Abstract
Introduction: The facial bones are prone to severe injuries due to high exposure and the labile nature of the bones, and they are injured in a significant proportion of trauma patients. Varying from simple, common nasal fractures to communited fractures of the face, management of such injuries can be extremely challenging due to fact that these injuries involve a highly vascular zone with proximity to the airway. In spite of being very well trained in surgeries of face and head neck area, with the exception of nasal bones, not many ENT surgeons in India perform facial bone fracture surgeries. Objective: This questionnaire-based study was planned to explore this key issue to understand as why many ENT surgeons do not perform facial trauma surgeries. Method: A cross-sectional questionnaire-based study was conducted over a period of 2 months Responses were obtained from ENT surgeons across various social groups on a Google Form-based questionnaire. The answers were collected and analysed. Result: A total of 240 valid responses were obtained. Most (56.7%) of the ENT surgeons had more than 15 years of practice. Around half (52%) of surgeons never did facial trauma surgery, and 65% of respondents replied that the main reason for their lack of involvement in facial trauma surgery was that they had no exposure to it during postgraduate training. The majority (65%) also wanted to enter this subspeciality if given a chance. Conclusion: To develop facial trauma management as a subspeciality in ENT, more and more ENT departments in medical colleges should include these surgeries as part of their training programmes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-024-04604-z.
Keywords: Maxilla-facial Trauma, Facial Trauma, ENT, Otorhinolaryngologist
Introduction
Facial bone injuries are prone to severe injuries due to high exposure and the labile nature of bones, and form a significant proportion in trauma patients. The number of facial bone injuries is continuously on rise due to a rise in road traffic accidents [1]. Varying from simple, common nasal fractures to communited fractures of the face, management of such injuries can be extremely challenging. Injuries of this highly vascular zone are complicated by the presence of the upper airway and proximity to the cranial and cervical structures that may be concomitantly involved [2].
Due to the complexity of this area and the nature of injuries itself, the treatment of facial trauma is a demanding aspect of the surgical specialities dealing with these patients. The common specialities treating facial trauma injuries are plastic surgeons, oral and maxillofacial surgeons, and ENT surgeons [3].
In spite of being very well trained in surgeries of the face, head, and neck area, with the exception of fractured nasal bones, not many ENT surgeons in India perform other facial bone fracture surgeries. Thus, this questionnaire-based study was planned to explore the key issues as to why many ENT surgeons do not perform facial trauma surgeries.
Methodology
A cross-sectional questionnaire-based study was conducted over a period of 2 months after obtaining institutional ethical clearance. The questionnaire was produced on Google Forms and circulated to various ENT groups in India on social media. The questionnaire began with an introduction about the details of the study and consent for participation.
There were total of four questions in the questionnaire Table 1. The first question was regarding the seniority of the ENT surgeon. The second question asked if the surgeon performs facial trauma surgeries. Nasal bone fracture reduction surgery was excluded as the majority of ENT surgeons do perform fracture nasal bone reduction. The third question asked why they think that few ENT surgeons perform facial trauma surgery, and the last question asked whether they are trained and, given the chance, would they be interested in performing such surgeries.
Table 1.
The questionnaire for the study
| Sr No | Questions | Response |
|---|---|---|
| 1 | Since how many years have you been in field of ENT? | (a) 5 (b) 5–10 (c) 10–15 d) > 15 |
| 2 | Do you perform facial trauma surgeries regularly (Not including fracture nasal bone)? |
(a) No (b) Yes (c) Rarely (d) With OMFS e) With plastic surgeon |
| 3 | Why do you think ENT surgeons don’t perform Facial trauma surgeries |
a) Not exposed in Post Graduation b) Not many cases seen in practice c) Too complicated surgeries d) Mostly done my OMFS e) Mostly done by Plastic surgeon f) Lack of interest |
| 4 | Given a chance will you like to do facial trauma surgeries |
a) Yes b) No c) May be d) I won’t but want other ENT to do pick this speciality |
Results
A total of 252 ENT surgeons responded to the questionnaire; however, a few of the responses were incomplete and were therefore removed. The 240 participants who completely filled the questionnaire were included in the study.
This data consisting of responses of 240 ENT surgeons was collected and summarised in an Excel spreadsheet.
The responses to Question One, which was regarding the seniority of the ENT surgeon, are shown in Fig. 1. The majority (56.7%) of surgeons had experience of more than 15 years and only 10% were those with less than 5 years of experience.
Fig. 1.
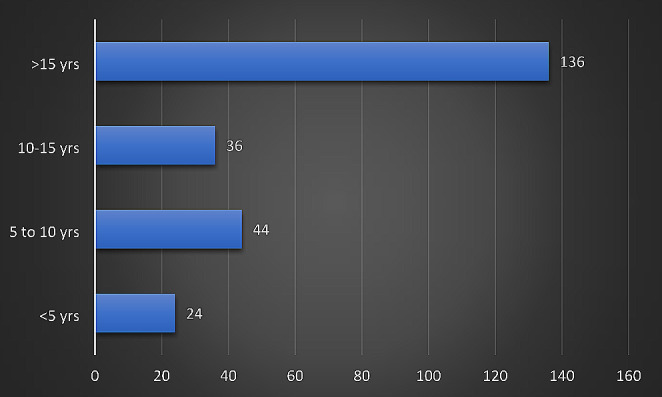
Seniority of ENT surgeons forming part of study
The response to Question Two, which asked whether the ENT surgeon performed facial trauma surgery (excluding fractured nasal bones) are shown in Fig. 2.
Fig. 2.

Proportion of ENT surgeons performing Facial Trauma Surgery
Question Three asked why the ENT surgeons felt that not many of them perform facial trauma surgery. This is as per Fig. 3. The total of this response is more than 100% because multiple options were allowed by one responder. Most (65%) responders agreed that they don’t perform facial trauma surgery as they were not exposed to it during postgraduate training, and 26% felt that most of these cases were done either by OMFS or plastic surgeons.
Fig. 3.

Responses as to why ENT surgeons don’t perform facial trauma surgery
Lastly, the response to the fourth question, which asked the responders whether, if given a chance, they would like to perform facial trauma surgeries. The response was as per Fig. 4. The majority (65%) of ENT surgeons showed interest in performing these surgeries if given a chance.
Fig. 4.

Given a chance, will you perform facial trauma surgeries?
Discussion
Patients with facial trauma must be well assessed so as to avoid any life- and sight-threatening injuries, functional problems, and cosmetic issues. These injuries are managed by a team of ENT surgeons, plastic surgeons, OMFS, and ophthalmologists [4]. A UK-based study by Rehman et al. [5] suggested that the majority of emergency physicians refer facial trauma injuries to the OMFS department.
This was a cross-sectional survey which aimed to understand why many ENT surgeons do not perform facial trauma surgeries. With many sub specialities branching out from the main subject of ENT, management of facial trauma has not been able to generate much of interest. To the best of our knowledge, this was the first such Indian study conducted to understand this topic. A study by Rios-Diaz et al. [6] in the US suggested that more plastic surgeons are taking care of facial trauma cases rather than ENT or OMFS.
The questionnaire was circulated in various ENT forums and surgeons were asked to fill in the Google Form. We included 240 ENT surgeons who completed the questions: 17 further responses were incomplete and were excluded from the study. Of those included, 56% were senior ENT surgeons with experience of more than 15 years.
Despite ENT surgeons being able to perform all of the complex surgeries in the ear, nose, throat, head, and neck, 10% of them actually performed facial trauma surgeries independently, and 52% never did these surgeries [7, 8, 9].
The third question asked the reason why many ENT surgeons did not venture in to facial trauma surgeries. The majority of them (65%) were not exposed to such surgeries during their postgraduate training and so never realised that this as part of ENT surgery. If ENT faculties in medical colleges started performing facial trauma surgeries and exposing postgraduates in this field, there is high chance that this sub-speciality may grow further in ENT.
A possible reason that this is not be taught in medical schools is that ENT surgeons may be less aware of terms such as occlusion, dental relations, intermaxillary fixations, and wiring. However, these are minor points that can be learnt from books, practice, and attending workshops.
Lastly, it was heartening to receive a positive response to the fourth question: if given a chance, 65% would be interested in this field and few very senior surgeons said that they would not venture into it, but wanted young surgeons to develop this subspeciality further.
It is logical that ENT surgeons should be more involved in facial trauma surgeries due to the fact that these injuries also commonly involve severe epistaxis and airway and laryngo-tracheal injuries, and ENT surgeons are well-versed in managing these areas. Studies also suggest more and more use of endoscopes in maxillo-facial injuries to reduce the hospital stay and improve functional and cosmetic outcomes, and ENT surgeons are familiar with the endoscopic anatomy of this area.
The practicing otolaryngologist frequently encounters consultations for injuries in the head and neck area. Restoration of form and function is essential for normal activities of daily living and quality of life. ENT surgeons should be well-versed in managing facial trauma cases. It is medicolegally also apt that ENT surgeons do this surgery as it is part of the national ENT curriculum and of standard textbooks.
Conclusion
The results of this questionnaire-based study show that the main reason why many ENT surgeons do not perform facial trauma surgery is that they have had no exposure during their residencies. At the same, time if given a chance, most of them would like to take up this subspeciality.
To make this sub-speciality of facial trauma develop in ENT, faculties in teaching schools should make a point to expose residents to such cases.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Declarations
Conflict of Interest
No financial Interest.
Institutional Ethical Clerance taken.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Singh V, Malkunje L, Mohammad S, Singh N, Dhasmana S, Das SK (2012) The maxillofacial injuries: a study. Natl J Maxillofac Surg 3(2):166–171. 10.4103/0975-5950.111372 10.4103/0975-5950.111372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jose A, Nagori SA, Agarwal B, Bhutia O, Roychoudhury A Management of maxillofacial trauma in emergency: an update of challenges and controversies. J Emerg Trauma Shock 2016 Apr-Jun ;9(2): 73–80. 10.4103/0974-2700.179456 [DOI] [PMC free article] [PubMed]
- 3.Bagheri SC, Dimassi M, Shahriari A, Khan HA, Jo C, Steed MB (2008) Facial trauma coverage among level-1 trauma centers of the United States. J Oral Maxillofac Surg 66(5):963–967. 10.1016/j.joms.2008.01.020 10.1016/j.joms.2008.01.020 [DOI] [PubMed] [Google Scholar]
- 4.Peeters N, Lemkens P, Leach R, Gemels B, Schepers S, Lemmens W (2016) Facial trauma. B-ENT Suppl 26(2):1–18 [PubMed] [Google Scholar]
- 5.Rehman U, Sarwar MS, Shafiq U, Brennan PA (2022) Facial trauma education within two English medical schools. Br J Oral Maxillofac Surg 60(6):817–822. 10.1016/j.bjoms.2021.12.003 10.1016/j.bjoms.2021.12.003 [DOI] [PubMed] [Google Scholar]
- 6.Rios-Diaz AJ, Kosyk MS, Cunning JR, Broach RB, Naga HI, Whitely C, Serletti JM, Swanson JW (2022) Does the geographical distribution of facial trauma surgeons correspond to facial trauma burden? A nationwide population-level analysis. J Craniofac Surg 33(4):997–1002. 10.1097/SCS.0000000000008306 10.1097/SCS.0000000000008306 [DOI] [PubMed] [Google Scholar]
- 7.Filiaci F, Riccardi E, Ungari C, Rinna C, Quarato D (2013 Jul-Aug) Endoscopic approach to maxillo-facial trauma. Ann Ital Chir 84(4):371–376 [PubMed]
- 8.Prade V, Seguin P, Boutet C, Alix T (2014) Résultats Du traitement chirurgical assisté par endoscopie des fractures du condyle mandibulaire: étude rétrospective sur 22 patients [Outcome of endoscopically assisted surgical treatment of mandibular condyle fractures: a retrospective study of 22 patients]. Rev Stomatol Chir Maxillofac Chir Orale 115(6):333–342. 10.1016/j.revsto.2014.10.005. French 10.1016/j.revsto.2014.10.005 [DOI] [PubMed] [Google Scholar]
- 9.Kelts GI, Newberry TR (2023) Current trends in head and neck trauma. Otolaryngol Clin North Am 56(4):791–800. 10.1016/j.otc.2023.04.011 10.1016/j.otc.2023.04.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


