Increases in injection drug use (IDU) as a result of increasing levels of opioid misuse in the United States may increase risk for new, rapidly transmitted HIV infections in communities with otherwise low HIV prevalence.1 Changing characteristics and geographic locations of persons at risk for HIV infection due to injection-related risk behavior present ongoing challenges to partner services for HIV prevention. These jurisdictions have historically had less need for HIV-related partner services and therefore less investment in HIV outbreak preparedness and prevention infrastructure. Jurisdictions with low HIV prevalence have also had to rely on cluster investigation methods that were developed for primary use in urban areas. In early 2019, the US strategic plan to end the HIV epidemic in the United States within 10 years was announced, which prioritizes the rapid detection and response to emerging clusters of HIV infection to further reduce new transmissions as 1 of the 4 main pillars of the initiative.2
Historically, partner services, the process of disease intervention specialists (DIS) interviewing persons with newly diagnosed HIV, eliciting names and contact information for their recent sexual and IDU partners, and reaching out to those persons for risk counseling and HIV testing, have been the principle prevention and control measure used in HIV and sexually transmitted disease (STD) outbreak response.3,4 Disease intervention specialists from state and local health departments, as well as the Centers for Disease Control and Prevention (CDC), continue to provide partner services in the United States as a primary component of both HIV and STD prevention and control programs.5 However, partner services protocols and methods have not evolved at the speed of changing HIV and STD epidemics. For example, the increased use of technology to meet and communicate with sexual partners has been associated with increased number of anonymous or casual sex partners,6-9 which are impediments to partner services owing to the potential for lack of reliable partner contact information. In addition, rural jurisdictions with historically low HIV prevalence may have smaller DIS staff and limited training opportunities compared with larger urban areas. These factors combine to make implementation of partner services more difficult in rural settings.
In late 2017, a team of DIS and epidemiologists from the CDC and the West Virginia Department of Health and Human Resources (WV DHHR), Bureau of Public Health, investigated and responded to a combined molecular and epidemiological cluster of HIV infections in West Virginia counties previously identified as highly vulnerable to rapid HIV dissemination through IDU behavior.10 Findings from this response indicated that most HIV infections were attributable to male-to-male sexual behavior.11 However, using enhanced partner services methods, we found evidence of potential bridging of HIV transmission from this network to persons who inject drugs.12 There are limited data and published programmatic experiences on how best to carry out effective HIV cluster investigations in the context of populations at risk for rapidly transmitted HIV infection due, in part, to IDU behavior. Here, we describe the preresponse approaches to HIV prevention that were already in place and the surge approach used in this response, with the intent of informing best practices for future HIV outbreak responses and strategic plans.
PRERESPONSE APPROACHES TO HIV PREVENTION IN WEST VIRGINIA
Paper-Based Data
At the time of the investigation, case assignments, interview records, and case management records were entirely paper based. Field and case management records were delivered via interoffice mail from the WV DHHR office to the WV DIS across the state’s 8 regions, which contributed to lack of timeliness in investigating clusters. Upon closure (disposition) of a field record and/or closure of a case file, the documents were mailed by WV DIS back to the WV DHHR office in Charleston. In addition, the absence of digital management software meant there was no formal system for tracking WV DIS progress with contact tracing and monitoring workloads for each WV DIS, creating significant barriers to timely STD/HIV surveillance.
Case Prioritization, Review, and Interview Practices
Review of WV DIS case prioritization protocols revealed that, although a prioritization system was in place with guidance for WV DIS, HIV and syphilis cases were equally prioritized for partner services investigations. In practice, HIV, syphilis, gonorrhea, and chlamydia cases were assigned concurrently to WV DIS for investigation. Although gonorrhea and chlamydia cases were concurrently investigated, priority was given to HIV and syphilis investigations per CDC partner services recommendations.5 However, there was no supervisory triage system to respond to a cluster of HIV infections. As a result, WV DIS would investigate cases linearly prioritizing index case investigations over investigating contacts within clusters—and did not have the flexibility to shift their priorities based on the identification of an ongoing HIV cluster. Although cases may often be investigated because they are reported in low prevalence jurisdictions, the CDC recommends maintaining structured case prioritization based on disease.5 Standard West Virginia HIV partner services practices involved interviewing only contacts of persons diagnosed with HIV who also tested positive for HIV It was also standard practice for DIS to collect information for past 12-month behavior during interviews.
Staffing-Related Barriers
There were several vacant WV DIS positions preceding and during the HIV cluster investigation leading the WV state DIS supervisor to function as a DIS. As a result, the WV state DIS supervisor was unable to provide critical supervision to WV DIS staff throughout the state or ensure that new WV DIS would undergo appropriate training. In addition, “chalk talks,” or DIS case conferences, were not routine practice within the WV partner services program. Chalk talks are a case management tool and considered partner services best practices,13 where DIS share investigative and interview techniques in an in-person or telephone-based peer-to-peer discussion to ensure that the information obtained through contact tracing is properly documented and effectively analyzed. Communication and coordination between WV DIS were informal, infrequent, and not centrally facilitated.
Partner Services Locating Capabilities
West Virginia DIS did not have access to the HIV or hepatitis surveillance registries to perform searches. The HIV, STD, and hepatitis data were also stored separately, making it difficult to identify coinfected individuals. Consequently, different WV DIS may have been trying to contact the same case or partner unknowingly for different infections. Furthermore, WV DIS had limited access to electronic databases for legal and public records–related information, such as LexisNexis, and instead relied on Internet search engines (e.g., Bing and Google) to find partners. The use of the Internet and venues accessed through the Internet, such as social networking sites, e-mail, instant messaging, and mobile devices, to conduct partner services, known as technology-based partner services or Internet partner services (IPS),14,15 had not been formally implemented by the WV partner services program. Therefore, WV DIS would use personal devices and personal social media accounts for partner notification; however, some WV DIS reported being uncomfortable using personal accounts. If WV DIS were uncomfortable using personal accounts, they would often create alternate accounts with which to contact partners. Partner notification and conducting interviews by telephone were default for WV partner services because of small number of available DIS and increasing numbers of cases and contacts. However, if the partner could not be reached by telephone in a reasonable time frame, other methods would be used including contact via social media, written letter, or field visits if necessary.
Geographic Considerations
Geography posed a challenge both in the terrain and long distances required to visit clients in person. DIS had to cover large rural areas, often facing issues relating to infrastructure including damaged roads or housing that could not be accessed via roads. HIV field testing was conducted if a partner could not or would not come to a local health department. The preference was for DIS to meet clients at the local health department for interviews and conduct concurrent HIV/STD testing. Because of increases in the number of individuals diagnosed with both HIV and syphilis, coming to the local health department allowed for both tests to be conducted and also mitigated issues posed by travel. However, partners also faced similar challenges in making their way to local health departments because of the geographic challenges.
Linkage to Care and Prevention Barriers
Routine WV DIS work included linkage to Ryan White Part B HIV case managers and implementation of HIV prevention strategies. There was not a designated linkage coordinator within WV DHHR, which is not unusual in jurisdictions with historically low HIV prevalence. Although DIS worked directly with HIV case managers in their respective region to link people to care, DIS sometimes had to directly link people recently diagnosed with HIV infections to HIV providers as the number of HIV cases increased quickly preresponse. Linkage to care for people who tested positive for HIV was also challenging owing to the limited number of HIV providers in WV Standardized risk reduction language was used by WV DIS while counseling clients on HIV prevention strategies; however, direct linkage to prevention tools such as preexposure prophylaxis (PrEP) could not always be provided. West Virginia DIS reported substantial barriers to referring clients for PrEP as part of HIV/STD partner services including limited PrEP provision among local healthcare providers, lack of informational materials for WV DIS to share with clients, and limited knowledge of PrEP access (e.g., how patients without insurance could obtain PrEP) among WV DIS. West Virginia DIS would refer clients that expressed interest in PrEP to regional infectious disease providers. No WV county health department clinics were prescribing PrEP at the time of the WV HIV cluster investigation.
SURGE RESPONSE ACTIVITIES
From September 27 to November 9, 2017, the CDC provided an 8-person surge team, consisting of CDC DIS and epidemiologists, who rotated time in the field to intensify partner services efforts in 15 counties in southern West Virginia and to determine whether bridging of HIV risk was occurring between gay, bisexual, or other men who have sex with men diagnosed with HIV in 2017 and 1 or more networks of persons who inject drugs alongside WV DIS. The CDC surge team had experience working in more than 20 different state and local health departments conducting STD/HIV case investigations and additional experience in surveillance, DIS training/development, and program management. Partner services best practices5 informed the CDC surge response, and in collaboration with the WV DHHR, an intensified partner services response was launched.
To ensure an orderly and well-informed response, several detailed protocols and standard operating procedures to guide response implementation that were informed by previous HIV outbreak responses16-18 were developed that were specific to the WV context. To further tailor the response design and approach, the CDC surge team also conducted in-depth interviews with the WV DIS supervisor and 2 WV DIS. The protocols detailed the structure of the response teams, daily operations, and laboratory procedures for CDC DIS. An enhanced interview guide was developed and integrated into the preexisting WV DHHR interview forms typically completed by WV DIS during interviews. The CDC surge team organized an orientation in Charleston before going into the field, during which all CDC DIS surge team members obtained state health department ID badges from the WV DHHR (Fig. 1). Having local ID badges was considered of great importance to address reported feelings of distrust toward outsiders including federal entities. DIS from the CDC were trained on the protocols and standard operating procedures before they left for the field.
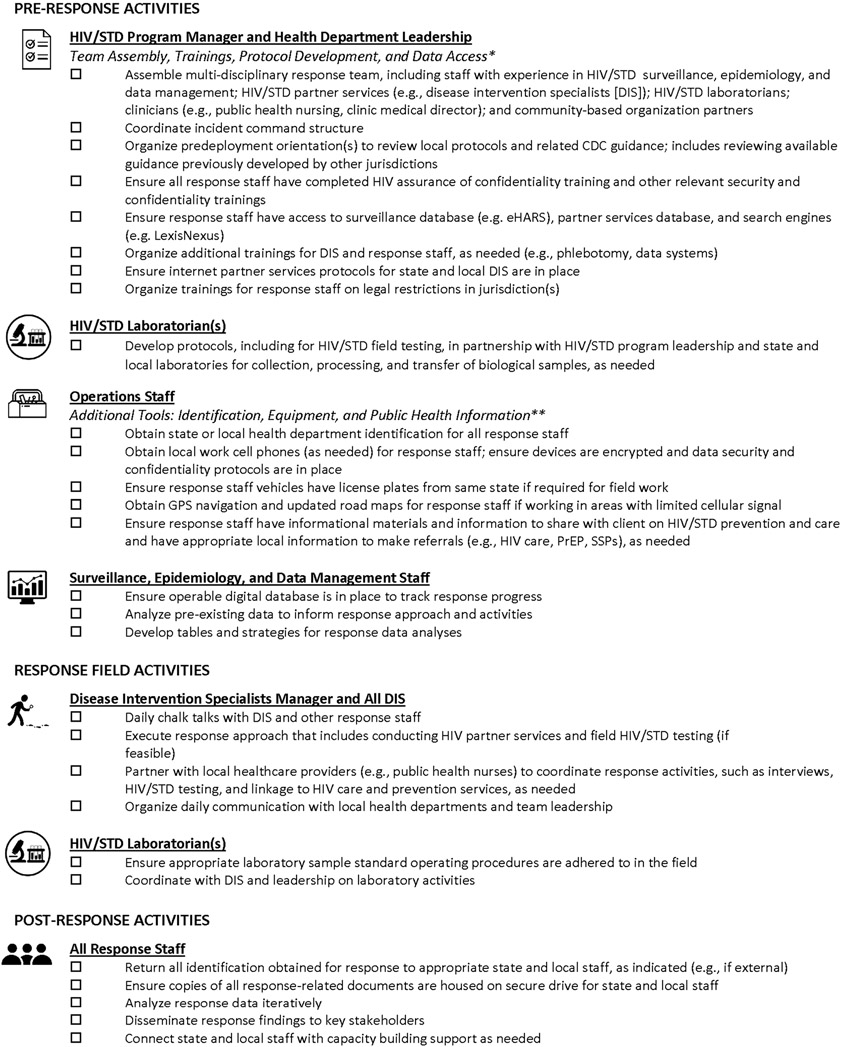
Figure 1.
Preparedness checklist for an HIV cluster or outbreak surge response. Best practices and activities are organized into a checklist that can be used by HIV cluster or outbreak surge response teams. The checklist is categorized by both response role (e.g., STD/HIV program leader and disease intervention specialist) and timing of when they should be considered during the response (e.g., preresponse activities, field activities, and postresponse activities).
*Activities may require longer time period for development and approvals (e.g., weeks to months) and should be planned ahead of time accordingly, as feasible
**Provision of materials, such as equipment, may be more resource intensive and depend on available funding
Abbreviations: eHARS, enhanced HIV/AIDS Reporting System; PrEP, pre-exposure prophylaxis; SSPs, syringe services programs
Before the surge team arrival, standard HIV partner services in WV entailed providing partner services only to HIV-positive contacts of persons diagnosed with HIV. During the surge, contacts of persons diagnosed with HIV (first-generation contacts) were tested for HIV and, regardless of their HIV status, interviewed by CDC DIS for risk behaviors and elicitation of contacts (second-generation contacts). DIS from the CDC also tested and interviewed second-generation contacts. Phlebotomy-trained CDC DIS drew blood from each participant for HIV, syphilis, hepatitis B, and HCV testing and performed rapid (fingerstick) HIV tests in the field. We also implemented a fourth-generation rapid HIV testing algorithm rapid tests, including the INSTI® HIV-1/HIV-2 Antibody Test and the Alere Determine HIV–1/2 Ag/Ab Combo19 to replace third-generation testing as part of the surge response best practices. Cases and contacts were referred to HIV clinical and prevention services, as appropriate, including regional harm reduction programs in 2 of the response counties, social services, and follow-up care. Additional information on WV harm reduction programs is published elsewhere.12
Several activities helped ensure success in this response including digitization of case investigation records, structure of response teams, and daily operations.
Digitization of Case Investigation Records and Partner Location Efforts
In an effort to digitize all of the HIV case investigation records, a short-term partner services database in Microsoft Access that mirrored the WV DHHR interview record and field record forms was created. All the data from the existing HIV case interview records and field record forms, including all named contacts, were entered into the database. Data from enhanced HIV/AIDS reporting system were merged into the short-term partner services database to identify clients previously diagnosed with HIV. Data from the STD and hepatitis databases could not be merged with the short-term partner services database. However, we were able to abstract data from these respective databases to inform contact tracing efforts. We enhanced record searching capacity by enabling CDC DIS access to search engines including LexisNexis. DIS from the CDC also had access to the short-term partner services database to conduct searches and update information. The database allowed us to track assignments to CDC DIS and manage information on cases, first-generation contacts, and second-generation contacts during the response, including real-time results of HIV and STD field testing. DIS from the CDC used encrypted work mobile phones such that they could communicate with clients while in the field, as well as other team members. To ensure data security and confidentiality, all devices were securely wiped of all investigation information immediately after the case investigation and overall response. All DIS completed assurance of confidentiality training.
Structure of Response Teams
A total of 6 CDC DIS were based in 3 distinct field sites dispersed across the 15 counties included in the response to be able to better reach clients who were often in remote areas. DIS from the CDC visited local county health departments near their respective field sites to perform record searches and speak with health department staff and WV DIS in an effort to reach clients in their respective areas. They would record search at the local county health office and engage Clerical and Public Health Nursing (PHN) staff who served as key partners in providing additional information and links to other relevant agencies. The CDC surge staff were also based out of the 3 field sites to support CDC DIS, including an HIV/STD laboratorian who served as a counterpart to the state and local laboratory partners and assisted with the development of the laboratory protocols and the tracking of laboratory results for clients throughout the response.
Daily Operations
The CDC DIS surge team, WV DIS, and PHN staff held regular daily meetings at their respective field sites to discuss open investigations. These meetings, similar in content and purpose to chalk talks used in routine partner services practice, afforded an opportunity to prioritize contacts based on real-time information, discuss successes and challenges, address problems, and ensure mutual understanding of goals and objectives. Routinely in these discussions, WV DIS were able to provide extensive insight into logistics, health care resources, cultural nuances, and relevant information that facilitated the successful disposition of case investigations. The daily meetings were also important opportunities to engage with PHN staff who served as key partners in encouraging contacts to come in for testing and interviewing and linking contacts to additional health services. In addition to meetings and contact tracing, CDC staff generated data reports to inform the outreach approach, including social network data visualization using MicrobeTrace software.20 The team was able to approach the response from a cluster perspective rather than working cases in a linear fashion owing to the social network data visualizations.
DIS from the CDC were able to share best practices, policies, and procedures from the CDC and other state health departments to assist the host site. The CDC surge team shared additional tools and guidance including best practices for interview periods, prioritization of STD/HIV cases when faced with heavier-than-usual workloads, and IPS protocols.5,15 The CDC encourages the adaption and integration of technology into partner services activities,15 which can enhance partner services outcomes including partner elicitation, notification, testing, and identifying new infections.14 As part of HIV and STD outbreak response plans, health departments should have IPS protocols in place, which can outline staffing, technological, and training needs, standard operating procedures, and local policies to ensure data security and confidentiality are maintained. After the response, the team was able to compile and share DIS manuals from other jurisdictions with WV DHHR to adapt for the local context. As CDC DIS encountered and tested contacts and others at risk for HIV during the response, they noted that PrEP awareness was low. A simple palm card was subsequently created listing all PrEP providers in southern WV and shared with clients during the investigation. The palm card was updated twice during the response as a result of work to increase PrEP accessibility in coordination with WV DHHR, local area providers, and county health department leadership. We secured educational materials about PrEP from Charleston Medical Center for the CDC and WV DIS to have on hand for clients as well.
RESPONSE OUTCOMES
As described by Bradley et al.,12 as a result of the cluster surge response, the response team interviewed 78 people including 39 (83%) of the 47 with 2017 HIV diagnoses and 39 (20%) of the 192 reported contacts (first and second generations) using the enhanced interview guide. Other persons with 2017 diagnoses (17%; n = 8) and contacts (80%; n = 153) could not be located or reached for interview. The response rate for interviewing contacts was suboptimal and contributed to an incomplete picture of the network. Among men interviewed during the surge response, most reported having had sex with at least 1 male partner (71% of men with diagnosed HIV and 86% of male contacts) in the past 12 months; a smaller proportion reported female sex partners (32% of men with diagnosed HIV and 24% of male contacts). When asked about past 12-month IDU behavior, 13% of persons with 2017 HIV diagnoses and 21% of their contacts reported IDU. In addition, 8% of persons with 2017 HIV diagnoses and 16% of their contacts reported sharing needles or other injection equipment in the past 12 months. Additional information on the main response outcomes is published elsewhere.11
There were several challenges faced by staff during this investigation. Clients reported high levels of stigma in the small, local communities related to HIV and IDU. Alongside stigma related to HIV and IDU, experienced and perceived homophobias were commonly reported. Taken together, this stigma affected clients’ willingness to communicate with CDC or WV DIS staff in the field and contributed to fears regarding confidentiality. The close nature of social networks in the small communities across southern WV intensified concerns and was a barrier to performing traditional in-person partner services activities. Fears regarding stigma in the community were further compounded by a general distrust of people not from that respective community including CDC DIS who came from out of state. DIS from the CDC used work mobile phones and rental cars with license plates from other states making them more recognizable and potentially contributed to overall distrust of the CDC DIS among community members.
Navigation of the regional geographic terrain also posed as a major challenge to CDC DIS in trying to reach clients during this investigation. The CDC and WV DIS had to travel long distances along mountain roads that were at times too steep and/or narrow to drive or, in some instances, were blocked by felled trees or taken out by rockslides or mudslides. Therefore, it could take an entire day to reach and interview a single client. Signals for mobile phones, tablets, and GPS within vehicles were unreliable in these rural regions, making it difficult to use navigational services or to communicate with clients or other field staff. In addition, clients could be difficult to locate because of frequent unstable housing and telephone numbers, such that home addresses and telephone numbers on file were not always reliable. In other circumstances, communities had recently renamed streets or redesignated address numbers; however, corresponding changes were not implemented within GPS services or local maps, resulting in CDC DIS driving long distances to incorrect locations. In cases where there were no searchable addresses for clients, CDC DIS had to rely on detailed instructions from local community members on how best to locate clients.
LONG-TERM CAPACITY BUILDING
Establishing programmatic approaches to increases in HIV or other diseases before they occur are critical; local and state health departments may benefit from identifying preparedness opportunities in their programs. Capacity-building strategies for programs as longer-term investments are recommended for HIV cluster prevention and effective HIV outbreak response plans across all jurisdictions, particularly those with increased vulnerability for rapid HIV transmission. These strategies may be particularly important for jurisdictions that have historically low HIV prevalence and as a result have not had as much applied experience navigating HIV outbreaks. This includes prioritizing investment in partner services and social network visualization software, the digitization of case investigation records, and integrating data across separate databases (bacterial STDs, HIV, and hepatitis). Comprehensive partner services software and social network visualization software, such as MicrobeTrace,20 can help identify clusters in real time, assist in prioritizing clusters for investigation, and provide a more complete picture of the networks for public health staff. MicrobeTrace and similar software are available from the CDC at little or no expense to jurisdictions. HIV molecular surveillance data have been used for use in addressing the HIV epidemic21,22 and can help identify HIV infections that are genetically linked and therefore may represent a cluster of infections. However, the ability of molecular surveillance data to help control HIV outbreaks relies heavily on the success of prevention and control measures such as partner services and HIV testing. Molecular surveillance is not able to fill in the network gaps that may result from contacts that have not been tested for HIV and those that are unlocatable or anonymous. Furthermore, molecular surveillance for prioritizing partner services during a response is limited because of the time lag receiving genetic sequence data. Digitization of case investigation records allows for the data to be easily analyzed and examined regularly, such that clusters can be identified early and public health efforts can be targeted. HIV and STD program collaboration and service integration, including use of local surveillance data, is recommended by the CDC to maximize public health impact and facilitate comprehensive delivery of services.5 This alignment of programs and services should be prioritized to include data systems integration to ensure more comprehensive prevention and control HIV/STD services. The integration of HIV and STD data across separate databases can improve efficiency and streamline partner services investigations to prevent multiple DIS investigating the same contacts for a coinfected client. Furthermore, reports of new HCV infections can serve as markers of communities at risk for rapid HIV transmission due to IDU.16 Integrated HIV/STD data systems can also increase the ability for partner services programs and DIS to recognize these communities and individuals at risk and potentially link them to preventative services.
Alongside investment in software and data integration, workforce development is a key long-term partner services capacity-building strategy. This includes hiring, training, and retraining staff who have expertise to investigate and intervene during HIV cluster responses. These staff can be tasked with developing and implementing approaches to integrate data rapidly and provide real-time information on cluster detection and response. They should be supported to attend national-level training and conferences to ensure they are up-to-date on the most recent partner services approaches. All relevant staff can be trained to implement policies and systems to support secure and smooth data sharing with appropriate partners within and across jurisdictions. In addition, jurisdictions can leverage existing infrastructure for response preparedness, including training a variety of staff from across health department divisions on disease outbreak response plans such that they could be pulled quickly and efficiently to fill needed response roles. Furthermore, jurisdictions can harness existing partnerships with community-based organizations and/or academic institutions to assist with trainings and capacity-building activities.
CONCLUSIONS
HIV cluster investigation and response is a key pillar of the end the HIV epidemic plan outlined by Fauci et al.2 Multiple methods for identifying HIV clusters including partner services, epidemiological data, and molecular data exist.17,21,22 However, many jurisdictions recently impacted by HIV vis-à-vis the opioid epidemic must rely on traditional partner services that may not necessarily be as effective in rural areas as demonstrated by our findings of suboptimal contact rates from enhanced partner services. Rural jurisdictions with historically low HIV prevalence may benefit from technological advancements such as digitization of case investigation records and partner location efforts, in addition to HIV and STD data systems integration; data system integration can reduce DIS burden and time spent per individual contact, and allow for increased coordination with injurisdictions. Funding and support for local health departments and health department efforts related to partner services has been slowly eroding over the past decade. Reductions in funding alongside low historic need for HIV prevention in rural jurisdictions, such as West Virginia, have meant the capacity-building efforts outlined here could not be supported. However, it will be important to consider these capacity-building options as the United States increases efforts to eliminate HIV transmission. The recommendations put forward here can help jurisdictions prepare for HIV clusters and have the capacity to respond rapidly when they are detected.
Conflict of Interest and Sources of Funding:
No conflicts of interest have been declared for any author on this article. This work was supported by the US Centers for Disease Control and Prevention.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Lerner AM, Fauci AS. Opioid injection in rural areas of the United States: A potential obstacle to ending the HIV epidemic. JAMA 2019; 322(11):1041–104. [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS, Redfield RR, Sigounas G, et al. Ending the HIV epidemic: A plan for the United States. JAMA 2019; 321:844–845. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein KT, Stephens SC, Moss N, et al. Partner services as targeted HIV screening—Changing the paradigm. Public Health Rep 2014; 129 Suppl 1(Suppl 1):50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golden MR, Hogben M, Handsfield HH, et al. Partner notification for HIV and STD in the United States: Low coverage for gonorrhea, chlamydial infection, and HIV. Sex Transm Dis 2003; 30:490–496. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm Rep 2008; 57(RR-9): 1–83; quiz CE1–4. [PubMed] [Google Scholar]
- 6.Taylor M, Aynalem G, Smith L, et al. Correlates of Internet use to meet sex partners among men who have sex with men diagnosed with early syphilis in Los Angeles County. Sex Transm Dis 2004; 31:552–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chew Ng RA, Samuel MC, Lo T, et al. Sex, drugs (methamphetamines), and the internet: Increasing syphilis among men who have sex with men in California, 2004-2008. Am J Public Health 2013; 103:1450–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA 2000; 284:443–446. [DOI] [PubMed] [Google Scholar]
- 9.Kim AA, Kent C, McFarland W, et al. Cruising on the Internet highway. J Acquir Immune Defic Syndr 2001; 28:89–93. [DOI] [PubMed] [Google Scholar]
- 10.Van Handel MM, Rose CE, Hallisey EJ, et al. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J Acquir Immune Defic Syndr 2016; 73:323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans ME, Labuda SM, Hogan V, et al. Notes from the field: HIV infection investigation in a rural area—West Virginia, 2017. MMWR Morb Mortal Wkly Rep 2018; 67:257–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bradley H, Hogan V, Agnew-Brune C, et al. Increased HIV diagnoses in West Virginia counties highly vulnerable to rapid HIV dissemination through injection drug use: A cautionary tale. Ann Epidemiol 2019; 34:12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Program Operations Guidelines for STD Prevention: Partner Services. Atlanta, GA: US Department of Health and Human Services, 2001. Available at: https://stacks.cdc.gov/view/cdc/40225. [Google Scholar]
- 14.Kachur R, Hall W, Coor A, et al. The use of technology for sexually transmitted disease partner services in the United States: A structured review. Sex Transm Dis 2018; 45:707–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kachur RSF, Kinsey J, Collins D. Introducing Technology into Partner Services: A Toolkit for Programs. Atlanta, GA: Centers for Disease Control and Prevention, 2015. Available at: https://www.cdc.gov/std/program/ips/default.htm. [Google Scholar]
- 16.Peters PJ, Pontones P, Hoover KW, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med 2016; 375:229–239. [DOI] [PubMed] [Google Scholar]
- 17.Campbell EM, Jia H, Shankar A, et al. Detailed transmission network analysis of a large opiate-driven outbreak of HIV infection in the United States. J Infect Dis 2017; 216:1053–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dasgupta S, Broz D, Tanner M, et al. Changes in reported injection behaviors following the public health response to an HIV outbreak among people who inject drugs: Indiana, 2016. AIDS Behav 2019; 23:3257–3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Implementing HIV Testing in Nonclinical Settings: A Guide for HIV Testing Providers. Atlanta, GA: US Department of Health and Human Services, 2016. Available at: https://www.cdc.gov/hiv/testing/nonclinical/index.html. [Google Scholar]
- 20.Boyles A, Aslakson E. MicrobeTrace. [Website] 2018; v.0.2.0: Available at: http://github.com/cdcgov/microbetrace. Accessed February 18, 2020. [Google Scholar]
- 21.Oster AM, France AM, Panneer N, et al. Identifying clusters of recent and rapid HIV transmission through analysis of molecular surveillance data. J Acquir Immune Defic Syndr 2018; 79:543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oster AM, France AM, Mermin J. Molecular epidemiology and the transformation of HIV prevention. JAMA 2018;319:1657–1658. [DOI] [PubMed] [Google Scholar]