Abstract
Background:
Lung cancer surgery has a significant impact on health-related quality of life (HRQOL). In prior studies of HRQOL after lung cancer surgery, HRQOL domains of interest were selected by the researchers. To increase the patient-centeredness of these studies, we conducted a qualitative study to ascertain which aspects of HRQOL are most relevant to them postoperatively, and to identify Patient-Reported Outcome Measurement Information System (PROMIS) measures most germane to patients undergoing lobectomy for lung cancer.
Methods:
We conducted in-depth semi-structured interviews with 25 patients after lobectomy for lung cancer to solicit input regarding the physical, social and emotional HRQOL domains relevant after surgery. Interviews were transcribed verbatim and a thematic content analysis to identify HRQOL themes was performed; themes were integrated to create a conceptual framework to guide outcome measurement selection.
Results:
Qualitative analysis indicated that within the physical health domain, patients were most concerned about general physical function (100% of participants), pain (96%), fatigue (96%) and dyspnea (76%). Neuropathic pain was reported by 28% of participants. Instrumental (100%) and emotional social support (88%) and positive emotions/relief/hope (96%) were also important. Two cross-cutting themes were the desire to maintain independence (32%) and preparing for surgery/expectations (92%).
Conclusions:
Our results indicate that a number of physical, social and emotional HRQOL domains are relevant after lobectomy for lung cancer. These domains are currently represented by PROMIS measures and can be readily assessed for clinical or research purposes.
In 2020, an estimated 228,820 people will be diagnosed with lung cancer in the US [1], approximately 20% of whom have localized disease [2] for which surgical resection is the standard of care. Thoracic surgeons focus on measuring objective outcomes including morbidity, mortality and long-term survival after lung cancer resection [3,4]. While these outcomes are important, the impact of the operation on an individual’s functional status and wellbeing is not uniformly assessed.
Evidence suggests that lung cancer surgery has a significant impact on health-related quality of life (HRQOL). HRQOL is a multidimensional construct reflecting the extent to which one’s perceived wellbeing in the three domains of health – physical, social and emotional – is impacted by a medical condition or its treatment [5]. For example, a patient may have undergone lobectomy without complications, but developed chronic pain that limited their daily activities. This operation would be considered a success by current standard metrics, but the impact on HRQOL is not captured in any national database and could go unrecognized unless the surgeon inquires. Without data on HRQOL outcomes after surgery, thoracic surgical care is not fully patient-centered. Assessing postoperative HRQOL can help improve understanding of the full impact of surgery, enhance patient-surgeon communication, improve patient counseling and establishment of expectations, monitor progress of recovery and detect and intervene on poor recovery trajectories.
The most common method of assessing HRQOL is via patient-reported outcome measures (PROMs). PROMs are any report of health status that comes directly from the patient without interpretation of the response by a clinician [6]. PROMs are typically assessed via structured questionnaires. The NIH supported the development of the Patient-Reported Outcomes Measurement Information System (PROMIS), a publicly available system for assessing HRQOL [7,8]. One study of lung cancer resection patients has established the feasibility of integrating PROMIS into an institutional database [9]. However, for this and other HRQOL studies that have reported high rates of pain [10,11], dyspnea, fatigue, decreased physical [12] and social functioning [13,14], and emotional/mental distress after surgery [15], HRQOL domains of interest were chosen by investigators rather than patient input. This raises the possibility that facets of HRQOL important to patients after lung cancer resection have not been adequately studied. According to the Food and Drug Administration (FDA), as the purpose of a PROM is to capture the patient’s experience, patients should provide input in PROM development and selection [6].
To guide effective use of PROMs for patients undergoing lung cancer resection, a conceptual framework reflecting aspects of HRQOL that are important to patients is needed. To address the current gaps in knowledge about the HRQOL domains affected by surgery, we conducted a qualitative study to develop a patient-centered conceptual framework of HRQOL after lobectomy for lung cancer. The extensive array of PROMIS measures offers a logical measurement solution for assessing HRQOL; our conceptual framework will be used to identify PROMIS measures for this population.
Patients and Methods
Davis Health were screened for eligibility for enrollment over one year. English-speaking patients who provided informed consent and agreed to participate underwent an in-depth, semi-structured interview that ranged from 1 to1.5 hour in duration via telephone approximately 2 months after surgery. Demographic and clinical information for each patient were recorded. Each participant received a $40 VISA gift card by mail after completing the interview. Each interview was conducted by a PhD sociologist (MMG) with expertise in qualitative research, who utilized an interview guide that began with open-ended questions followed by exploratory prompts to solicit input regarding the HRQOL domains affected by surgery. Each interview was audio-recorded, transcribed verbatim and then uploaded into Dedoose for data management, an online platform for analyzing qualitative data.
Each interview transcript was coded by two independent coders (LB, MG) and two experts (CAV, AK) completed interrater reliability analyses and reconciled discrepancies in coding. A combination deductive and inductive content coding approach that replicates the PROMIS methodology was used to identify major and minor themes within pre-identified domains of HRQOL (physical, social, emotional) in the transcripts [16]. For each domain, four investigators (LB, MG, CAV, AK) collaboratively identified major and minor (sub-) themes (i.e. open coding). These major and minor/sub-themes were used to develop a codebook for each HRQOL domain (hierarchical taxonomy). The codebook went through a series of iterative revisions as all interview transcripts were coded; all transcripts that had been coded with an earlier version of the codebook were then recoded with the final version. Correspondence between PROMIS measures and major/minor themes was examined. This study was approved by the Institutional Review Board of the University of California, Davis.
Results
Participant Cohort
Forty participants were enrolled in the study; 13 were unable to be contacted and 2 decided not to participate. Data were collected from 25 participants (Table 1).
Table 1.
Participant Cohort
| Factor | Median (IQR) or N (%) |
|---|---|
| Age | 71 years (34–82 years) |
| Sex | |
| Female | 18 (72%) |
| Male | 7 (28%) |
| Race | |
| White | 22 (88%) |
| Black | 1 (4%) |
| Asian | 1 (4%) |
| Pacific Islander | 1 (4%) |
| Marital Status | |
| Single | 1 (4%) |
| Married | 15 (60%) |
| Widowed | 8 (32%) |
| Divorced | 1 (4%) |
| Surgical Approach | |
| Video-Assisted | 8 (32%) |
| Robot-Assisted | 10 (40%) |
| Thoracotomy | 7 (28%) |
| Lobe Resected | |
| Right upper | 8 (32%) |
| Right upper bilobectomy | 1 (4%) |
| Right lower | 8 (32%) |
| Left upper | 6 (24%) |
| Left lower | 2 (8%) |
| Lung Cancer Stage (pathologic) | |
| pCR | 1 (4%) |
| IA2 | 3 (12%) |
| IA3 | 2 (8%) |
| IB | 8 (32%) |
| IIA | 1 (4%) |
| IIB | 5 (20%) |
| IIIA | 5 (20%) |
| Chemotherapy | |
| Neoadjuvant | 1 (4%) |
| Adjuvant | 9 (36%) |
HRQOL Themes
The final codebook consisted of 20 themes, 18 within either the physical, social or emotional health domain and 2 cross-cutting themes. Example interview quotations and number and percentage of participants who experienced each domain are listed in Table 2. This table also includes PROMIS measures that correspond to the domain and whether the measure is available as a short form, computer adaptive form (CAT), or both. Short forms are questionnaires with a fixed set of items or questions for one domain. CAT items are dynamically selected from an item bank based on the respondent’s previous answer.
Table 2.
| HRQOL Domains | Example Quotation | N (%) | PROMIS Measures3 | Short Form | CAT4 |
|---|---|---|---|---|---|
| Physical Health | N=25 | ||||
|
| |||||
| General Physical Function | “I’m able to do light housework. Grocery shopping is a bit of a chore, lifting the groceries into the house; I get tired and lose my breath kind of easily, so I need help with that.” | 25 (100%) | Mobility | X | |
| Physical Function | X | X | |||
| Upper Extremity | X | X | |||
|
| |||||
| Pain | “I had no idea my ribs would hurt. My ribs still hurt and we’re over 2½ months out” | 24 (96%) | Pain Interference | X | X |
| Pain Behavior | X | X | |||
| Pain Intensity | X | ||||
| Nociceptive Pain Quality | X | ||||
|
| |||||
| Fatigue | “There are a lot of things that I want to go and do, but I end up not doing them because I don’t have the energy to get up and do it.” | 24 (96%) | Fatigue | X | X |
|
| |||||
| Dyspnea | “Staircases are kind of a problem for me. I get up to the top and I am a little bit on the winded side.” | 19 (76%) | Dyspnea Functional Limitations | X | X |
| Dyspnea Severity | X | X | |||
| Dyspnea Characteristics | X | ||||
| Dyspnea Emotional Response | X | ||||
| Dyspnea Task Avoidance | X | ||||
| Dyspnea Time Extension | X | ||||
|
| |||||
| Strength | “There’s no way at two to four weeks I would have been able to go back to work and resume my normal activities. I didn’t have the strength.” | 12 (48%) | None Available | ||
|
| |||||
| Sleep | “In terms of pain, nighttime was the hardest because you can’t sleep on your side, only on your back, elevated.” | 11 (44%) | Sleep Disturbance | X | X |
| Sleep-Related Impairment | X | X | |||
|
| |||||
| Neuropathic Pain | “It’s a very sharp, shooting, stabbing pain.” | 7 (28%) | Neuropathic Pain Quality | X | |
|
| |||||
| Breast Pain | “I still have that pain in my breast. So I’d say it shoots from the nipple all the way through the breast.” | 6 (24%) | None Available | ||
|
| |||||
| Numbness | “I had read that your skin would be numb, but I hadn’t realized it would be such a big part of me and that it would still be there, you know, 10 weeks later.” | 6 (24%) | None Available | ||
|
| |||||
| Cough | “I expected pain, but I did not expect the cough, and I’m still troubled by the cough. It’s been the most troubling thing of my recovery.” | 5 (20%) | None Available | ||
|
| |||||
| Social Health | |||||
|
| |||||
| Instrumental Support | “My granddaughter and my daughter were there. They’ve come over to help do things around here.” | 25 (100%) | Instrumental Support | X | X |
|
| |||||
| Emotional Support | “I have a good support system. I have a fiancé that is very dedicated to keeping my spirits up.” | 22 (88%) | Emotional Support | X | X |
|
| |||||
| Companionship | “I get together with my family and have a barbeque and just enjoy the people around me, my grandkids. You know, watching them.” | 14 (56%) | Companionship | X | |
|
| |||||
| Informational Support | “The advice I would give to someone in this position is to make sure that you take somebody with you when you go to your first consultations with your doctor because you are going to miss things. You need other people there writing this down, asking other questions that you may not have even thought of, which happened to me. My son had questions I never even thought of.” | 9 (36%) | Informational Support | X | X |
|
| |||||
| Emotional Health | |||||
|
| |||||
| Positive Emotions Relief Hope | “I think having a positive attitude before, during and after surgery is vital to recovery.” | 24 (96%) | General Life Satisfaction | X | X |
| Meaning and Purpose | X | X | |||
| Positive Affect | X | X | |||
|
| |||||
| Depression Sadness Hopelessness | “I think the pain is the number one thing that affects my mood. When I’m really hurting, it’s not happy.” | 16 (64%) | Depression | X | X |
|
| |||||
| Anxiety Fear Worry | “I had some anxiety issues, some stress, you know, getting overwhelmed. They had me work on breathing and controlling my breathing to help calm me down. That actually did help calm me down a lot and it helped control some of the pain.” | 16 (64%) | Anxiety | X | X |
|
| |||||
| Anger Frustration | “The nerve pain I am experiencing now ticks me off. When I hear reports of it can go as quickly as it came, can last a few months, or your whole life, I get upset.” | 15 (60%) | Anger | X | X |
Health-Related Quality of Life
Patient-Reported Outcomes Measurement Information System
PROMIS measures available at healthmeasures.net
Computer Adaptive Test
The following themes were identified in all 25 interviews: general physical function (physical health) and instrumental support (social health). Pain, fatigue and positive emotions/relief/hope (emotional health) were identified in all but one interview. All themes were analyzed for co-occurrence. This symmetric theme by theme matrix indicated the frequencies for which all theme parings were applied to the same quotation, including overlapping quotations. The top pairs of themes were social support and positive emotions/relief/hope, pain and preparing for surgery/expectations, and general physical function and breathing.
Two cross-cutting themes strongly associated with HRQOL were identified. The first is the desire to maintain independence. Eight (32%) participants cited maintaining independence as important. Some example quotes are: “I didn’t want them [family] to wait on me anymore than I absolutely needed”, “I wanted to do as much as I could by myself” and “I didn’t want to go to a nursing home or something. I wanted to feel like I could do this myself. It was very important for me to be independent.” The second is preparing for surgery and preoperative expectations; expectations may be updated by preoperative counseling and after surgery, patients compare their symptoms to what they had expected. The following quote is illustrative, “I wasn’t told to expect the cough. Of all the things, I expected pain, but I did not expect the cough. It has been the most troubling thing of my recovery.” Participants expressed most concern about signs and symptoms that they did not expect. Moreover, if the surgeon indicated that a symptom such as shortness of breath would be present after surgery, but would likely improve with time, participants typically reported that they were not troubled by such a symptom because they anticipated it to improve with time. Twenty three (92%) participants discussed preoperative expectations during their interview. Additionally, trust and faith in the surgeon and health care team was cited by 19 (76%) of participants as central to the surgeon’s ability to effectively set expectations.
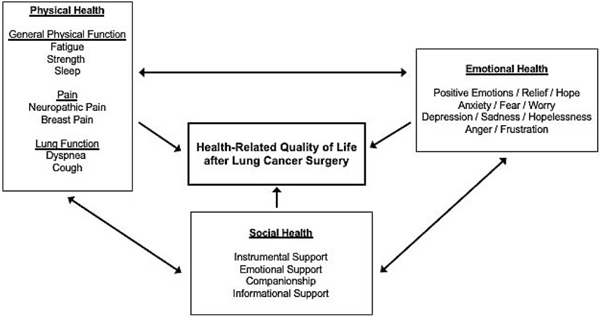
Conceptual Framework
Based on the identified themes, we developed a conceptual framework of HRQOL after lung cancer resection (Figure 1). HRQOL broadly consists of physical, social and emotional domains, with multiple subdomains that are germane to patients’ perceptions of wellbeing after lung resection.
Figure 1.
Conceptual framework of factors associated with HRQOL of individuals after lung cancer resection.
Comment
This is the first study to identify, using qualitative methods, which aspects of HRQOL are most important and relevant to patients after lung cancer surgery, to develop a conceptual framework of HRQOL and inform PROM selection specific to these patients. Our results indicate that all three domains of HRQOL are affected by surgery for lung cancer and suggest that existing PROMIS items banks may provide the most comprehensive assessment of patients undergoing lung cancer resection.
As the focal point of this study is lung cancer resection, the interviews provided a great deal of information regarding physical symptoms. Almost all patients are asymptomatic prior to surgery and therefore the impact of thoracic surgery can be significant from a physical health standpoint. For example, an estimated half of patients undergoing thoracotomy and one third undergoing VATS develop chronic pain [11,17]. While the emphasis is on outcomes after surgery, if the goal is to return patients to their baseline HRQOL, we recommend measuring PROMs at baseline to compare preoperative with postoperative HRQOL. Baseline data may also be used to determine which patients are more likely to have a different recovery trajectory. For example, patients with pain from another source prior to surgery may be more likely to have a greater pain level at baseline and a greater change in pain between baseline and after surgery than those without pain before surgery. By measuring these physical health PROMs, we can determine when a patient is deviating from the expected recovery trajectory in order to intervene early. For example, those with dyspnea interfering with daily activities may benefit from postoperative pulmonary rehabilitation.
Social support for recovery was universally important, in particular instrumental and emotional support. Although many patients voiced their desire to maintain or regain independence, all recognized the need for temporary help with daily activities. In a study of patients with chronic lung disease who were interviewed regarding willingness to undergo lung resection given an array of potential outcomes, patients were least likely to choose surgery if the risk of nursing home placement or loss of independence were high [18]. Importantly, social support has been demonstrated to promote self-efficacy which is a person’s belief in his or her ability to accomplish a task [19]. For example, a patient with a high level of self-efficacy will feel confident in their ability to take the necessary steps to recover from surgery. We did not directly measure self-efficacy and this is an area that warrants further study as we hypothesize that those with good social support and a high level of self-efficacy may recover from surgery more easily than those without either of these. Although we did not measure self-efficacy, we did measure the emotional health factor positive outlook. Having a positive outlook was frequently mentioned as being important to recovery and when patients mentioned having a positive outlook it was often in the context of social support indicating an association between the two.
Patients typically have a postoperative follow-up visit 2–4 weeks after discharge. These follow-up visits are usually short, 15–20 minutes. Given this, there is inadequate time during the office visit to thoroughly inquire about these aspects of HRQOL. However, several randomized trials have discovered that using PROMs in clinical practice aids discussion between patient and physician without prolonging the visit [20,21]. Ideally, patients would complete the PROMs prior to the office visit and these data would be readily available to the surgeon before seeing the patient so that the time can be spent on the most important topics as identified by the patient, thus ensuring that patients’ concerns are addressed. Successful implementation of PROMIS Item Banks into clinical workflow for lung cancer resection patients and capture of these data into an institutional database has already been demonstrated [9]. PROMIS is a publicly available system for measurement of HRQOL applicable to both the general population and patients with a variety of diseases and conditions [7]. PROMIS measures are available for administration as either a static standardized short form or computer adaptive test (CAT). PROMIS short forms can be administered via paper or electronically while CATs can only be administered electronically. PROMIS measures are scored via the Assessment Center Website [22]; scores are calibrated to a weighted distribution of scores from the US general population using a T-score algorithm.
The next steps are to refine the PROMs used to measure HRQOL in these patients using the information provided herein and conduct pilot studies to assess implementation into clinical workflow and database capture as well as clinical trials to determine whether these PROMs can be used to improve HRQOL after surgery. There are many PROMIS measures relevant to patients undergoing lung cancer resection, and in general, these measures can be completed rapidly. In a pilot study of PROMIS measures in patients undergoing lung cancer resection, seven short forms (each with 4 to 10 questions) and three CATS (each with 4 to 12 questions) were completed before surgery, at first postoperative clinic visit, and at 6 months after surgery with median times to complete the assessments of 13, 14, and 15 minutes, respectively [9]. It may be most useful for patients to complete their assessments prior to each encounter so that the surgical team can focus on any low scoring domain(s).
There are several strengths to this study. First, each interview was conducted by the same investigator, a qualitative expert. This was done for two reasons, 1) consistency and 2) to avoid social desirability bias. If interviewed by the surgeon, some participants may answer questions in a manner that would be viewed favorably by their surgeon. Second, each interview was transcribed verbatim, coded by two investigators and coding was consistent between the two and adjudicated by two expert investigators. However, there are some limitations to this study. First, almost all participants are white and therefore, we are unable to determine whether individuals of other races and ethnicities have the same HRQOL concerns after lung cancer resection. This study should be repeated in a more diverse sample to determine whether any different PROMIS domains are germane to individuals of races and ethnicities other than white. Second, we aimed to enroll half men and half women to determine whether there are sex differences in relevant HRQOL domains after lung cancer surgery. As we interviewed two-thirds women and one-third men, we were unable to rigorously compare responses to identify differences by sex. Despite these limitations, it is likely that HRQOL domains relevant to those undergoing lung cancer resection are similar regardless of demographic factors, but the degree to which each domain is impacted by surgery may differ according to these factors.
In conclusion, we have identified a set of PROMIS domains important and relevant to patients undergoing lung cancer resection. This PROM system can be used to improve patient-centered care such that the patient’s perspective of the impact of surgery on their physical function and wellbeing will be incorporated as an outcome of the operation. There is potential for these PROMs to improve communication between the patient and the surgical team, identify HRQOL issues after surgery and implement interventions to improve or restore HRQOL.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].American Cancer Society Key Statistics for Lung Cancer. https://www.cancer.org/content/cancer/en/cancer/lung-cancer/about/key-statistics.html. Accessed April 4, 2020.
- [2].National Cancer Institute. https://seer.cancer.gov/statfacts/html/lungb.html. Accessed April 4, 2020.
- [3].Kozower BD, Sheng S, O’Brien SM, Liptay MJ, Lau CL, Jones DR, et al. STS database risk models: Predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg 2010;90:875–81. [DOI] [PubMed] [Google Scholar]
- [4].Chansky K, Detterbeck FC, Nicholson AG, Rusch VW, Vallières E, Groome P, et al. The IASLC Lung Cancer Staging Project : External Validation of the Revision of the TNM Stage Groupings in the Eighth Edition of the TNM Classifi cation of Lung Cancer. J Thorac Oncol 2017;12:1109–21. [DOI] [PubMed] [Google Scholar]
- [5].Cella D. Measuring quality of life in palliative care. Semin Oncol 1995;22:73–81. [PubMed] [Google Scholar]
- [6].Food and Drug Administration. Guidance for Industry Use in Medical Product Development to Support Labeling Claims Guidance for Industry. Fed Regist 2009:65132–3. [Google Scholar]
- [7].HealthMeasures. Intro to PROMIS. www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis. Accessed April 4, 2020.
- [8].Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient-Reported Outcomes Measurement Information (PROMIS): Progress of an NIH Roadmap Cooperative Group During its First Two Years. Med Care 2007;45:S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Khullar OV., Rajaei MH, Force SD, Binongo JN, Lasanajak Y, Robertson S, et al. Pilot Study to Integrate Patient Reported Outcomes After Lung Cancer Operations Into The Society of Thoracic Surgeons Database. Ann Thorac Surg 2017;104:245–53. [DOI] [PubMed] [Google Scholar]
- [10].Bayman EO, Parekh KR, Keech J, Selte A, Brennan TJ. A Prospective Study of Chronic Pain after Thoracotomy. Anesthesiology 2017;126:938–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bayman EO, Brennan TJ. Incidence and severity of chronic pain at 3 and 6 months after thoracotomy: Meta-Analysis. J Pain 2014;15:887–97. [DOI] [PubMed] [Google Scholar]
- [12].Kenny PM, King MT, Viney RC, Boyer MJ, Pollicino CA, McLean JM, et al. Quality of life and survival in the 2 years after surgery for non-small-cell lung cancer. J Clin Oncol 2008;26:233–41. [DOI] [PubMed] [Google Scholar]
- [13].Balduyck B, Hendriks J, Lauwers P, Van Schil P. Quality of Life after Lung Cancer Surgery: A Prospective Pilot Study comparing Bronchial Sleeve Lobectomy with Pneumonectomy. J Thorac Oncol 2008;3:604–8. [DOI] [PubMed] [Google Scholar]
- [14].Balduyck B, Hendriks J, Lauwers P, Nia PS, Van Schil P. Quality of life evolution after lung cancer surgery in septuagenarians: a prospective study. Eur J Cardio-Thoracic Surg 2009;35:1070–5. [DOI] [PubMed] [Google Scholar]
- [15].Poghosyan H, Sheldon LK, Leveille SG, Cooley ME. Health-related quality of life after surgical treatment in patients with non-small cell lung cancer: A systematic review. Lung Cancer 2013;81:11–26. [DOI] [PubMed] [Google Scholar]
- [16].Kisala P, Tulsky D. Opportunities for CAT applications in medical rehabilitation: development of targted item banks. J Appl Meas 2010;11:315–30. [PMC free article] [PubMed] [Google Scholar]
- [17].Bayman EO, Parekh KR, Keech J, Selte A, Brennan TJ. A Prospective Study of Chronic Pain after Thoracic Surgery. Anesthesiology 2017;126:938–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cykert S, Kissling G, Hansen CJ. Patient preferences regarding possible outcomes of lung resection: What outcomes should preoperative evaluations target? Chest 2000;117:1551–9. [DOI] [PubMed] [Google Scholar]
- [19].Banik A, Luszczynska A, Pawlowska I, Cieslak R, Knoll N, Scholz U. Enabling, Not Cultivating: Received Social Support and Self-Efficacy Explain Quality of Life After Lung Cancer Surgery. Ann Behav Med 2017;15:1–12. [DOI] [PubMed] [Google Scholar]
- [20].Detmar SB, Muller MJ, Schornagel JH, Wever LD V, Aaronson NK. Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. JAMA 2002;288:3027–34. [DOI] [PubMed] [Google Scholar]
- [21].Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: A randomized controlled trial. J Clin Oncol 2004;22:714–24. [DOI] [PubMed] [Google Scholar]
- [22].HealthMeasures. HealthMeasures Scoring Service powered by Assessment Center. https://www.assessmentcenter.net. Accessed, April 4, 2020.