Abstract
Objective
To evaluate the role of psychosocial well-being on perioperative pain and opioid use among patients with cleft lip and palate (CLP) undergoing alveolar bone grafting (ABG).
Design
Retrospective review.
Setting
Tertiary level craniofacial clinic.
Participants
34 patients with CLP (median age: 11.7 years), including 25 (73.5%) unilateral CLP and 9 (26.5%) bilateral CLP, who underwent ABG from 2015 to 2022.
Interventions
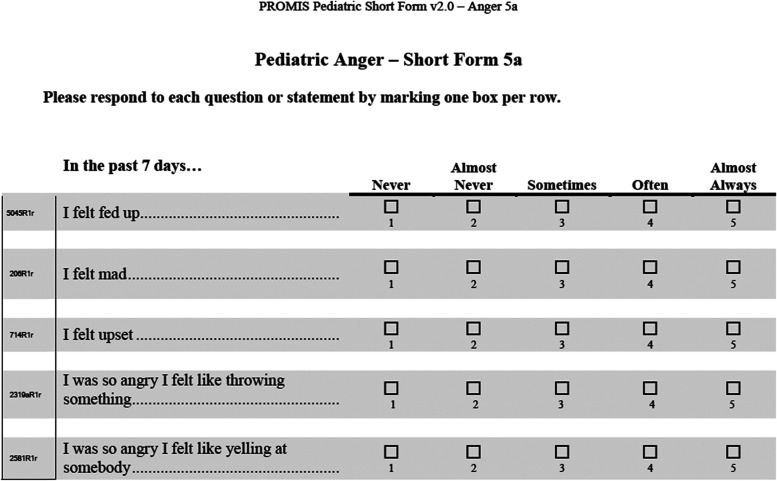
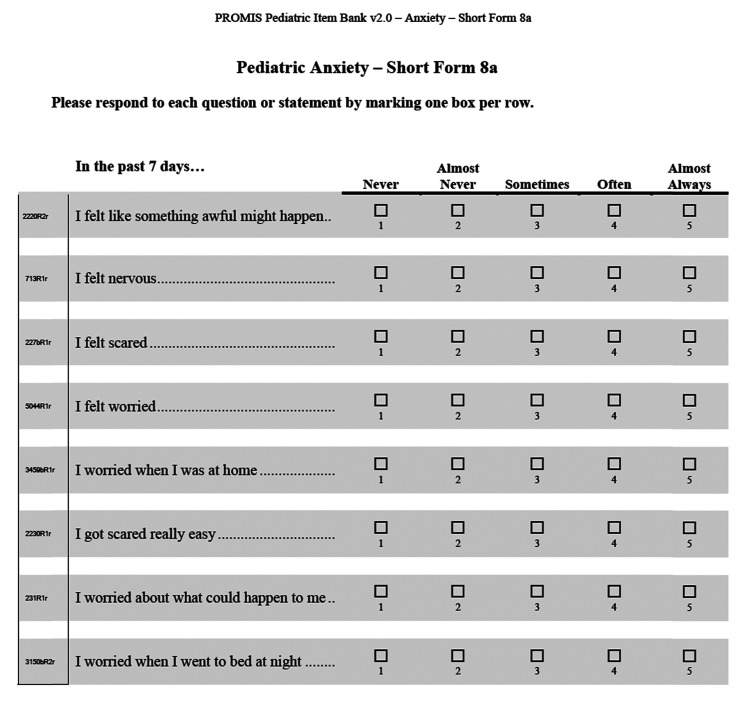
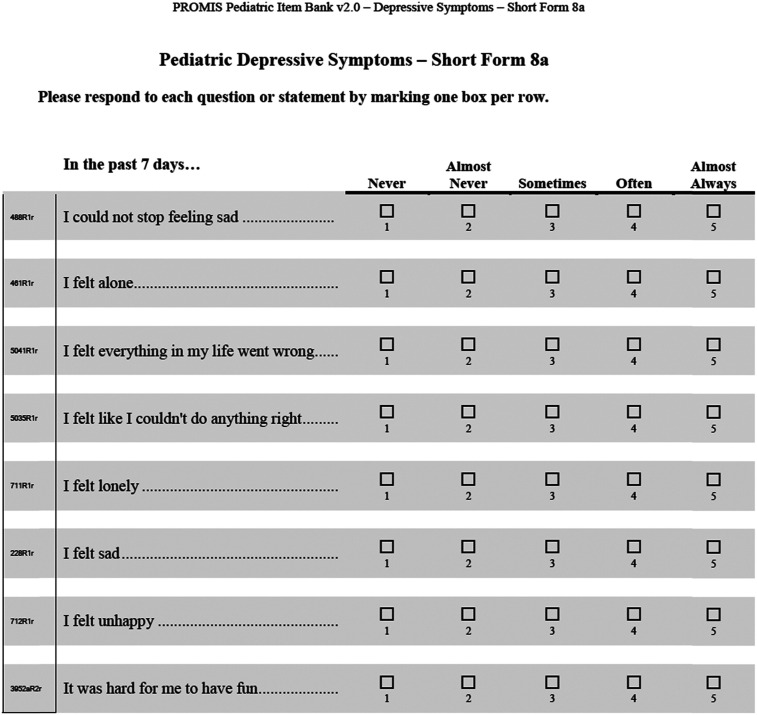
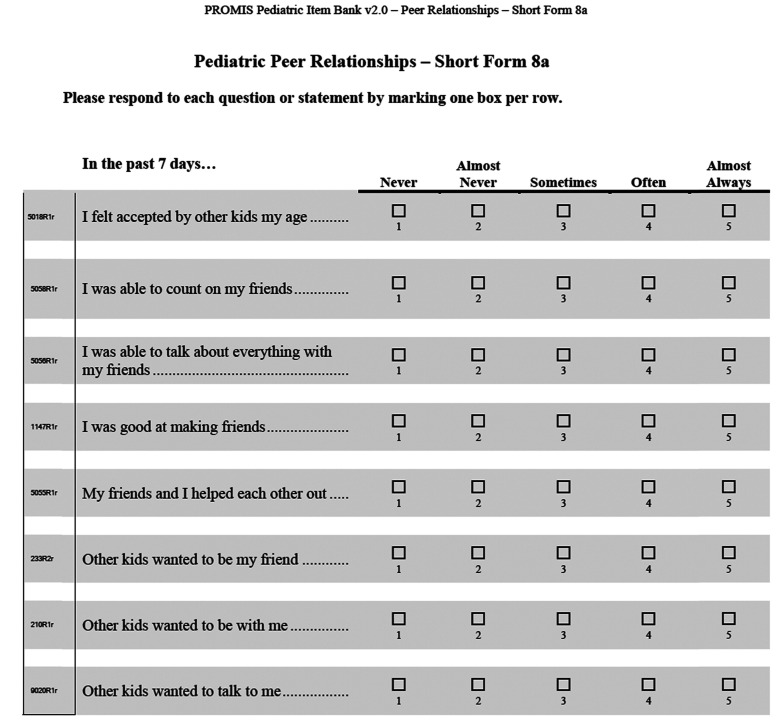
ABG using iliac crest bone graft. Patients were prospectively administered four patient-reported psychosocial instruments from the Patient-Reported Outcomes Measurement Information System.
Main Outcome Measures
Perioperative opioid use in morphine equivalent dosage/kilogram, patient-reported pain scores, and length of hospital stay after ABG.
Results
Patient-reported anxiety (r = 0.41, p = 0.02) and depressive symptoms (r = 0.35, p = 0.04) correlated to higher perioperative opioid usage. Multivariable regression models including psychosocial scores, total acetaminophen usage, length of surgery, and other simultaneous surgeries were developed for total opioid usage, patient-reported pain, and length of hospital stay. Patient-reported anxiety was independently predictive of higher perioperative opioid use (β=0.36, p = 0.01) and higher pain scores (β=0.39, p = 0.02), but not length of hospital stay.
Conclusions
We identified an association for patient-reported anxiety and perioperative opioid use and pain in a CLP cohort undergoing ABG. Future considerations in preoperative patient and family consultation may be indicated in patients self-reporting higher anxiety in an effort to minimize perioperative opioid usage.
Keywords: cleft lip and palate, perioperative opioid use, pain, length of hospital stay, psychosocial functioning, depressive symptoms, anxiety.
Introduction
Increasing awareness of the relationship between surgery and persistent opioid use has generated tremendous interest in identifying potential risk factors as well as developing methods for reducing perioperative opioid use.1–7 A 2018 study by Harbaugh et al. found that opioid-naïve patients aged 13 to 21 who underwent surgical procedures were more likely to refill their postoperative prescriptions and refill persistently 90 to 180 days after surgery, compared to an age-matched non-surgical group. 2 Within craniofacial surgery, patients born with cleft lip and palate (CLP) are particularly vulnerable to persistent opioid use given their inherently iterative reconstructive surgical care pathway. 8 Compared to a 0.1% incidence of long-term opioid use for non-surgical patients, patients who underwent CLP corrective surgery demonstrated a 4.4% incidence of long-term opioid use. 1 These findings highlight the need for careful consideration of perioperative opioid usage in patients with CLP.
A clear relationship between psychological distress and perioperative pain has been reported by a number of investigators.9–12 While the majority of the literature focused on adult populations, a recent prospective cohort study of 215 pediatric patients undergoing thumb carpometacarpal osteoarthritis surgery found that anxiety and pessimism were significant predictors for acute postoperative pain. 9 Among patients with CLP, there remains a paucity of reports assessing whether an association between psychosocial functioning and perioperative pain, and thereby opioid use, may exist. The purpose of this study is to explore the impact of patient-reported psychosocial functioning on perioperative opioid usage and pain in patients with CLP undergoing alveolar bone graft (ABG).
Methods
Patient Characteristics
Patients with a diagnosis of CLP at the University of California Los Angeles (UCLA) were enrolled as part of an ongoing longitudinal prospective study on psychosocial functioning of patients with cleft and craniofacial diagnoses between 2015 and 2022 (Institutional Review Board protocol no. 15-000979). Two independent reviewers (SM, JCL) extracted data from patient charts. Demographic and clinical characteristics were collected, including age at the time of surgery, sex, ethnicity, diagnosis, surgery type, and laterality of CLP. To determine the invasiveness of the procedure, the method of bone graft harvest was categorized as either open or trephine. Other simultaneous procedures that occurred during ABG were considered for analysis and included cleft nose revision, cleft lip revision, cleft nose and lip revision, dental extraction, palatal fistula closure, intermaxillary fixation screw placement, and pharyngoplasty port revision. Length of surgery was determined from the procedure start time to the procedure end time in minutes (min). The length of hospital stay was calculated from the procedure start time to discharge time in hours (hr). Postoperative patient-reported pain scores were taken as a subjective score out of 10, with scores of 1–3 considered mild, 4–6 considered moderate, 7–10 considered severe, and +10 considered breakthrough. Pain scores were taken by nursing staff every 2 h in the postoperative inpatient setting by verbal description and were recorded in the patients’ medical charts. Average pain scores were reported for each patient during their hospital stay. Furthermore, inpatient perioperative opioid medications were evaluated, including fentanyl, oxycodone, codeine, hydromorphone, and morphine. The medications were categorized into two groups: acetaminophen or cumulative opioids administered perioperatively. Acetaminophen dosages were considered for analysis in milligrams per kilogram weight of the patient at the time of surgery (mg/kg). Narcotic dosages were converted into morphine equivalent dosage (MED) for comparison and analyzed as MED per kilogram of patient weight (MED/kg). 13 This study received ethics approval from the University of California, Los Angeles Institutional Review Board protocol no. 15-000979.
Psychosocial Functioning
Validated, quantitative, and self-reported instruments from the Patient Reported Outcomes Measurement Information System (PROMIS) were administered during annual multidisciplinary craniofacial clinics.14–18 For each patient, the most proximate PROMIS score, either before or after the procedure, was considered to represent perioperative psychosocial functioning. Patients completed four PROMIS short form version 2.0 instruments, including Anger 5a, Anxiety 8a, Depressive Symptoms 8a, and Peer Relationships 8a. Raw scores were converted to standardized t scores set to the United States population with a mean score of 50 and a standard deviation of 10. 19
Statistical Analyses
To determine variables that are associated with perioperative opioid use, univariate analyses using Pearson correlations followed by multivariable linear regression analyses were performed. Perioperative opioid usage, patient-reported postoperative pain scores, and length of hospital stay (hr) were compared to various demographic and medical variables: total acetaminophen (mg/kg), length of surgery (min), laterality of CLP, gender, age at surgery, open bone graft harvest, other simultaneous procedures, and PROMIS scores. Multivariable models were developed incorporating significant demographic and clinical variables from the univariate analyses. Each significant PROMIS score was independently incorporated into the models to further evaluate the association between psychosocial functioning and perioperative opioid use. Data analyses were conducted using IBM SPSS Version 26 (IBM Corp., Armonk, N.Y.) with an alpha level of p < 0.05.
Results
Patient Characteristics
34 patients with CLP aged 8 to 24 years (median age of 11.7 years) who underwent ABG were included in this study. (Table 1). Patients were diagnosed with either unilateral (73.5%) or bilateral (26.5%) CLP. ABG was performed using iliac crest bone graft harvested via a trocar (50.0%) or open (50.0%) technique, and the surgery time averaged 144.1 min. More than half of the patients (61.8%) underwent ABG surgery simultaneously with other procedures. In addition, PROMIS scores were on average within one standard deviation of the national mean for anger (50.0 ± 9.0), anxiety (43.1 ± 7.9), depressive symptoms (49.8 ± 11.3), and peer relationships (45.9 ± 9.9). For 38% of the patients (n = 13), the most proximate PROMIS score was prior to surgery, and the rest only had postoperative scores.
Table 1.
Patient and Surgical Characteristics.
| Total Cohort (n = 34) | |
|---|---|
| Age at surgery, median (IQR), yr | 11.7 (10.1–13.7) |
| Weight at surgery, median (IQR), kg | 40.6 (29.2–51.6) |
| Male, n (%) | 21 (61.8) |
| Bilateral, n (%) | 9 (26.5) |
| More than one diagnosis, n (%) | 8 (23.5) |
| Bone graft harvest, n (%) | |
| Open | 17 (50.0) |
| Trephine | 17 (50.0) |
| Other simultaneous surgeries, n (%) | 21 (61.8) |
| Cleft nose revision | 9 (26.5) |
| Cleft lip revision | 4 (11.8) |
| Cleft nose and lip revision | 2 (5.9) |
| Dental extractions | 2 (5.9) |
| Other (palatal fistula closure, intermaxillary fixation screw placement, pharyngoplasty port revision) | 4 (11.8) |
| Length of surgery, mean ± SD, min | 144.1 ± 56.3 |
| Private insurance, n (%) | 13 (38.2) |
| Age at PROMIS, median (IQR), yr | 12.4 (11.1–15.1) |
| Time between surgery and PROMIS, median (IQR), yr | −0.63 (−2.2–0.3) |
| PROMIS scores, mean ± SD | |
| Peer relationships | 50.0 ± 9.0 |
| Anger | 43.1 ± 7.9 |
| Anxiety | 49.8 ± 11.3 |
| Depressive symptoms | 45.9 ± 9.9 |
IQR, interquartile range; SD, standard deviation; yr, years; kg, kilograms; min, minutes.
During their hospital stay, patients overall received a median (IQR) of 0.7 (0.4–1.0) MED/kg of total opioids perioperatively and 43.9 (22.6–60.1) mg/kg of acetaminophen (Table 2). Median postoperative pain scores were 0.5 (IQR: 0–1.9) and length of hospital stay was 26.0 (IQR: 22.0–28.0) hours.
Table 2.
Analgesic Medications, Patient-Reported Pain Scores, and Length of Hospital Stay.
| Total Cohort (n = 34) | |
|---|---|
| Analgesic medications | |
| Total opioids, median (IQR), MED/kg | 0.7 (0.4–1.0) |
| Perioperative opioids | 0.5 (0.4–0.8) |
| Fentanyl, IV | 0.4 (0.3–0.6) |
| Hydromorphone, IV | 0.1 (0–0.01) |
| Morphine, IV | 0 |
| Postoperative opioids | 0.1 (0–0.3) |
| Oxycodone, PO | 0.1 (0–0.3) |
| Codeine, PO | 0 |
| Hydromorphone, IV | 0 |
| Morphine, IV | 0 |
| Total acetaminophen, median (IQR), mg/kg | 43.9 (22.6–60.1) |
| Perioperative acetaminophen, IV | 15.0 (0–15.0) |
| Postoperative acetaminophen, PO | 30.0 (14.6–45.1) |
| Patient-reported pain scores, median (IQR) | 0.5 (0–1.9) |
| Length of hospital stay, median (IQR), hr | 26.0 (22.0–28.0) |
MED, morphine equivalent dose; IQR, interquartile range; IV, intravenous; PO, per os; kg, kilograms; hr, hours.
Correlations with Perioperative Opioid use, Pain, and Length of Hospital Stay
Demographic and clinical variables associated with perioperative opioid use, postoperative pain, and length of hospital stay were identified using Pearson correlations (Table 3). Total perioperative opioid use demonstrated a significant positive correlation with acetaminophen use (r = 0.54, p < 0.001), length of surgery (r = 0.39, p = 0.02), anxiety (r = 0.41, p = 0.02), and depressive symptoms (r = 0.35, p = 0.04). There were also significant positive relationships between patient-reported postoperative pain scores and acetaminophen use (r = 0.37, p = 0.03) and patient-reported anxiety scores (r = 0.44, p = 0.008). Additionally, increased length of hospital stay was significantly associated with elevated acetaminophen use (r = 0.61, p < 0.001), length of surgery (r = 0.45, p = 0.007), and the presence of other simultaneous procedures (r = 0.40, p = 0.02).
Table 3.
Pearson Correlations for Total Opioid Usage, Pain, and Length of Hospital Stay After Alveolar Bone Grafting.
| Total Opioid Usage (MED/kg) | Pain Scores | Length of Hospital Stay (yr) | ||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Total acetaminophen (mg/kg) | 0.54 | <0.001 | 0.37 | 0.03 | 0.61 | <0.001 |
| Length of surgery | 0.39 | 0.02 | 0.01 | 0.94 | 0.45 | 0.007 |
| Bilateral cleft lip and palate | 0.13 | 0.48 | 0.05 | 0.78 | 0.13 | 0.47 |
| Male | −0.12 | 0.51 | −0.12 | 0.51 | −0.02 | 0.91 |
| Age at surgery | −0.20 | 0.26 | −0.19 | 0.29 | −0.20 | 0.27 |
| Open harvest of bone graft | 0.18 | 0.32 | 0.09 | 0.62 | 0.07 | 0.68 |
| Other simultaneous surgeries | 0.24 | 0.18 | −0.16 | 0.38 | 0.40 | 0.02 |
| PROMIS scores | ||||||
| Peer relationships | −0.02 | 0.90 | −0.01 | 0.95 | 0.17 | 0.35 |
| Anger | 0.23 | 0.20 | 0.23 | 0.19 | 0.02 | 0.90 |
| Anxiety | 0.41 | 0.02 | 0.44 | 0.008 | 0.29 | 0.10 |
| Depressive symptoms | 0.35 | 0.04 | 0.33 | 0.05 | 0.16 | 0.36 |
MED, morphine equivalent dose; kg, kilograms; mg, milligrams; yr, years.
Association of Psychosocial Functioning with Perioperative Opioid use, Postoperative Pain, and Length of Hospital Stay After Alveolar Bone Grafting
To determine factors associated with increased perioperative opioid use, multivariable linear regression models were constructed incorporating variables with significant correlations to opioid use, pain scores, or length of hospital stay in the univariate analyses. Demographic and clinical variables integrated in the model included total acetaminophen use, length of surgery, and the presence of other simultaneous procedures. Patient-reported anxiety and depressive symptoms were separately incorporated into the final models associated with perioperative opioid use, postoperative pain, and length of hospital stay.
Models incorporating patient-reported anxiety accounted for 49.0% of the variance in perioperative opioid use (F4,29 = 7.0, p < 0.001), 31.3% of the variance in postoperative pain scores (F4,29 = 3.3, p = 0.02), and 58.1% of the variance in length of hospital stay (F4,29 = 10.1, p < 0.001) (Table 4). Acetaminophen dosage over the perioperative period was associated with perioperative opioid use and hospital length of stay, while trending towards a significant positive association with patient-reported pain scores. Increased patient-reported anxiety was associated with elevated perioperative opioid use (β=0.36, p = 0.01), postoperative pain (β=0.39, p = 0.02), but not with length of hospital stay. The presence of other simultaneous procedures occurring with ABG was also associated with increased length of hospital stay (β=0.35, p = 0.01).
Table 4.
Association of Patient-Reported Anxiety with Total Opioid Usage, Pain Scores, and Length of Hospital Stay After Alveolar Bone Grafting.
| Opioid Use | Pain Scores | Length of Hospital Stay | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 = 0.490 | R2 = 0.313 | R2 = 0.581 | |||||||
| F4,29 = 7.0 | F4,29 = 3.3 | F4,29 = 10.1 | |||||||
| p < 0.001 | p = 0.02 | p < 0.001 | |||||||
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| Total acetaminophen (mg/kg) | 0.43 | (0.12, 0.72) | 0.005 | 0.34 | (0, 0.67) | 0.05 | 0.51 | (0.25, 0.77) | <0.001 |
| Length of surgery | 0.16 | (−0.20, 0.50) | 0.31 | −0.08 | (−0.43, 0.28) | 0.66 | 0.15 | (−0.14, 0.43) | 0.30 |
| Other simultaneous surgeries | 0.20 | (−0.10, 0.50) | 0.18 | −0.10 | (−0.44, 0.25) | 0.57 | 0.35 | (0.08, 0.62) | 0.01 |
| Anxiety | 0.36 | (0.08, 0.63) | 0.01 | 0.39 | (0.06, 0.71) | 0.02 | 0.24 | (−0.01, 0.49) | 0.06 |
CI, confidence interval.
Models evaluating the predictive value of depressive symptoms accounted for 44.7% of the variance in perioperative opioid use (F8,29 = 5.9, p = 0.001) and 53.7% of the variance in length of hospital stay (F8,29 = 8.4, p < 0.001) (Table 5). However, this model did not demonstrate a statistically significant representation of postoperative pain scores. Unlike anxiety, depressive symptoms scores did not independently predict perioperative opioid use or length of hospital stay.
Table 5.
Association of Patient-Reported Depressive Symptoms with Total Opioid Usage, Pain Scores, and Length of Hospital Stay After Alveolar Bone Grafting.
| Opioid Use | Pain Scores | Length of Hospital Stay | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 = 0.447 | R2 = 0.218 | R2 = 0.537 | |||||||
| F4,29 = 5.9 | F4,29 = 2.0 | F4,29 = 8.4 | |||||||
| p = 0.001 | p = 0.12 | p < 0.001 | |||||||
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| Total acetaminophen (mg/kg) | 0.41 | (0.12, 0.72) | 0.01 | 0.34 | (−0.02, 0.70) | 0.07 | 0.52 | (0.24, 0.80) | <0.001 |
| Length of surgery | 0.18 | (−0.10, 0.50) | 0.27 | −0.06 | (−0.43, 0.31) | 0.76 | 0.16 | (−0.14, 0.46) | 0.28 |
| Other simultaneous surgeries | 0.22 | (−0.10, 0.53) | 0.17 | −0.10 | (−0.47, 0.28) | 0.60 | 0.34 | (0.05, 0.63) | 0.02 |
| Depressive symptoms | 0.30 | (0, 0.59) | 0.05 | 0.23 | (−0.12, 0.59) | 0.19 | 0.11 | (−0.17, 0.38) | 0.43 |
CI, confidence interval.
Discussion
In this work, we evaluated the relationships between patient-reported psychosocial functioning and pain for patients with CLP after undergoing ABG. Using four different instruments, we found that both anxiety and depressive symptoms scores correlated to increased opioid use. Anxiety scores were also correlated to patient-reported pain scores, albeit neither variable correlated to the length of hospital stay. To understand whether these bivariate correlations were influenced by other factors, we then performed multivariable linear regression analyses incorporating potentially associated independent variables such as total acetaminophen, length of surgery, and the presence of other simultaneous procedures with psychosocial outcomes scores. In multivariable models, patient-reported anxiety demonstrated a significant and independent positive association with perioperative opioid use and postoperative pain scores.
Multiple reconstructive surgical procedures are performed within the cleft care pathway from birth to maturity. In each of these procedures, opioid usage within the hospital setting frequently translates to postoperative opioid prescriptions. The risk of persistent opioid use in children and adolescents who have had any surgical procedure, including cleft-related surgeries, has been reported to be over 40 times greater than that of the general pediatric population.1,2 These data suggest that efforts to identify potential modifiable factors that may result in a reduction of opioid usage should be considered, particularly in a pediatric population subjected to multiple surgeries.
The current findings corroborate other studies on the effect of anxiety on opioid use and pain for various types of surgical interventions. In a cohort of pediatric patients undergoing orthopaedic or general surgical procedures, Page and colleagues reported that increased scores on the Multidimensional Anxiety Scale for Children and Child Pain Anxiety Symptoms Scale were significantly predictive of pain intensity on the Numeric Pain Rating Scale within 48–72 h after surgery. 20 Similarly in adults, Caumo et al. found that general and preoperative transient anxiety levels corresponded with moderate to intense acute pain as measured by the Pain Visual Analog Scale 12 and 24 h after abdominal elective surgery. 21 In an adolescent scoliosis cohort, Yang et al. reported that the diagnosis of anxiety was a risk factor for prolonged opioid use after posterior spinal fusion. 22 Of particular concern, this risk of prolonged opioid use was further increased with previous opioid prescriptions. The identification of prior opioid usage and anxiety as risk factors for prolonged use deserves consideration for patients with CLP as the care pathway directly increases opioid exposure. While we did not directly evaluate prolonged opioid use in the current cohort, understanding of lifetime opioid usage in patients with CLP may warrant future investigation.
The ability to screen for anxiety prior to surgery using patient-reported outcomes measures allows for attention to several strategies in reducing pain and perioperative opioid usage in patients reporting higher anxiety scores. First, parent and patient counseling may be critical in preoperative preparation for patients with higher anxiety. Second, multimodal non-narcotic regimens, such as the addition of intraoperative nerve blocks, may be particularly important in such patients. 23 Third, within the hospital setting, non-pharmacologic methods of reducing anxiety may also be aggressively explored. Weiner and colleagues reported that in 146 pediatric patients who underwent lower extremity trauma surgeries, the involvement of Certified Child Life Specialists reduced the amount of opioid use and pain ratings over the course of the hospital length of stay. 24 Similarly, Nilsson et al. compared pediatric patients undergoing outpatient surgeries who were unexposed or exposed to 45 min of music in the immediate postoperative period and noted that music medicine decreased the quantity of morphine administered as well as scores on the Facial Affective Scale. 25
This study has several limitations that deserve mention. The small sample size could have precluded some variables from reaching statistically significant correlations with the three outcomes variables. Additionally, there could be other confounding variables that explain perioperative opioid use that was not included in the multivariable regression model. To characterize psychosocial status, we used the most proximate score, which was either before or after ABG as the PROMIS scores were heterogeneously available depending upon the timing of assessments which were performed solely during the annual multi-disciplinary appointments. Additionally, it should be noted that more than half of the patients (61.8%) in our cohort had other surgical procedures at the time of the ABG surgery. Simultaneous surgeries could potentially pose a challenge in understanding the effect of ABG on patient pain and anxiety postoperatively. However, our results suggest that the presence of other surgeries did not significantly impact the main outcomes of our study, namely postoperative opioid use and pain scores. We did observe that simultaneous surgeries were associated with increased length of hospital stay, which likely reflect the additional time required for the patients to recover from multiple procedures. Future research could focus on closely evaluating the impact of simultaneous combination surgeries on patient perceptions and postoperative outcomes to determine potential additive effects.
Conclusions
Our study demonstrates that patient-reported anxiety is associated with increased pain and perioperative opioid use in patients with CLP following ABG.
Disclosers
All authors have no financial interests including products, devices, or drugs associated with this manuscript. There are no commercial associations that might pose or create a conflict of interest with information presented in this submitted manuscript such as consultancies, stock ownership, or patent licensing arrangements. All sources of funds supporting the completion of this manuscript are under the auspices of the University of California, Los Angeles.
Appendices
PROMIS short forms: Anger 5a, Anxiety 8a, Depressive Symptoms 8a, and Peer Relationships 8a.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JCL is a medical education consultant for Stryker.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Bernard G. Sarnat Endowment for Craniofacial Biology (JCL) and the Jean Perkins Foundation (JCL). JCL is additionally supported by the National Institutes of Health/National Institute of Dental and Craniofacial Research R01 DE028098 and R01 DE029234.
ORCID iDs: Michelle K. Oberoi https://orcid.org/0000-0003-0993-489X
Justine C. Lee https://orcid.org/0000-0002-8943-0837
References
- 1.Bennett KG, Harbaugh CM, Hu HM, et al. Persistent opioid use among children, adolescents, and young adults after common cleft operations. J Craniofac Surg. Oct 2018;29(7):1697‐1701. doi: 10.1097/SCS.0000000000004762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harbaugh CM, Lee JS, Hu HM, et al. Persistent opioid use among pediatric patients after surgery. Pediatrics. 2018;141(1):e20172439. doi: 10.1542/peds.2017-2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286‐1293. doi: 10.1001/jamainternmed.2016.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunn LK, Yerra S, Fang S, et al. Incidence and risk factors for chronic postoperative opioid use after major spine surgery: A cross-sectional study with longitudinal outcome. Anesth Analg. 2018;127(1):247‐254. doi: 10.1213/ANE.0000000000003338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rao AG, Chan PH, Prentice HA, et al. Risk factors for postoperative opioid use after elective shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27(11):1960‐1968. doi: 10.1016/j.jse.2018.04.018 [DOI] [PubMed] [Google Scholar]
- 6.Lu Y, Beletsky A, Cohn MR, et al. Perioperative opioid use predicts postoperative opioid use and inferior outcomes after shoulder arthroscopy. Arthroscopy. 2020;36(10):2645‐2654. doi: 10.1016/j.arthro.2020.05.044 [DOI] [PubMed] [Google Scholar]
- 7.Owusu-Agyemang P, Cata JP, Meter AV, et al. Perioperative factors associated with persistent opioid use after extensive abdominal surgery in children and adolescents: A retrospective cohort study. Paediatr Anaesth. 2018;28(7):625‐631. doi: 10.1111/pan.13386 [DOI] [PubMed] [Google Scholar]
- 8.Potemra HMK, Lin J, Bertrand AA, et al. Long-term effect of multiple operations on psychosocial function in teenage cleft lip and palate patients. Plast Reconstr Surg. 2020;146(1):61e‐68e. doi: 10.1097/PRS.0000000000006905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wouters RM, Porsius JT, van der Oest MJW, et al. Psychological characteristics, female sex, and opioid use predict acute postoperative pain in patients surgically treated for thumb base osteoarthritis: A cohort study. Plast Reconstr Surg. 2020;146(6):1307‐1316. doi: 10.1097/PRS.0000000000007337 [DOI] [PubMed] [Google Scholar]
- 10.Pinto PR, McIntyre T, Araújo-Soares V, Costa P, Ferrero R, Almeida A. A comparison of predictors and intensity of acute postsurgical pain in patients undergoing total hip and knee arthroplasty. J Pain Res. 2017;10:1087‐1098. doi: 10.2147/JPR.S126467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roth ML, Tripp DA, Harrison MH, Sullivan M, Carson P. Demographic and psychosocial predictors of acute perioperative pain for total knee arthroplasty. Pain Res Manag. 2007;12(3):185‐194. doi: 10.1155/2007/394960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nielsen S, Degenhardt L, Hoban B, Gisev N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf. 2016;25(6):733‐737. doi: 10.1002/pds.3945 [DOI] [PubMed] [Google Scholar]
- 14.Shapiro DN, Waljee J, Ranganathan K, Buchman S, Warschausky S. Using the patient reported outcomes measurement information system to evaluate psychosocial functioning among children with craniofacial anomalies. Plast Reconstr Surg. 2015;135(6):1673‐1679. doi: 10.1097/PRS.0000000000001269 [DOI] [PubMed] [Google Scholar]
- 15.Bruce B, Fries J, Lingala B, Hussain YN, Krishnan E. Development and assessment of floor and ceiling items for the PROMIS physical function item bank. Arthritis Res Ther. 2013;15(5):R144. doi: 10.1186/ar4327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): Depression, anxiety, and anger. Assessment. Sep 2011;18(3):263‐283. doi: 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Irwin DE, Stucky B, Langer MM, et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res. May 2010;19(4):595‐607. doi: 10.1007/s11136-010-9619-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Irwin DE, Stucky BD, Langer MM, et al. PROMIS Pediatric Anger Scale: An item response theory analysis. Qual Life Res. May 2012;21(4):697‐706. doi: 10.1007/s11136-011-9969-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Broderick JE, DeWitt EM, Rothrock N, Crane PK, Forrest CB. Advances in patient-reported outcomes: The NIH PROMIS(®) measures. EGEMS (Wash DC). 2017;1(1):1015. doi: 10.13063/2327-9214.1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pagé MG, Stinson J, Campbell F, Isaac L, Katz J. Pain-related psychological correlates of pediatric acute post-surgical pain. J Pain Res. 2012;5:547‐558. doi: 10.2147/JPR.S36614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caumo W, Schmidt AP, Schneider CN, et al. Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiol Scand. Nov 2002;46(10):1265‐1271. doi: 10.1034/j.1399-6576.2002.461015.x [DOI] [PubMed] [Google Scholar]
- 22.Yang S, Werner BC. Response to risk factors for prolonged postoperative opioid use after spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop. 2019;39(9):e729‐e730. doi: 10.1097/BPO.0000000000001180 [DOI] [PubMed] [Google Scholar]
- 23.Pfaff MJ, Nolan IT, Musavi L, et al. Perioperative pain management in cleft lip and palate surgery: A systematic review and meta-analysis of randomized controlled studies. Plast Reconstr Surg. Jul 01 2022;150(1):145e‐156e. doi: 10.1097/PRS.0000000000009231 [DOI] [PubMed] [Google Scholar]
- 24.Weiner J, Zeno R, Thrane SE, Browning KK. Decreasing opioid use in pediatric lower extremity trauma: A quality improvement project. J Pediatr Health Care. 2020;34(5):446‐452. doi: 10.1016/j.pedhc.2020.05.001 [DOI] [PubMed] [Google Scholar]
- 25.Nilsson S, Kokinsky E, Nilsson U, Sidenvall B, Enskär K. School-aged children's experiences of postoperative music medicine on pain, distress, and anxiety. Paediatr Anaesth. Dec 2009;19(12):1184‐1190. doi: 10.1111/j.1460-9592.2009.03180.x [DOI] [PubMed] [Google Scholar]


