Abstract
Abdominal pain in patients with significant alcohol use and smoking history presents diagnostic challenges due to overlapping clinical features of complications like acute cholecystitis and peptic ulcers. The unreliable physical examinations of intoxicated patients often complicate accurate diagnosis. We present a case of a 56-year-old male with a history of alcoholism and smoking, who presented to the emergency department with nonspecific abdominal pain. Initial imaging suggested cholecystitis, but due to the patient's intoxication, his physical examination was unreliable. During a laparoscopic cholecystectomy, a perforated prepyloric ulcer was unexpectedly discovered, sealed by the gallbladder. This case highlights the limitations of relying solely on imaging for diagnosing abdominal conditions in intoxicated patients. The intraoperative discovery of the perforated ulcer necessitated a shift in the surgical approach, emphasizing the need for flexibility in surgical planning and a high index of suspicion for other abdominal pathologies in patients with significant lifestyle risks. The successful management of this patient through adaptive surgical techniques and comprehensive postoperative care, including Helicobacter pylori eradication therapy, underscores the importance of maintaining a broad differential diagnosis and readiness to adapt surgical plans. This approach is essential for managing complex cases effectively, ensuring that both the immediate surgical issues and underlying causes are addressed to optimize recovery and prevent recurrence.
Keywords: Abdominal pain, Acute cholecystitis, Prepyloric ulcer, Peptic ulcer perforation, Alcoholism, Smoking, Helicobacter pylori, Laparoscopic surgery, Graham patch repair
Introduction
Abdominal pain is one of the most common yet complex challenges in emergency medicine, demanding a deep understanding of its diverse causes and implications [1]. Among the critical conditions associated with abdominal pain are acute cholecystitis and duodenal ulcers, which stand out due to their potential severity and the complexities involved in their diagnosis and management [1,2]. Acute cholecystitis, often triggered by gallstones, manifests typically with right upper quadrant pain [3]. The variability in presentation, influenced by the level of inflammation and complications such as perforation, highlights the necessity for precise diagnostic strategies.
The reliability of the abdominal examination often becomes compromised in cases involving intoxicated or noncooperative patients, further complicating the identification of underlying pathologies, particularly when symptoms are vague [4]. These scenarios require a high index of suspicion and often rely heavily on imaging techniques, although these tools also have limitations. This scenario exemplifies the need for adaptable diagnostic approaches that can accommodate the complexities of individual patient presentations [5,6].
Furthermore, the impact of lifestyle factors such as alcohol consumption and smoking on the gastrointestinal system cannot be overstated [6]. Both habits significantly contribute to the development of gastrointestinal disorders, including ulcers and gallbladder diseases [7]. Alcohol, by increasing gastric acid secretion and decreasing mucosal defense, and smoking, by impairing mucosal blood flow and enhancing the harmful effects of Helicobacter pylori, synergistically elevate the risk of complications like perforations [8,9]. Understanding these relationships is crucial for effective patient counseling and preventive care strategies, emphasizing the need for an integrated approach to patient education and management [10].
Case presentation
A 56-year-old male with a significant history of alcoholism and smoking presented to the emergency department exhibiting non-specific abdominal pain. The patient was notably intoxicated upon arrival, complicating the clinical examination. He was uncooperative and exhibited right upper quadrant tenderness and guarding. His medical history was significant for a Mallory-Weiss syndrome episode, likely induced by excessive alcohol consumption.
On initial presentation, the lab results were as follows: white blood cell count (WBC) was 6.6 K/uL (normal range: 4.0-11.0 K/uL), hemoglobin (Hgb) was 13.0 g/dL (normal range: 13.8-17.2 g/dL), total bilirubin was 0.30 mg/dL (normal range: 0.3-1.2 mg/dL), aspartate aminotransferase (AST) was 32 U/L (normal range: 10-40 U/L), and alanine aminotransferase (ALT) was 39 U/L (normal range: 7-56 U/L).
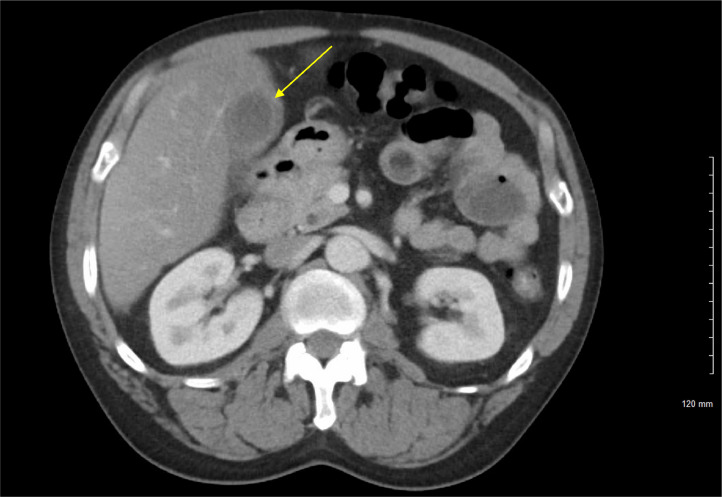
Despite his intoxication, a CT scan (Fig. 1, Fig. 2) and ultrasound (Fig. 3, Fig. 4) of his abdomen were performed due to the persistence of his symptoms. The imaging revealed gallbladder wall thickening and cholelithiasis, suggesting acute cholecystitis. Given the patient's symptoms and imaging results, he was scheduled for a laparoscopic cholecystectomy.
Fig. 1.
Axial computerized tomography (CT) with IV contrast of the abdomen that shows gallbladder wall thickening and mucosal enhancement (yellow arrow). No radiopaque stones were identified. Findings are consistent with acute cholecystitis.
Fig. 2.
Sagittal CT with IV contrast of the abdomen and pelvis, blue arrow pointing to gallbladder mucosal enhancement.
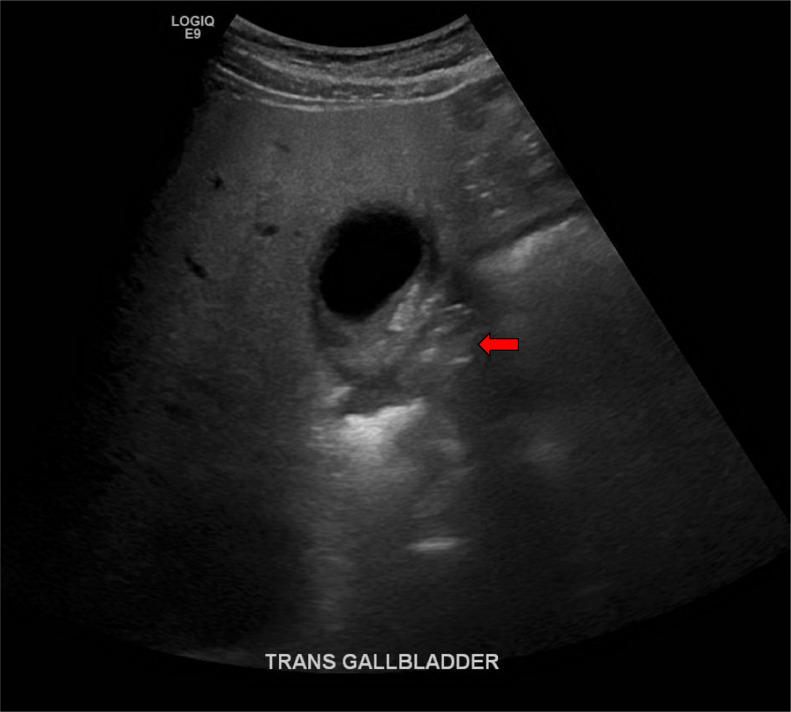
Fig. 3.
Right upper quadrant ultrasound sagittal view with cholelithiasis (blue arrow) and gallbladder wall thickening.
Fig. 4.
Right upper quadrant ultrasound transverse view, shows gallbladder wall thickening and a red arrow pointing to the area of contained perforated pre-pyloric ulcer.
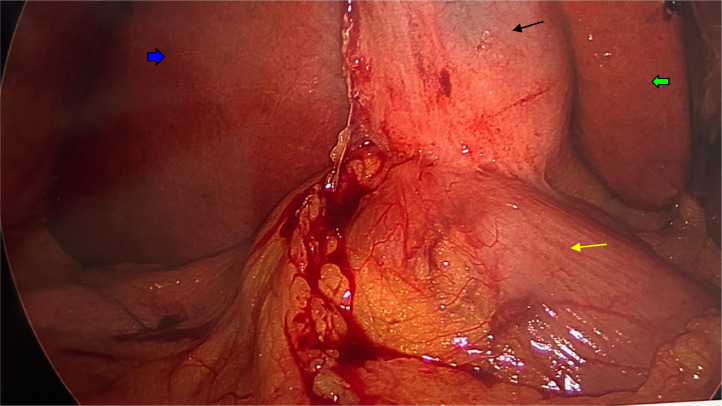
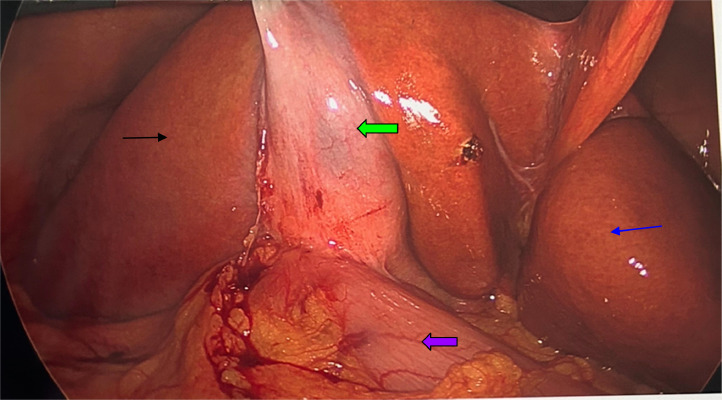
Intraoperative findings
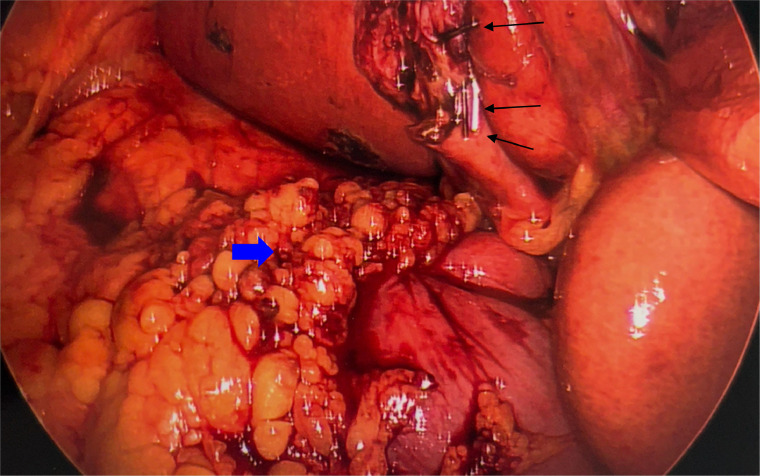
During the laparoscopic procedure, dense adhesions were found between the gallbladder and the duodenum. Upon dissection, an abscess cavity was entered, revealing a prepyloric ulcer sealed by the gallbladder wall (Fig. 5, Fig. 6). This finding necessitated a modified approach; a Graham patch repair was performed on the prepyloric ulcer (Fig. 7), and the cholecystectomy proceeded with careful dissection due to significant inflammation.
Fig. 5.
Intraoperative laparoscopic view of the right upper quadrant. Blue arrow (right lobe of the liver) black arrow (retracted gallbladder), green arrow (left lobe of the liver), yellow arrow (pylorus).
Fig. 6.
Intraoperative laparoscopic view of the right upper quadrant. The black arrow (right hepatic lobe), blue arrow (left hepatic lobe), green arrow (retracted gallbladder), and purple arrow (pylorus).
Fig. 7.
Intraoperative laparoscopic view of the right upper quadrant after completion of the procedure. Black arrows show clips on the cystic duct and cystic artery, and the blue arrow points to a tongue of omentum used for graham patch repair.
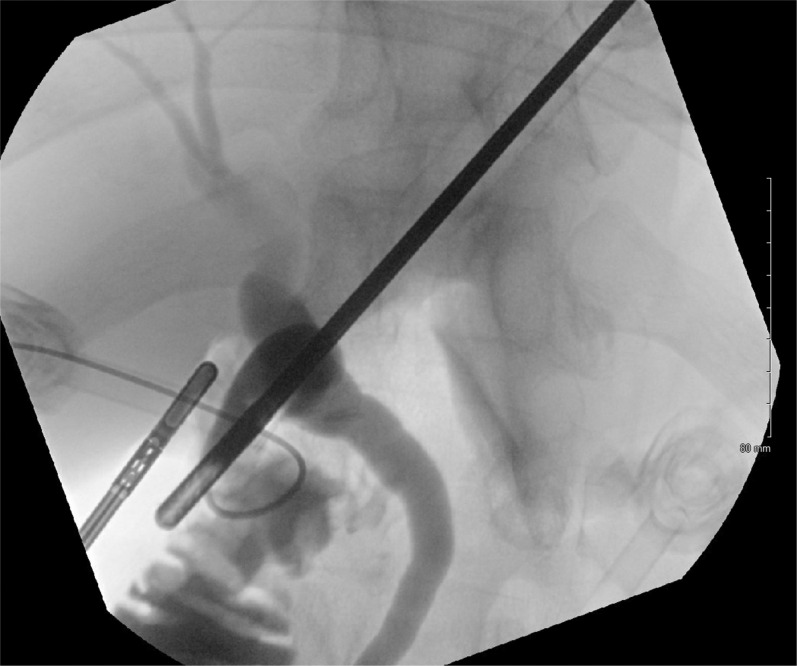
The inflamed tissues and complex adhesions led to challenges in controlling the cystic artery, which was eventually clipped for hemostatic control. Multiple cholangiograms were performed to ensure there were no bile duct injuries or leaks before concluding the surgery (Fig. 8).
Fig. 8.
Intraoperative cholangiogram shows good proximal and distal filling of the biliary tree and good emptying into the duodenum. No filling defects are appreciated.
Postoperative course
The patient's postoperative period was unremarkable. He was managed with nasogastric suction, intravenous antibiotics, and PPIs to prevent infection and manage gastric acidity. His recovery was monitored with an upper GI study (Fig. 9) which confirmed no leaks from the ulcer repair site. The patient was gradually transitioned from a clear liquid diet to a regular diet and discharged on postoperative day 6 on triple therapy for Helicobacter pylori eradication.
Fig. 9.
Fluoroscopic Gastrographin upper GI study. Water-soluble contrast was administered through the patient's nasogastric tube. The image demonstrates opacification of the stomach and proximal small bowel without evidence of extravasation of the contrast to suggest a leak. Contrast flowed freely into the proximal small bowel loops.
Discussion
This case report describes a 56-year-old male with significant lifestyle risks (alcoholism and smoking), presenting with nonspecific abdominal pain, who was ultimately found to have a perforated pre-pyloric ulcer sealed by the gallbladder during an operation initially intended to treat presumed acute cholecystitis. This scenario illustrates the complexities involved in diagnosing and managing abdominal emergencies, particularly in patients with unreliable clinical examinations.
Diagnostic challenges
The initial assessment was hindered by the patient's intoxication, which is a common obstacle in emergency settings. The diagnostic process in such patients must be approached with flexibility and a readiness to adapt based on evolving intraoperative findings. Although imaging studies (CT and ultrasound) suggested cholecystitis by showing gallbladder wall thickening and cholelithiasis, these modalities failed to detect the prepyloric ulcer, a critical finding only revealed during surgery. This highlights a pivotal learning point about the limitations of imaging in abdominal diagnostics, especially in the presence of acute inflammatory processes that may obscure or mimic other pathologies.
Diagnostic limitations of imaging modalities
Imaging studies play a crucial role in the initial evaluation and diagnosis of abdominal pain, especially in patients with confounding factors such as intoxication. However, the literature highlights significant limitations of imaging modalities in certain contexts [11]. While CT scans and ultrasounds are invaluable in diagnosing conditions like acute cholecystitis, as they can reveal gallbladder wall thickening, cholelithiasis, and mucosal enhancement, they may fail to detect other critical pathologies [12]. For instance, prepyloric ulcers, particularly those sealed by adjacent organs like the gallbladder, can be missed. Studies indicate that the sensitivity of CT scans for detecting perforated peptic ulcers can be compromised by factors such as localized inflammation and the presence of adhesions, which obscure direct visualization of the ulcer site [13]. Additionally, ultrasound, although effective for identifying gallbladder-related issues, is less reliable for detecting gastric and duodenal ulcers due to its lower resolution for deeper abdominal structures [14].
Surgical insights
The intraoperative discovery of the prepyloric ulcer necessitated an immediate surgical strategy adjustment, illustrating the importance of being prepared for unexpected findings during abdominal surgeries. The use of a Graham patch repair, a procedure typically reserved for peptic ulcer perforations, points out the adaptability required in surgical practice.
Lifestyle factors and gastrointestinal health
This case also brings to light the detrimental impact of lifestyle choices on gastrointestinal health. Alcohol and smoking are well-documented risk factors for both cholecystitis and peptic ulcers [8]. Alcohol can increase gastric acid secretion while decreasing the protective mucosal barrier, thereby predisposing to ulcer formation. Smoking not only exacerbates the effects of Helicobacter pylori but also impairs the healing of gastric mucosa [15]. Recognizing these factors is crucial for developing effective management and preventative strategies, highlighting the necessity of integrating lifestyle modification counseling as part of comprehensive patient care.
Management of helicobacter pylori
Another critical aspect of this case is the management of Helicobacter pylori, a key factor in the development of duodenal ulcers [16]. The decision to initiate triple therapy postoperatively reflects the current best practices for managing Helicobacter pylori-associated peptic ulcer disease [16].
Conclusion
This case report encapsulates the critical importance of adaptability and comprehensive care in the management of complex abdominal pathologies. The discovery of a contained perforated pre pyloric ulcer during a routine cholecystectomy highlights the necessity for surgeons to remain vigilant and prepared for unexpected findings, particularly in patients with complicating factors such as intoxication and unreliable selfreporting.
The insights derived from this case contribute to the broader medical understanding of how intertwined lifestyle factors and underlying health conditions can complicate the presentation and management of abdominal emergencies. Ultimately, this case emphasizes the critical need for thorough evaluation, preparedness for variable intraoperative scenarios, and a tailored approach to treatment that addresses all aspects of the patient's health.
Patient consent
We confirm that we have obtained written, informed consent from the patient for the publication of this case report. The patient has been thoroughly informed about the details that will be published and understands the implications of the publication. The written consent is stored securely and is available for review by the editorial team upon request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Yew KS, George MK, Allred HB. Acute abdominal pain in adults: evaluation and diagnosis. Am Fam Physician. 2023;107(6):585–596. [PubMed] [Google Scholar]
- 2.Minten L, Messiaen P, Van der Hilst J. Acute abdominal pain: a challenging diagnosis. Acta Gastroenterol Belg. 2022;85(4):646–647. doi: 10.51821/85.4.9860. [DOI] [PubMed] [Google Scholar]
- 3.Gallaher JR, Charles A. Acute cholecystitis: a review. JAMA. 2022;327(10):965–975. doi: 10.1001/jama.2022.2350. [DOI] [PubMed] [Google Scholar]
- 4.Rezar R, Jung C, Mamandipoor B, Seelmaier C, Felder TK, Lichtenauer M, et al. Management of intoxicated patients - a descriptive outcome analysis of 4,267 ICU patients. BMC Emerg Med. 2022;22(1):38. doi: 10.1186/s12873-022-00602-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hakala T, Kylmä J, Mäkelä KL, Noppari E, Koivunen M. Caring for alcohol-intoxicated patients in an emergency department from the nurses' point of view: focus on attitudes and skills. Scand J Caring Sci. 2021;35(1):115–122. doi: 10.1111/scs.12825. [DOI] [PubMed] [Google Scholar]
- 6.Yuan S, Chen J, Ruan X, Sun Y, Zhang K, Wang X, Li X, Gill D, et al. Smoking, alcohol consumption, and 24 gastrointestinal diseases: Mendelian randomization analysis. Elife. 2023;12:e84051. doi: 10.7554/eLife.84051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGee EE, Jackson SS, Petrick JL, Van Dyke AL, Adami HO, Albanes D, et al. Smoking, alcohol, and biliary tract cancer risk: a pooling project of 26 prospective studies. J Natl Cancer Inst. 2019;111(12):1263–1278. doi: 10.1093/jnci/djz103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Xiao Z, Ye K, Xu L, Zhang Y. Smoking, alcohol consumption, diabetes, body mass index, and peptic ulcer risk: a two-sample Mendelian randomization study. Front Genet. 2022;13:992080. doi:10.3389/fgene.2022.992080 [DOI] [PMC free article] [PubMed]
- 9.Tuerk E, Doss S, Polsley K. Peptic ulcer disease. Prim Care. 2023;50(3):351-362. doi:10.1016/j.pop.2023.03.003 [DOI] [PubMed]
- 10.Cutilli CC. Excellence in patient education: evidence-based education that “sticks” and improves patient outcomes. Nurs Clin North Am. 2020;55(2):267–282. doi: 10.1016/j.cnur.2020.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Nam D, Barrack RL, Potter HG. What are the advantages and disadvantages of imaging modalities to diagnose wear-related corrosion problems? Clin Orthop Relat Res. 2014;472(12):3665–3673. doi: 10.1007/s11999-014-3579-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hussain S, Mubeen I, Ullah N, Shah SSUD, Khan BA, Zahoor M, Ullah R, et al. Modern diagnostic imaging technique applications and risk factors in the medical field: a review. Biomed Res Int. 2022;2022:5164970. doi: 10.1155/2022/5164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Catalano O. [Computed tomography in the study of gastrointestinal perforation] Radiol Med. 1996;91(3):247–252. [PubMed] [Google Scholar]
- 14.Chen CH, Huang HS, Yang CC, Yeh YH. The features of perforated peptic ulcers in conventional computed tomography. Hepatogastroenterology. 2001;48(41):1393–1396. [PubMed] [Google Scholar]
- 15.Collatuzzo G, Alicandro G, Bertuccio P, Pelucchi C, Bonzi R, Palli D, et al. Peptic ulcer as mediator of the association between risk of gastric cancer and socioeconomic status, tobacco smoking, alcohol drinking and salt intake. J Epidemiol Community Health. 2022;76(10):2–6. doi: 10.1136/jech-2022-219074. [DOI] [PubMed] [Google Scholar]
- 16.Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou JM, Schulz C, et al. European Helicobacter and Microbiota Study group. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022;71(9):1724–1750. doi: 10.1136/gutjnl-2022-327745. [DOI] [Google Scholar]