no conflicts of interest.
References
- 1.Radunovic M., Lazovic R., Popovic N., et al. Complications of laparoscopic cholecystectomy: our experience from a retrospective analysis. Open Access Maced. J. Med. Sci. 2016;4:641–646. doi: 10.3889/oamjms.2016.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunn D. Ghost surgery: a frank look at the issue and how to address it. AORN J. 2015;102:603–613. doi: 10.1016/j.aorn.2015.10.003. (quiz 614–6) [DOI] [PubMed] [Google Scholar]
- 3.Mathew G., Sohrabi C., Franchi T., et al. Preferred Reporting Of Case Series in Surgery (PROCESS) 2023 guidelines. Int. J. Surg. 2023;109:3760–3769. doi: 10.1097/JS9.0000000000000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang T.L., Cheng Y.F., Chen C.L., et al. Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant. Proc. 1996;28:1669–1670. [PubMed] [Google Scholar]
- 5.Kaafarani H.M.A., Smith T.S., Neumayer L., et al. Trends, outcomes, and predictors of open and conversion to open cholecystectomy in Veterans Health Administration hospitals. Am. J. Surg. 2010;200:32–40. doi: 10.1016/j.amjsurg.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 6.Katwal G., Thapa Y., Shrestha A., et al. Open cholecystectomy among patients undergoing laparoscopic cholecystectomy in a tertiary care centre: a descriptive cross-sectional study. JNMA J. Nepal Med. Assoc. 2022;60:444–447. doi: 10.31729/jnma.7371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moghul F., Kashyap S. StatPearls Publishing; 2023. Bile Duct Injury. [PubMed] [Google Scholar]
- 8.Ejaz A., Spolverato G., Kim Y., et al. Long-term health-related quality of life after iatrogenic bile duct injury repair. J. Am. Coll. Surg. 2014;219:923–932.e10. doi: 10.1016/j.jamcollsurg.2014.04.024. [DOI] [PubMed] [Google Scholar]
- 9.Clavien P.-A., Sarr M.G., Fong Y., et al. Springer; 2015. Atlas of Upper Gastrointestinal and Hepato-pancreato-biliary Surgery. [Google Scholar]
- 10.Myburgh J.A. The Hepp-Couinaud approach to strictures of the bile ducts. I. Injuries, choledochal cysts, and pancreatitis. Ann. Surg. 1993;218:615–620. doi: 10.1097/00000658-199321850-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kapoor V.K. Springer Nature; 2020. Post-cholecystectomy Bile Duct Injury. [Google Scholar]
- 12.Shah S.R., Mirza D.F., Afonso R., et al. Changing referral pattern of biliary injuries sustained during laparoscopic cholecystectomy. Br. J. Surg. 2000;87:890–891. doi: 10.1046/j.1365-2168.2000.01446.x. [DOI] [PubMed] [Google Scholar]
- 13.Stewart L., Way L.W. Laparoscopic bile duct injuries: timing of surgical repair does not influence success rate. A multivariate analysis of factors influencing surgical outcomes. HPB. 2009;11:516–522. doi: 10.1111/j.1477-2574.2009.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapoor V.K. Medico-legal aspects of bile duct injury. J Minim Access Surg. 2016;12:1–3. doi: 10.4103/0972-9941.169995. [DOI] [PMC free article] [PubMed] [Google Scholar]