Coronary artery perforation is a serious potential complication of percutaneous coronary intervention (PCI), with an incidence of approximately 0.5%.1 Covered stents are used as a part of the treatment algorithm; however, when a perforation occurs at a bifurcation, 1 branch may become occluded after covered stent deployment. This case management adds to the armamentarium used to overcome this situation.
Case
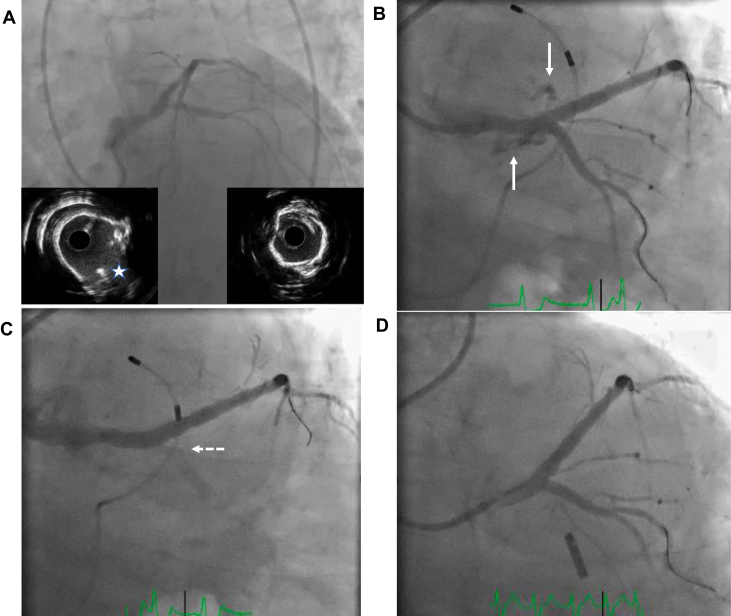
An 83-year-old man with coronary artery disease, prior left anterior descending (LAD) stenting, peripheral vascular disease, and severe asthma on chronic steroids presented with chest pain and dyspnea. He was diagnosed with a non−ST-elevation myocardial infarction. Coronary angiography revealed moderate diffuse disease in the right coronary artery and significant left main (LM), LAD, and left circumflex (LCx) disease (Figure 1A); his ejection fraction was 40%. A heart team meeting was held, and the decision to proceed with PCI over bypass surgery was made, given his comorbidities.
Figure 1.
(A) Left coronary artery showing significantly calcified, distal left main (LM), left anterior descending (LAD), and left circumflex (LCx). The intravascular ultrasound (IVUS) of the ostial LAD on the bottom right corner. IVUS of the distal LM on the bottom left corner. LCx wire entering the distal LM (white star). Severe, circumferential calcification seen in the LM into the LAD using IVUS. (B) After IVUS-guided final kissing balloon inflation of the LM-LAD-LCx (last step of double-kiss crush), an Ellis III perforation of the distal LM into the LAD occurred (arrows). (C) After the placement of a PK Papyrus covered stent into the LM-LAD, the LCx was occluded (dotted arrow). (D) Successful fenestration and ballooning of PK Papyrus into the LCx, with the placement of a drug-eluting stent in the ostial LCx into the LM in T-and-protrustion formation. Fenestration was performed using a stiff wire guided by an angled microcatheter.
A 7F sheath was placed in the right femoral artery. An Extra-Backup (EBU) 3.5 guide (Medtronic) was advanced into the LM. The LAD and LCx were wired, ballooned, and then examined using intravascular ultrasound (IVUS). There was a moderate amount of calcium in the LM and LCx. The LAD was severely calcified, with circumferential calcium detected using IVUS (Figure 1A). Orbital atherectomy of the LM into the LAD was successfully performed. IVUS-guided stenting of the LM-LAD-LCx bifurcation was performed using the double-kiss crush stent technique.
Following final kissing balloon inflation, the patient became hemodynamically unstable, and an Ellis III perforation was detected in the distal LM into the ostial LAD (Figure 1B). Balloon inflation in the LM proximal to the site of the perforation was performed to occlude flow while a PK Papyrus (Biotronik) covered stent was prepared. The balloon was then exchanged for the PK Papyrus covered stent, which was rapidly deployed in the LM into the LAD, occluding the previously stented LCx (Figure 1C). The patient remained hemodynamically unstable, and a pericardial effusion was revealed on a bedside echocardiogram. Pericardiocentesis was then performed, and an intra-aortic balloon pump was inserted.
The focus was then shifted to LCx rescue. A 90°-angled microcatheter was used along with an Astato 20 0.014-inch wire (ASAHI INTECC USA) directed toward the recently placed LCx stent to perforate the polyurethane membrane of the covered stent. Once the wire punctured the covered stent, the pre-existing LCx stent was used to guide wiring down the LCx. The angled microcatheter was advanced slightly to dilate the fenestration to facilitate blood flow in the vessel and was then exchanged for a Turnpike LP catheter (Teleflex) to further dilate the fenestration and easily advance the microcatheter down the LCx. Next, the Astato 20 was exchanged for a workhorse wire, followed by balloon angioplasty of the ostial and proximal LCx. The LCx was then restented with a drug-eluting stent using the T-and-protrusion technique, with excellent angiographic results (Figure 1D). The patient recovered fully and was discharged home 2 weeks later.
Discussion
The predictors of coronary artery perforation include calcified and noncompliant arteries, the use of atheroablative devices, the use of chronic steroids, and older patients with hypertension and acute coronary syndrome.2,3 The incidence of coronary artery perforation is higher with high-pressure balloon inflation and atherectomy, including rotablation and orbital atherectomy. The presentation of coronary artery perforation is broad, ranging from asymptomatic to acute hemodynamic collapse in the setting of tamponade.
Its treatment ranges from conservative management to the placement of covered stents. The other options include prolonged balloon inflation; coil, fat, or gelfoam embolization in the setting of distal wire perforations; pericardiocentesis when appropriate; and, rarely, surgery. Treatment depends on the type of perforation, which includes Ellis type I (extraluminal crater without extravasation), type II (pericardial or myocardial blush without contrast jet extravasation), type III (frank perforation into the pericardium), type IV (into a cardiac chamber), and type V (distal perforation).
In our case example, following atherectomy, double-kiss crush stenting, and high-pressure balloon inflation of the severely calcified coronary artery, an Ellis III perforation occurred, which led to tamponade and required covered stent placement, pericardiocentesis, and an intra-aortic balloon pump. The placement of the covered stent in this case unfortunately resulted in the occlusion of the LCx system. This situation has been seen in 2 previous case reports, but the method of side branch rescue differed slightly.4,5 In those 2 cases, the side branch was recovered using a dual-lumen microcatheter rather than an angled microcatheter. An angled microcatheter may allow for a more directed side branch puncture and rapid fenestration dilation. We perforated the covered stent in only 1 location, followed the wire with a microcatheter, and were then able to serially dilate that fenestration. This allowed for faster recovery of flow into the side branch compared with the use of a dual-lumen catheter because microcatheter dilation could be performed immediately after wire fenestration. Additionally, in our case, it was favorable to have placed a previous stent at the ostium of the occluded side branch, which was then used as a target to direct our stiff puncturing wire, reducing ambiguity. However, if the LM perforation had occurred prior to LCx stenting, an alternative would have been to place a workhorse wire down the LCx and then jail that wire with the covered stent. This jailed wire can then be used as a target for puncture and rewiring to reduce ambiguity.
Conclusion
Coronary perforations requiring a covered stent, resulting in significant side branch loss, can be rapidly treated with the fenestration of the covered stent using a stiff wire and an angled microcatheter to help intentionally direct the wire toward the sacrificed side branch. Prior stenting of the occluded side branch as a part of a 2-stent PCI technique can facilitate the fenestration of the covered stent and subsequent wiring of the occluded vessel, reducing ambiguity and accelerating side branch recovery. The use of an angled microcatheter directed toward a recently placed side branch stent (“stick-the-stent”) is a useful approach to the management strategy for this dreaded complication.
Acknowledgments
Declaration of competing interest
Dr Jaffer receives funding grants from Canon Medical Systems Corporation, Shockwave Medical Inc, Teleflex, Mercator MedSystems, Boston Scientific Corp, and HeartFlow Inc; is a consultant or advisory to SIEMENS, Boston Scientific Corp, Magenta Therapeutics, Philips, and BIOTRONIK Inc; has equity or stocks in Intravascular Imaging Inc and DurVena; has licensing arrangements with Massachusetts General Hospital; and receives royalties from Terumo, Canon, and Spectrawave. Drs Cilia, Schmidt, and Sakhuja reported no financial interests.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics statement
The research reported has adhered to the relevant ethical guidelines.
References
- 1.Rogers J.H., Lasala J.M. Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invasive Cardiol. 2004;16(9):493–499. [PubMed] [Google Scholar]
- 2.Al-Lamee R., Ielasi A., Latib A., et al. Incidence, predictors, management, immediate and long-term outcomes following grade III coronary perforation. JACC Cardiovasc Intv. 2011;4(1):87–95. doi: 10.1016/j.jcin.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 3.Ellis S.G., Semenec T., Lander K., Franco I., Raymond R., Whitlow P.L. Effects of long-term prednisone (≥ 5 mg) use on outcomes and complications of percutaneous coronary intervention. Am J Cardiol. 2004;93(11):1389–1390. doi: 10.1016/j.amjcard.2004.02.036. [DOI] [PubMed] [Google Scholar]
- 4.Adusumalli S., Gaikwad N., Raffel C., Dautov R. Treatment of rotablation-induced ostial left circumflex perforation by papyrus covered stent and its fenestration to recover the left anterior descending artery during CHIP procedure. Catheter Cardiovasc Interv. 2019;93(6):E331–E336. doi: 10.1002/ccd.28114. [DOI] [PubMed] [Google Scholar]
- 5.Werner G.S., Ahmed W.H. Fenestration of a Papyrus PK covered stent to recover the occluded left main bifurcation after sealing a left main perforation during a CTO procedure. Cardiovasc Revasc Med. 2017;18(6S1):41–44. doi: 10.1016/j.carrev.2017.03.006. [DOI] [PubMed] [Google Scholar]