Atrial functional mitral regurgitation (aFMR) represents a subtype of secondary mitral regurgitation (MR) closely associated with left atrial (LA) enlargement and mitral annular dilation in the setting of preserved left ventricular ejection fraction (LVEF), absence of primary mitral valve pathology, and commonly, presence of atrial fibrillation (AF).1, 2, 3 However, there is no consensus on a unified definition of aFMR. Published studies had different cutoffs for LVEF, LA volume index, and left ventricular dimensions. Some studies did not require AF to be present, while others considered AF to be one of the determinants of aFMR (Supplemental Table S1). Recently, studies have reported results for patients with aFMR undergoing mitral transcatheter edge-to-edge repair (mTEER). In this meta-analysis, we pooled the clinical and echocardiographic outcomes to provide further insights into this topic.
We performed a literature search using Medline, EMBASE, and CENTRAL databases through December 31, 2022, using search terms “transcatheter edge-to-edge repair,” “TEER,” “atrial functional mitral regurgitation,” and “aFMR.” We included studies reporting the association of mTEER with all-cause mortality, heart failure (HF) hospitalization, reduction in MR, and improvement in New York Heart Association (NYHA) class III to IV in patients with aFMR. We extracted outcomes at the maximum follow-up duration. Two authors (T.H. and S.U.K.) independently conducted the study search and selection process and abstracted and appraised the data. We performed a random-effects meta-analysis and measured risk ratios (RRs) for categorical outcomes and mean differences (MDs) for continuous outcomes with 95% CIs before and after mTEER. We used I2 statistics to measure statistical heterogeneity (I2 ≥ 50%: high heterogeneity). For all analyses, statistical significance was set at 5%; we used Comprehensive Meta-analysis V 3.0 (Biostat).
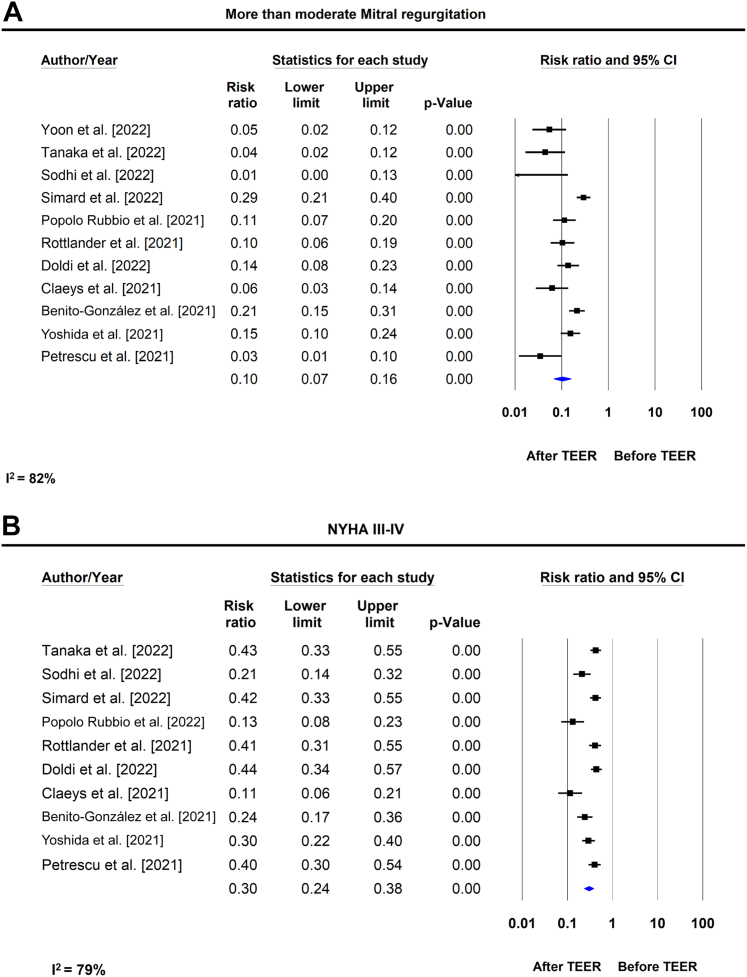
Of 3328 citations, 11 observational studies (n = 738) were selected (Tanaka et al,2 Doldi et al,3 and Petrescu et al4 and PMIDs 36075642, 33612563, 34826500, 35312231, 35535629, 34610357, 36075643, and 34794621). The median age was 80 (Q1-Q3, 79-82) years, 60% were women, and 85% had AF. The mean (SD) number of devices was 1.5 (0.6). The final mean mitral gradient was 3.6 (0.4) mm Hg (reported in 6 studies). For echocardiographic parameters, 5 of 11 studies reported pre- and post-mTEER outcomes. At a median follow-up of 1 year (Q1-Q3, 1-2), the pooled all-cause mortality was 12% (95% CI, 8.1%-17.4%) and HF hospitalization was 8.5% (95% CI, 4.8%-14.6%) after mTEER. Before mTEER, the mean (SD) LA volume index was 74 (18) mL/m2, left ventricular end-diastolic dimension was 48 (1) mm, and LVEF was 56% (3). mTEER was associated with a significant reduction in LA volume index (MD, −19.1; 95% CI, −23.8 to −14.4; I2 = 0) and left ventricular end-diastolic dimension (MD, −3.4; 95% CI, −6.4 to −0.3; I2 = 87%). However, there was no significant change in LVEF after mTEER (MD, 0.02%; 95% CI, −0.05 to 0.01; I2 = 73%). At baseline, the proportions of patients with MR grade ≥3+ and 4+ were 95.4% (95% CI, 89.5%-98.1%) and 51.4% (95% CI, 42.7%-60.1%), respectively. After mTEER, only 7.1% (95% CI, 3.9%-12.4%) had residual MR >3+ (RR, 0.09; 95% CI, 0.05-0.19; I2 = 82%), whereas 74.9% (95% CI, 62.2%-84.4%) achieved an MR of ≤1+, and 90.8% (95% CI, 85.5%-94.3%) achieved an MR of ≤2+. At baseline, 85.9% (95% CI, 77.7%-91.4%) patients were in NYHA class III to IV; after mTEER, 26% (95% CI, 19%-34%) of patients had NYHA III/IV (RR, 0.32; 95% CI, 0.24-0.38; I2 = 79%) (Figure 1).
Figure 1.
Effect of mitral transcatheter edge-to-edge repair therapy on (A) residual moderate mitral regurgitation (≥3) and (B) New York Heart Association Class III/IV in patients with atrial functional mitral regurgitation. NYHA, New York Heart Association; TEER, transcatheter edge-to-edge repair.
In this meta-analysis, mTEER was associated with a low all-cause and low rate of HF hospitalization in patients with aFMR, the majority of whom had AF. The majority of patients (60%) were women, which can be attributed to the fact that most female patients with secondary MR are labeled as having disproportionate MR even when having a severely dilated left ventricle. This highlights the significance of having sex-specific echocardiographic cutoffs that can help better identify patients that will most likely benefit from mTEER.5 Furthermore, mTEER significantly reduced LA volume index and MR severity and improved NYHA functional class. The reduction of LA volume index is likely related to reduced MR, which is associated with improvement in symptoms.1 These results are congruent with the recently published Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation trial showing similar outcomes at 2 years between FMR secondary to LA enlargement or AF compared with other mechanisms of functional MR.6 Limitations of this study include reliance on study-level information, small sample size, short follow-up, and variable definitions of end points across trials. In addition, a unified definition of aFMR is currently lacking, and therefore, patients included in various studies may be different and not entirely comparable. Our findings emphasize the importance of conducting randomized controlled trials in this patient population to validate and corroborate our results. In conclusion, mTEER in aFMR is a feasible and effective treatment.
Acknowledgments
Declaration of competing interest
Michael J. Reardon is a consultant for Medtronic, Boston Scientific, Abbott, and W L Gore & Associates. Marvin D. Atkins is a consultant for W L Gore & Associates. Neal S. Kleiman is a local principal investigator in trials sponsored by Abbott, Boston Scientific, Edwards Lifesciences, and Medtronic. Sachin S. Goel is a consultant for Medtronic and W. L. Gore & Associates and is on the speaker bureau for Abbott Structural Heart. Taha Hatab, Safi Khan, Hassaan Arshad, Syed Zaid, Priscilla Wessly, Nadeen Faza, Stephen Little, and William Zoghbi reported no financial interests.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics statement and patient consent
The current study strictly adhered to the relevant ethical guidelines, ensuring the protection of human subjects' rights.
Footnotes
To access the supplementary material accompanying this article, visit the online version of the Journal of the Society for Cardiovascular Angiography & Interventions at 10.1016/j.jscai.2023.101050.
Supplementary material
References
- 1.Alkhouli M., Hahn R.T., Petronio A.S. Transcatheter edge-to-edge repair for atrial functional mitral regurgitation: effective therapy or elusive target? J Am Coll Cardiol Intv. 2022;15(17):1741–1747. doi: 10.1016/j.jcin.2022.06.035. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka T., Sugiura A., Öztürk C., et al. Transcatheter edge-to-edge repair for atrial secondary mitral regurgitation. J Am Coll Cardiol Intv. 2022;15(17):1731–1740. doi: 10.1016/j.jcin.2022.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Doldi P., Stolz L., Orban M., et al. Transcatheter mitral valve repair in patients with atrial functional mitral regurgitation. J Am Coll Cardiol Img. 2022;15(11):1843–1851. doi: 10.1016/j.jcmg.2022.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Petrescu A., Geyer M., Ruf T., et al. Edge-to-edge transcatheter valve repair of atrial functional mitral regurgitation positively influences atrial pathology. Eur Heart J. 2021;42(suppl 1) [Google Scholar]
- 5.Shah S.V., Bavry A.A., Kumbhani D.J. Transcatheter mitral valve edge-to-edge repair for secondary mitral regurgitation: why sex matters. Circulation. 2021;143(7):621–623. doi: 10.1161/CIRCULATIONAHA.120.052345. [DOI] [PubMed] [Google Scholar]
- 6.Cavalcante J.L., Asch F.M., Garcia S., et al. Functional mitral regurgitation staging and its relationship to outcomes in the COAPT trial. J Am Coll Cardiol Intv. 2022;15(17):1773–1775. doi: 10.1016/j.jcin.2022.07.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.