Abstract
Background
For bifurcating coronary lesions, a provisional stent technique is recommended compared with a routine 2-stent strategy. However, much of these data are from trials involving first-generation drug-eluting stents (DES) or bare-metal stents where the risk of restenosis with the 2-stent technique is higher. We investigated the efficacy of various 2-stent techniques versus a provisional stent technique for bifurcation lesions with newer-generation DES.
Methods
PubMed and Embase were searched through May 2022 for randomized control trials investigating bifurcation percutaneous coronary intervention techniques using newer-generation DES, and a meta-analysis was conducted. The primary end point was major adverse cardiovascular events (MACE) at the longest reported follow-up time.
Results
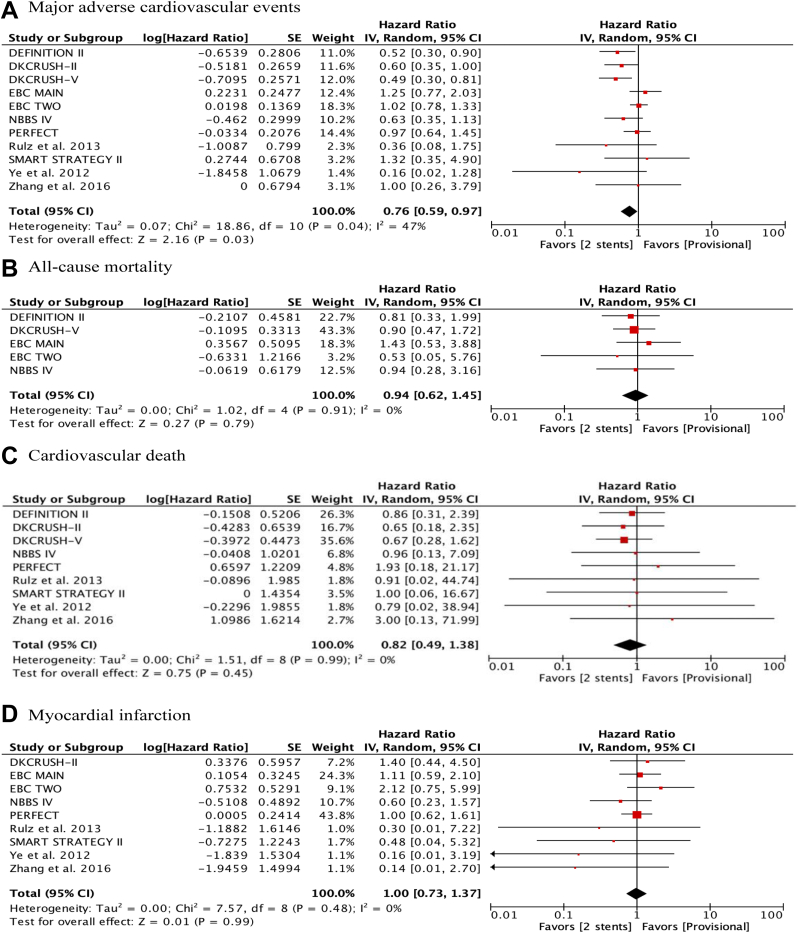
Our study identified 13 randomized control trials including 4041 patients. Compared with the provisional technique, 2-stent techniques significantly decreased MACE (hazard ratio [HR], 0.76; 95% CI, 0.59-0.97; P = .03), target vessel myocardial infarction (HR, 0.38; 95% CI, 0.20-0.71; P = .002), and target vessel revascularization (HR, 0.66; 95% CI, 0.47-0.93; P = .02). There were no significant differences in all-cause mortality (HR, 0.94; 95% CI, 0.62-1.45; P = .79), cardiovascular mortality (HR, 0.82; 95% CI, 0.49-1.38; P = .45), myocardial infarction (HR, 1.00; 95% CI, 0.73-1.37; P = .99), and stent thrombosis (HR, 0.86; 95% CI, 0.52-1.44; P = .58). Of the 2-stent techniques, the double kissing crush technique significantly decreased MACE and target lesion revascularization than other 2-stent techniques.
Conclusions
In this era of newer-generation DES, a 2-stent approach, especially the double kissing crush technique, is superior to a provisional stenting technique for a bifurcation lesion, with a significant reduction in MACE, target vessel myocardial infarction, and revascularization.
Keywords: 2-stent, bifurcation, coronary artery disease, DK crush, drug-eluting stent, provisional
Central Illustration
Highlights
-
•
Coronary bifurcations account for 20% of percutaneous coronary interventions.
-
•
It is uncertain if a provisional side branch stenting approach is as effective as 2-stent techniques for bifurcation lesions.
-
•
Two-stent approaches, especially the DK-crush technique, are associated with decreased risks of ischemic endpoints compared with the provisional technique with newer-generation drug-eluting stents.
Introduction
Coronary bifurcations account for up to 20% of all percutaneous coronary interventions (PCIs), and they consist of one of the most challenging subsets in terms of procedural success rate and long-term cardiac events.1, 2, 3, 4, 5 A provisional side branch (SB) stenting strategy is recommended as an initial standard approach for most bifurcation lesions, and the use of intentional 2-stent techniques is recommended under specific circumstances.6,7 Despite these recommendations, conflicting data remain regarding the optimal approach to bifurcation lesions.8, 9, 10, 11, 12, 13, 14 The recommendations mentioned above are based on studies in which first-generation drug-eluting stents (DES) or bare-metal stents were utilized. These stents have a higher risk of restenosis than contemporary DES, and a provisional stent approach makes intuitive sense. However, given the lower stent-related events with newer-generation DES, it is not clear whether the above results apply to the contemporary practice of PCI with newer-generation DES. Therefore, we sought to evaluate the optimal bifurcation PCI techniques in the era of newer-generation DES.
Methods
This meta-analysis is reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement standards.15 This study was registered in the PROSPERO database (registration number: CRD42020211736).
Eligibility criteria
The eligibility criteria were the following: (1) the study was published in a peer-reviewed journal, (2) the design was a randomized controlled trial (RCT) or subgroup analyses of RCTs in patients undergoing PCIs for bifurcation lesions, comparing bifurcation PCI techniques, (3) the studies included patients who underwent PCIs with second-generation DES, and (4) the study reported outcomes of interest (listed below).
Information sources and search
All studies investigating bifurcation PCI techniques were searched using a 2-level search strategy. First, PubMed and Embase were searched from inception through May 31, 2022, using web-based search engines (PubMed and OVID). Search terms included random, coronary, bifurcation, stenting OR percutaneous coronary intervention OR PCI, single stent OR one stent OR 1 stent OR double stent OR two stent OR 2 stent OR simple OR complex stent OR provisional OR T stenting OR T and protrusion OR crush OR DK-crush OR double-kissing crush OR mini-crush OR culotte OR reverse culotte OR V stenting OR Y stenting. We did not apply any language restrictions.
Study selection and data collection process
Relevant studies were identified through a manual search of secondary sources, including references of initially identified articles, reviews, and commentaries. All references were downloaded for consolidation, elimination of duplicates, and further analyses. Two independent and blinded authors (T.K.16 and T.F.) reviewed the search results to select the studies based on inclusion and exclusion criteria. When a consensus was not reached between the 2 authors, a third author (H.T.) was consulted to reach a decision. Disagreements were resolved by consensus.
We collected data according to the following PICOS: P (Population), patients with bifurcations undergoing PCIs; I (Intervention), 2-stent approach; C (Comparison), provisional approach or a different 2-stent technique; O (Outcome), all-cause mortality, cardiovascular mortality, myocardial infarction (MI), target vessel myocardial infarction (TVMI), target lesion revascularization (TLR), target vessel revascularization (TVR), and stent thrombosis (ST); and S (Study type), RCT.
Risk of bias assessment
Study quality was assessed using the Cochrane Collaboration risk of bias 2.0 tool.17 Two investigators (T.K. and T.F.) reviewed the studies and judged selection, comparability, and outcomes independently using the Cochrane risk of bias tool.
Outcomes
The primary end point was major adverse cardiovascular events (MACE) defined in the individual trials. The secondary end points were all-cause mortality, cardiovascular death, MI, TVMI, TVR, TLR, and ST. Hazard ratio (HR) or risk ratio was obtained from each study.
Statistical analysis
The Review Manager (RevMan) version 5.4 (The Cochrane Collaboration, 2020) was used to calculate the pooled HRs with 95% CIs. The random-effects model was used regardless of the heterogeneity among studies because it allows a more conservative assessment of the pooled effect size. Significant heterogeneity was considered present when the I2 index was >50% or P for heterogeneity was <.05. Publication bias was assessed using funnel plots.
As a sensitivity analysis, we performed the same analysis including studies in which newer-generation DES were used in >50% of patients. In addition, we performed an additional sensitivity analysis, in which studies were stratified by Double Kissing Crush (DKCRUSH) trials versus non-DKCRUSH trials, to test subgroup differences. Moreover, an additional analysis stratified by left-main trials versus non–left-main trials was performed to test subgroup differences.
Finally, we performed a network meta-analysis using the “netmeta” 3.6.2 package (R Foundation for Statistical Computing)18 for all outcomes comparing each PCI technique. PCI techniques were classified into double kissing (DK) crush, culotte, T-and-protrusion (TAP), and others. Other 2-stent PCI techniques such as the T stent technique or crush technique were classified into the “others” group. If a specific PCI technique was used in >50% of the patients, the group was classified into the specific PCI technique group. Within the framework, I2 and Q statistics, which represent the proportion of total variation in study estimates because of heterogeneity, were used to quantify heterogeneity.19,20 The Q statistics are the sum of a statistic for heterogeneity, and a statistic for inconsistency, representing the variability of treatment effect between direct and indirect comparisons at the meta-analytical level.21 The P-score metric was used to rank the comparative hierarchy of efficacy and safety of the treatments. The value of P-score ranges between 0 and 1. A higher value means a higher likelihood that the therapy is more effective or safe.
Results
Our study included 13 RCTs (Figure 1) with a total of 4041 patients from analyses of DKCRUSH-II,8 the study by Ruiz-Salmerón et al,22 the study by Ye et al,23 DKCRUSH-III,24 PERFECT,25 Nordic-Baltic Bifurcation Study (NBBS) IV,26 European Bifurcation Coronary (EBC) TWO,27 Bifurcation Bad Krozingen II,28 the study by Zhang et al,29 DKCRUSH-V,9 DEFINITION II,10 SMART STRATEGY,30 and EBC MAIN.14 Eleven trials compared the 2-stent technique with the provisional technique. One trial compared the DK crush technique with the culotte technique. Another trial compared the culotte technique with the TAP technique. In the 2-stent group of the DEFINITION II trial, the DK crush technique was used in 77% of patients. In the 2-stent group of the EBC MAIN trial, the culotte technique was used in 53% of patients. In the 2-stent group of SMART STRATEGY, the proportion of each PCI technique was not reported. The mean (±SD) weighted follow-up duration was 23.8 ± 15.1 months. In a sensitivity analysis that included studies in which newer-generation DES were used in >50% of patients, we excluded the study by Ye et al,23 PERFECT, and NBBS IV, identifying 10 eligible RCTs including 3106 patients.
Figure 1.
The Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram of study selection. Thirteen randomized controlled trials with 4041 patients were included in this meta-analysis.
Baseline characteristics
The demographic characteristics of patients in each trial are summarized in Table 1. The mean age ranged from 61 to 71 years, and the percentage of men ranged from 67% to 87%. Most patients underwent PCIs for unstable or stable angina pectoris. The details of angiographic findings, PCI techniques, and stents used are summarized in Table 2 and Supplemental Table S1. Among 4041 patients included in this study, bifurcation lesions were located in the left main artery in 1756 (43%) patients, left anterior descending artery in 1839 (46%) patients, left circumflex artery in 334 (8%) patients, and right coronary artery in 113 (3%) patients. The DKCRUSH-III, DKCRUSH-V, SMART STRATEGY II, and EBC MAIN trials investigated PCI techniques for left main bifurcation lesions only. True bifurcation lesions were present in 3954 (98%) patients. A 2-stent approach was used in 2392 (59%) patients. The final kissing balloon technique was more commonly performed in the 2-stent group. First-generation DES were used in a proportion of patients in 5 studies included in this analysis. For example, 50% of patients in the NBBS IV study and 9% of patients in the Bifurcation Bad Krozingen II study received Cypher stents. The percentage of Cypher stents used among patients with sirolimus-eluting stents in the study by Ye et al23 and the PERFECT trial were not available. More than 80% of the patients included in this analysis received newer-generation DES. In a sensitivity analysis, the patients in the study by Ye et al,23 PERFECT, and NBBS IV were removed, and >99% of patients received newer-generation DES. All studies were generally considered of an intermediate bias risk (Supplemental Figure S1).
Table 1.
Basic characteristics of patients in each trial.
| Reference (trial), year | PCI technique | Sample size | Age (y), mean ± SD | Male (%) | Smoking (%) | DM (%) | HTN (%) | HLP (%) | Previous MI (%) | Previous PCI (%) | STEMI (%) | NSTEMI (%) | Unstable angina (%) | Stable angina (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al (DKCRUSH-II),8 2011 | DK | 185 | 64 ± 11 | 146 (79) | 57 (31) | 36 (20) | 121 (65) | 63 (34) | 32 (17) | 39 (21) | 25 (14) | 5 (3) | 123 (67) | 29 (16) |
| Pro | 185 | 65 ± 10 | 141 (76) | 44 (24) | 44 (24) | 112 (61) | 53 (29) | 26 (14) | 38 (21) | 22 (12) | 9 (5) | 126 (68) | 21 (11) | |
| Ruiz et al,22 2013 | Pro | 33 | 64 ± 13 | 28 (85) | 20 (61) | 15 (45) | 22 (67) | 17 (51) | NA | 7 (21) | NA | NA | NA | NA |
| T stent | 36 | 64 ± 13 | 28 (78) | 18 (50) | 12 (33) | 26 (72) | 23 (64) | NA | 9 (25) | NA | NA | NA | NA | |
| Ye et al,23 2012 | Pro | 30 | 62 ± 9 | 23 (77) | NA | 4 (13) | 20 (67) | 6 (20) | 2 (7) | NA | 0 | NA | 19 (63.3) | 11 (37) |
| DK | 38 | 63 ± 10 | 24 (63) | NA | 7 (18) | 29 (76) | 7 (18) | 4 (11) | NA | 0 | NA | 27 (71.1) | 11 (29) | |
| Chen et al (DKCRUSH-III),24 2015 | DK | 208 | 64 ± 10 | 162 (77) | 58 (28) | 67 (32) | 148 (70) | 87 (41) | 32 (15) | 47 (22) | 0 | 0 | 165 (79) | 21 (10) |
| Culotte | 207 | 63 ± 9 | 167 (80) | 54 (26) | 63 (30) | 128 (61) | 88 (42) | 29 (14) | 31 (15) | 0 | 0 | 174 (83) | 20 (10) | |
| Kim et al (PERFECT),25 2015 | Crush | 213 | 61 ± 9 | 160 (75) | 54 (25) | 55 (26) | 118 (55) | 132 (62) | 9 (4) | 20 (9) | NA | NA | 74 (35) | 130 (61) |
| Pro | 206 | 61 ± 9 | 155 (75) | 67 (32) | 60 (29) | 114 (55) | 118 (57) | 9 (4) | 11 (5) | NA | NA | 65 (32) | 127 (62) | |
| Kumsars et al (NBBS IV),26 2015 | Pro | 220 | 64 ± 12 | NA | 41 (19) | 36 (16) | 152 (70) | 178 (82) | NA | 78 (35) | 0 | 0 | 28 (13) | 188 (87) |
| Culotte | 228 | 63 ± 11 | NA | 48 (21) | 35 (15) | 149 (66) | 184 (81) | NA | 77 (33) | 0 | 0 | 38 (17) | 187 (82) | |
| Hildick-Smith et al (EBC TWO),27 2016 | Pro | 103 | 63 ± 11 | 87 (85) | 58 (56) | 26 (25) | 65 (63) | 72 (70) | 40 (39) | 41 (40) | 32 (31) | 71 (69) | ||
| Culotte | 97 | 64 ± 12 | 76 (78) | 49 (50) | 30 (31) | 66 (68) | 70 (70) | 40 (41) | 40 (41) | 31 (32) | 66 (68) | |||
| Ferenc et al (BBK II),28 2016 | Culotte | 150 | 66 ± 11 | 107 (71) | 17 (11) | 41 (27) | 132 (88) | NA | 24 (16) | 57 (38) | 32 (21) | 118 (78) | ||
| TAP | 150 | 69 ± 10 | 114 (76) | 17 (11) | 42 (28) | 128 (85) | NA | 32 (21) | 48 (32) | 29 (19) | 121 (81) | |||
| Zhang et al,29 2016 | Pro | 52 | 65 ± 11 | 48 (92) | 31 (60) | 10 (19) | 35 (67) | 6 (11) | 12 (23) | 13 (25) | 5 (10) | 7 (13) | 25 (48) | 15 (29) |
| Culotte | 52 | 64 ± 7 | 43 (83) | 27 (52) | 11 (21) | 33 (63) | 6 (11) | 10 (19) | 12 (23) | 3 (6) | 1 (2) | 28 (54) | 20 (38) | |
| Chen et al (DKCRUSH-V),9 2019 | DK | 240 | 64 ± 10 | 188 (78) | 78 (32) | 62 (26) | 156 (64) | 115 (47) | 51 (21) | 43 (18) | 31 (13) | 168 (70) | 34 (14) | |
| Pro | 242 | 65 ± 9 | 199 (83) | 82 (34) | 69 (29) | 175 (73) | 114 (47) | 52 (22) | 33 (14) | 26 (11) | 180 (74) | 26 (10) | ||
| Zhang et al (DEFINITION II),10 2020 | Pro | 325 | 64 ± 10 | 250 (77) | 98 (30) | 116 (36) | 230 (70) | 223 (69) | 42 (13) | 54 (17) | 73 (23) | 164 (51) | 71 (22) | |
| 2 stent | 328 | 63 ± 11 | 255 (78) | 93 (28) | 112 (34) | 215 (66) | 227 (69) | 39 (12) | 65 (20) | 72 (22) | 160 (49) | 79 (24) | ||
| Kim et al (SMART STRATEGY II),30 2020 | Pro | 23 | 66 ± 9 | 15 (65) | 6 (26) | 10 (44) | 18 (78) | 11 (48) | 1 (4) | 5 (22) | NA | NA | NA | NA |
| 2 stent | 23 | 66 ± 11 | 16 (70) | 5 (22) | 11 (48) | 17 (74) | 9 (39) | 2 (9) | 4 (17) | NA | NA | NA | NA | |
| Hildick-Smith et al (EBC MAIN),14 2021 | Pro | 230 | 71 ± 10 | 182 (79) | 36 (16) | 66 (29) | 180 (79) | 158 (70) | 60 (28) | 93 (41) | 78 (33) | 149 (66) | ||
| 2 stent | 237 | 71 ± 10 | 177 (74) | 30 (13) | 62 (27) | 190 (82) | 166 (72) | 66 (28) | 99 (43) | 93 (40) | 139 (60) | |||
DK, double kissing; DM, diabetes mellitus; HLP, hyperlipidemia; HTN, hypertension; MI, myocardial infarction; NA, not available; NSTEMI, non ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; Pro, provisional; ST, stent thrombosis; STEMI, ST-elevation myocardial infarction; TAP, T-and-protrusion.
Table 2.
Angiographic and procedural characteristics.
| Reference (trial), year | PCI technique | Sample size | LM (%) | LAD (%) | LCX (%) | RCA (%) | True bifurcation (%) | SB (mm), mean ± SD | FKBI (%) |
|---|---|---|---|---|---|---|---|---|---|
| Chen et al (DKCRUSH-II),8 2011 | DK | 185 | 33 (18) | 112 (61) | 23 (12) | 17 (9) | 185 (100) | 15.3 ± 11.1 | 183 (100) |
| Pro | 185 | 29 (16) | 110 (60) | 30 (16) | 16 (9) | 185 (100) | 14.6 ± 11.9 | 144 (79) | |
| Ruiz et al,22 2013 | Pro | 33 | 0 | 24 (71) | 9 (26) | 1 (3) | 27 (79) | NA | 14 (42) |
| T stent | 36 | 0 | 26 (72) | 6 (17) | 4 (11) | 33 (92) | NA | 23 (64) | |
| Ye et al,23 2012 | Pro | 30 | 0 | 53 (78) | 10 (15) | 5 (7) | 37 (100) | 10.2 ± 8.4 | 26 (87) |
| DK | 38 | 38 (100) | 16.9 ± 8.2 | 38 (100) | |||||
| Chen et al (DKCRUSH-III),24 2015 | DK | 208 | 210 (100) | 0 | 0 | 0 | 210 (100) | 16.5 ± 11.1 | 209 (99) |
| Culotte | 207 | 209 (100) | 0 | 0 | 0 | 209 (100) | 17.0 ± 13.0 | 208 (99) | |
| Kim et al (PERFECT),25 2015 | Crush | 213 | 0 | 200 (94) | 10 (5) | 3 (1) | 194 (91) | 10.3 ± 8.2 | 204 (96) |
| Pro | 206 | 0 | 190 (92) | 15 (7) | 1 (0) | 169 (82) | 8.3 ± 7.3 | 163 (79) | |
| Kumsars et al (NBBS IV),26 2015 | Pro | 220 | 6 (3) | 161 (74) | 36 (17) | 14 (7) | 218 (100) | 6.4 ± 4.1 | 79 (36) |
| Culotte | 228 | 3 (1) | 174 (77) | 40 (18) | 9 (4) | 228 (100) | 7.7 ± 4.9 | 208 (91) | |
| Hildick-Smith et al (EBC TWO),27 2016 | Pro | 103 | 0 | 80 (78) | 16 (15) | 6 (6) | 103 (100) | 9.7 (SD7.1) | 97 (94) |
| Culotte | 97 | 0 | 75 (77) | 18 (19) | 4 (4) | 97 (100) | 10.8 (SD7.3) | 93 (96) | |
| Ferenc et al (BBK II),28 2016 | Culotte | 150 | 28 (19) | 82 (55) | 36 (24) | 4 (3) | 147 (98) | 13.8 ± 6.6 | NA |
| TAP | 150 | 23 (15) | 83 (55) | 38 (25) | 6 (4) | 143 (95) | 15.5 ± 6.9 | NA | |
| Zhang et al,29 2016 | Pro | 52 | 16 (31) | 33 (63) | 3 (6) | 0 | 52 (100) | 12.8 ± 4.9 | 43 (83) |
| Culotte | 52 | 14 (27) | 34 (65) | 2 (4) | 2 (4) | 52 (100) | 14.1 ± 7.1 | 48 (92) | |
| Chen et al (DKCRUSH-V),9 2019 | DK | 240 | 242 (100) | 0 | 0 | 0 | 242 (100) | NA | 239 (99) |
| Pro | 242 | 242 (100) | 0 | 0 | 0 | 242 (100) | NA | 191 (79) | |
| Zhang et al (DEFINITION II),10 2020 | Pro | 325 | 94 (29) | 197 (61) | 25 (8) | 9 (3) | 315 (97) | 19.9 ± 9.3 | 109 (34) patients underwent first kissing balloon inflation after first stent implantation. 73 (23) patients underwent 2 stent technique, and 70 (22) underwent FKBI. |
| 2 stent | 328 | 94 (29) | 205 (63) | 17 (5) | 12 (4) | 325 (99) | 20.7 ± 10.1 | 287 (99) | |
| Kim et al (SMART STRATEGY II),30 2020 | Pro | 23 | 23 (100) | 0 | 0 | 0 | 23 (100) | NA | 16 (70) |
| 2 stent | 23 | 23 (100) | 0 | 0 | 0 | 23 (100) | NA | 22 (96) | |
| Hildick-Smith et al (EBC MAIN),14 2021 | Pro | 230 | 230 (100) | 0 | 0 | 0 | 227 (99) | 5.8 ± 4.0 | 202 (89) patients underwent first kissing balloon inflation after first stent implantation. 51 (22) patients underwent 2 stent technique and underwent FKBI. |
| 2 stent | 237 | 237 (100) | 0 | 0 | 0 | 237 (100) | 7.9 ± 5.7 | 217 (93) |
FKBI, final kissing balloon inflation; LAD, left anterior descending artery; LCX, left circumflex artery; LM, left main; NA, not available; PCI, percutaneous coronary intervention; Pro, provisional; RCA, right coronary artery; SB, side branch.
Outcomes
In the direct comparison meta-analysis, 2-stent techniques significantly decreased the primary end point (HR, 0.76; 95% CI, 0.59-0.97; P = .03), TVMI (HR, 0.38; 95% CI, 0.20-0.71; P = .002), and TVR (HR, 0.66; 95% CI, 0.47-0.93; P = .02) with numerically lower TLR (HR, 0.67; 95% CI, 0.45-1.01; P = .06) than a provisional technique (Figure 2). There were no significant differences in all-cause mortality (HR, 0.94; 95% CI, 0.62-1.45; P = .79), cardiovascular mortality (HR, 0.82; 95% CI, 0.49-1.38; P = .45), MI (HR, 1.00; 95% CI, 0.73-1.37; P = .99), and ST (HR, 0.86; 95% CI, 0.52-1.44; P = .58) (Figure 2). The definitions of the MACE used in each trial are listed in Supplemental Table S2. There was no significant heterogeneity among studies. Funnel plots did not show a significant publication bias for any of the outcomes assessed (Supplemental Figure S2).
Figure 2.
Effect of bifurcation percutaneous coronary intervention techniques on each end point. Forest plot showing the risk of (A) major adverse cardiovascular events, (B) all-cause mortality, (C) cardiovascular death, (D) myocardial infarction, (E) target vessel myocardial infarction, (F) target lesion revascularization, (G) target vessel revascularization, and (H) stent thrombosis. IV, inverse variance.
A sensitivity analysis that restricted studies to newer-generation DES use in >50% of patients (>99% of patients received newer-generation DES) showed largely similar results (Supplemental Figure S3). A sensitivity analysis, in which studies were stratified by DKCRUSH trials versus non-DKCRUSH trials, showed significant subgroup differences in MACE (Supplemental Figure S4). A sensitivity analysis stratified by trials that compared bifurcation PCI techniques only for the left main artery versus other trials did not show significant subgroup differences for each end point tested (Supplemental Figure S5).
Network meta-analysis
The 2-stent group in the DEFINITION II trial was classified into the DK crush group given that 77.8% of patients received DK crush stenting. The 2-stent group in the EBC MAIN trial was classified into culotte as >50% of patients received the culotte technique. The results from the network meta-analysis are shown in Supplemental Figures S6-S12. The DK crush technique significantly decreased MACE than the culotte technique (HR, 0.43; 95% CI, 0.32-0.59), other 2-stent techniques (HR, 0.53; 95% CI, 0.33-0.85), and the provisional approach (HR, 0.48; 95% CI, 0.37-0.63) (Supplemental Figure S6). The DK crush technique significantly decreased the TLR than the culotte technique (HR, 0.41; 95% CI, 0.22-0.75), other 2-stent techniques (HR, 0.32; 95% CI, 0.12-0.81), and the provisional technique (HR, 0.42; 95% CI, 0.26-0.67) (Supplemental Figure S7). There was no significant heterogeneity and inconsistency for these analyses for the primary end point and TLR. There were no significant differences between any techniques for all-cause mortality, cardiovascular death, and MI (Supplemental Figures S8-S10), and there was no significant heterogeneity and inconsistency for these analyses. There were no significant differences between any techniques for TVR and ST (Supplemental Figures S11 and S12), but there was a significant heterogeneity and inconsistency for these analyses. The P-score analyses demonstrated that the DK crush technique was most likely the best treatment for all end points (Central Illustration).
Central Illustration.
The P-score analysis and ranking of each PCI technique for bifurcation lesions. A higher value of P-score means a higher likelihood that therapy is more effective.
Discussion
The main findings of the present study can be summarized as follows: (1) 2-stent techniques significantly decreased the primary end point, as well as rates of TVMI and TVR than a provisional technique; (2) when using a 2-stent strategy, the DK crush technique significantly decreased the primary end point and TLR than other techniques; and (3) there were no significant differences between any PCI techniques for hard end points, including all-cause mortality, cardiovascular death, and ST.
Prior studies did not show superiority of 2-stent techniques over provisional 1-stent techniques, and 2-stent techniques were associated with prolonged procedure time, increased contrast use, and increased radiation exposure.11,12,14 Currently, the provisional approach with the philosophy of “keep it simple and safe” is the standard approach for most noncomplex bifurcated lesions.6,7 In contrast, DKCRUSH trials showed the superiority of 2-stent techniques over provisional stenting in complex true bifurcation lesions,8,9 and most recent guidelines recommend 2-stent techniques only in patients with complex bifurcated lesions with SB length of >5 mm, SB diameter of ≥2.75 mm, and difficulty accessing the SB after main vessel stenting.6
There are a few prior meta-analyses that included several studies in which first-generation DES were implanted in a significant proportion of patients.31,32 For example, Ford et al31 demonstrated that a provisional strategy is associated with a reduction of all-cause mortality compared with 2-stent techniques at a mean follow-up period of 3.1 years. Di Gioia et al32 reported that the DK crush technique is associated with fewer MACE defined as a composite of cardiac death, MI, and TLR driven by lower rates of repeat revascularization, and showed a clinical benefit of 2-stent techniques over provisional stenting in bifurcation with SB lesion length of ≥10 mm at a median follow-up period of 12 months. The main limitation of these studies was the difficulty applying the findings to contemporary clinical practice with newer-generation stents. Our study overcame the limitation of previous studies and showed improved outcomes of 2-stent techniques in the modern practice with newer-generation DES.
The introduction of DES has been critical to the success of PCIs in the prevention of restenosis.33 Furthermore, the use of newer-generation DES, compared with first-generation DES, is associated with reduced rates of restenosis and ST.34,35 Newer-generation DES have become the most widely used DES worldwide, replacing bare-metal stents and first-generation DES. The NBBS IV study demonstrated that newer-generation stents decreased MACE, a composite of cardiac death, MI, TLR, and definite ST, by 50% in the 2-stent technique group in complex bifurcation lesions compared with first-generation stents.26 Similarly, a retrospective study showed that the use of second-generation DES was associated with a significantly reduced risk of 5-year target lesion failure than the use of first-generation DES among patients treated with PCIs for bifurcation lesions.36 The improved features of newer-generation DES, such as thinner strut, open-cell design, decreased links, and conformability, might be associated with a safety gain in expanding SB stents in 2-stent techniques. Furthermore, more biocompatible polymers, improved pharmacokinetics of eluting drugs, use of intracoronary imaging, which allows precise stenting in complex bifurcation lesions,37 and more routine high-pressure postdilatation might be associated with the improved safety of 2-stent techniques.
Recently, the DEFINITION II trial showed that the 2-stent approach was associated with a significant improvement in TVMI and TLR, resulting in fewer 1-year target lesion failures compared with the provisional approach.10
We demonstrated that a 2-stent technique is associated with a lower risk of TVMI than provisional stenting with newer-generation DES. The analysis included 2 trials9,10 in which the DK crush technique was used in most patients; thus, the evidence is largely from trials incorporating patients treated with the DK crush technique. Lower rates of restenosis in the SB in the DK crush group and a higher rate of the carina shifting, plaque shifting, and SB recoiling in the provisional stenting group are proposed as potential explanations for the DK crush technique being associated with improved acute gain and late loss of SB fractional flow reserve compared with provisional stenting.23 Other studies showed that the DK crush technique increased the rate of satisfactory final kissing balloon inflation than other techniques, and it was associated with less TLR and a significantly higher SB fractional flow reserve after PCI,38,39 which might explain the lower risk for TVMI in the 2-stent group in our study.
Our network meta-analysis demonstrated that the DK crush technique might be one of the most effective techniques among the 2-stent techniques. A study showed that the DK crush technique decreased the risk of in-stent restenosis and ostial restenosis in the SB compared with the culotte technique.24 Longer total stent length, increased area of overlapping stents, and suboptimal apposition of struts at the SB ostium in the culotte technique might explain this difference.27,40 More detailed information such as stent configuration or strut gap after each bifurcation PCI technique needs to be further investigated to better explain the different outcomes of each 2-stent technique.
There are several limitations to our study. First, this is a meta-analysis of trial-level data. Thus, we could not fully account for differences in trial design, treatment regimens, and individual patient data. Second, although most studies examined a bifurcation stent strategy using second-generation DES, some studies included patients receiving a first-generation DES. However, a sensitivity analysis in which >99% of patients received newer-generation DES showed concordant results with the main analysis. Third, there were insufficient data of angiographic findings, laboratory data, characteristics of the PCI culprit vessels, and perioperative medications to further evaluate differences between PCI techniques. Thus, the association between these unmeasured confounders cannot be assessed. Fourth, sensitivity analyses for acute coronary syndrome or length of the side branch lesions were not assessed because of a lack of enough studies to perform these analyses. Fifth, our study included DKCRUSH studies conducted by the same group of researchers, and those studies might need validation by other groups. Finally, moderate heterogeneity was observed for MACE and TLRs in the main analysis; however, we performed sensitivity network meta-analyses with random-effects models, and heterogeneity was no longer observed.
Conclusion
In this era of newer-generation DES, a 2-stent approach, especially the DK crush technique, is superior to a provisional stenting technique for bifurcation lesions, with a significant reduction in MACE, TVMI, and revascularization. Our analysis afforded the unique opportunity to comprehensively assess the outcomes of different bifurcation PCI techniques in the modern era. Further RCTs are warranted to investigate new approaches and technologies to improve outcomes for patients with bifurcation lesions.
Acknowledgments
Declaration of competing interest
Dr Latib is a consultant and on the advisory board of Medtronic, Abbott, Boston Scientific, and Philips. Dr Bangalore is an advisory board member for Abbott Vascular, Biotronik, Amgen, Pfizer, and Reata. Drs Fujisaki, Kuno, Numasawa, Takagi, Briasoulis, Kwan, and Tamis-Holland reported no financial interests.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics statement
This study was conducted in accordance with ethical regulatory requirements.
Footnotes
To access the supplementary material accompanying this article, visit the online version of the Journal of the Society for Cardiovascular Angiography & Interventions at 10.1016/j.jscai.2022.100410.
Supplementary material
References
- 1.Collins N., Seidelin P.H., Daly P., et al. Long-term outcomes after percutaneous coronary intervention of bifurcation narrowings. Am J Cardiol. 2008;102(4):404–410. doi: 10.1016/j.amjcard.2008.03.075. [DOI] [PubMed] [Google Scholar]
- 2.Tsuchida K., Colombo A., Lefèvre T., et al. The clinical outcome of percutaneous treatment of bifurcation lesions in multivessel coronary artery disease with the sirolimus-eluting stent: insights from the Arterial Revascularization Therapies Study part II (ARTS II) Eur Heart J. 2007;28(4):433–442. doi: 10.1093/eurheartj/ehl539. [DOI] [PubMed] [Google Scholar]
- 3.Kuno T., Sugiyama T., Imaeda S., et al. Novel insights of jailed balloon and jailed corsair technique for percutaneous coronary intervention of bifurcation lesions. Cardiovasc Revasc Med. 2019;20(12):1065–1072. doi: 10.1016/j.carrev.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 4.Grundeken M.J., Wykrzykowska J.J., Ishibashi Y., et al. First generation versus second generation drug-eluting stents for the treatment of bifurcations: 5-year follow-up of the LEADERS all-comers randomized trial. Catheter Cardiovasc Interv. 2016;87(7):E248–E260. doi: 10.1002/ccd.26344. [DOI] [PubMed] [Google Scholar]
- 5.Raphael C.E., O’Kane P.D., Johnson T.W., et al. Evolution of the crush technique for bifurcation stenting. JACC Cardiovasc Interv. 2021;14(21):2315–2326. doi: 10.1016/j.jcin.2021.08.048. [DOI] [PubMed] [Google Scholar]
- 6.Neumann F.J., Sousa-Uva M., Ahlsson A., et al. 2018 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention. 2019;14(14):1435–1534. doi: 10.4244/EIJY19M01_01. [DOI] [PubMed] [Google Scholar]
- 7.Burzotta F., Lassen J.F., Lefèvre T., et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15th consensus document from the European Bifurcation Club. EuroIntervention. 2021;16(16):1307–1317. doi: 10.4244/EIJ-D-20-00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S.L., Santoso T., Zhang J.J., et al. Clinical outcome of double kissing crush versus provisional stenting of coronary artery bifurcation lesions: the 5-year follow-up results from a randomized and multicenter DKCRUSH-II study (randomized study on double kissing crush technique versus provisional stenting technique for coronary artery bifurcation lesions) Circ Cardiovasc Interv. 2017;10(2) doi: 10.1161/CIRCINTERVENTIONS.116.004497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen X., Li X., Zhang J.J., et al. 3-year outcomes of the DKCRUSH-V trial comparing DK crush with provisional stenting for left main bifurcation lesions. JACC Cardiovasc Interv. 2019;12(19):1927–1937. doi: 10.1016/j.jcin.2019.04.056. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J.J., Ye F., Xu K., et al. Multicentre, randomized comparison of two-stent and provisional stenting techniques in patients with complex coronary bifurcation lesions: the DEFINITION II trial. Eur Heart J. 2020;41(27):2523–2536. doi: 10.1093/eurheartj/ehaa543. [DOI] [PubMed] [Google Scholar]
- 11.Ferenc M., Gick M., Kienzle R.P., et al. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J. 2008;29(23):2859–2867. doi: 10.1093/eurheartj/ehn455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colombo A., Bramucci E., Saccà S., et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) study. Circulation. 2009;119(1):71–78. doi: 10.1161/CIRCULATIONAHA.108.808402. [DOI] [PubMed] [Google Scholar]
- 13.Hildick-Smith D., de Belder A.J., Cooter N., et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010;121(10):1235–1243. doi: 10.1161/CIRCULATIONAHA.109.888297. [DOI] [PubMed] [Google Scholar]
- 14.Hildick-Smith D., Egred M., Banning A., et al. The European bifurcation club Left Main Coronary Stent study: a randomized comparison of stepwise provisional vs. systematic dual stenting strategies (EBC MAIN) Eur Heart J. 2021;42(37):3829–3839. doi: 10.1093/eurheartj/ehab283. [DOI] [PubMed] [Google Scholar]
- 15.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 16.Kuno T., Takagi H., Ando T., et al. Oral anticoagulation for patients with atrial fibrillation on long-term hemodialysis. J Am Coll Cardiol. 2020;75(3):273–285. doi: 10.1016/j.jacc.2019.10.059. [DOI] [PubMed] [Google Scholar]
- 17.Sterne J.A.C., Savović J., Page M.J., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 18.Neupane B., Richer D., Bonner A.J., Kibret T., Beyene J. Network meta-analysis using R: a review of currently available automated packages. PLoS One. 2014;9(12) doi: 10.1371/journal.pone.0115065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rücker G. Network meta-analysis, electrical networks and graph theory. Res Synth Methods. 2012;3(4):312–324. doi: 10.1002/jrsm.1058. [DOI] [PubMed] [Google Scholar]
- 20.You R., Cao Y.S., Huang P.Y., et al. The changing therapeutic role of chemo-radiotherapy for loco-regionally advanced nasopharyngeal carcinoma from two/three-dimensional radiotherapy to intensity-modulated radiotherapy: a network meta-analysis. Theranostics. 2017;7(19):4825–4835. doi: 10.7150/thno.21815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ribassin-Majed L., Marguet S., Lee A.W.M., et al. What is the best treatment of locally advanced nasopharyngeal carcinoma? An individual patient data network meta-analysis. J Clin Oncol. 2017;35(5):498–505. doi: 10.1200/JCO.2016.67.4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruiz-Salmerón R.J., Valenzuela L.F., Pérez I., et al. Approach to coronary bifurcation lesions using the everolimus-eluting stent: comparison between a simple strategy and a complex strategy with T-stenting. Rev Esp Cardiol (Engl Ed) 2013;66(8):636–643. doi: 10.1016/j.rec.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Ye F., Chen S.L., Zhang J.J., et al. Hemodynamic changes of fractional flow reserve after double kissing crush and provisional stenting technique for true bifurcation lesions. Chin Med J (Engl) 2012;125(15):2658–2662. [PubMed] [Google Scholar]
- 24.Chen S.L., Xu B., Han Y.L., et al. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013;61(14):1482–1488. doi: 10.1016/j.jacc.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 25.Kim Y.H., Lee J.H., Roh J.H., et al. Randomized comparisons between different stenting approaches for bifurcation coronary lesions with or without side branch stenosis. JACC Cardiovasc Interv. 2015;8(4):550–560. doi: 10.1016/j.jcin.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 26.Kumsars I., Holm N.R., Niemelä M., et al. Randomised comparison of provisional side branch stenting versus a two-stent strategy for treatment of true coronary bifurcation lesions involving a large side branch: the Nordic-Baltic Bifurcation Study IV. Open Heart. 2020;7(1) doi: 10.1136/openhrt-2018-000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hildick-Smith D., Behan M.W., Lassen J.F., et al. The EBC TWO study (European Bifurcation Coronary Two): a randomized comparison of provisional T-stenting versus a systematic 2 stent culotte strategy in large caliber true bifurcations. Circ Cardiovasc Interv. 2016;9(9) doi: 10.1161/CIRCINTERVENTIONS.115.003643. [DOI] [PubMed] [Google Scholar]
- 28.Ferenc M., Gick M., Comberg T., et al. Culotte stenting vs. TAP stenting for treatment of de-novo coronary bifurcation lesions with the need for side-branch stenting: the Bifurcations Bad Krozingen (BBK) II angiographic trial. Eur Heart J. 2016;37(45):3399–3405. doi: 10.1093/eurheartj/ehw345. [DOI] [PubMed] [Google Scholar]
- 29.Zhang L., Zhong W., Luo Y., Chen L. A pilot study on culottes versus crossover single stenting for true coronary bifurcation lesions. Acta Cardiol Sin. 2016;32(4):450–459. doi: 10.6515/ACS20151112A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim J., Lee J.M., Park T.K., et al. Optimal strategy for side branch treatment in patients with left main coronary bifurcation lesions. Rev Esp Cardiol (Engl Ed) 2021;74(8):691–699. doi: 10.1016/j.rec.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 31.Ford T.J., McCartney P., Corcoran D., et al. Single- versus 2-stent strategies for coronary bifurcation lesions: a systematic review and meta-analysis of randomized trials with long-term follow-up. J Am Heart Assoc. 2018;7(11) doi: 10.1161/JAHA.118.008730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Di Gioia G., Sonck J., Ferenc M., et al. Clinical outcomes following coronary bifurcation PCI techniques: a systematic review and network meta-analysis comprising 5,711 patients. JACC Cardiovasc Interv. 2020;13(12):1432–1444. doi: 10.1016/j.jcin.2020.03.054. [DOI] [PubMed] [Google Scholar]
- 33.Bangalore S., Kumar S., Fusaro M., et al. Short- and long-term outcomes with drug-eluting and bare-metal coronary stents: a mixed-treatment comparison analysis of 117 762 patient-years of follow-up from randomized trials. Circulation. 2012;125(23):2873–2891. doi: 10.1161/CIRCULATIONAHA.112.097014. [DOI] [PubMed] [Google Scholar]
- 34.Jensen L.O., Thayssen P., Christiansen E.H., et al. Safety and efficacy of everolimus- versus sirolimus-eluting stents: 5-year results from SORT OUT IV. J Am Coll Cardiol. 2016;67(7):751–762. doi: 10.1016/j.jacc.2015.11.051. [DOI] [PubMed] [Google Scholar]
- 35.Räber L., Magro M., Stefanini G.G., et al. Very late coronary stent thrombosis of a newer-generation everolimus-eluting stent compared with early-generation drug-eluting stents: a prospective cohort study. Circulation. 2012;125(9):1110–1121. doi: 10.1161/CIRCULATIONAHA.111.058560. [DOI] [PubMed] [Google Scholar]
- 36.Choi K.H., Song Y.B., Lee J.M., et al. Differential long-term effects of first- and second-generation DES in patients with bifurcation lesions undergoing PCI. JACC: Asia. 2021;1(1):68–79. doi: 10.1016/j.jacasi.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Räber L., Mintz G.S., Koskinas K.C., et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2018;39(35):3281–3300. doi: 10.1093/eurheartj/ehy285. [DOI] [PubMed] [Google Scholar]
- 38.Chen S.L., Zhang J.J., Ye F., et al. Study comparing the double kissing (DK) crush with classical crush for the treatment of coronary bifurcation lesions: the DKCRUSH-1 Bifurcation Study with drug-eluting stents. Eur J Clin Invest. 2008;38(6):361–371. doi: 10.1111/j.1365-2362.2008.01949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ye F., Zhang J.J., Tian N.L., et al. The acute changes of fractional flow reserve in DK (Double Kissing), crush, and 1-stent technique for true bifurcation lesions. J Interv Cardiol. 2010;23(4):341–345. doi: 10.1111/j.1540-8183.2010.00568.x. [DOI] [PubMed] [Google Scholar]
- 40.Finn A.V., Kolodgie F.D., Harnek J., et al. Differential response of delayed healing and persistent inflammation at sites of overlapping sirolimus- or paclitaxel-eluting stents. Circulation. 2005;112(2):270–278. doi: 10.1161/CIRCULATIONAHA.104.508937. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.