Since the start of humanity, males and females, men and women, have been biologically different, but in many other aspects, equal; however, Western philosophers, theologians, and scientists have previously considered “the second sex,” as dubbed by Simone de Beauvoir, a 20th century female French philosopher, supposedly less noble. So, sex in the Nordic-Baltic-British left main revascularization (NOBLE) trial provides us with new scientific insights into what happens when a man or a woman undergoes coronary revascularization of left main disease.
Writing this editorial, we could not resist the temptation to remind our colleagues/investigators/trialists that the guidelines on “Sex and Gender Equity in Research” have formally recommended using the terms “sex” and “gender” carefully to avoid confusion.1 “Sex” refers to a set of biological attributes: chromosomes, gene expression, hormone function, and sexual anatomy while “gender” refers to socially constructed roles, behavior, and a state of mind that may be guided by sexual preference.1
In this issue of JSCAI, McEntegart et al2 report that while long-term outcomes following treatment of left main coronary artery disease favored coronary artery bypass surgery (CABG) compared to percutaneous coronary intervention (PCI) in men and women, the treatment effect was stronger in females. Importantly, there was no between-sex difference in all-cause mortality at 5 years. The authors proposed possible mechanistic explanations for their observation: higher rate of comorbidities, increased risk of myocardial infarction with nonobstructive coronary artery disease, and the smaller caliber of coronary arteries in female patients than that in male counterparts. Therefore, targeting modifiable risk factors such as intensive lipid-lowering therapy using inhibition of PCSK9, assessing the microcirculation after revascularization, and/or using novel drug-coated balloons for coexisting small vessel disease might be advisable in those patients with left main stem disease.
During his career, the corresponding author of this editorial has personally been involved in multiple major trials comparing PCI to CABG, including “coronary angioplasty vs bypass revascularisation investigation” (CABRI)3 (1988-92), Arterial Revascularization Therapies Study (ARTS) I4 (1997-98), Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX)5 (2005-07), Synergy Between PCI With TAXUS and Cardiac Surgery: SYNTAX Extended Survival (SYNTAXES),6 Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL)7 (2010-14), and multiple meta-analyses.8,9 Repeatedly, he has struggled with the impact of biological sex on the scientific interpretation of the outcomes of these trials.
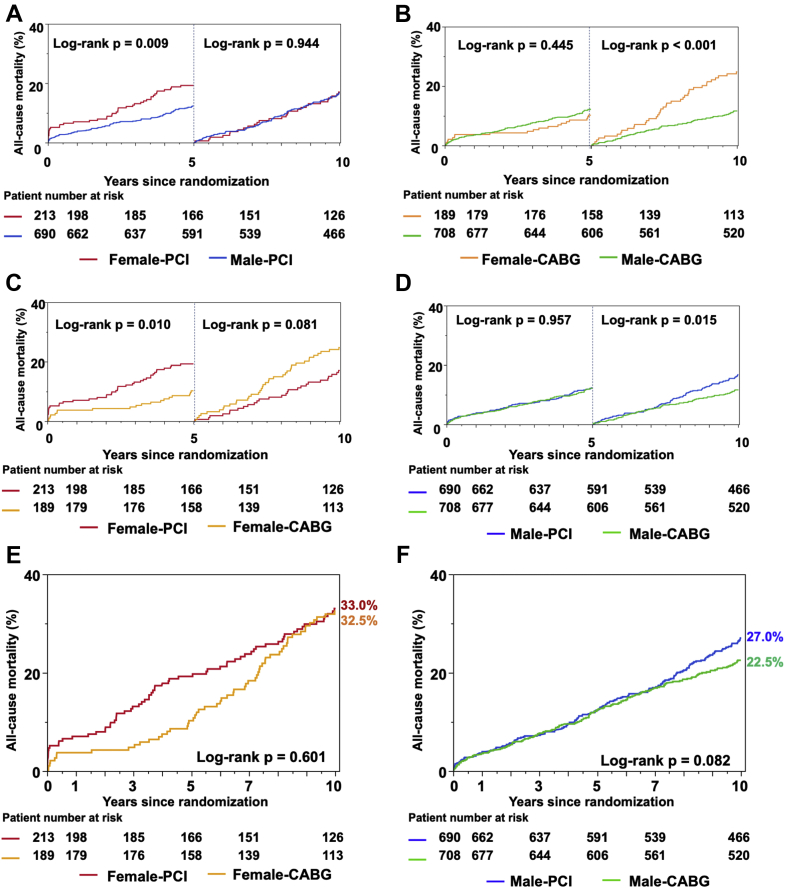
First, traditional statistics has taught us that apparent sex differences in outcome disappear when appropriately adjusting for all kinds of confounding factors (age, hypertension, diabetes, smoking, etc.). Second, there are obvious differences in trials performed with percutaneous balloon angioplasty (percutaneous transluminal coronary angioplasty [PTCA]), bare metal stents, and drug-eluting stents. Third, substantial differences exist between trials enrolling patients exclusively with 3-vessel disease (ARTS I, Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease [FREEDOM],10 Randomized Comparison of Coronary Artery Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients with Multivessel Coronary Artery Disease [BEST]11), 3-vessel disease with allowed inclusion of left main disease (SYNTAX), and those including primarily left main disease with none, 1-, 2-, or 3-vessel disease (EXCEL and NOBLE). Fourth, the duration of the clinical follow-up, up to 1, 3, 5, 8, and 10 years, has to be seriously considered when looking at outcomes such as major adverse cardiovascular outcomes or all-cause mortality (Figure 1).6 Fifth, the surgical technique involving single vs multiple arterial bypass grafts has a major impact on the survival of the surgical cohort.12
Figure 1.
Impact of revascularization strategy on all-cause death in females and males. (A) Female and male patients in the percutaneous coronary intervention (PCI) arm. (B) Female and male patients in the coronary artery bypass graft surgery (CABG) arm. (C and E) The PCI and CABG arms in females. (D and F) The PCI and CABG arms in males.
During the early days of PTCA, the CABRI trial3 reported a higher risk of 1-year mortality in females (relative risk, 2.07; 95% confidence interval [CI], 1.07-4.01; P = .0031), with females randomized to PTCA also more likely to have clinically significant angina (relative risk, 1.54; 95% CI, 1.09-2.16; P = .012) at 1 year than males randomized to either PTCA or CABG.
The ARTS I, FREEDOM, and BEST trials of patients with 3-vessel disease did not show, based on sex, any significant difference in event-free survival within both treatment groups.
The inclusion of female sex as a variable of the SYNTAX score II13 was based on the results of the SYNTAX trial at 4 years and was inferred from the fact that women who underwent PCI had a higher adjusted risk of all-cause death than men (hazard ratio [HR], 1.70; 95% CI, 1.11-2.60), whereas the risk for those who underwent CABG was similar between the sexes (HR, 0.59; 95% CI, 0.32-1.10; Pinteraction = .0059). However, the absence of a favorable treatment benefit with CABG over PCI in women at 10-year follow-up in the SYNTAXES study6 led to the disappearance of sex as an independent determinant factor of mortality in the SYNTAX score II-2020.14 This observation emphasizes the importance of long vs very long follow-up (Figure 1). Notably, in these trials, which were conducted in different chronological periods (from 1988 to 2015), the age between men and women at enrollment varied considerably: ARTS I 5.2 years, CABRI 4.3 years, SYNTAX 3.9 years, EXCEL 1.5 years, and NOBLE 1 year. Putatively, longer life expectancy in women compared with men may have compensated for their older age at enrollment.
In the EXCEL trial,7 sex was not an independent predictor of adverse outcomes after revascularization at 5 years; however, women undergoing PCI had a trend toward worse outcomes than men, again a finding related to associated comorbidities and increased periprocedural complications.
Surgeons in a meta-analysis of 10,479 men and 2714 women found that while women had worse outcomes (a composite of all-cause mortality, myocardial infarction, stroke, or repeat revascularization) than men in the first 5 years after CABG (adjusted HR, 1.12; 95% CI, 1.04-1.21; P = .004), they had similar mortality (adjusted HR, 1.03; 95% CI, 0.94-1.14; P = .51).15
Interventional cardiologists in a meta-analysis of 23,736 men and 9141 women found that female sex was an independent predictor of major adverse cardiovascular outcomes (cardiac death, myocardial infarction, or ischemia-driven target lesion revascularization) but not all-cause mortality at 5 years after contemporary PCI.9 In a similar fashion, a recent individual patient data meta-analysis of 4 randomized trials of revascularization in left main disease (SYNTAX subgroup, PRECOMBAT, NOBLE, and EXCEL) found no statistically significant heterogeneity in 5-year all-cause death across sex subgroups (PCI vs CABG in men: HR, 1.06; 95% CI, 0.86-1.31; in women: HR, 1.18; 95% CI, 0.82-1.71; Pinteraction = .60).8
When undergoing coronary revascularization, the outcome of the noble sex (females in the 21st century) remains enigmatic, but at least both sexes seem to be equal when undergoing left main revascularization, be it percutaneously or surgically. Yes, we are unisex when undergoing left main revascularization.
Declaration of competing interest
Dr Serruys reports a relationship with Philips, SMT, Novartis Pharmaceuticals Corp, Xeltis BV, and Meril Life Sciences Pvt Ltd that includes consulting or advisory. All other authors declare no conflicts to disclose.
References
- 1.Heidari S., Babor T.F., De Castro P., Tort S., Curno M. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2016;1:2. doi: 10.1186/s41073-016-0007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McEntegart M.B., Holm N.R., Lindsay M.M., et al. Sex-specific clinical outcomes after treatment of left main coronary artery disease. A NOBLE substudy. J Soc Cardiovasc Angiogr Interv. 2022;1:100338. [Google Scholar]
- 3.First-year results of CABRI (coronary angioplasty versus bypass revascularisation investigation). CABRI Trial Participants. Lancet. 1995;346:1179–1184. [PubMed] [Google Scholar]
- 4.Serruys P.W., Ong A.T., van Herwerden L.A., et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575–581. doi: 10.1016/j.jacc.2004.12.082. [DOI] [PubMed] [Google Scholar]
- 5.Farooq V., Serruys P.W., Bourantas C., et al. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial. Eur Heart J. 2012;33:3105–3113. doi: 10.1093/eurheartj/ehs367. [DOI] [PubMed] [Google Scholar]
- 6.Hara H., Takahashi K., van Klaveren D., et al. Sex differences in all-cause mortality in the decade following complex coronary revascularization. J Am Coll Cardiol. 2020;76:889–899. doi: 10.1016/j.jacc.2020.06.066. [DOI] [PubMed] [Google Scholar]
- 7.Serruys P.W., Cavalcante R., Collet C., et al. Outcomes after coronary stenting or bypass surgery for men and women with unprotected left main disease: the EXCEL trial. JACC Cardiovasc Interv. 2018;11:1234–1243. doi: 10.1016/j.jcin.2018.03.051. [DOI] [PubMed] [Google Scholar]
- 8.Sabatine M.S., Bergmark B.A., Murphy S.A., et al. Percutaneous coronary intervention with drug-eluting stents versus coronary artery bypass grafting in left main coronary artery disease: an individual patient data meta-analysis. Lancet. 2021;398:2247–2257. doi: 10.1016/S0140-6736(21)02334-5. [DOI] [PubMed] [Google Scholar]
- 9.Kosmidou I., Leon M.B., Zhang Y., et al. Long-term outcomes in women and men following percutaneous coronary intervention. J Am Coll Cardiol. 2020;75:1631–1640. doi: 10.1016/j.jacc.2020.01.056. [DOI] [PubMed] [Google Scholar]
- 10.Farkouh M.E., Domanski M., Dangas G.D., et al. Long-term survival following multivessel revascularization in patients with diabetes: the FREEDOM follow-on study. J Am Coll Cardiol. 2019;73:629–638. doi: 10.1016/j.jacc.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park S.J., Ahn J.M., Kim Y.H., et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med. 2015;372:1204–1212. doi: 10.1056/NEJMoa1415447. [DOI] [PubMed] [Google Scholar]
- 12.Thuijs D., Davierwala P., Milojevic M., et al. Long-term survival after coronary bypass surgery with multiple versus single arterial grafts. Eur J Cardiothorac Surg. 2022;61:925–933. doi: 10.1093/ejcts/ezab392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farooq V., van Klaveren D., Steyerberg E.W., et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381:639–650. doi: 10.1016/S0140-6736(13)60108-7. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi K., Serruys P.W., Fuster V., et al. Redevelopment and validation of the SYNTAX score II to individualise decision making between percutaneous and surgical revascularisation in patients with complex coronary artery disease: secondary analysis of the multicentre randomised controlled SYNTAXES trial with external cohort validation. Lancet. 2020;396:1399–1412. doi: 10.1016/S0140-6736(20)32114-0. [DOI] [PubMed] [Google Scholar]
- 15.Gaudino M., Di Franco A., Alexander J.H., et al. Sex differences in outcomes after coronary artery bypass grafting: a pooled analysis of individual patient data. Eur Heart J. 2021;43:18–28. doi: 10.1093/eurheartj/ehab504. [DOI] [PMC free article] [PubMed] [Google Scholar]