Each year at the Society for Cardiovascular Angiography & Interventions (SCAI) Annual Scientific Sessions meeting, collaborative think tanks involving interventional cardiologists, administrative partners, and members of industry are convened for each SCAI clinical practice area to discuss topics of particular interest to the group. This document presents the proceeding of the 2023 structural heart disease session, which focused on treating patients with symptomatic severe aortic stenosis (AS). The hope for this discussion was to identify the needs and promote actions by the participants, leading to a positive impact on patient care.
As transcatheter aortic valve replacement (TAVR) has become the dominant treatment for patients with severe symptomatic AS, research has focused on whether a broader group of patients, including those with asymptomatic severe AS or moderate AS, may benefit from TAVR. However, the underutilization of TAVR among patients with symptomatic severe AS receives inadequate attention. A study of 366,909 patients hospitalized for aortic valve disease from 2012 through 2016 found that 73.4% did not undergo valve replacement despite clear evidence of higher short-term mortality in patients with medically managed disease.1 Additionally, ageism may contribute to the underreferral of patients with known symptomatic severe AS to a multidisciplinary heart valve team, with 46.0% of patients aged <65 years undergoing valve replacement compared with only 20.5% of patients aged 85 years. SCAI convened a Think Tank with industry partners to explore the causes of AS undertreatment and to develop solutions to maximize access to TAVR.
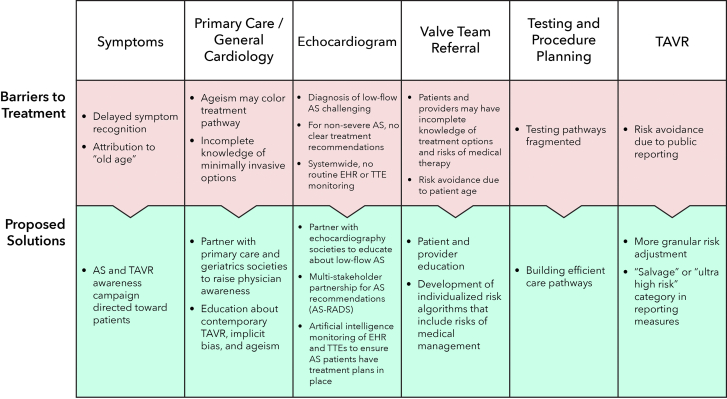
Potential causes of AS undertreatment include patient-level, diagnostic, and health care system factors (Figure 1). At the individual patient level, older patients generally have more comorbidities and greater risk for any invasive procedure. Although age is an important predictor for adverse outcomes in multivariable analyses, using age as a heuristic for treatment may exclude patients likely to benefit, as previously demonstrated in the case of coronary artery bypass grafting.2 From the patient’s perspective, exertional intolerance attributed to “normal aging” may instead indicate symptomatic AS. Both patients and providers may fear intervention in elderly and frail individuals, being unaware that contemporary TAVR carries much lower risk than TAVR even one decade ago, evolving from 24F sheaths, general anesthesia, and prolonged hospitalization to 14F sheaths, moderate sedation, and next-day discharge. TAVR in-hospital mortality is low in nonagenarians (1.8%) and octogenarians (1.5%), only slightly higher than in septuagenarians (0.9%; P < .01).3 Underrepresented minorities in particular may be underinformed about TAVR due to insufficient access to health care information. Elderly patients may struggle to comply with multiple medical appointments and tests in the process of AS work-up.
Figure 1.
Barriers to treatment are at the top with the proposed solutions on the bottom. AS, aortic stenosis; EHR, electronic health record; RADS, Reporting and Data System; TAVR, transcatheter aortic valve replacement; TTE, transthoracic echocardiogram
Diagnostically, there is heterogeneity in echocardiographic findings among patients with severe AS. While traditional, high-gradient AS (peak velocity > 4.0 m/s; mean gradient > 40 mm Hg) may be straightforward, diagnosing severe AS in low-flow states can be challenging and less likely to be referred for TAVR.4 In contrast to standardized reporting and follow-up recommendations for other disease states (ie, follow-up screening recommendations for pulmonary nodules or breast masses), there is an incomplete reporting paradigm regarding concrete next steps in patients with varying degrees of AS.
At the health care system and population level, data are limited regarding referral practices prior to presentation to the multidisciplinary heart valve team. The elective TAVR procedure is the last stop on a journey beginning with primary care and continuing with echocardiography. Prior to presentation to valve clinic, patients and providers may have inadequate or inaccurate assessments of individuals’ symptoms and risks, both procedural risks as well as risks associated with medical management. Furthermore, because all TAVR outcomes are reported publicly to the national Society for Thoracic Surgeons (STS) and the American College of Cardiology (ACC) Transcatheter Valve Therapy (TVT) Registry, certain operators or health care systems may shy away from treating patients who are at higher risk.
Faced with these barriers to TAVR access, the SCAI Think Tank identified potential actions to reduce undertreatment of severe AS. SCAI is poised to lead in implementing many of these recommendations, given its position as the global society representing interventional cardiology practitioners and patients. At the patient level, shared decisionmaking begins with providers delivering longitudinal care (ie, primary care, general cardiology). Given that most patients referred to the heart valve team are treated, identifying specific barriers to referral may ensure timely access to appropriate care. In place of the age heuristic to risk stratify patients, more granular risk scores encompassing broader criteria can identify not only patients for whom treatment may be suitable but also those for whom treatment may be futile.5 SCAI and industry partnerships with internal medicine and geriatrics societies may help raise awareness about contemporary transcatheter heart therapies to further inform patients and providers.
At the diagnostic level, SCAI’s partnership with cardiovascular imaging societies may help standardize echo-based reporting of AS severity including low gradient states and clarify the role of adjunctive assessments such as aortic valve calcium scoring and dobutamine stress echocardiography along with specific recommendations regarding follow-up and treatment. Such a partnership would be similar to the Breast Imaging Reporting and Data System collaboration among the American College of Radiology, American Medical Association, National Cancer Institute, Centers for Disease Control and Prevention, Food and Drug Administration, American College of Surgeons, and College of American Pathologists.
Within health care systems, establishment of streamlined referral pathways with seamless testing and evaluation may mitigate the burden of preprocedural evaluation for underserved and elderly populations. Artificial intelligence–based solutions to identify patients with AS and recommend an appropriate treatment plan may reduce undertreatment. Platforms such as mPirik (www.mpirik.com) and Egnite (www.egnitehealth.com) leverage advanced data processing and natural language processing tools to identify patients with specific disease states. Finally, Registry public reporting requires robust risk adjustment coupled with exceptions for salvage or other exceptionally high-risk procedures to combat the “risk-treatment” paradox.
Few medical interventions help patients both feel better and live longer, but appropriate TAVR does both. Given the time course over which severe AS develops, undertreatment of severe AS due to delayed presentation or incomplete risk/benefit profiling is a health care system failure and requires a multidisciplinary effort to identify patients and to deliver treatment. The SCAI Think Tank identified clear patient-level, diagnostic, and health care system factors contributing to the undertreatment of severe AS and offered specific, actionable solutions to mitigate these factors in order to provide timely treatment to appropriately selected patients.
Acknowledgments
Peer review statement
Associate Editor Andrew M. Goldsweig had no involvement in the peer review of this article and has no access to information regarding its peer review. Full responsibility for the editorial process for this article was delegated to Associate Editor Sandeep Nathan.
Declaration of competing interest
Amit N. Vora is a consultant to Medtronic. Wayne B. Batchelor is a consultant to Medtronic and Edwards Lifesciences. Ramesh Daggubati is a speaker at Medtronic. Sammy Elmariah is a consultant to Edwards Lifesciences and Medtronic. James B. Hermiller is a consultant to Edwards Lifesciences, Medtronic, and Abbott. Omar Khalique is a consultant to Edwards and Philips. Chad Kliger is a consultant to Siemens, Medtronic, and Edwards Lifesciences; is a speaker at Siemens, Medtronic, and Edwards Lifesciences; and is a Principal Investigator at Abbott, Edwards Lifesciences, Medtronic, and Siemens. Paul D. Mahoney is a consultant to Edwards Lifesciences, Medtronic, and Abbott. Kimberly A. Skelding is a proctor at Medtronic and reports honorarium from Medtronic. Triston B. B. J. Smith is a consultant to Edwards Lifesciences. Molly Szerlip is a speaker at Boston Scientific, Edwards Lifesciences, and Medtronic and is on the advisory board of Abbott Vascular. Andrew M. Goldsweig is a consultant to Philips and speaker at Philips and Edwards Lifesciences. Konstantinos Dean Boudoulas reported no financial interests. Michael Church is employed at Corazon. Natalie Contreras is employed at LiveNova. Mounia Haddad is employed at Boston Scientific. Novena Rangwala is employed at GE Healthcare. David Schleifer and Kristen Skelton are employed at Edwards Lifesciences. Lucy R. Schlueter is employed at Medtronic.
Funding sources
This work was not supported by funding agencies in the public, commercial, or not-for-profit sectors.
Ethics statement and patient consent
The authors adhered to the relevant ethical guidelines when developing this manuscript.
References
- 1.Goldsweig A.M., Tak H.J., Chen L.W., et al. The evolving management of aortic valve disease: 5-year trends in SAVR, TAVR, and Medical Therapy. Am J Cardiol. 2019;124(5):763–771. doi: 10.1016/j.amjcard.2019.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olenski A.R., Zimerman A., Coussens S., Jena A.B. Behavioral heuristics in coronary-artery bypass graft surgery. N Engl J Med. 2020;382(8):778–779. doi: 10.1056/NEJMc19112893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ismayl M., Abbasi M.A., Al-Abcha A., et al. Outcomes of transcatheter aortic valve implantation in Nonagenarians and Octogenarians (analysis from the national inpatient sample database) Am J Cardiol. 2023;199:59–70. doi: 10.1016/j.amjcard.2023.04.049. [DOI] [PubMed] [Google Scholar]
- 4.Li S.X., Patel N.K., Flannery L.D., et al. Trends in utilization of aortic valve replacement for severe aortic stenosis. J Am Coll Cardiol. 2022;79(9):864–877. doi: 10.1016/j.jacc.2021.11.060. [DOI] [PubMed] [Google Scholar]
- 5.Chuang M., Akodad M., Chatfield A., et al. Frailty assessment of transcatheter aortic valve replacement patients: contemporary practice and future directions. Structural Heart. 2021;5(4):357–366. doi: 10.1080/24748706.2021.1921318. [DOI] [Google Scholar]