Abstract
Background:
Knee osteoarthritis (OA) is a prevalent degenerative disease affecting synovial joints, predominantly the knee, leading to various complications, including mental health conditions like depression and anxiety. This systematic review aimed to determine the prevalence of depression and anxiety in knee OA patients.
Methods:
A comprehensive literature search was conducted in various databases till September 15, 2023. Studies focusing on the prevalence of mental health issues in patients with knee OA were included, excluding narrative reviews, protocols, unpublished reports, editorials, case reports, abstracts, and commentaries. All statistical analyses were performed in R version 4.2.3.
Results:
This review included a total of 14 studies involving middle-aged to elderly adult patients with knee OA, with ages ranging from 45 to 75 years. Among these, 13 studies involving 3390 adult patients with an average age of 59.75 years reported a pooled prevalence of depression of 30% (95% confidence interval: 18–43), demonstrating a substantial heterogeneity (I 2=98%). Additionally, anxiety was identified with a combined prevalence of 27% (95% confidence interval: 24–30) based on three studies that included 1407 older adult patients with an average age of 62.1 years. These studies displayed minimal heterogeneity (I 2=7%).
Conclusion:
The findings show a significant prevalence of depression among adult patients with knee OA and anxiety among older adults with knee OA, emphasizing the need for integrated healthcare approaches that address both orthopedic and mental health conditions. More comprehensive research is essential to deepen our understanding of the connection between mental illnesses and knee OA and to develop effective preventive and treatment strategies.
Keywords: anxiety, depression, osteoarthritis, prevalence, systematic review
Introduction
Highlights
A significant prevalence of depression (30%) and anxiety (27%) among knee osteoarthritis (OA) patients aged 45–75 years underscores the global mental health challenge within this demographic.
Variations in depression prevalence due to different diagnostic scales and study designs underscore the impact of diagnostic methods on outcomes, highlighting the necessity for standardized diagnosis.
Psychological health assessments, including routine screenings for depression and anxiety, into knee OA management, emphasizing a holistic care approach that addresses both orthopedic and mental health needs.
OA is a quintessential degenerative illness predominantly affecting synovial joints1. It registers the highest incidence among all inflammatory joint diseases. The condition is characterized by gradual degeneration and ensuing damage to the articular cartilage, often leading to secondary harm to adjacent structures like bones and ligaments1. OA typically results in deformity, pain, and functional disability. Radiographically, pathological alterations such as the degeneration of articular cartilage, the formation of osteophytes, and the narrowing of joint space are discernible. Clinically, the manifestations of OA extend to stiffness, joint pain, a diminished range of motion, and crepitus and can also contribute to the development of mental disorders2. Knee joint OA may lead to abnormalities in gait, while hip joint OA can impact posture and, in the case of hand OA, result in the formation of osteophytes.
A majority of individuals with OA often contend with mental health challenges, including depression and anxiety, experiencing a decline in quality of life. Additionally, they face physical impediments such as challenges in performing activities of daily living and increased susceptibility to falls. Persistent pain and stiffness may also give rise to potential substance abuse issues3,4. The enduring pain and discomfort associated with knee OA, coupled with the consequential restrictions on physical activity, are significant contributors to the development of mental health conditions like depression and anxiety5. The continuous struggle with performing everyday tasks, coupled with a reduction in mobility, can induce feelings of despair, helplessness, and hopelessness, impacting individuals’ psychological well-being substantially. The chronic progression of knee OA often requires enduring and multifaceted management strategies, including lifestyle modifications, medication regimes, and possibly surgical interventions6. The ongoing nature of these interventions can be mentally taxing and frustrating, leading to heightened stress and potential exacerbation of existing mental health conditions. The limitations imposed by the condition can also lead to social isolation, which can further intensify feelings of loneliness and depression, creating a vicious cycle of physical pain and mental anguish.
Moreover, persistent pain and the ongoing need for management can sometimes lead to sleep disturbances, further impacting mental health and overall quality of life. The struggle with disrupted sleep can lead to heightened irritability, diminished cognitive function, and exacerbated feelings of anxiety and depression7. Understanding the interplay between mental health conditions such as depression, stress, anxiety, and knee OA is crucial for optimizing patient care and improving the overall quality of life.
Several studies have explored the relationship between mental health conditions such as depression, stress, and anxiety and their prevalence among patients with knee OA8–11. Studies indicate a significant relationship between mental health issues, particularly depression, and knee OA. A systematic review highlighted that depression is strongly associated with knee pain, while anxiety showed limited evidence of a relationship, and poor mental health showed minimal evidence of a connection with knee pain12. Studies have shown that psychological functioning plays a crucial role in knee pain, with higher pain levels correlating with an increased likelihood of anxiety and depression12,13. Additionally, there is evidence that depression can worsen arthritis symptoms, lower pain thresholds, and lead to more functional limitations, affecting treatment adherence and overall health outcomes14.
The current published studies have reported the prevalence of mental illness in OA patients15–19. However, it varies substantially between investigations. Therefore, this systematic review is conducted to synthesize existing research to determine the prevalence of these mental health conditions in individuals suffering from knee OA.
Materials and methods
The present systematic review has been conducted following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and registered with PROSPERO under the registration number CRD42023469320 (Supplementary Table S1, Supplemental Digital Content 1, http://links.lww.com/MS9/A535).
Inclusion and exclusion criteria
We included studies that report on the prevalence of mental health issues in individuals with knee OA, encompassing both observational studies and clinical trials. Studies focusing on other forms of arthritis or OA manifesting in joints other than the knee were also excluded to maintain specificity. Inclusion was limited to preprints and articles published in English, but no restrictions were placed on geographical location or research environment, allowing for a broad range of studies. Detailed inclusion and exclusion criteria are enlisted in Supplementary Table S2 (Supplemental Digital Content 1, http://links.lww.com/MS9/A535).
Search strategy and screening
A comprehensive literature search was conducted up to September 15, 2023, utilizing several prominent databases, including PubMed, EMBASE, Scopus, and Web of Science. The search strategy implemented involved a combination of keywords and synonyms related to knee OA and mental illnesses. Additionally, manual searches were performed in Google Scholar and other preprint platforms to find additional relevant articles. No restrictions were placed on the year of publication, ensuring an inclusive collection of available literature. Detailed information about the search strategy and the specific keywords and terms used is delineated in Supplementary Table S3 (Supplemental Digital Content 1, http://links.lww.com/MS9/A535).
After acquiring search results, duplicate entries were diligently eliminated, and Mendeley was deployed as a reference management tool to organize the accumulated references systematically. The ensuing initial screening process was collaboratively undertaken by two independent researchers utilizing Rayyan software, a tool designed to facilitate the early stages of systematic review preparation20,21. Both researchers, working independently, scrutinized the titles and abstracts of each retrieved study to exclude those deemed irrelevant to the review’s focus. Following this, an examination of the full texts of the shortlisted studies was conducted to assess their compliance with the inclusion criteria. In cases of discrepancies or differing opinions concerning a study’s eligibility, the input of a third independent researcher was sought to resolve any disagreements.
Data extraction
Three reviewers meticulously extracted data from the selected studies to ensure accuracy and thoroughness. The information extracted from each study included the first author’s name, the country where the study was conducted, the publication year, demographic details, total sample size, type of mental issue, criteria for diagnosing the mental issue, and the number of patients.
Quality assessment
The quality of the included studies was assessed using a modified version of the Newcastle–Ottawa Scale, ranging from 0 to 6, which was employed since the outcome of concern is prevalence22–25. The Cochrane RoB 2 tool was used for randomized controlled trials (RCTs)26,27. A study garnering a higher score was deemed to possess superior methodological quality and presented a lower risk of bias28. This meticulous approach to data extraction and quality assessment ensures the reliability and robustness of the findings derived from the reviewed studies.
Statistical analysis
A random-effects model was utilized to compute the pooled prevalence of mental health conditions in knee OA patients to accommodate the potential variations between the included studies. This model is advantageous as it accounts for the anticipated heterogeneity across studies, offering a more reliable and encompassing estimation of overall prevalence. The number of patients diagnosed with mental illness (events) and total sample size were taken to determine the pooled prevalence24,29. The extent of heterogeneity, or variability in results across different studies, was quantified using I 2 and tau-squared statistics30. I 2 values of 25, 50, and 75% typically represent ‘low,’ ‘moderate,’ or ‘high’ heterogeneity31. A predefined significance level was established to assess the statistical significance of the observed heterogeneity. Conventionally, a P value of less than 0.05 indicates statistical significance. The tau-squared value was calculated employing the maximum likelihood estimator. Additionally, sensitivity analyses and influencer diagnostic analyses were conducted to scrutinize the robustness and reliability of the results. All statistical analyses were conducted using R software, version 4.2.332.
Results
Literature search outcomes
A total of 12 846 records were screened from various databases, and an additional four records were found through a citation search. After primary screening, 815 articles were assessed for eligibility through full-text screening, during which 802 were excluded for various reasons. Ultimately, 14 articles met our criteria for inclusion, with 13 of these included in the meta-analyses. The screening and selection of articles are presented in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram (Fig. 1).
Figure 1.
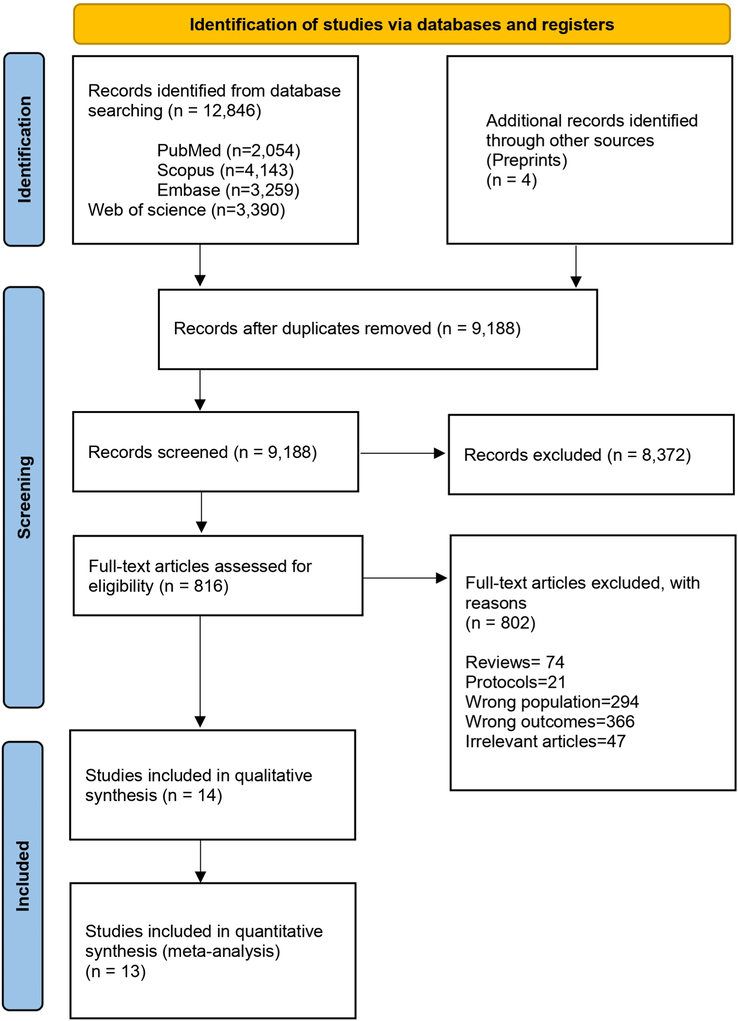
PRISMA flow diagram depicting the screening and selection process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Characteristics of included studies
The characteristics of the included studies are given in Table 1. The included studies span a variety of countries and regions, including Pakistan15, Taiwan33, India16, the Netherlands34, Canada19,35, Korea18,36, the USA37, China9,38,39, Japan17, and Turkey40, reflecting a diverse and comprehensive range of demographics and cultural contexts. The mean age of participants across the studies varied, ranging from 45 to 70.91 years, primarily focusing on middle-aged to elderly populations, which is pertinent given the increased prevalence of knee OA in these age groups. The study designs were diverse, incorporating cross-sectional studies, prospective observational studies, retrospective studies, a population-based cohort, and results from a RCT, enabling the synthesis of findings from varied methodological approaches. The proportion of male participants in the studies varied significantly, with some studies not reporting sex-specific data. Regarding the clinical outcomes, the total number of patients with knee OA and the number of participants developing mental illnesses like depression, anxiety, and stress were reported, with varying prevalence rates observed across different studies. Several different scales were employed to measure mental illness across the studies, including the Beck Depression Inventory (BDI), the Geriatric Depression Scale (GDS), the Hospital Anxiety and Depression Scale (HADS), patient self-reported depression, the Center for Epidemiologic Studies Depression Scale (CES-D), and the Patient Health Questionnaire-9 (PHQ-9).
Table 1.
Characteristics of included studies
| Study | Country | Study design | Mean age | Male % | Total no of patients with knee OA | No. of individuals with mental illness | Scale used to measure mental illness |
|---|---|---|---|---|---|---|---|
| Aqeel et al. 202115 | Pakistan | Cross-sectional study | 55 | 57.6 | 250 | Depression=232 | BDI |
| Chen et al. 201933 | Taiwan | Prospective cohort study | 70.91 | 27.5 | 102 | Depression=4 | GDS |
| Dhaon et al. 201916 | India | Cross-sectional study | NA | 67 | 100 | Depression=19 | HADS |
| Duivenvoorden et al. 201334 | Netherlands | Prospective cohort study | 66.2 | 43.7 | 128 | Anxiety=29, depression=26 | HADS |
| Gandhi et al. 201535 | Canada | Prospective cohort study | 64.7 | 43 | 475 | Depression=58 | Patient self-reported depression |
| Iijima et al. 201817 | Japan | Cross-sectional study | 74.8 | 32.6 | 95 | Depression=43 | GDS |
| Lee et al. 202036 | Korea | Retrospective cross-sectional study | 65.1 | 27.7 | 1157 | Anxiety=331 Depression=283 Stress=370 |
CES-D |
| Lee et al. 202218 | Korea | Prospective cohort study | 70.7 | 10.8 | 106 | Depression=18 | PHQ-9 |
| Possley et al. 200937 | USA | Prospective cohort study | 65.9 | NA | 105 | Depression=44 | CES-D |
| Sayre et al. 202019 | Canada | Population-based cohort study | 55 | NA | 122 | Anxiety=32, Depression=25 | HADS |
| Wong et al. 20159 | China | Cross-sectional study | 65 | NA | 115 | Psychiatric morbidity=45 | HADS |
| Yilmaz et al. 201540 | Turkey | Prospective cohort study | 45 | NA | 139 | Depression=44 | BDI |
| Zheng et al. 202138 | China | Results from RCT | 63.3 | NA | 397 | Depression=101 | PHQ-9 |
| Zheng et al. 202239 | China | Cross-sectional study | 69.2 | NA | 214 | Depression=94 | GDS |
BDI, Beck Depression Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; GDS, Geriatric Depression Scale; HADS, Hospital Anxiety and Depression Scale; PHQ-9, Patient Health Questionnaire; RCT, randomized controlled trial.
Quality assessment
The quality assessment of the included studies revealed a variation in scores. Four studies received a score of 3, five studies scored 4, two scored 5, and two achieved a score of 6. The RCT also showed a low risk of bias. The overall quality of the included studies can be characterized as moderate to high (Supplementary Table S4, Supplemental Digital Content 1, http://links.lww.com/MS9/A535).
Data synthesis
Depression
A total of 13 studies reported on the prevalence of depression among patients with knee OA15,16,18,19,33–40. These studies encompassed 3390 patients, from which a pooled prevalence of 30% [95% confidence interval (CI): 18–43] for depression was observed. The heterogeneity was significant, I 2=98%. Figure 2 presents the forest plot illustrating the pooled prevalence of depression.
Figure 2.
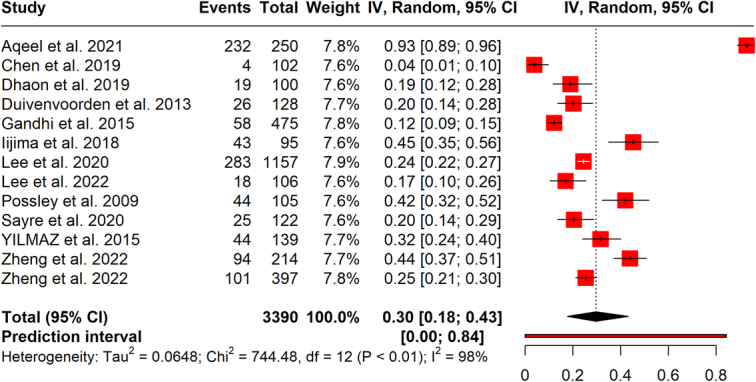
Forest plot illustrating the pooled prevalence of depression.
Anxiety
Three studies reported anxiety in knee OA patients19,34,36. A pooled prevalence of 27% (95% CI: 24–30) was found for anxiety from a total of 1407 patients. Heterogeneity was found to be low, with I 2=7%. Figure 3 shows the pooled prevalence of anxiety among knee OA patients.
Figure 3.
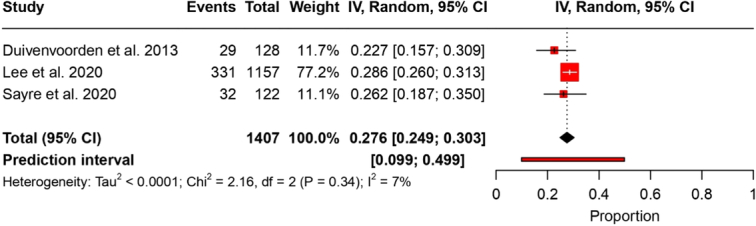
Forest plot illustrating the prevalence results of anxiety.
Subgroup analysis
Given the marked heterogeneity among the studies, we conducted a subgroup analysis based on the study design and the various scales used to assess depression.
Based on assessment scales
Two studies involving a total of 381 patients utilized the BDI, unveiling a pooled prevalence of 66% (95% CI: 0.66–1.00) for depression, with a high I 2 of 99%, indicating significant heterogeneity. The GDS was employed in three other studies with 411 patients, yielding a pooled prevalence of 28% (95% CI: 5–60) and a similarly high heterogeneity (I 2 of 99%). Three studies that involved 350 participants used the HADS, demonstrating a pooled prevalence of 20% (95% CI: 0.15–0.24) for depression, with no observed heterogeneity (I 2=0%). The CES-D was applied in two studies, comprising 1262 patients, and revealed a pooled prevalence of 32% (95% CI: 0.16–0.50) with substantial heterogeneity I 2 of 93%. The PHQ-9 scale was used in two studies with 503 patients and showed a pooled prevalence of 22% (95% CI: 0.14–0.30) for depression, with a moderate heterogeneity I 2 of 71%. A single study, which relied on patient-reported criteria and included 475 patients, indicated a 12% (95% CI: 0.14–0.30) prevalence of depression among patients with knee OA. The outcomes of these subgroup analyses, delineated by the varying diagnostic scales for depression, are illustrated in Figure 4.
Figure 4.
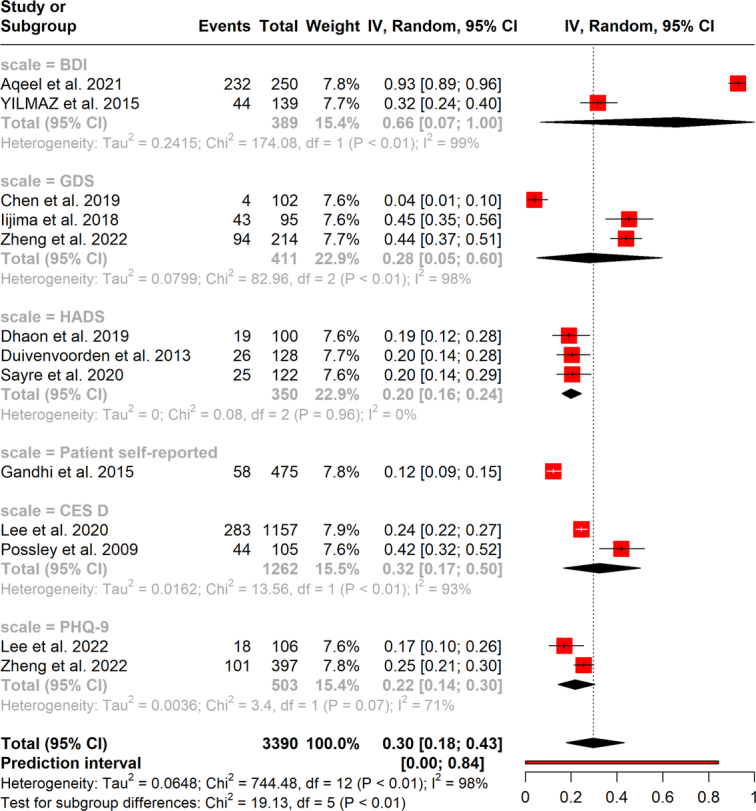
Forest plot depicting the results of subgroup analysis for the scale used to measure depression.
Based on the study design
Five cross-sectional studies involving 1816 patients found the prevalence of depression to be 46% (95% CI: 0.17–0.76). These studies had significant heterogeneity, with an I 2 of 99%. Conversely, seven cohort studies with 1177 participants reported a pooled prevalence of depression at 20% (95% CI: 0.12–0.29), and these studies also exhibited significant heterogeneity with an I 2 of 92% (Fig. 5).
Figure 5.
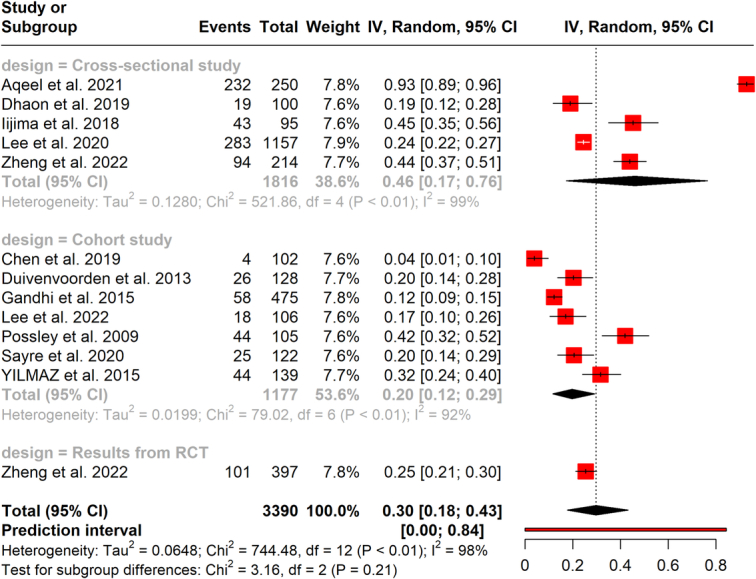
Results of depression subgroup analysis based on study design.
Psychiatric morbidity
Wong et al.9 reported psychiatric morbidity among OA patients. Of the 115 OA patients studied, 65 exhibited psychiatric morbidity.
Sensitivity analysis
We conducted several sensitivity analyses. The Baujat plots indicated that the study by Aqeel et al.15 contributed to heterogeneity and impacted the overall result for the prevalence of depression (Supplementary Fig. S1, Supplemental Digital Content 1, http://links.lww.com/MS9/A535). Similarly, influence analysis of pooled depression results15 affected the overall result (Supplementary Fig. S2, Supplemental Digital Content 1, http://links.lww.com/MS9/A535).
We performed a leave-one-out analysis, omitting one study at a time. Excluding the study by Aqeel et al. 15 reduced the prevalence of depression among knee OA patients to 24% (95% CI: 18–31); I 2=93% (Supplementary Fig. S3, Supplemental Digital Content 1, http://links.lww.com/MS9/A535).
Publication bias
Funnel plots were utilized to detect any presence of publication bias. Visual inspection of the funnel plot suggested some asymmetry. However, the Egger test indicated no publication bias (P=0.706) Supplementary Figure S4, Supplemental Digital Content 1, http://links.lww.com/MS9/A535 depicts the funnel plot.
Discussion
Our study was undertaken to evaluate the aggregated prevalence of mental illnesses, mainly focusing on patients with knee OA. We discovered a substantial prevalence of depression within this demographic, with 30% of the population being affected. However, a notable element in our findings was the presence of significant heterogeneity across the included studies. This heterogeneity may stem from the varied criteria employed by different studies to measure depression. Each study may have used distinct scales, methodologies, or thresholds to assess depressive symptoms, contributing to the variability in reported prevalence rates. It suggests that the observed prevalence of depression among knee OA patients may not be universally applicable due to differences in measurement approaches, and it underscores the need for standardized measurement techniques in future research to ensure comparability and reliability of findings. A previous systematic review also found similar results among general OA7. Their findings indicate that approximately 20% of individuals with OA exhibit significant levels of depressive symptoms, a pattern that aligns with observations within the rheumatoid arthritis demographic, where depression is reportedly prevalent.
Nonetheless, due to the scarcity of comparative studies, it remains undetermined whether individuals with OA have a heightened susceptibility to depressive symptoms compared to the broader population. Moreover, anxiety is present in nearly one-fifth of individuals with OA. However, the lack of comparative data makes it challenging to ascertain whether this proportion is higher than those without OA. The result of our subgroup analysis showed a varied prevalence of depression based on the study design. Cohort studies have shown a relatively lower incidence. One possible reason is differences in how depression is measured over time (longitudinal and cross-sectional) and potential errors introduced by the selection of study participants in cohort studies.
A prior study highlighted the relationship between deteriorated indicators of mental well-being and the incidence and risk of pain flare-ups related to OA. The overall state of mental health, being an adjustable aspect of health, could potentially introduce a novel pathway for averting episodes of pain associated with OA8. Aqeel et al. 15 indicate that there is a positive correlation between the perception of knee OA and depression. However, no significant correlation was found between the perception of knee OA and pain, anxiety, and positive and negative effects. Additionally, relationships were identified among pain, anxiety, depression, and affected knee OA patients. Existing literature consistently suggests an interplay between depressive symptoms and the development of musculoskeletal pain. Patients with OA who experience symptoms of depression often experience increased functional limitations and increased pain, which can lead to other psychological problems such as mood swings and reduced physical function that is already limited due to OA. The study underscores that the severity of OA pain intensifies with the manifestation of depression symptoms, possibly resulting in increased functional impairments. Another study by Chen et al. 33 illustrates that in elderly patients with knee OA who underwent intraarticular hyaluronic acid (IAHA), knee pain, and depression were the predominant factors adversely impacting patient-reported knee functional outcomes.
Furthermore, it was established that age correlates with suboptimal patient-reported functional outcomes post-IAHA. Additionally, patients with a higher radiographic Kellgren and Lawrence grade (grade 3) exhibited significantly more depression and poorer knee functional outcomes compared to those with a lower radiographic OA grade (grade 2), both initially and across a 6-month longitudinal follow-up post-IAHA. Duivenvoorden et al. 34 unveiled a high prevalence of anxiety and depressive symptoms among individuals with end-stage hip and knee OA. Both groups observed a notable decline in the prevalence of these psychological symptoms postsurgery. The existence of preoperative depressive symptoms forecasted a diminished patient-reported outcome postsurgery for both hip and knee patients. Those who experienced preoperative anxiety or depressive symptoms reported lower satisfaction levels after the surgery. The hypothesis stemmed from the intricate link between psychological symptoms and pain and disability, leading us to anticipate a high prevalence of psychological symptoms in patients with end-stage hip and knee OA. Preoperatively, depressive symptoms were more prevalent among hip OA patients compared to knee OA patients, potentially due to differences in their ability to carry out activities of daily living before the surgery. However, to substantiate this hypothesis, further research is essential.
The pronounced prevalence of depression and anxiety among patients with knee OA, as illuminated by our study and various others, underscores the imperative need for integrated healthcare approaches that amalgamate orthopedic and mental health interventions. Clinically, healthcare providers should be vigilant to the psychosocial dimensions of OA, incorporating routine screenings for depressive and anxiety symptoms, especially in those with advanced and end-stage OA. Early identification and management of these psychological morbidities can be pivotal in enhancing the overall quality of life and functional outcomes postintervention, such as surgery41,42. There is a manifest need to consider psychological well-being as an integral component of preoperative and postoperative care, addressing mental health concerns concurrently with physiological ones. For patients undergoing IAHA, particular attention to depressive symptoms and pain management can be decisive in optimizing patient-reported outcomes and postoperative satisfaction levels. Various types of interventions designed to mitigate the perception of pain are effective in patients with chronic pain43,44. The observed correlations between depression, pain severity, and functional restrictions accentuate the need for multidisciplinary approaches, enveloping psychological counseling, pharmacological interventions, and physical therapy, to address the multifaceted challenges faced by OA patients holistically. On a public health front, the insights gained from these studies spotlight the necessity for awareness campaigns to educate patients, caregivers, and healthcare providers about the intertwined nature of physical and mental health in chronic musculoskeletal conditions45. Developing robust, evidence-based guidelines and fostering research on standardized measurement techniques for mental health symptoms in OA patients are crucial steps in advancing understanding and care. These comprehensive strategies can facilitate the creation of a health ecosystem where the psychological ramifications of OA are recognized, addressed, and mitigated, fostering improved health outcomes and quality of life for the affected individuals.
Our study does present several limitations that warrant consideration. First, including only articles published in English potentially omits valuable insights from studies conducted in other languages, biasing our findings. Second, we could only find studies predominantly on depression and anxiety, thereby limiting the scope to understand the prevalence and impact of other forms of mental illnesses among individuals with knee OA. Additionally, the substantial heterogeneity and the variability in the criteria used to assess mental illness across different studies constrain the generalizability of our results. These variations might have influenced the aggregated prevalence rates and the overall conclusions drawn from our study. Therefore, our findings should be interpreted with caution, and it is imperative to conduct more inclusive and diversified research in this domain to substantiate and expand the understanding of the relationship between mental illnesses and knee OA. We could not perform subgroup analysis based on sex due to a lack of sufficient data. Future studies should focus on the effect of demographics (sex, age) on mental illness in this population. The development of standardized measurement techniques and criteria for assessing mental illness in this population would significantly enhance the reliability and comparability of future studies, paving the way for more comprehensive and nuanced insights.
Conclusions
The findings of this study indicate a significant prevalence of depression and anxiety among patients with knee OA. This highlights a compelling need for further research aimed at exploring the spectrum of mental health conditions prevalent within this population and identifying the contributory factors. It is critical to develop and implement comprehensive strategies that significantly enhance the mental well-being of individuals with knee OA. These interventions should prioritize both the prevention and active management of mental health conditions, integrating these efforts into the overall therapeutic plans for patients with knee OA. This integrated approach promises to improve holistic health outcomes and elevate the quality of life for this affected demographic.
Ethical approval
Ethics approval was not required for this systematic review.
Consent
Informed consent was not required for this systematic review.
Source of funding
No financial support received for the research, authorship, and/or publication of this systematic review.
Author contribution
M.O.O.: funding acquisition, resources, and supervision. All authors were involved in conceptualization, investigation and project administration, validation, visualization, writing-original draft, and writing-review and editing.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
Name of the registry: PROSPERO – for systematic review.
Unique identification number or registration number: CRD42023469320.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023469320.
Guarantor
Malik O. Oduoye.
Data availability statement
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Supplementary Material
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.lww.com/annals-of-medicine-and-surgery.
Published online 24 June 2024
Contributor Information
Borja Merry del Val, Email: borjamerry@gmail.com.
Saurin R. Shukla, Email: saurinshukla3003@gmail.com.
Malik O. Oduoye, Email: malikolatunde36@gmail.com;olihealthmagazinewestafrica@gmail.com.
Mugisha Nsengiyumva, Email: mnsengiyumva16@gmail.com.
Tadele Tesfaye, Email: ttadele500@gmail.com.
Wojciech M. Glinkowski, Email: wojciech.glinkowski@wum.edu.pl.
References
- 1.Sen R, Hurley JA. Osteoarthritis Treasure Island: Stat Pearls; 2022. [Google Scholar]
- 2.Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet 2005;365:965–973. [DOI] [PubMed] [Google Scholar]
- 3.Hurley MV, Mitchell HL, Walsh N. In osteoarthritis, the psychosocial benefits of exercise are as important as physiological improvements. Exerc Sports Sci Rev 2003;31:138–143. [DOI] [PubMed] [Google Scholar]
- 4.Park H-J, Lee S-K. The association between osteoarthritis and health-related quality of life in women aged 50 years and over using the Korea National Health and Nutrition Examination Survey (KNHANES) data. Korean J Health Educ Promot 2012;29:23–32. [Google Scholar]
- 5.Jung JH, Seok H, Kim JH, et al. Association between osteoarthritis and mental health in a Korean population: a nationwide study. Int J Rheum Dis 2018;21:611–619. [DOI] [PubMed] [Google Scholar]
- 6.Lee YC, Lu B, Bathon JM, et al. Pain sensitivity and pain reactivity in osteoarthritis. Arthrit Care Res 2011;63:320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stubbs B, Aluko Y, Myint PK, et al. Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing 2016;45:228–235. [DOI] [PubMed] [Google Scholar]
- 8.Wise B, Niu J, Zhang Y, et al. Psychological factors and their relation to osteoarthritis pain. Osteoarthr Cartil 2010;18:883–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong L-Y, Lo RY, Chiu C-K, et al. Prevalence of psychiatric morbidity in Chinese subjects with knee osteoarthritis in a Hong Kong orthopaedic clinic. East Asian Arch Psychiatry 2015;25:150–158. [PubMed] [Google Scholar]
- 10.Rani M, Sharma L, Advani U, et al. Acupressure as an adjunct to pharmacological treatment for depression, anxiety, and stress in patients with knee osteoarthritis. J Acupunct Meridian Stud 2020;13:129–135. [DOI] [PubMed] [Google Scholar]
- 11.Axford J, Heron C, Ross F, et al. Management of knee osteoarthritis in primary care: pain and depression are the major obstacles. J Psychos Res 2008;64:461–467. [DOI] [PubMed] [Google Scholar]
- 12.Phyomaung PP, Dubowitz J, Cicuttini FM, et al. Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskelet Disord 2014;15:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walter N, Hinterberger T, Szymanski D, et al. Psychological comorbidities in osteoarthritis in Germany. Sci Rep 2023;13:2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lwin MN, Serhal L, Holroyd C, et al. Rheumatoid arthritis: the impact of mental health on disease: a narrative review. Rheumatol Ther 2020;7:457–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aqeel M, Rehna T, Sarfraz R. The association among perception of osteoarthritis with adverse pain anxiety, symptoms of depression, positive and negative effects in patients with knee osteoarthritis: a cross-sectional study. J Pak Med Assoc 2021;71:645–650. [DOI] [PubMed] [Google Scholar]
- 16.Dhaon P, Khan H, Singh RR, et al. Depression in patients of primary knee osteoarthritis: a cross-sectional study. Indian J Rheumatol 2020;15:27–31. [Google Scholar]
- 17.Iijima H, Aoyama T, Fukutani N, et al. Psychological health is associated with knee pain and physical function in patients with knee osteoarthritis: an exploratory cross-sectional study. BMC Psychol 2018;6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee N-K, Won SJ, Lee J-Y, et al. Presence of night pain, neuropathic pain, or depressive disorder does not adversely affect outcomes after total knee arthroplasty: a prospective cohort study. J Korean Med Sci 2022;37:e309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayre EC, Esdaile JM, Kopec JA, et al. Specific manifestations of knee osteoarthritis predict depression and anxiety years in the future: Vancouver Longitudinal Study of Early Knee Osteoarthritis. BMC Musculoskelet Disord 2020;21:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016;5:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goel S, Shabil M, Kaur J, et al. Safety, efficacy and health impact of electronic nicotine delivery systems (ENDS): an umbrella review protocol. BMJ Open 2024;14:e080274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alqahtani JS, Oyelade T, Aldhahir AM, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PloS One 2020;15:e0233147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bushi G, Shabil M, Padhi BK, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hygiene 2023;118:1–11. [DOI] [PubMed] [Google Scholar]
- 24.Shabil M, Bushi G, Beig MA, et al. Cardiovascular manifestation in tuberculosis cases: a systematic review and meta-analysis. Curr Probl Cardiol 2023;48:101666. [DOI] [PubMed] [Google Scholar]
- 25.Bushi G, Shabil M, Padhi BK, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg 2024;118:1–11. [DOI] [PubMed] [Google Scholar]
- 26.Sterne JA, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing the risk of bias in randomised trials. BMJ 2019;366:4898. [DOI] [PubMed] [Google Scholar]
- 27.Alrahbeni T, Mahal A, Alkhouri A, et al. Surgical interventions for intractable migraine: a systematic review and meta-analysis. Int J Surg 2024. Article in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shabil M, Bushi G, Bodige PK, et al. Effect of fenugreek on hyperglycemia: a systematic review and meta-analysis. Medicina 2023;59:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bushi G, Padhi BK, Shabil M, et al. Cardiovascular disease outcomes associated with obstructive sleep apnea in diabetics: a systematic review and meta-analysis. Diseases 2023;11:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Langan D, Higgins JP, Jackson D, et al. A comparison of heterogeneity variance estimators in simulated random‐effects meta‐analyses. Res Synth Methods 2019;10:83–98. [DOI] [PubMed] [Google Scholar]
- 31.IntHout J, Ioannidis JP, Rovers MM, et al. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 2016;6:e010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swarup SS, Padhi BK, Satapathy P, et al. Cardiovascular consequences of financial stress: a systematic review and meta-analysis. Curr Probl Cardiol 2023;6:102153. [DOI] [PubMed] [Google Scholar]
- 33.Chen Y-P, Huang Y-Y, Wu Y, et al. Depression negatively affects patient-reported knee functional outcomes after intraarticular hyaluronic acid injection among geriatric patients with knee osteoarthritis. J Orthop Surg Res 2019;14:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duivenvoorden T, Vissers M, Verhaar J, et al. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthr Cartil 2013;21:1834–1840. [DOI] [PubMed] [Google Scholar]
- 35.Gandhi R, Zywiel MG, Mahomed NN, et al. Depression and the overall burden of painful joints: an examination among individuals undergoing hip and knee replacement for osteoarthritis. Arthritis 2015;2015:327161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee Y, Lee SH, Lim SM, et al. Mental health and quality of life of patients with osteoarthritis pain: the sixth Korea National Health and Nutrition Examination Survey (2013-2015). PLoS One 2020;15:e0242077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Possley D, Budiman-Mak E, O’Connell S, et al. Relationship between depression and functional measures in overweight and obese persons with osteoarthritis of the knee. J Rehabilit Res Dev 2009;46:1091–1098. [DOI] [PubMed] [Google Scholar]
- 38.Zheng S, Tu L, Cicuttini F, et al. Depression in patients with knee osteoarthritis: risk factors and associations with joint symptoms. BMC Musculoskelet Disord 2021;22:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zheng X, Wang Y, Jin X, et al. Factors influencing depression in community-dwelling elderly patients with osteoarthritis of the knee in China: a cross-sectional study. BMC Geriatr 2022;22:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yilmaz H, Karaca G, Demir Polat HA, et al. Comparison between depression levels of women with knee osteoarthritis, rheumatoid arthritis, and fibromyalgia syndrome: a controlled study. Turk J Phys Med Rehab 2015;61:197–202. [Google Scholar]
- 41.Shabil M, Murti K, Kumar VU, et al. Older PLHIV are at higher cardiovascular risk with poor quality of life. Curr HIV Res 2023;21:354–360. [DOI] [PubMed] [Google Scholar]
- 42.Shabil M, Kumar VU, Dhingra S, et al. Current scenario and strategies to tackle cardiovascular disease risk in HIV geriatrics. Curr Pharmacol Rep 2023;9:523–539. [Google Scholar]
- 43.Basile G. Beneficial effects of music in the healing process of traumatic injuries: perceptual control of suffering and possible abatement of disability conditions. Clin Ter 2023;174:531–536. [DOI] [PubMed] [Google Scholar]
- 44.Majeed MH, Ali AA, Sudak DM. Mindfulness-based interventions for chronic pain: Evidence and applications. Asian J Psychiatr 2018;32:79–83. [DOI] [PubMed] [Google Scholar]
- 45.Shabil M, Satapathy P, Kabir R, et al. Shigellosis in Sweden: a public health concern. Clin Infect Pract 2023;17:100221. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


