Abstract
The field of interventional cardiology (IC) has evolved dramatically over the past 40 years. Training and certification in IC have kept pace, with the development of accredited IC fellowship training programs, training statements, and subspecialty board certification. The application process, however, remained fragmented with lack of a universal process or time frame. In recent years, growing competition among training programs for the strongest candidates resulted in time-limited offers and high-pressure situations that disadvantaged candidates. A grassroots effort was recently undertaken by a Society for Cardiovascular Angiography & Interventions task force, to create equity in the system by establishing a national Match for IC fellowship. This manuscript explores the rationale, process, and implications of this endeavor.
Keywords: graduate medical education, interventional cardiology
Introduction
Training and certification in interventional cardiology (IC) have evolved since the first live demonstration courses held by Andreas Gruentzig more than 40 years ago. In 1999, several developments led to the formalization of IC training. These included the publication of the first IC advanced training statement developed by national cardiovascular societies, adoption of IC fellowship program accreditation, and recognition by the American Board of Internal Medicine (ABIM) of IC as a board-certified subspecialty. Since the practice pathway for certification closed in 2003, IC candidates desiring to qualify for board certification have trained in accredited programs. As a result, IC training programs now play a critical role in maintaining the IC workforce and high standards of care.
As IC training programs have proliferated and as the complexities and expectations required for competent care have risen, so too has the competition among training programs for the strongest fellowship candidates. While the number of programs and positions has increased over the years, the diversity in the applicant pool has remained low, and processes for fellow selection remain site-specific. In fact, over the past several years program directors and candidates found that the process has devolved, with wide variation in application timelines and on-the-spot offers, which disadvantage candidates and programs looking to interview a range of applicants.
The pressures and unfair features of the existing system were further fueled by the transition to virtual interviews related to the COVID-19 pandemic. With logistics of travel no longer a consideration, programs could commence interviews nearly immediately after the applications became available. This led to more candidates being interviewed in rapid succession, and a system evolved in which programs quickly assessed candidates, offered positions, and applied pressure for candidates to accept offers or be passed over for other candidates.
In response to the shortcomings of the current system, members of Society for Cardiovascular Angiography & Interventions (SCAI) were inspired to lead a grassroots educational campaign to organize IC program directors and the broader interventional community to commit to a regulated “Match” process under the established National Resident Match Program (NRMP). This manuscript provides an account of how this process unfolded and how a Match for IC fellowship was ultimately created.
The history of IC training
Following Andreas Gruentzig’s presentation of the first-in-human coronary angioplasty at the American Heart Association (AHA) Scientific Sessions in 1977, there was recognition of the potential efficacy of the procedure and the need to disseminate the new technique. Practicing cardiologists with prerequisite skills in performing diagnostic angiography who were interested in learning angioplasty attended a “Gruentzig Course,” where didactic lectures and live case demonstrations of percutaneous coronary intervention (PCI) comprised the curriculum. Course attendees returned to their home institutions, practiced and honed the newly learned techniques, developed skills, and then—in turn—became teachers for the next rounds of learners. This relatively informal process often involved periods of apprenticeship or observation and enabled the early growth and evolution of the IC.
Some institutions performed large volumes of PCI procedures, and selected cardiology fellows at these institutions had the opportunity to be proctored in the technical skills of PCI by faculty mentors in a process that comprised the first iteration of IC fellowship. In 1999, 2115 cardiology candidates who trained in PCI through this process were considered as having achieved from ABIM an “area of added qualification” in IC under the “practice pathway.” This designation required that the interventionalist had performed 500 PCI over the course of their career or 150 PCI over the prior 2 years.1 These clinicians were deemed eligible to take the newly developed board certification exam in IC and were “grandfathered” into board eligibility based on their procedural experience rather than specific training requirements.
In parallel, a task force established by the American College of Cardiology (ACC) in 1999 published an advanced training statement that identified the medical knowledge and clinical and technical skills required for competency in the practice of IC.2 This curriculum established standards for IC fellowship training and served as the blueprint for the ABIM IC certification examination, which was first offered that same year. Between 1999 and 2003, individuals who had met the requirements for certification through the “practice pathway” criteria were able to do so; but, thereafter, the ABIM adopted a formal subspecialty board certification process and closed the practice pathway. Starting in 2006, only individuals completing an accredited 12-month IC fellowship program and meeting designated procedural volume requirements were eligible for IC board certification.
Accreditation of IC fellowship programs
To prepare for the closing of the practice pathway, cardiovascular disease fellowship programs interested in offering formal training in IC had to identify subspecialty program directors and apply for accreditation from the Accreditation Council for Graduate Medical Education (ACGME) for a specific number of positions. The ACGME is a not-for-profit organization established in 1981 to ensure that training programs meet specialty-specific quality standards.3 The ACGME Review Committee for Internal Medicine accredited the first IC programs in 1999. ACGME requirements stipulate that fellowship programs must be 12 months in duration and provide prescribed volumes and varieties of procedures, an educational/didactic curriculum, and opportunities for research in an environment supportive of learning. The ACGME developed tools for categorizing and evaluating competencies in multiple domains critical for physicians. Programs are currently evaluated under the Next Accreditation System.4 In the current academic year (2023-2024), there are 180 accredited IC fellowship programs and 353 positions. IC ranks fourth among internal medicine subspecialties in terms of number of programs and eighth in terms of number of fellows.3 Of note, this underestimates the number of IC fellows, as they do not include fellows training at programs that offer IC training in nonaccredited fellowships—some of which are for advanced years beyond the ACGME IC fellowship and others that generally follow the ACGME pathway but do not offer accreditation.
A changing field prompts changes in fellowship training
In the nearly 25 years since the first IC program was accredited, the field has dramatically evolved. Despite declining coronary procedural volumes by operators in the US, the complexity of cases and patient risk profile have risen substantially.5, 6, 7 Additionally, the introduction of transcatheter valve technologies and structural heart interventions, the growing number of endovascular procedures for peripheral vascular disease, and further subspecialization in complex coronary intervention have expanded the spectrum of training in IC.8,9 Training programs are accredited for 1 year; however, there are growing differences among the programs in overall structure, with some programs offering 2 years of training to incorporate noncoronary areas of expertise, while others offer dedicated additional years of nonaccredited “sub” subspecialty training in structural, endovascular, or complex coronary interventions. To address training in the current era, the 2023 ACC/AHA/SCAI Advanced Training Statement in Interventional Cardiology10 was developed to provide a robust “roadmap” for training programs. The statement defines the required competencies, minimum procedural volume, core procedural interventional skills, and training standards for coronary, peripheral vascular, and structural heart interventions. Importantly, the document supports the 1-year format of the “core” IC fellowship for attainment of competency in coronary intervention with the option of added competency in limited specialty areas within peripheral vascular and structural interventions.
A flawed fellowship recruitment process prompts the need to institute a Match
To date, IC fellowship programs have not been required to conform to any formalized process for selection of fellowship candidates, which has resulted in significant variation across institutions regarding the application and interview process. From a programmatic perspective, each IC fellowship could establish its own recruitment process, deciding if and when to accept applications and whether and when to conduct interviews. Programs could determine their own timeframe in which to provide candidates with an offer for a fellowship position and how long to permit the candidate to consider the offer before providing a commitment to matriculate. Many, but not all, programs use the Electronic Residency Application Service (ERAS) to organize candidate portfolios. ERAS, a service of the Association of American Medical Colleges, facilitates and streamlines the application process for candidates, programs, program directors, and the authors of letters of recommendation. ERAS opens for candidate review in December of each year, providing a streamlined process for the upload, storage, and review of candidate applicant files. Some programs use their own institutional applications, whereas others do not require any formal application. Programs could recruit internal candidates to fill available training slots starting years in advance, they could compete for external applicants, or they could do both. Given the lack of standardization, programs have been free to offer positions at any time, resulting in significant variability in the application process.
From the applicant’s perspective, the lack of a structured timeline for the application process required candidates to make career decisions early in the first year of cardiovascular disease training and to compose their application materials 2 years in advance of starting IC training. With ERAS open to application submission in the fall of the second year for the December release to programs, fellows had limited time on clinical rotations to determine their interest and aptitude for IC. Additionally, letters of recommendation, written at this early stage, risked not being fully reflective of each candidate’s capacity to improve and develop the technical skills and clinical knowledge important for success in the field. There were other disadvantages to candidates in the existing system. Fellows at programs with an IC fellowship had an advantage of securing an internal spot but were often pressured to limit their exploration of the opportunities at other programs, potentially disadvantaging them in the long term.
Another problem with the existing system was that the pressure to recruit candidates on a tight timeline limited the opportunity to interview applicants from a wide variety and diversity of programs, potentially reducing the ability to recruit underrepresented candidates from varied programs. Despite an overall increase in the diversity of physicians entering the workforce,11 there has been little change in the applicant pool for IC over the years, with fewer than 5% of applicants self-reporting as Black race or Hispanic ethnicity and only 10% identifying as women.12
Competition among the programs, each vying for the seemingly strongest candidates, degenerated into a system that favored quick decision-making on the part of programs to offer positions as early as possible. The influence of the COVID-19 pandemic in 2020 and 2021 negatively impacted an already high-pressure application process, compounding its many weaknesses.13 Fellowship interviews were hosted virtually rather than in person, which enabled candidates to interview at a greater number of programs without the need to travel. In addition, the virtual format accelerated the tempo of an application process that was already felt to be too fast, resulting in an increase in so-called “exploding offers”—offers that required the accepted candidate to respond within a very short timeframe or risk losing the offer. This practice placed significant pressure on candidates to make quick decisions, often forcing them to determine whether to accept the offer from 1 institution before having the opportunity to participate in interviews with—let alone see and evaluate—other programs or fully understand the ramifications of accepting an offer on their personal lives. At the same time, the accelerated timetable left many programs scrambling to identify applicants, as the number of available candidates diminished rapidly due to applicants accepting time-sensitive, exploding offers.
2021 SCAI Fellows Course conversation, then the “Tweet Heard ‘Round the World”
As programs and applicants experienced these issues in real-time during the IC fellowship application season of Fall/Winter 2021, the challenging features of the recruitment and selection process reached a tipping point. Following extensive discussions at the 2021 SCAI Fellows Course, a poll was posted on Twitter by Dr Ajay J. Kirtane, interventional cardiologist and SCAI member, on December 17, 2021, entitled “Do we need an interventional fellowship Match?” The post garnered a great deal of attention—effectively a “Tweet heard ‘round the world”—and precipitated additional discussion in a large, national listserv comprising cardiac catheterization laboratory directors, fellowship directors, and SCAI leadership, escalating the discussion. Several key concerns were identified, including the cadence of the application season requiring submission of applications by fellows so early in cardiology fellowship, the accelerating timetable prompting programs to conduct interviews earlier each year to compete for the strongest candidates, and the problem of “exploding offers” to candidates with limited time to respond. These discussions, occurring in real-time in the middle of the fellowship selection process, resonated profoundly within the IC community. In response, the SCAI Education Committee, chaired by Dr Sahil A. Parikh, requested the urgent development of a Match Task Force. The request was granted by Drs Timothy D. Henry and Sunil V. Rao, then president and president-elect of SCAI, respectively, on December 21, 2021, and a formal working group was established with the goal to develop an IC fellowship Match. The SCAI Executive Committee approved the Match Task Force creation on February 2, 2022, and a working group was established including members of the SCAI Education committee, SCAI leadership, ACGME IC program directors, IC fellows, and SCAI staff.
The logistics of a fellowship Match
The concept of a clearinghouse to match graduating physicians and residency positions has existed since the early 1950s, and the matching algorithm has been modified iteratively over the past 70 years. In 1995, the NRMP developed the algorithm that is currently in place.14 The theoretical basis of 2-sided matching—with applicants on one side and prospective programs on the other—is centered around making “stable” matches. Specifically, if the Match is successful:
-
1.
there will be no applicant or program that is matched to an unacceptable partner; and
-
2.
there will not be any applicant–program pairs such that a given applicant prefers another program over the matched program.
The NRMP Match mechanism employs a “worker-proposing” version of a deferred acceptance algorithm, where the applicant applies for the positions at the top of their preference list. If each program rejects unacceptable candidates, a candidate who is rejected at any step would then automatically apply to the next highest-ranked program.
The 2022-2023 effort to institute a Match
In May 2022, the SCAI Match Task Force convened a meeting at the SCAI Annual Scientific Sessions and concluded that the ERAS timeline would need to coordinate with the NRMP timeline for an IC fellowship Match to be successful. Notably, sponsors in the Specialties Matching Service must have commitment and active participation of 75% of the eligible IC programs and a minimum of 75% of the available positions for an IC Match to be approved. In July 2022, SCAI staff met with ERAS to consider the logistics of reducing the application cycle from 18 months to 12 months prior to matriculation to align the IC application cycle with other cardiology and subspecialty fellowship programs. The ERAS administrative team indicated that there would have to be consensus among IC fellowship programs to implement such a change.
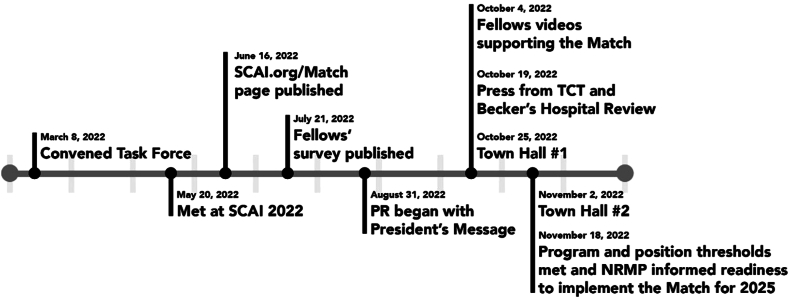
In September 2022, SCAI launched a nationwide campaign to garner support from programs to participate in the IC fellowship Match (Figure 1). SCAI used an online form for programs to pledge their support for the following items:
-
1.
commitment to join the Match;
-
2.
number of positions committed to the Match; and
-
3.
agreement to change the ERAS cycle from 18 months to 12 months, ie, from a December application cycle to a July application cycle.
Figure 1.
Timeline of Society for Cardiovascular Angiography & Interventions (SCAI) campaign to institute the interventional cardiology Match. NRMP, National Resident Match Program; PR, public relations; SCAI, Society for Cardiovascular Angiography & Interventions.
The campaign focused effort on communicating the rationale for the Match to IC program directors, fellows, and the broader IC community. The challenge of obtaining commitment from the necessary number of programs was not underestimated. A SCAI President’s message kicked off the campaign, followed by surveys sent to IC fellows confirming their support for this process. SCAI members and staff created informational video content, distributed communications via email and social media, and held informational webinars/town halls to openly discuss the pros/cons of the Match. Town halls were well-attended, with active question-and-answer sessions following compelling stories from current and former fellows and program directors, transcripts of which can be found in Supplemental Table S1.
While these and other messages were being disseminated, a grassroots effort commenced to explain the rationale of the Match to program directors. The 23-member task force was augmented by 25 additional member volunteers from the SCAI Board of Trustees, Executive Committee, Education Committee, and the Emerging Leaders Mentorship program. These 48 SCAI members reached out to 180 program directors and program staff through emails, phone calls, and text messages, with some IC fellowship program directors receiving contact and advocacy from as many as 4 members of the SCAI Match Task Force. SCAI created a website dedicated to the effort that included a video “Why SCAI wants to join the Match” along with key talking points and interviews from current and former fellows. The website also included a sign-up form for programs to express their support of the Match, as well as a listing of programs that had committed to the Match. During outreach to many programs, the ability to share a list of programs that had already committed support served as a mechanism for positive peer pressure. The real-time tracking mechanism on the SCAI Match website served as another motivational tool for Task Force members and program directors to witness the nationwide interest and momentum building toward this goal.
As with other national efforts of this magnitude, the path to develop consensus in favor of a Match was not without challenges. There were several program directors around the country who strongly opposed the institution of a Match. These were well-regarded academicians and clinician educators who expressed very sincere concerns about the impact on fellows in their programs. The members of the SCAI Match Task Force addressed as many concerns as possible, providing the information necessary for each program director to make the best decision for their institution. A minority of program directors remained opposed to the initiative or did not engage with Task Force members despite multiple attempts to be contacted.
The Match campaign proved highly effective, and by November 2022, the 75% threshold of programs and positions to implement the Match was met, and the NRMP was notified. A letter was then sent to the Association of American Medical Colleges, officially notifying them of the change in the timeline. In January 2023, SCAI signed a sponsor agreement with the NRMP for SCAI to sponsor NRMP’s Specialty Match Services for IC. As the sponsor of the Match, SCAI considered the pros and cons of the “All In Policy,” where registered programs must attempt to fill all ACGME positions at the program through the Match.15,16 SCAI opted out of the “All In Policy” to allow programs to have flexibility for unique situations that require commitment to a candidate outside of the Match. Keeping positions outside of the Match is not expected to be the norm, as the minimum threshold of participation of programs and positions needs to be continually met each year. Applicants who participate in a Match can choose a position outside of the Match; however, the candidate is then required to withdraw from the Match.
Timeline for the IC NRMP Match
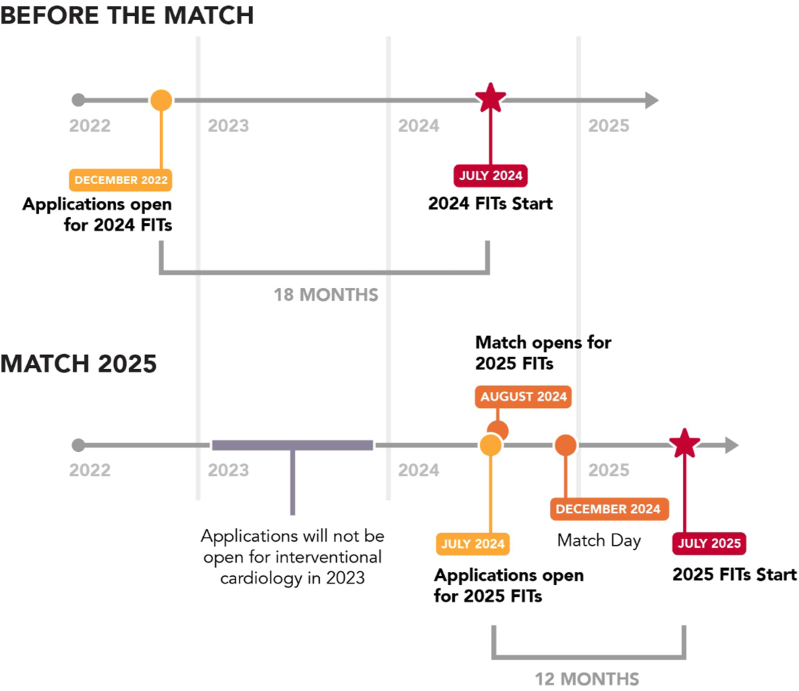
As a result of the successful implementation of the Match in IC, the first Match cycle for incoming IC fellows will open in the summer of 2024. Individuals eligible to apply include cardiovascular disease fellows in their third or final year of training and graduates who have completed fellowship and are in clinical practice. This class will start IC training in July 2025 (Figure 2). ERAS will open its site for programs to download applications in July 2024. Programs must register with the NRMP to receive a unique 9- to 11-character code for applicants to use when ranking programs. Programs must disclose the method they will use to accept applications (most programs use ERAS, but it is not required). The timetable of the Match will enable trainees to apply to the desired number of programs and participate in program interviews for invited applicants throughout the fall of 2024. Applicants can learn about programs without the pressure of deciding until the due date of the candidate rank order list on November 13, 2024. Programs also submit their rank list, and all parties await Match Day on December 4, 2024, for the academic year starting in July 2025.
Figure 2.
Comparison between the current system and National Resident Match Program (NRMP) interventional cardiology Match. FIT, fellow in training.
What will the Match mean for programs: Pros and cons?
The IC Match will lead to important changes in the recruitment process that will require programs to adapt to an applicant ranking process. Faculty and fellow members of IC training programs across the country are hopeful that the Match will ease the pressure and burden of the recruitment process and promote equity. There are several advantages to a fellowship Match (Table 1). Programs have extended time to thoroughly review applications and select fellows that are the best fit for their program. Programs can highlight their strengths, garner consideration from a larger applicant pool, and know that matched candidates share mutual interests and are entering a binding contract. Another important benefit of the Match is that a more diverse pool of applicants can be considered with respect to gender identity, underrepresented ethnic groups, geographic region, cardiovascular disease training programs, and career interest. With the new timeline later in cardiovascular disease training, applicants will be more confident in their career choice, and programs have more time for direct observation of a fellow’s performance to ensure they have the right skill set and characteristics for training in IC before they enter the Match. Interviews can be conducted over a period of days, allowing for ample time to meet with each candidate. If desired, programs will have more time to reach out to colleagues at other institutions familiar with an applicant’s performance. Virtual interviews are recommended, but depending on organizational recommendations and institutional policy, other interview formats may better serve programs.17
Table 1.
Advantages and disadvantages of the interventional cardiology fellowship Match.
| Advantages of the Match | Disadvantages of the Match |
|---|---|
|
|
The Match is a binding contract. Currently, most programs request that an applicant sign a statement of intent as soon as they have accepted their offer; however, it is not uncommon for candidates to rescind their application days, months, or even a year after their initial acceptance. This leaves programs with the unenviable task of identifying a candidate for their program well after other applicants have accepted other positions. While the institution can pursue legal action against the candidate, such lawsuits are rare. This situation is less common with the Match, which establishes an agreement with the applicant such that an accepted position cannot be abandoned.
Finally, the Match will act as an important source of data for future analysis. Over time, the information from the NRMP will allow programs to track candidates, assess the caliber of the program a candidate may have ranked over their own, and evaluate their own rank ratio to identify areas for improvement within their training program and recruitment process. Demographic trends across applicants in IC can also be tracked to allow for comparisons across programs.
There are some limitations to the Match process (Table 1). Programs that have traditionally recruited fellows from within their own institution face more administrative burden and change in the recruitment process. Additionally, as a result of the imposed timeline, IC fellowship recruitment will take place at the same time as the general cardiology fellowship recruitment, which may place a great burden on smaller programs sharing administrative resources with the general fellowships. Finally, despite the carefully constructed mathematical algorithms created by the NRMP aimed at providing applicants and programs with their most eligible choice of candidates, the programs ultimately will not have the final say in the candidate selected for their institution. As with any new process, there will be a learning curve for programs, and there is a possibility that some fellowship programs will not fill their quota. This may lead these programs to participate in a post-Match scramble or seek a fellow outside the Match. The experience of the clinical electrophysiology fellowship Match18 is instructive in this regard, where the accuracy and desirability of the outcomes improved rapidly, with increasing proportion of programs filled and number of fellows matched year over year.
What will the Match mean for fellows?
The transition to an IC Match prioritizes the professional development of cardiovascular disease fellows by facilitating the exploration and affirmation of their career interest in IC. The introduction of a standardized application timeline that begins in the final year of training and is aligned with other Match participating cardiovascular subspecialties permits maximal exposure to the cardiac catheterization laboratory and other cardiovascular subspecialties to inform career decision-making (Table 2). The standardization of the application timeline also eliminates the historically unpredictable pressure of staggered application deadlines and variable interviews and offers timelines that require fellows to commit to a program prior to completion of all interviews, at times without consultation of family and mentors.
Table 2.
What the Match will mean for fellows.
| Prior to the Match | Interventional cardiology Match |
|---|---|
| Apply in the second year of the cardiology fellowship | Apply in the third year of the cardiology fellowship |
| Variable application timelines | Standardized application timeline |
| Variable interview dates | Standardized interview timeline |
| “Exploding” offers | Rank list in order of fellows’ Match preference |
The introduction of the Match affords prospective IC fellows the freedom to explore programs outside of their home institution, if interested. IC fellowship programs may continue to prioritize recruitment of their internal applicants, and may clearly communicate their priority to those internal candidates, but they may not request an equivalent—or binding—commitment from the candidates. IC fellowship applicants may rank their preference of training programs entirely confidentially and may alter their rank list at any time up until the deadline, assuring their freedom from external pressures or potential coercion by training programs. Consequently, applicants may find it necessary to apply to a greater number of programs and to invest more time— and potentially financial resources—in order to ensure that they will find a match and secure an IC fellowship position.
Establishing an IC fellowship Match: Lessons learned and future vision
SCAI recognizes the need for ongoing support of IC training programs and fellows during implementation of the IC Match. Resources for program directors included a dedicated information session at the SCAI 2024 Scientific Sessions and development of resources for structured interviews and other methods to ensure unbiased assessment of applicants. SCAI also understands the need to monitor and address any issues with the Match so that the required program participation is not compromised in the future.
The process of establishing a Match for IC has brought together stakeholders and created a common purpose for programs that elevate the culture and state of training for IC in the US. Specifically, while the development of a Match required tremendous investment of energy, there was a palpable sense of enthusiasm, commitment, and even inevitability once the process was initiated. Program directors, candidates, and leaders of national societies banded together with a common purpose and a belief that converting to a Match was ethical and necessary. This outcome represents a success for IC on many levels. First, training programs from across the country, with different needs, expectations, and value systems recognized that the current recruitment process was broken and had to be changed. Second, seemingly disparate programs came together to establish consensus, arriving at a profound majority decision in favor of the Match. Third, converting to a Match restores a sense of agency to the applicants and a strong vote of support by program directors to foster a healthy, diverse, and inclusive pipeline for the future of the field of IC. The successful implementation of the IC Match is another step in the evolution of IC training that addresses the increasingly complex nature of IC and lays the groundwork for the field’s continued success.
Acknowledgments
Peer review statement
Given his role as Associate Editor, Sahil A. Parikh had no involvement in the post-submission peer review of this article and has no access to information regarding its peer review.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding sources
This work was not supported by funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
To access the supplementary material accompanying this article, visit the online version of the Journal of the Society for Cardiovascular Angiography & Interventions at 10.1016/j.jscai.2024.101980.
Supplementary material
References
- 1.Bass T.A. Certification and competency in interventional cardiology: the changing landscape. Circ Cardiovasc Interv. 2012;5(4):450–453. doi: 10.1161/CIRCINTERVENTIONS.112.972844. [DOI] [PubMed] [Google Scholar]
- 2.Hirshfeld J.W., Banas J.S., Brundage B.H., et al. American College of Cardiology training statement on recommendations for the structure of an optimal adult interventional cardiology training program: a report of the American College of Cardiology task force on clinical expert consensus documents. J Am Coll Cardiol. 1999;34(7):2141–2147. doi: 10.1016/s0735-1097(99)00477-5. [DOI] [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education ACGME frequently asked questions. https://www.acgme.org/about/acgme-frequently-asked-questions/
- 4.Nasca T.J., Philibert I., Brigham T., Flynn T.C. The next GME accreditation system — rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 5.Inohara T., Kohsaka S., Spertus J.A., et al. Comparative trends in percutaneous coronary intervention in Japan and the United States, 2013 to 2017. J Am Coll Cardiol. 2020;76(11):1328–1340. doi: 10.1016/j.jacc.2020.07.037. [DOI] [PubMed] [Google Scholar]
- 6.Valle J.A., Tamez H., Abbott J.D., et al. Contemporary use and trends in unprotected left main coronary artery percutaneous coronary intervention in the United States: an analysis of the national cardiovascular data registry research to practice initiative. JAMA Cardiol. 2019;4(2):100–109. doi: 10.1001/jamacardio.2018.4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waldo S.W., Gokhale M., O’Donnell C.I., et al. Temporal trends in coronary angiography and percutaneous coronary intervention: insights from the VA clinical assessment, reporting, and tracking program. JACC Cardiovasc Interv. 2018;11(9):879–888. doi: 10.1016/j.jcin.2018.02.035. [DOI] [PubMed] [Google Scholar]
- 8.Mack M., Carroll J.D., Thourani V., et al. Transcatheter mitral valve therapy in the United States: a report from the STS-ACC TVT registry. J Am Coll Cardiol. 2021;78(23):2326–2353. doi: 10.1016/j.jacc.2021.07.058. [DOI] [PubMed] [Google Scholar]
- 9.Carroll J.D., Mack M.J., Vemulapalli S., et al. STS-ACC TVT registry of transcatheter aortic valve replacement. J Am Coll Cardiol. 2020;76(21):2492–2516. doi: 10.1016/j.jacc.2020.09.595. [DOI] [PubMed] [Google Scholar]
- 10.Bass T.A., Abbott J.D., Mahmud E., et al. 2023 ACC/AHA/SCAI advanced training statement on Interventional Cardiology (coronary, peripheral vascular, and structural heart interventions) J Soc Cardiovasc Angiogr Interv. 2023;2(2) doi: 10.1016/j.jscai.2022.100575. [DOI] [PubMed] [Google Scholar]
- 11.Association of American Medical Colleges Diversity increases at medical schools in 2022. https://www.aamc.org/news/press-releases/diversity-increases-medical-schools-2022
- 12.Association of American Medical Colleges Interventional Cardiology (Internal Medicine) https://www.aamc.org/media/7056/download
- 13.Shah S., Castro-Dominguez Y., Gupta T., et al. Impact of the COVID-19 pandemic on interventional cardiology training in the United States. Catheter Cardiovasc Interv. 2020;96(5):997–1005. doi: 10.1002/ccd.29198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roth A.E., Peranson E. The redesign of the matching market for American physicians: some engineering aspects of economic design. Am Econ Rev. 1999;89(4):748–780. doi: 10.1257/aer.89.4.748. [DOI] [PubMed] [Google Scholar]
- 15.McCartney C.R., Gianoukakis A.G., Gopalakrishnan G., et al. Voluntary adoption of an all in match policy in the medical specialties matching program: advantages and disadvantages. J Grad Med Educ. 2019;11(4):378–381. doi: 10.4300/JGME-D-18-01090.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Resident Matching Program Fellowship Match all in policy. https://www.nrmp.org/policy/fellowship-match-all-in-policy/ Published November 18, 2021.
- 17.Association of American Medical Colleges Interviews in GME: where do we go from here? https://www.aamc.org/about-us/mission-areas/medical-education/interviews-gme-where-do-we-go-here
- 18.Crossley G.H., Montgomery J., Kanagasundrum A. EP match. Heart Rhythm. 2019;16(7):1131–1132. doi: 10.1016/j.hrthm.2019.01.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.