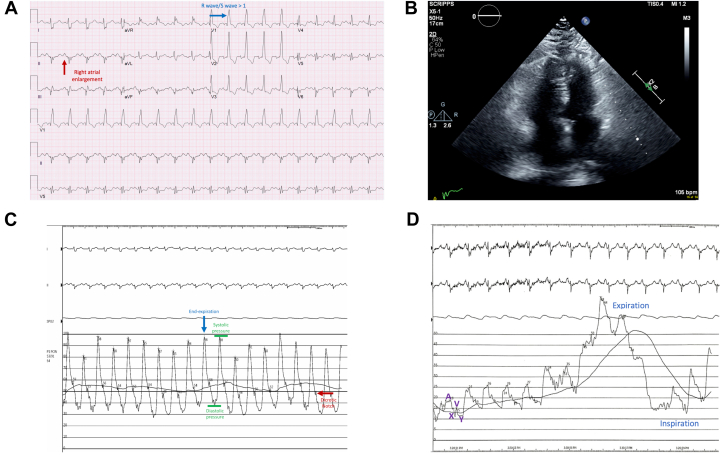
A 42-year-old woman described worsening chest pain and New York Heart Association II-III dyspnea. Her medical history included obesity, obstructive sleep apnea treated with continuous positive airway pressure, hypothyroidism, depression, and hypertension. Electrocardiogram showed sinus tachycardia with right heart strain (Figure 1A). Her brain natriuretic peptide level was 869 pg/mL. Chest x-ray revealed central pulmonary artery prominence. Echocardiogram showed an ejection fraction (EF) of 61% and peak estimated pulmonary artery (PA) pressure of 50 mm Hg. Right ventricle (RV) was dilated with decreased function (Figure 1B). She was taken for coronary angiography without significant epicardial coronary artery disease. Right heart catheterization showed right atrium (RA) 9 mm Hg, RV 94/7 mm Hg, PA 94/44 mm Hg with mean 62 mm Hg (Figure 1C), and mean pulmonary capillary wedge pressure 15 mm Hg (Figure 1D). A saturation run revealed RA 71%, RV 68.9%, and PA 70.4%. Arterial saturation was 94.5%, and her calculated pulmonary vascular resistance was 8 WU. She underwent computed tomography angiography of the chest, VQ scan, and lower extremity Doppler that showed negative findings for thrombus. Computed tomography of the chest showed a dilated main pulmonary artery of 4.0 cm and emphysema. Her final diagnosis was idiopathic pulmonary arterial hypertension.
Figure 1.
(A) Electrocardiogram showed sinus tachycardia with right heart strain, with an R wave–to–S wave ratio >1 in lead V1, right bundle branch block, and increased P wave amplitude in lead II from right atrial enlargement. (B) Echocardiogram apical 4-chamber view with an ejection fraction of 61%. The right ventricle is dilated with mildly decreased function. (C) Right heart catheterization showed elevated pulmonary artery pressures. Blue arrow, assess pressures at end-expiration, when intrathoracic pressure is closest to 0; green lines, systolic and diastolic pulmonary artery pressures; red arrow, The dicrotic notch occurs when the pulmonic valve closes at the start of diastole. (D) Right heart catheterization showed normal pulmonary capillary wedge pressures. A, X, V, and Y waves were present. Respiratory changes were present, so it is crucial to evaluate the respiratory cycle to capture accurate wedge pressures, particularly when diagnosing pulmonary hypertension.
Pulmonary hypertension (PH) is defined as mean PA pressure >20 mm Hg.1 Exertional chest pain can manifest from subendocardial hypoperfusion from high oxygen demand. Brain natriuretic peptide levels may be elevated from RV wall stretch. In patients younger than 60 years without structural left heart disease, there is low probability that left heart disease is sufficient to explain PH.2 A normal pulmonary capillary wedge pressure (≤15 mm Hg) is important to exclude postcapillary PH. In addition, an elevated pulmonary vascular resistance of ≥3 WU supports a diagnosis of precapillary PH.1 Her PH was also out of proportion to her lung disease. Further management included pulmonary vasodilator testing to determine responsiveness to calcium channel blockers.3 Although, initially, our patient’s hypertension and pulmonary disease supported other PH classifications, invasive hemodynamics ultimately diagnosed precapillary PH.
Acknowledgments
Declaration of competing interest
Dr. Srivastava serves on the advisory board for Medtronic and Abbott.
Ethics Statement
The case report has adhered to the relevant ethical guidelines with patient consent.
Pearls in Hemodynamics
-
1.
Pulmonary hypertension (PH) is defined as mean pulmonary artery pressure >20 mm Hg.
-
2.
A normal pulmonary capillary wedge pressure (≤15 mm Hg) is important to exclude postcapillary PH.
-
3.
An elevated pulmonary vascular resistance ≥3 WU supports a diagnosis of precapillary PH.
References
- 1.Simonneau G., Montani D., Celermajer D.S., et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53(1) doi: 10.1183/13993003.01913-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frost A., Badesch D., Gibbs J.S.R., et al. Diagnosis of pulmonary hypertension. Eur Respir J. 2019;53(1) doi: 10.1183/13993003.01904-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tonelli A.R., Alnuaimat H., Mubarak K. Pulmonary vasodilator testing and use of calcium channel blockers in pulmonary arterial hypertension. Respir Med. 2010;104(4):481–496. doi: 10.1016/j.rmed.2009.11.015. [DOI] [PubMed] [Google Scholar]