The dynamics of percutaneous coronary intervention (PCI) have changed significantly since the inception of stents. For the past 3 decades, there has been constant evolution in stent technology, but reducing the incidence of stent thrombosis (ST) and in-stent restenosis (ISR), 2 major Achilles’ heels, has proven elusive. Initially, stents were approved for the treatment of tackling acute dissections and abrupt closure after plain old balloon angioplasty (POBA).1 Later, approval was granted for the prevention of restenosis based on the results of randomized clinical trials demonstrating the superiority of bare-metal stents (BMS) over POBA, with lower restenosis rates.2 When they were launched, BMS had high rates of ST and ISR,3,4 which called into question their utility in coronary intervention; however, ST rates were mitigated with the utilization of antiplatelet therapy. The issue of ISR was addressed with the development of drug-eluting stents (DES), utilizing antiproliferative drugs such as paclitaxel and sirolimus that suppressed smooth muscle proliferation, delayed reendothelialization, and reduced neointimal formation.4,5 Although first-generation DES markedly reduced the rates of ISR when compared with BMS, they spiked the rates of subacute, late, and very late ST, which were associated with serious cardiac events, including myocardial infarction and death.5, 6, 7 This led to a recommendation for a minimum of 12 months of dual antiplatelet therapy (DAPT) after PCI.8 Prolonged DAPT mitigates the rates of ST but is associated with patient compliance issues and an increase in the bleeding rate, creating the need for a safer stent.
Therefore, the quest for further improvement in the performance of DES continued and led to the development of second- and third-generation DES. Iterations in stent design, reduction in strut thickness, utilizing biocompatible or biodegradable polymers, reduction of drug load, and switching from paclitaxel to limus-based drugs further reduced the rates of ST and restenosis.9 In addition, the utilization of intravascular imaging and better understanding of concepts such as stent expansion, stent malapposition, and adequate vessel preparation contributed to additional improvement of post-PCI outcomes. The randomized controlled trials comparing second- vs first-generation DES have shown favorable data with considerably lower rates of ST7,10 and have allowed for shorter durations of DAPT, from 12 months to 1 month, especially in patients known to have a high bleeding risk.11
On the ISR front, although DES reduced the overall restenosis rates, they are still associated with an increase in late and very late restenosis, with rates of up to 3% per year,7,9,12 accounting for up to 10% of procedures in contemporary practice and remaining a therapeutic challenge. To solve this lingering issue, a look back toward the principle of medical practice focusing on the old saying “prevention is better than treatment” is necessary. Adequate vessel preparation before stent implantation and imaging-guided stent implantation have demonstrated a further reduction in ISR and ST and are essential before stent deployment.6,13 Currently, we have enough evidence, including randomized trials, demonstrating that the use of intracoronary imaging-guided revascularization is associated with lower rates of major adverse cardiac events and target lesion revascularization compared with angiographic guidance.14,15 Despite this, intracoronary imaging modalities, including intravascular ultrasound (IVUS) and optical coherence tomography (OCT), continue to be underutilized (<25%) during PCI in the United States.16 The standardized use of intracoronary imaging during de novo coronary disease intervention with optimal vessel preparation before deploying the stent should be a fundamental step toward the prevention of ISR. For example, calcified lesions should be treated by adjunctive atherectomy or intravascular lithotripsy before stent deployment.17
Intracoronary imaging is also essential in understanding the mechanism of ISR and should be the key initial step when approaching the management of stent failure pathologies. Although the use of either IVUS or OCT is interchangeable, ISR is a special clinical scenario where the use of OCT may be preferred due to the limited ability to evaluate neoatherosclerosis by IVUS. The use of intracoronary imaging not only outlines the underlying mechanism of stent failure—mechanical or biological—but also determines the treatment strategy for the target lesion. The underutilization of intracoronary imaging can be improved by training interventional cardiologists and identifying physical barriers obscuring its use. The OCT-ISR app is a free educational tool to understand different types of ISR, with examples of OCT images and their treatment methodology. Mechanical issues, including stent underexpansion and stent undersizing, are most likely mitigated by high-pressure balloons such as the OPN-NC (SIS Medical AG) balloon or off-label use of intravascular lithotripsy. Stent fracture is also best evaluated by OCT and is characterized by the absence of stent struts at the site of the fracture, with a predisposition to nonuniform drug distribution, and will most likely need implantation of another layer of the stent. Well-expanded stents with severe neointimal hyperplasia may be best treated with brachytherapy, drug-coated balloons (DCBs) if available, or an additional layer of DES.
The final question remains how to optimally treat ISR of DES. POBA alone is associated with a high recurrence rate, and adding another layer of stent for the treatment of DES-ISR, although the most common therapy today, is not desired. This leaves DCBs as a potential first-line treatment of DES-ISR. Although the DCB is an appealing technology, its future utilization is subjected to the results of well-powered randomized clinical trials testing their noninferiority to DES. With the initial promising results of both paclitaxel- and sirolimus-based DCBs,18,19 the randomized studies will assess DCB safety and efficacy against standard-of-care POBA or best-in-class second-generation DES for the treatment of ISR. Meanwhile, vascular brachytherapy remains the most potent option for second and further recurrences of ISR,20 but it is also associated with late recurrences, and unfortunately its availability is limited to only a few centers in the United States.
Keeping this in mind, the SCAI Expert Consensus Statement on the Management of In-Stent Restenosis and Stent Thrombosis21 is a commendable step toward standardizing guidelines for treating stent failure pathologies. The expert consensus document discusses risk factors and various classifications and stresses the importance of using intracoronary imaging to determine the cause and choosing effective management strategies for the treatment of both ISR and ST. This document can be used to better understand the modifiable factors that can result in improved outcomes of stenting for coronary intervention and can be used as guidance for the prevention and treatment of both ST and ISR.
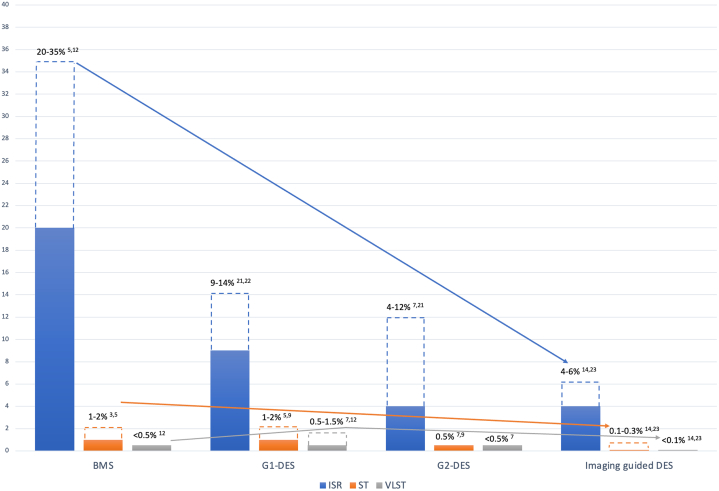
Over the past 3 decades, investigators have been asking whom to blame for the adverse events related to stents. Are they related to the stent technology, the patient and lesion complexity, or the operator’s technique? The answer is most likely all of the above. Nevertheless, ISR and ST rates are in constant decline (Figure 1)22, 23, 24 and a moving target due to the awareness and improvements that have been implemented over the years. Finally, after 3 decades of stenting every vessel and every lesion, we should ask the questions “Are we placing too many stents?” and “Is it time to consider other emerging technologies such as biodegradable scaffolds or DCBs, which promote the concept of leaving nothing behind?” Although biodegradable scaffolds were removed from marketing in the United States due to mixed results when compared with DES, DCBs are emerging as an alternative to DES for de novo lesions and have the potential to further reduce the rates of ST and ISR by reduction of usage of stents. DCBs may be considered for broadened use if proven to be noninferior to DES in randomized clinical trials, especially in small and distal vessel lesions and in bifurcation lesions. The premise of this technology is simple: do not cage the vessel with metal, and you will not have ST or ISR. Hence, stent technology will continue to be challenged for continued improvements until the abolishment of ST and ISR, or it will be replaced by other emerging technologies in the future.
Figure 1.
The rates and trends of in-stent restenosis (ISR), stent thrombosis (ST), and very late stent thrombosis (VLST) fromthebaremetal stent (BMS)erato the intracoronary imaging-guided drug-eluting stent (DES) era. The rates of ISR5,7,12,14,22, 23, 24 and ST3,5,7,9,14,24 constantly declined; however, the rates of VLST increased with first generation DES (G1-DES)7,12 but declined with the use of second generation DES (G2-DES)7 and intracoronary imaging.14, 24
Acknowledgments
Declaration of competing interest
Ron Waksman reports serving on the advisory boards of Abbott Vascular, Boston Scientific, Medtronic, Philips IGT, and Pi-Cardia Ltd; being a consultant for Abbott Vascular, Biotronik, Boston Scientific, Cordis, Medtronic, Philips IGT, Pi-Cardia Ltd, Swiss Interventional Systems/SIS Medical AG, Transmural Systems Inc, and Venous MedTech; receiving institutional grant support from Amgen, Biotronik, Boston Scientific, Chiesi, Medtronic, and Philips IGT; and being an investor in MedAlliance and Transmural Systems. Sukhdeep Bhogal reported no financial interests.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Sigwart U., Puel J., Mirkovitch V., Joffre F., Kappenberger L. Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl J Med. 1987;316(12):701–706. doi: 10.1056/NEJM198703193161201. [DOI] [PubMed] [Google Scholar]
- 2.Serruys P.W., de Jaegere P., Kiemeneij F., et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331(8):489–495. doi: 10.1056/NEJM199408253310801. [DOI] [PubMed] [Google Scholar]
- 3.Tada T., Byrne R.A., Simunovic I., et al. Risk of stent thrombosis among bare-metal stents, first-generation drug-eluting stents, and second-generation drug-eluting stents: results from a registry of 18,334 patients. J Am Coll Cardiol Intv. 2013;6(12):1267–1274. doi: 10.1016/j.jcin.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Moses J.W., Leon M.B., Popma J.J., et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003;349(14):1315–1323. doi: 10.1056/NEJMoa035071. [DOI] [PubMed] [Google Scholar]
- 5.Stettler C., Wandel S., Allemann S., et al. Outcomes associated with drug-eluting and bare-metal stents: a collaborative network meta-analysis. Lancet. 2007;370(9591):937–948. doi: 10.1016/S0140-6736(07)61444-5. [DOI] [PubMed] [Google Scholar]
- 6.Hong M.K., Mintz G.S., Lee C.W., et al. Intravascular ultrasound predictors of angiographic restenosis after sirolimus-eluting stent implantation. Eur Heart J. 2006;27(11):1305–1310. doi: 10.1093/eurheartj/ehi882. [DOI] [PubMed] [Google Scholar]
- 7.Jensen L.O., Thayssen P., Christiansen E.H., et al. Safety and efficacy of everolimus- versus sirolimus-eluting stents: 5-year results from SORT OUT IV. J Am Coll Cardiol. 2016;67(7):751–762. doi: 10.1016/j.jacc.2015.11.051. [DOI] [PubMed] [Google Scholar]
- 8.Fihn S.D., Gardin J.M., Abrams J., et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126(25):3097–3137. doi: 10.1161/CIR.0b013e3182776f83. [DOI] [PubMed] [Google Scholar]
- 9.Gada H., Kirtane A.J., Newman W., et al. 5-year results of a randomized comparison of XIENCE V everolimus-eluting and TAXUS paclitaxel-eluting stents: final results from the SPIRIT III trial (clinical evaluation of the XIENCE V everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions) J Am Coll Cardiol Intv. 2013;6(12):1263–1266. doi: 10.1016/j.jcin.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Maeng M., Tilsted H.H., Jensen L.O., et al. Differential clinical outcomes after 1 year versus 5 years in a randomised comparison of zotarolimus-eluting and sirolimus-eluting coronary stents (the SORT OUT III study): a multicentre, open-label, randomised superiority trial. Lancet. 2014;383(9934):2047–2056. doi: 10.1016/S0140-6736(14)60405-0. [DOI] [PubMed] [Google Scholar]
- 11.Mehran R., Cao D., Angiolillo D.J., et al. 3- or 1-month DAPT in patients at high bleeding risk undergoing everolimus-eluting stent implantation. J Am Coll Cardiol Intv. 2021;14(17):1870–1883. doi: 10.1016/j.jcin.2021.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Kastrati A., Mehilli J., Pache J., et al. Analysis of 14 trials comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med. 2007;356(10):1030–1039. doi: 10.1056/NEJMoa067484. [DOI] [PubMed] [Google Scholar]
- 13.Fujii K., Mintz G.S., Kobayashi Y., et al. Contribution of stent underexpansion to recurrence after sirolimus-eluting stent implantation for in-stent restenosis. Circulation. 2004;109(9):1085–1088. doi: 10.1161/01.CIR.0000121327.67756.19. [DOI] [PubMed] [Google Scholar]
- 14.Hong S.J., Mintz G.S., Ahn C.M., et al. Effect of intravascular ultrasound–guided drug-eluting stent implantation: 5-year follow-up of the IVUS-XPL randomized trial. J Am Coll Cardiol Intv. 2020;13(1):62–71. doi: 10.1016/j.jcin.2019.09.033. [DOI] [PubMed] [Google Scholar]
- 15.Gao X.F., Ge Z., Kong X.Q., et al. 3-year outcomes of the ULTIMATE trial comparing intravascular ultrasound versus angiography-guided drug-eluting stent implantation. J Am Coll Cardiol Intv. 2021;14(3):247–257. doi: 10.1016/j.jcin.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Elgendy I.Y., Ha L.D., Elbadawi A., et al. Temporal trends in inpatient use of intravascular imaging among patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol Intv. 2018;11(9):913–915. doi: 10.1016/j.jcin.2018.01.254. [DOI] [PubMed] [Google Scholar]
- 17.Bhogal S, Garcia-Garcia HM, Klein A, et al. Intravascular lithotripsy for the treatment of severely calcified coronary artery disease: a DISRUPT CAD III intravascular ultrasound substudy. Cardiovasc Revasc Med. Published online March 11, 2023. doi:10.1016/j.carrev.2023.03.003 [DOI] [PubMed]
- 18.Costa R.A., Mandal S.C., Hazra P.K., et al. Sirolimus-coated balloon with a microsphere-based technology for the treatment of de novo or restenotic coronary lesions. Cardiovasc Revasc Med. 2022;45:18–25. doi: 10.1016/j.carrev.2022.08.037. [DOI] [PubMed] [Google Scholar]
- 19.Xu B., Gao R., Wang J., et al. A prospective, multicenter, randomized trial of paclitaxel-coated balloon versus paclitaxel-eluting stent for the treatment of drug-eluting stent in-stent restenosis: results from the PEPCAD China ISR trial. J Am Coll Cardiol Intv. 2014;7(2):204–211. doi: 10.1016/j.jcin.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Varghese M.J., Bhatheja S., Baber U., et al. Intravascular brachytherapy for the management of repeated multimetal-layered drug-eluting coronary stent restenosis. Circ Cardiovasc Interv. 2018;11(10) doi: 10.1161/CIRCINTERVENTIONS.118.006832. [DOI] [PubMed] [Google Scholar]
- 21.Klein L.W., Nathan S., Maehara A., et al. SCAI expert consensus statement on management of in-stent restenosis and stent thrombosis. J Soc Cardiovasc Angiogr Interv. 2023;2(4):100971. [Google Scholar]
- 22.Cassese S., Byrne R.A., Tada T., et al. Incidence and predictors of restenosis after coronary stenting in 10 004 patients with surveillance angiography. Heart. 2014;100(2):153–159. doi: 10.1136/heartjnl-2013-304933. [DOI] [PubMed] [Google Scholar]
- 23.Corbett S.J., Cosgrave J., Melzi G., et al. Patterns of restenosis after drug-eluting stent implantation: insights from a contemporary and comparative analysis of sirolimus- and paclitaxel-eluting stents. Eur Heart J. 2006;27(19):2330–2337. doi: 10.1093/eurheartj/ehl229. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J., Gao X., Kan J., et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE Trial. J Am Coll Cardiol. 2018;72(24):3126–3137. doi: 10.1016/j.jacc.2018.09.013. [DOI] [PubMed] [Google Scholar]