Abstract
Situs inversus, an uncommon disorder, causes the orientation of asymmetric organs to be opposite to that of normal anatomy. It can be either partial, affecting only the thoracic or abdominal cavities, or full, involving the transposition of both the thoracic and abdominal organs. A 31-year-old Ethiopian male patient presented with migratory abdominal pain in the left lower quadrant for 3 days. Associated with the pain, he experienced symptoms of nausea, vomiting of ingested matter, and loss of appetite. Investigations were consistent with left-sided appendicitis with situs inversus totalis. Therefore, the patient was operated on and discharged with no perioperative complications. Appendicitis is a rare cause of left lower quadrant pain. In order to reduce the delay in patient treatment and avoidable perioperative complications, emergency physicians, radiologists, and surgeons must become more knowledgeable about situs inversus and left side appendicitis.
Keywords: Acute appendicitis, perforation, situs inversus totalis, case report
Introduction
Acute appendicitis (AA) is the most frequently encountered intraabdominal condition that necessitates emergency surgery. It is a common disorder in both the adult and pediatric populations, typically manifesting between the ages of 10 and 20 years, with a lifetime risk of 8.6% for males and 6.7% for females, respectively. 1 The diagnosis of this condition is established based on well-established clinical symptoms, fundamental radiologic findings, and surgical evaluation. 2 The appendix vermiformis, being capable of occupying various positions within the abdomen, including retrocecal, pelvic, subcecal, preileal, and postileal, can cause pain that is localized outside of the right lower quadrant in approximately one-third of patients with AA. Less commonly, subhepatic, meso-celiac, mid-inguinal, and left-sided pain can also be experienced. 3 Acute perforation of the appendix is a serious complication of appendicitis that is associated with increased morbidity and mortality. Risk factors for perforated appendicitis encompass extremes of age, male gender, pregnancy, immunosuppression, concurrent medical conditions, and prior abdominal surgeries. 4
In rare cases, appendicitis can affect the left lower quadrant due to congenital anomalies such as a genuine left-sided appendix or an unusual presentation of a right-sided appendix that extends into the left lower quadrant. 5 The diagnosis and treatment of individuals with left-sided AA can be complicated by the presence of anatomical abnormalities such as situs viscerum inversus totalis (SIT) and midgut malrotation (MM) or by syndromic conditions like Kartagener’s syndrome. 6 To diagnose AA in patients with SIT or MM, various methods can be employed, including physical examination, electrocardiogram (ECG), chest X-ray, barium tests, ultrasonography (USG), computerized tomography scan, and diagnostic laparoscopy. 7 Research studies have shown that the incidence of AA in SIT cases ranges from 0.016% to 0.024%. 8 Here, we present a case of perforated appendicitis in a patient with SIT.
Clinical presentation
A 31-year-old Ethiopian male patient who presented with abdominal pain initially located in the periumblical area but later shifted to the left lower quadrant for 3 days duration. Along with the pain, he experienced symptoms of nausea, vomiting of ingested matter, and loss of appetite. The patient denied any history of previous abdominal surgery, medical illnesses, or trauma to the abdomen. He reported being a social drinker but had no previous history of similar illnesses, diabetes, hypertension, or asthma.
During the examination, the patient’s vital signs were within the normal range, including a blood pressure of 125/81 mmHg, a temperature of 36.9°C, a pulse rate of 82 beats per minute, and a respiratory rate of 14 breaths per minute. On chest examination, normal heart sounds (S1 and S2) were heard on the right side. Abdominal examination revealed direct tenderness and rebound tenderness in the left lower quadrant. Laboratory tests showed a high hematocrit level of 56, a white blood cell count of 17,300 with 87.3% neutrophilia, and a platelet count of 416,000/mcl of blood.
Therefore, an abdominal USG examination and a chest x-ray were ordered. The chest x-ray showed dextrocardia (Figure 1). The results of the USG showed that the liver was located on the left side of the abdomen, the spleen was on the right side, and the appendix was enlarged with an edematous wall. The diameter of the appendix was measured to be 9 mm, and it was noncompressible at gentle probe pressure. The location of the appendix was in the left lower quadrant. However, there was no free intraperitoneal fluid collection observed. Based on these findings, the diagnosis was left-sided AA with situs inversus.
Figure 1.
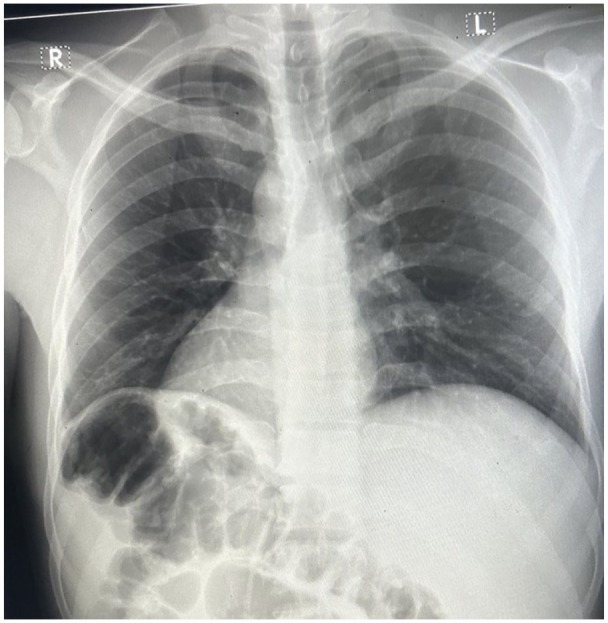
A chest x-ray of the patient showing dextrocardia.
Subsequently, a contrast-enhanced computed tomography (CT) scan of the abdomen was performed, which confirmed the diagnosis of left-sided AA with situs inversus (Figures 2 and 3). Therefore, for the diagnosis of left-side perforated appendicitis, an emergent laparotomy was performed. During the surgery, it was discovered that the liver was located on the left side of the abdomen and the spleen was on the right side. The appendix was found on the left side, and it had perforated at the middle third, forming adhesion with the greater omentum (Figure 4 and supplemental material video 1 (https://gemoo.com/tools/upload-video/share/656591234037886976?codeId=Mpm4yVbxa7l3o&card=656591229910700032&origin=videolinkgenerator)). An appendectomy was performed, and the peritoneum was washed with warm, normal saline. The fascia was closed, but the skin was left open for wound care.
Figure 2.
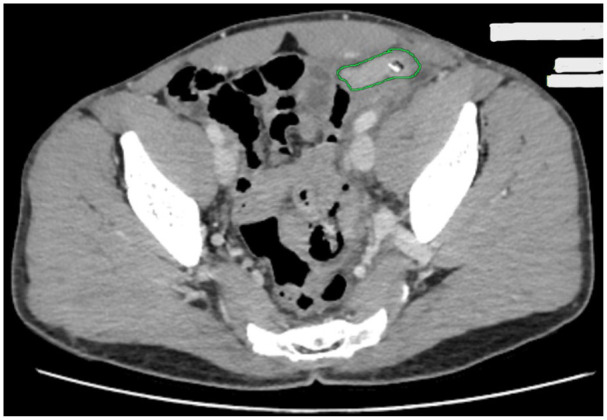
Axial computed tomography scan of the abdomen showing swollen appendix at the left lower quadrant of the abdomen.
Figure 3.

Abdominal computed tomography scan (coronal view) showing liver on the left upper quadrant and stomach and spleen on the right upper quadrant.
Figure 4.
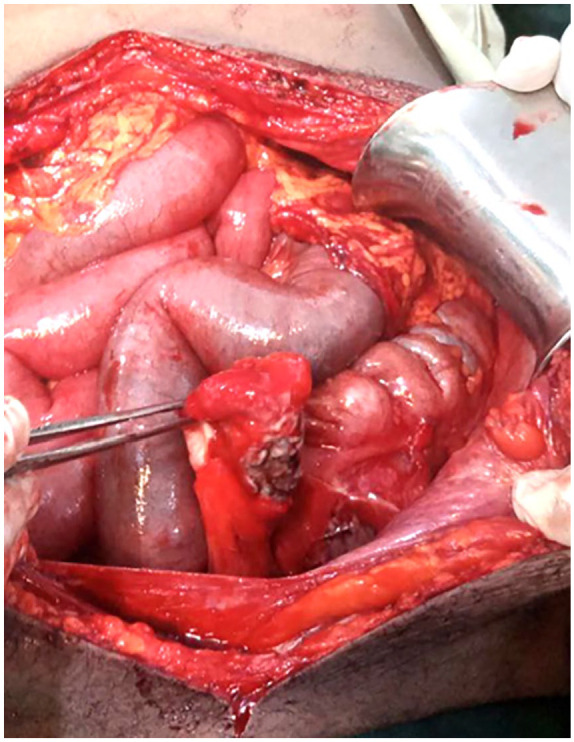
Intraoperative picture showing perforated appendix at the left lower quadrant of the abdomen.
After the surgery, the patient was extubated safely and transferred to the recovery area. The postoperative course was uneventful, and the patient showed improvement. He was discharged on the 6th postoperative day. The patient was followed up after discharge, and no complications were noted during the 3-week postoperative period.
Discussion
The conventional positioning of organs within the human body, known as situs solitus, dictates that the stomach and spleen reside on the left side of the abdomen, while the liver and gallbladder are situated on the right. Additionally, the heart is typically located on the left side of the thorax. 9 SIT, in which both the thoracic and abdominal organs are transposed in a mirror-image pattern, is an uncommon congenital anomaly. This condition represents a general defect in situs orientation, as it disrupts the normal left-right asymmetry and produces a range of laterality disturbances. 10 A series of signal molecules and genes collaborate to orchestrate the establishment of laterality during early development. Szenker-Ravi et al. have identified a group of genes responsible for encoding extracellular proteins that play a crucial role in determining the left-right axis in animal species possessing cilia in left-right organizers. Disruptions in these intricate processes can lead to heterotaxy, a condition characterized by abnormal development and organization of organs along the left-right axis, ranging from complete symmetry inversion to specific misarrangement of organs.11,12
Situs inversus causes the orientation of asymmetric organs to be opposite to that of normal anatomy. It can be either partial, affecting only the thoracic or abdominal cavities, or full, involving the transposition of both the thoracic and abdominal organs (SIT). 13 In a normal condition, the appendix is often found on the right side of the abdomen due to the natural 270° counterclockwise rotation of the abdominal organs during development. However, when the rotation is 270 clockwise, situs inversus occurs, resulting in a left-sided appendix.14,15 This condition poses challenges when performing therapeutic and diagnostic procedures. Due to its rarity, physicians, including radiologists, surgeons, and gastroenterologists, often have limited expertise in treating patients with situs inversus. It is an unusual occurrence that even a busy surgeon may encounter only once or twice in their lifetime. 16
AA often presents as pain in the right iliac fossa. However, around one-third of individuals with AA experience pain in other areas due to differences in the position of the vermiform appendix. 3 Various conditions, such as diverticulitis, renal colic, ruptured ovarian cyst, Meckel’s diverticulitis, epididymitis, incarcerated or strangulated hernia, bowel obstruction, regional enteritis, psoas abscess, and right- or left-sided appendicitis, can cause abdominal pain in the left lower quadrant.17,18 Due to inconsistent clinical findings, it can be difficult to differentiate LSAA from other conditions in an emergency situation, often resulting in a delayed diagnosis. 19 Imaging modalities, particularly CT scans, are highly effective in diagnosing this condition with precision and ease. CT imaging plays a pivotal role in the presurgical planning process, expediting the delivery of definitive treatment and guiding the primary clinical team in certain instances. 20
AA in patients with SIT or MM can be primarily diagnosed using abdominal ultrasound and CT scans. The physical examination may reveal the presence of right-sided heart sounds, tenderness in the left lower quadrant, a palpable liver edge on the left side, and the right testicle positioned lower than the left.2,7 Electrocardiography (ECG) can also be helpful, particularly in cases where dextrocardia is present. X-ray investigations were also useful in some instances, particularly in older patients, for identifying right-sided gastric bubbles and dextrocardia. In general, plain radiographs are not effective in diagnosing appendicitis. However, the presence of a right-sided gastric bubble on an abdominal X-ray and dextrocardia on a chest X-ray are extremely important indicators in identifying SIT. Currently, USG is frequently used to rule out AA, although it has some limitations, such as operator dependence and potential ineffectiveness in patients with a high body mass index. The sensitivity of a CT scan in diagnosing AA is 94%. 21 To accurately diagnose SIT, important indicators include a left-sided liver and a right-sided spleen and stomach. 22 Our patient was investigated with a chest x-ray, abdominal ultrasound, and abdominal CT scan. When faced with difficulties in diagnosing acute left lower quadrant discomfort, a barium enema with gastrografin can be utilized to potentially reveal MM or SIT. 23
Upon confirmation of the diagnosis of SIT with left-sided AA, the available surgical treatment options remain consistent with those typically employed for cases involving a normally positioned appendix. 7 AA can be treated with open or laparoscopic surgery. Our patient underwent open appendectomy, as we do not have a laparoscopy. However, treating AA with a laparoscopic appendectomy is a secure and efficient procedure as well. Laparoscopic appendectomy in SIT can be effectively conducted utilizing three ports; nevertheless, a universally accepted standard portal position has yet to be established. 24 This method offers numerous advantages over an open laparotomy. It has been associated with a decrease in postoperative complications, a shorter hospital stay, a reduction in psychological distress, and a faster recovery rate. 25
In cases where situs inversus is not identified preoperatively, laparoscopy provides the additional benefit of confirming the condition and enabling the surgeon to evaluate intra-abdominal tissues in case there are any doubts about the diagnosis. However, a few adjustments to the operating room setup and trocar placement are necessary for a successful procedure. Essentially, trocars can be inserted at various positions on the abdominal wall in accordance with the fundamental principle of laparoscopic triangulation, with the primary consideration being the surgeon’s ease of manipulation. Concurrently, the placement of ports is adjusted according to the patient’s specific medical circumstances and the precise location of the appendix as determined by imaging studies. 24 The monitor is positioned on the patient’s left side, while the surgeon and assistant stand on the right side of the patient. For an inexperienced surgeon, the reversed laparoscopic view may pose a technical challenge. In addition, handedness could influence the performance of the operation.26,27
Conclusion
In order to accurately diagnose left-sided AA, it is imperative to have a thorough understanding of the differential diagnoses of left lower quadrant abdominal pain and to maintain a high index of clinical suspicion. Utilizing imaging modalities such as ultrasound (USG), CT scans, and diagnostic laparoscopy can be used in establishing a precise and timely diagnosis. An open or laparoscopic appendectomy can be performed as a definitive treatment.
Supplemental Material
Supplemental material, sj-docx-1-sco-10.1177_2050313X241266522 for Left-sided perforated appendicitis in a patient with situs inversus totalis, a case report by Wondu Mekonnen Abebe, Deribe Mekonnen Workalemahu, Robera Amenu Leta, Mezgebu Alemnah Asefa, Hirut Tesfahun Alemu and Yohannis Derbew Molla in SAGE Open Medical Case Reports
Acknowledgments
None.
Footnotes
Author contributions: W.M.A. manuscript draft writing, and revision; D.M.W. Manuscript draft writing, and involved in the management of the patient; R.A.L. Manuscript revision and approval; M.A.A. Manuscript draft writing, and involved in the management of the patient; H.T.A. Manuscript revision and approval; Yohannis Derbew Molla: revision, and submission.
Availability of data and materials: The authors of this manuscript are willing to provide additional information regarding the case report.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Yohannis Derbew Molla  https://orcid.org/0000-0001-7881-0538
https://orcid.org/0000-0001-7881-0538
Supplemental material: Supplemental material for this article is available online.
References
- 1. Krzyzak M, Mulrooney SM. Acute Appendicitis review: background, epidemiology, diagnosis, and treatment. Cureus 2020; 12(6): e8562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Akbulut S, Caliskan A, Ekin A, et al. Left-sided acute appendicitis with situs inversus totalis: review of 63 published cases and report of two Cases. J Gastrointest Surg 2010; 14(9): 1422–1428. [DOI] [PubMed] [Google Scholar]
- 3. Hou SK, Chern CH, How CK, et al. Diagnosis of appendicitis with left lower quadrant pain. J Chin Med Assoc 2005; 68(12): 599–603. [DOI] [PubMed] [Google Scholar]
- 4. Balogun OS, Osinowo A, Afolayan M, et al. Acute perforated appendicitis in adults: management and complications in Lagos, Nigeria. Ann Afr Med 2019; 18(1): 36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Assefa MA, Molla YD, Yasin MO, et al. Left side perforated appendicitis with intestinal non-rotation: a case report. J Med Case Rep 2023; 17(1): 302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saliba C, Diab SH, Nicolas G, et al. Pitfalls of diagnosing left lower quadrant pain causes: making the uncommon common again. Am J Case Rep 2019; 20: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abdulla HA, Alqaseer A, Abushwemeh MA, et al. Left-sided acute appendicitis in a patient with situs inversus totalis. Cureus 2023; 15(4): e38105. https://www.cureus.com/articles/154238-left-sided-acute-appendicitis-in-a-patient-with-situs-inversus-totalis.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Di Buono G, Buscemi S, Galia M, et al. Acute appendicitis and situs viscerum inversus: radiological and surgical approach—A systematic review. Eur J Med Res 2023; 28(1): 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Deshimo G, Abebe H, Damtew G, et al. A case report of dextrocardia with situs inversus: a rare condition and its clinical importance. Case Rep Med 2024; 2024: 2435938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peeters H, Devriendt K. Human laterality disorders. Eur J Med Genet 2006; 49(5): 349–362. [DOI] [PubMed] [Google Scholar]
- 11. Sutherland: disorders of left–right asymmetry:. . . – Google Scholar, https://scholar.google.com/scholar_lookup?journal=American+Journal+of+Medical+Genetics+Part+C:+Seminars+in+Medical+Genetics&title=Disorders+of+left%E2%80%93right+asymmetry:+heterotaxy+and+situs+inversus&author=M.+J.+Sutherland&author=S.+M.+Ware&volume=151&issue=4&publication_year=2009&pages=307-317&doi=10.1002/ajmg.c.30228& (accessed 13 April 2024).
- 12. Szenker-Ravi E, Ott T, Khatoo M, et al. Discovery of a genetic module essential for assigning left-right asymmetry in humans and ancestral vertebrates. Nat Genet 2022; 54(1): 62–72. [DOI] [PubMed] [Google Scholar]
- 13. Akbulut S, Ulku A, Senol A, et al. Left-sided appendicitis: review of 95 published cases and a case report. World J Gastroenterol WJG 2010; 16(44): 5598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Patel RB, Bhadreshwara K, Hukkeri S. Laparoscopic appendicectomy in a patient with situs inversus totalis. Indian J Surg 2013; 75(S1): 41–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Versluis J, Suliman H. Appendicitis in a patient with situs inversus totalis. J Belg Soc Radiol 2014; 97(3): 182. [DOI] [PubMed] [Google Scholar]
- 16. Blegen HM. Surgery in situs inversus. Ann Surg 1949; 129(2): 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee MR, Kim JH, Hwang Y, et al. A left-sided periappendiceal abscess in an adult with intestinal malrotation. World J Gastroenterol WJG 2006; 12(33): 5399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Franklin ME, Jr, Almeida JA, Pérez ER, et al. Cholecystectomy and appendectomy by laparoscopy in a patient with situs inversus totalis. A case report and review of the literature. Rev Mex Cir Endoscópica 2001; 2(3): 150–153. [Google Scholar]
- 19. Ahmed JU, Hossain GM, Karim MM, et al. Left sided acute appendicitis with situs inversus in an elderly-an unusual case. J Chittagong Med Coll Teach Assoc 2007; 18(1): 29–31. [Google Scholar]
- 20. Hoang VT, Van HAT, Hoang TH, et al. Left-sided acute appendicitis with congenital gastrointestinal malrotation. JGH Open Open Access J Gastroenterol Hepatol 2022; 6(9): 647–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology 2006; 241(1): 83–94. [DOI] [PubMed] [Google Scholar]
- 22. Vettoretto N, Agresta F. A brief review of laparoscopic appendectomy: the issues and the evidence. Tech Coloproctol. 2011; 15(1): 1–6. [DOI] [PubMed] [Google Scholar]
- 23. Welte FJ, Grosso M. Left-sided appendicitis in a patient with congenital gastrointestinal malrotation: a case report. J Med Case Rep 2007; 1(1): 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hoang TV, Hoang HT, Vo HT, Chansomphou V. Laparoscopic appendectomy in an adult patient with situs inversus totalis. J Surg Case Rep 2023; 2023(3): rjad134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kumar S, Jalan A, Patowary BN, et al. Laparoscopic appendectomy versus open appendectomy for acute appendicitis: a prospective comparative study. Kathmandu Univ Med J KUMJ 2016; 14(55): 244–248. [PubMed] [Google Scholar]
- 26. Oms LM, Badia JM. Laparoscopic cholecystectomy in situs inversus totalis: the importance of being left-handed. Surg Endosc 2003; 17(11): 1859–1861. [DOI] [PubMed] [Google Scholar]
- 27. Di Buono G, Maienza E, Buscemi S, et al. Acute appendicitis in a patient with situs viscerum inversus totalis: role of laparoscopic approach. A case report and brief literature review. Int J Surg Case Rep 2020; 77: S29–S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sco-10.1177_2050313X241266522 for Left-sided perforated appendicitis in a patient with situs inversus totalis, a case report by Wondu Mekonnen Abebe, Deribe Mekonnen Workalemahu, Robera Amenu Leta, Mezgebu Alemnah Asefa, Hirut Tesfahun Alemu and Yohannis Derbew Molla in SAGE Open Medical Case Reports


