Case presentation
A 55-year-old Black man presented with ataxia and double vision after unintentional bleach inhalation at work. He was found to have multifocal infarcts on brain magnetic resonance imaging. Oxygen saturation (SpO2) was 82% on room air, requiring 11 L/min of oxygen to maintain an SpO2 of 90%. He had a history of hyperlipidemia and 40 pack-year tobacco use. Cardiac and pulmonary lung examination was unremarkable with no evidence of clubbing. His labs were notable for polycythemia with hemoglobin of 18.7 g/dL (normal 13.0-18.0 g/dL) and a hematocrit of 55.7% (normal 40%-52%). Differential diagnoses included interatrial shunt, obstructive or restrictive lung disease, pulmonary embolus, acute respiratory distress syndrome from chemical inhalational injury, viral or bacterial pneumonia, and pulmonary edema. The bleach inhalation was not considered to be significant based on the patient's history; however, given his profound hypoxemia, a chest computed tomography angiography was subsequently performed. This revealed emphysema, an enlarged left atrium (LA) with diverticular outpouching into a suspected congenital anomaly of the pulmonary vein (PV) (Fig. 1A, B). Pulmonary function testing revealed mild obstruction. A transthoracic echocardiogram with agitated saline demonstrated opacification of the LA in 3 to 4 heart beats (Video 1). During a 3-month follow-up, his SpO2 was 80%, which did not improve with 8 L/min of oxygen. A transesophageal echocardiogram (TEE) demonstrated the large right to left shunt but no evidence of a patent foramen ovale or atrial septal defect (ASD).
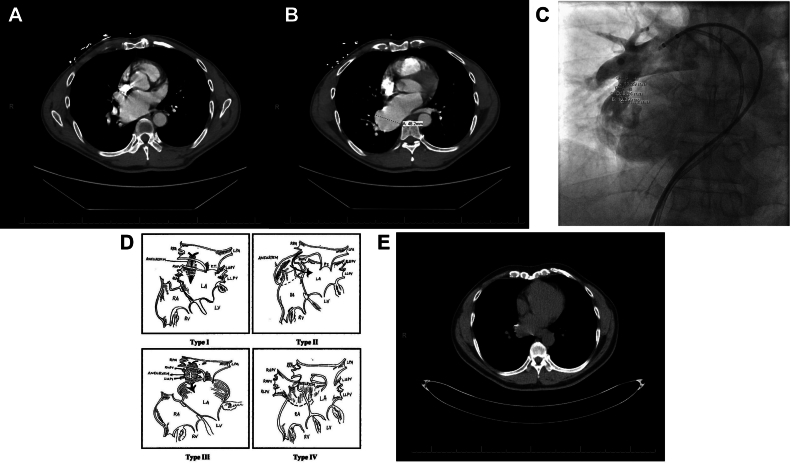
Figure 1.
Chest computed tomography (CT) demonstrating the dilated left atrium (A) and enlarged pulmonary artery (B). Pulmonary angiogram with the 7 Fr balloon wedge and 7 Fr NIH catheter demonstrating anomalous right inferior pulmonary artery fistula to the left atrium with contrast injection to obtain measurements prior to closure (C). One-month follow-up chest CT demonstrating decrease in size of the left atrium (D). Diagrammatic depiction of various right pulmonary artery to left atrium communications (E) taken from the study by Chowdhury et al,1 reproduced after obtaining permission from the publisher.
The patient underwent right heart catheterization to localize the extracardiac shunt. Under general anesthesia, the patient was electively intubated and placed on mechanical ventilation for this procedure. A 7 Fr balloon wedge (BW) catheter (Medtronic) was introduced via the right femoral vein. With TEE assistance, agitated saline was injected at multiple levels. The shunt was demonstrable when bubbles were injected into the right atrium, main pulmonary artery (PA), and right inferior PA but not in the right superior PA or left PA. Pulmonary angiography with balloon occlusion of the right PA revealed an anomalous fistula between the right inferior PA and LA (Video 2). With balloon occlusion of the right inferior PA, the SpO2 increased from 80% with an fraction of inspired oxygen (FiO2) of 100% to 98% on room air. Based on multidisciplinary discussion with adult and pediatric interventional cardiology, percutaneous catheter–based closure was considered feasible. At an FiO2 of 21%, the oxygen saturations were as follows: 72% in the superior vena cava, 71% in the high right atrium, 70% in the mid right atrium, 68% in the low right atrium, 68% in the inferior vena cava, 70% in the right PA, and 83% in the right femoral artery. The calculated Qp/Qs (pulmonary to systemic flow ratio) was 0.52:1.
Intravenous heparin at 50 U/kg to maintain an activated clotting time of >200 seconds and preprocedural prophylactic intravenous antibiotic of 2 g of cefazolin were administered. An 11 Fr sheath was inserted in the right femoral vein, and a 7 Fr BW catheter was used for right heart catheterization and subsequently advanced to the LA. The balloon was inflated to occlude the distal end of the fistula. Right inferior PA angiography demonstrated normal perfusion of all pulmonary segments with return of contrast to the LA via PVs. The BW catheter was exchanged over a J wire for a 7 Fr Amplatzer 45-degree delivery sheath. The length and proximal, mid, and distal widths of the fistula are described in Figure 1C.
Given the above dimensions and structure of the anomalous fistula, a 12-mm Amplatzer muscular ventricular septal defect (VSD) occluder (Abbott) was selected and delivered by deploying the distal rim against the LA and the proximal end in the right pulmonary artery (RPA) fistula. Angiograms were performed to document the position (Video 3). Right PA angiography demonstrated minimal contrast flow through the occluder with no obstruction of RPA flow. TEE documented patency of pulmonary venous return. SpO2 improved to 98% on room air. A transthoracic echocardiogram showed no pericardial effusion and minimal shunt with agitated saline. The patient was discharged on dual antiplatelet therapy with aspirin and clopidogrel for 6 months, followed by aspirin alone.
At 1-month follow-up, the patient remained asymptomatic and did not require any supplemental oxygen. He completed a 6-minute walk test with SpO2 at 97% on room air with ambulation and with a heart rate at 94 beats per minute. He had no shortness of breath. A follow-up noncontrast computed tomography of the chest demonstrated decreased aneurysmal dilation of the LA (Fig. 1D).
Discussion
To the best of our knowledge, we describe for the first time the use of an Amplatzer muscular VSD occluder in an adult for closure of an RPA-to-LA fistula.
An anomalous PA-to-LA fistula was first described in 1950 and is a rare condition, with fewer than 100 cases published to date.1 In the most common congenital forms present at birth, it has been described as a separation failure between the arterial and venous plexus of the pulmonary vasculature during embryological development. Chest trauma resulting in a PA-to-LA fistula has been described, though rare, and felt to be noncontributory in our patient, as he had no history of trauma. Patients with congenital forms, as suspected in our patient, are typically male (3:1 ratio) and present with central cyanosis (60%), dyspnea (50%), neurological symptoms (20%), and telangiectasias (33%). Clinically, patients have an average SpO2 of 72% on room air and polycythemia with an average hematocrit of 76%. The majority of cases are in the pediatric population, and it is interesting to note that despite this anomaly, our patient had an otherwise unremarkable cardiovascular physical examination and presented with symptoms later in life.
Four anatomical PA-to-LA fistula variations are described in the literature and categorized based on co-involvement of PVs, with type I (right PA and LA with normal PV anatomy) the most commonly reported (35.5% of all cases), which is the case in our patient who had direct communication between the RPA and LA without any involvement of the PVs. Type II involves a persistent, additional branch of the PA that may be directly connected to the LA, PV, or both in addition to the absence of the right inferior PV. In types III and IV, PVs are involved in the PA-to-LA fistula (Fig. 1E).1,2 Involvement of the left PA to LA is extremely rare, with only 3 cases reported to date.2
Once diagnosed, treatment options described in the literature include surgical versus transcatheter closure. Catheter-based techniques in adults have been largely derived from experiences in the neonatal and pediatric population3 and involve careful delineation of the anatomy, as inappropriate selection of the occluder device may result in embolization and compromise the PA branches and PVs. The first transcatheter case used a Gianturco coil in a neonate, followed by reports of septal, muscular VSD and duct occluders, mainly used in adolescent patients.3 Based on the measurements of the fistula and involvement of the PV, other closure options have included ASD and patent ductus arteriosus occluders. In our patient, a VSD occluder was chosen over a vascular plug device as (1) there was no discrete constriction for the vascular plug to latch onto and (2) the retention skirts/discs of the VSD occluder allowed for the device to maintain its position to avoid embolization. The ASD occluder was not chosen because the retention skirts on the ASD devices were too large and could occlude the pulmonary venous return. The patent ductus arteriosus occluder was not selected based on its inappropriate size to occlude the fistula. Careful use of TEE and pulmonary angiography assessment allowed for accurate measurement of the fistula and to ensure patency of the PV prior to occlusion.
Conclusions
RPA-to-LA fistula is a rare phenomenon. Catheter-based management of the RPA-to-LA fistula has largely been performed in the pediatric population. Thereby, a multidisciplinary approach involving interventional adult and pediatric cardiology is crucial for its accurate diagnosis and management to prevent any adverse postprocedural events.
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
To access the supplementary material accompanying this article, visit the online version of the Journal of the Society for Cardiovascular Angiography & Interventions at https://doi.org/10.1016/j.jscai.2022.100031.
Supplementary data
References
- 1.Chowdhury U.K., Kothari S.S., Airan B., Subramaniam G., Venugopal P. Right pulmonary artery to left atrium communication. Ann Thorac Surg. 2005;80:365–370. doi: 10.1016/j.athoracsur.2004.08.058. [DOI] [PubMed] [Google Scholar]
- 2.deSouza e Silva N.A., Giuciani E.R., Ritter D.G., Davis G.D., Pluth J.R. Communication between right pulmonary artery and left atrium. Am J Cardiol. 1974;34:857–863. doi: 10.1016/0002-9149(74)90710-3. [DOI] [PubMed] [Google Scholar]
- 3.Kumar V., Varghese M.J., George O.K. Transcatheter closure of direct right pulmonary artery to left atrial communication using vascular plug. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-212878. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.