Abstract
Purpose:
Discrepancies exist between the need to lock food away and satiety scores in the Smith-Magenis syndrome (SMS) population. This study sought to uncover food-related behaviors within this unique group of individuals.
Methods:
Caregivers (N = 24) representing 21 individuals with SMS, recruited from the Parents and Researchers Interested in SMS national meeting and social media platforms, participated in semistructured interviews. Interviews were digitally recorded, transcribed verbatim, coded, and analyzed using hybrid thematic analysis.
Results:
This study identified a global theme of “Blind to the perils while pursuing their goals,” supported by 5 organizing themes: (1) Biology-impacting behaviors, (2) Need for personalized strategies, (3) Controlling food experiences, (4) Need for parents to orchestrate life, and (5) Surprising resourcefulness. Subthemes within these organizing themes highlighted that individuals with SMS have unique food-related behaviors and often fixate on certain types of foods. Their constant obsession with food for many of them is driven by hunger, obsessive characteristics, a need for autonomy, and a need for fairness. Caregivers must put multiple guardrails in place and remain constantly vigilant to prevent overeating in these individuals.
Conclusion:
Individuals with SMS often perseverate on food and display unique food-related behaviors. Treating obesity in this population is likely to be ineffective without multicomponent, individualized strategies. Additionally, research in this population will likely require targeted instruments for the SMS population to more clearly define the underlying etiologies and to track changes over time in therapeutic trials.
Keywords: Food behaviors, Genetic obesity, Parent control, Personalized strategies, Smith-Magenis syndrome
Introduction
Smith-Magenis syndrome (SMS) is a complex neuro-behavioral disorder caused by either a deletion of chromo-some 17p11.2 or pathogenic variant in RAI1.1 The syndrome includes short stature, hearing loss, speech and motor delay, intellectual disability, sleep disturbance, and behavioral abnormalities, such as self-injurious behaviors, aggression, temper tantrums, and stereotypical behaviors.1,2 Individuals with SMS commonly experience excessive weight gain, which leads to obesity.3,4 Likely contributing to their propensity for weight gain, individuals with SMS also exhibit food-related behaviors, such as impaired satiety, equivalent to Prader-Willi syndrome (PWS).4 Although SMS patients may exhibit hyperphagia,4–6 it is not fully known exactly what causes or exacerbates weight gain in SMS patients because not all patients develop obesity. In addition to cognitive impairments, adults and children with SMS also suffer from anxiety, behavioral disturbances, and sleep disorder.1 How each of these comorbidities contribute to the presence or absence of food-related behaviors in SMS is unknown.
Clinical trials targeted to address the treatment and prevention of obesity in the SMS population are currently hampered by the lack of a clinical measure of food-related behaviors to adequately monitor outcomes in this population. Hyperphagia remains a poorly defined diagnosis in all populations but especially in those with cognitive impairments where questionnaires must be answered by caregivers. Adults and children with SMS have low to moderate scores on the Hyperphagia Questionnaire for Clinical Trials,7 a questionnaire designed for the PWS population.8,9 However, 57% of parents previously reported locking away food.4 Thus, there is a clear contradiction between elevated inappropriate responses to food, stealing food, and caregivers having to lock away food, with questionnaire-reported mild satiety disruptions. However, there has not been any systematic study to understand intricacies in food-related behaviors in the SMS population to understand if existing questionnaires are not adequate.
In this study, we performed qualitative analyses of focus groups comprising parents of individuals with SMS to understand the food-related behaviors common to the group.
Materials and Methods
We used a qualitative design to explore the food-related behaviors of individuals with SMS. This study was approved by our Institutional Review Board.
Subjects were caregivers of individuals with SMS (≥6 years old) who agreed to participate in a focus group and have their responses recorded. We recruited subjects from the Parents and Researchers Interested in SMS (PRISMS) foundation listserve and through the 11th International SMS Conference.
Focus groups and interviews
Using the Socio-Ecological Model as a guiding framework, the research team developed a semistructured interview script exploring food-related behaviors in individuals with SMS (Table 1).10,11 Guiding interview questions were developed in collaboration with an experienced qualitative researcher11,12 (S.S.) and an SMS expert1,2,4,7,13 (S.E.). The script included 6 open-ended questions with probes encouraging further discussion. It investigated (1) how food influenced behavior, (2) what strategies had been used to limit food intake, (3) contributing factors to food-related behavior, (4) situational aspects influencing food-related behaviors, (5) strategies the child uses to get food, and (6) medications that may influence behaviors.
Table 1.
Questions and focus group prompts
| Guided Script Prompts |
| “Can you describe how food influences your child’s behavior?” |
| “What things have you done to limit your child’s food intake?” (For each thing mentioned, ask “What age did you start using that strategy,” “Are you still using that now,” “What was the most helpful about that” and “What was the least helpful about that”?) |
| If not explicitly mentioned, ask if they have locked away food, used medications, used schedules, or used any other environmental controls. |
| “What things affect how your child relates to food?” |
| “Are there any situations or events which make your child’s behaviors around food better or worse?” |
| If not explicitly mentioned, ask about how sleep, changes to schedules, anxiety, lack or presence of favorite foods may alter behavior. |
| “What does your child do to gain food?” |
| If they do not mention them, ask if the following are ever used: becoming upset, bargaining or manipulating, foraging in the trash, getting up at night, sneaking into the pantry or fridge, breaking locks, stealing other people’s food, hiding food, complaining things are not fair, hitting others, eating non-food items. |
| “Are there any medications your child has taken or currently takes that alter his/her food behaviors?” |
| If not explicitly mentioned, ask about if anti-anxiety/depressant or mood stabilizers, stimulants, and sleep aids affect behavior. |
| For the different environmental controls or strategies used throughout the session, ask “How does____(insert strategy) influence how you answer questions regarding your child’s appetite and food-related behaviors?” |
Two individuals trained in both qualitative methods and study procedures conducted the interviews.11 Four focus groups were performed ranging from 3 to 13 individuals each. Two groups were performed in person and 2 via a video conferencing platform. All interviews were video and audio recorded, and random numbers were assigned to each subject.11 Subjects provided standard demographic information, including demographic data on their child with SMS.11
All interviews were professionally transcribed and checked for accuracy by one of the authors.11 Theoretical saturation was achieved after 4 groups, as evidenced by the lack of emergent new information.11
Statistical analyses
We analyzed the qualitative data using a semistructured thematic analytical approach, utilizing both deductive and inductive coding.14 Transcripts of the focus groups were annotated using video recordings to note the subject number for all quotes. Three trained members of the research team reviewed the transcripts multiple times to develop familiarity with responses.11 The team assembled an initial coding structure (deductive) based on the global concepts of the interview questions and overall knowledge of the responses.11,14 The transcripts were independently coded by 3 individuals, and additional codes (inductive) were added during this process to capture emergent data.11 A codebook of codes, definitions, and key decisions was maintained throughout analysis to preserve an audit trail.11 Research investigators routinely met to discuss and resolve coding differences.11 After coding and discussions were complete, codes were grouped into higher order categories and then grouped into themes.11 Among the themes, subthemes were then generated to represent crucial components of the theme.11 Subthemes are reported with the percentage of individuals with SMS whose caregiver(s) interview corresponding to each.11 Given that the thematic analysis centered on behaviors/needs in individuals with SMS, we based frequency calculations on the number of individuals with SMS represented in the quotes, not on the number of caregivers in the sample. Thus, all caregivers were individually coded but were only counted once for each pair in frequency calculations. Because (1) caregivers were not required to answer every question individually, and (2) a caregiver who had a partner in the focus group may not contribute additional comments if their partner had already mentioned a behavior, we chose to calculate each subtheme based on the total number of individuals with SMS and not the number that contributed to the theme. However, the number of caregivers and the individuals with SMS they represented are presented for each theme. A thematic network was generated to visually represent the relationship among themes.11 Quotes are verbatim and identified by randomly assigned numbers to protect confidentiality.11 Demographic data were calculated as the mean ± 1 standard deviation or as a percentage of the group.
Word Cloud
All quotes which were coded to fit into one of our themes were selected and the list edited to remove duplicates. These quotes were then copied and entered into an online program for generating pictographs (www.wordart.com). Common and nonspecific words (is, are, thing, um, really, etc) were deleted and the remaining words visualized. Frequently occurring words appear in relatively larger font sizes than less frequently appearing words.
Results
Recruitment identified 24 caregivers of a child or adult with SMS who consented to participate, and all contributed to one of the focus groups (Table 2). These individuals were 79.2% female and had a mean age of 49.5 ± 11.3 years. Two individuals who participated were not parents, 1 was a daytime caregiver, and 1 a host home provider. There were 3 mother-father couples in cases which both individuals contributed answers. Thus, the focus groups obtained behaviors on 21 individuals with SMS, who were 66.7% female, had a mean age of 19.3 ± 9.8 years, and 76.2% who lived at home with at least 1 parent.
Table 2.
Demographics of caregivers and individuals with SMS
| Demographics of Caregivers of Individuals with SMS | N = 24 |
|---|---|
| Female, % | 83.3 |
| Age, y | 49.5 ± 11.3 |
| Race/ethnicity | |
| Non-Hispanic White | 90.5 |
| Hispanic White | 14.3 |
| Non-Hispanic Black or Hispanic Black | 0 |
| Other/no answer | 9.5 |
| Demographics of individuals with SMS | N = 21 |
| Female, % | 66.7 |
| Age, y | 19.3 ± 9.8 |
| Race/ethnicity, % | |
| Non-Hispanic White | 85.7 |
| Hispanic White | 9.5 |
| Non-Hispanic Black or Hispanic Black | 0 |
| Other/no answer | 9.5 |
| Living arrangement | |
| At home with one or both parents, % | 76.2 |
| Group home, % | 9.5 |
| Other relatives or host home | 9.5 |
SMS, Smith-Magenis syndrome.
One global theme emerged (Blind to the perils while pursuing their goals), supported by 5 organizing themes: Biology impacting behaviors, Need for personalized strategies, Controlling food experiences, Need for parents to orchestrate life, and Surprising resourcefulness (Figure 1). Each theme is presented below, with subthemes, discussed in order of the frequency mentioned.11 The thematic network is presented in Figure 1.
Figure 1. Blind to the perils while pursuing their goals.
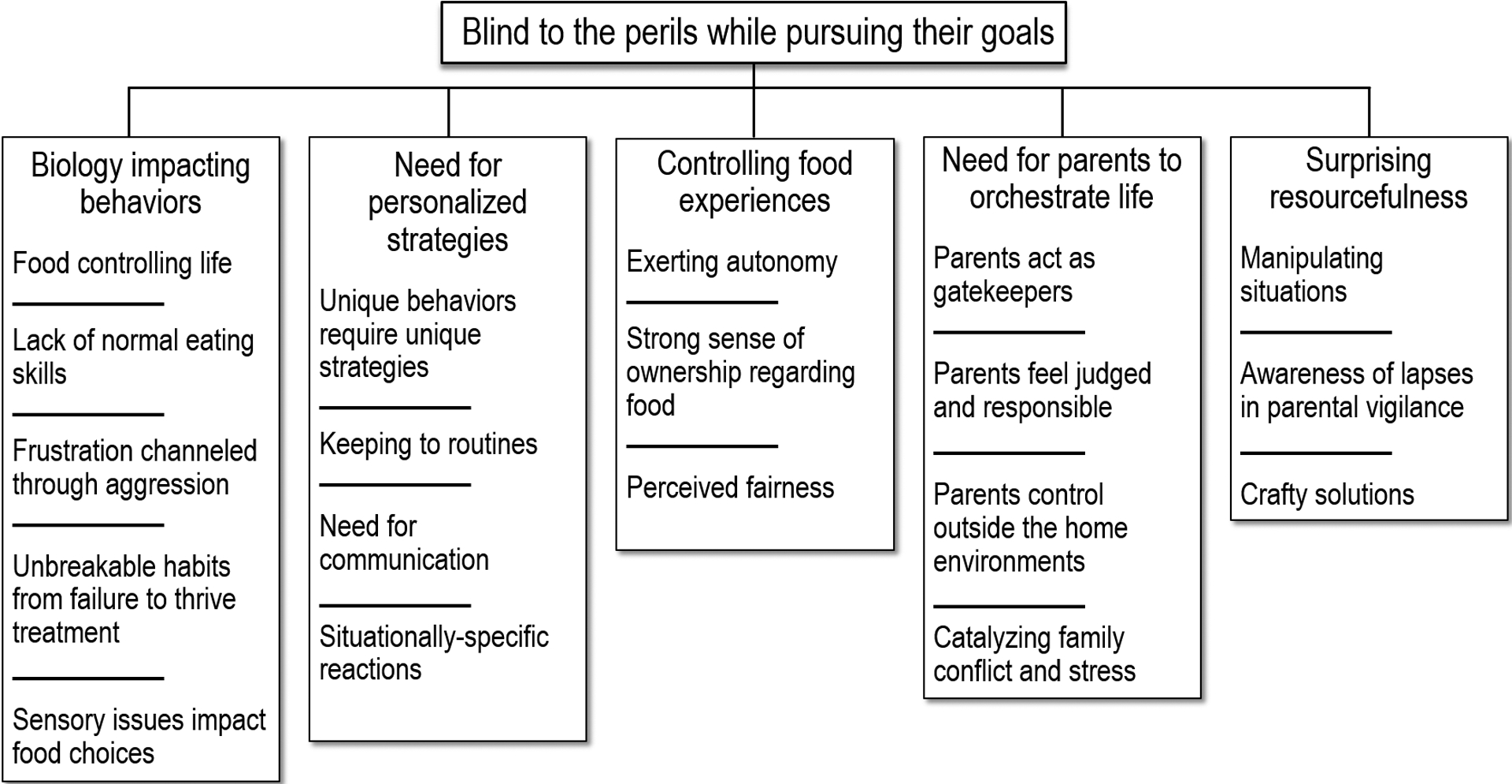
Hybrid thematic analysis revealed 1 overarching theme, 5 global themes, and several subthemes capturing the food-related behaviors of individuals with Smith-Magenis Syndrome as observed by their caregivers.
Global theme: Blind to the perils while pursuing their goals
Overall, individuals with SMS had intense goals relating to food (including types, amounts, and timing) and would pursue those goals without any regard for health or personal dangers or concerns of others. This behavior stemmed from the underlying biology of SMS, required personalized strategies, manifested itself in exerting control around food experiences, required parental vigilance to mitigate health risks, and resulted in a surprising resourcefulness to attain their goals.
Organizing theme #1: Biology affecting behaviors
Individuals with SMS have underlying neurodevelopmental deficits that affected their food-related behaviors. These underlying deficits included a lack of normal eating skills, sensory issues controlling food choices, motor deficits that initially caused failure to thrive, and emotional disruptions causing aggression when frustrated. All caregivers contributed to this theme.
Food controlling life (20/21; 95.2%)
Caregivers reported that almost all individuals with SMS obsessed or perseverated on food in some manner. Many caregivers noted that they saw individuals with SMS obsess about food to the point at which it controlled large parts of their life. “[Food] controls his day and behavior,” noted Caregiver 22. Caregiver 4 stated that food was “in the forefront of her thoughts like 99% of the time.” For many families, the requests for food were constant. Caregiver 14 stated, “probably everybody’s child wakes up and goes, ‘When are we going to eat dinner? What’s for dinner?’” whereas another caregiver noted, “It’s immediately. We can finish and 15 minutes later, she wants something else” (Caregiver 1). In fact, many parents stated that the obsession with food was the primary characteristic they would change of their child if they could.
Lack of normal eating skills (19/21; 90.5%)
We found many individuals with SMS struggled with a lack of normal eating skills. Over half of the group struggled with overeating in general, many who seemed to have no sense of satiety and who would eat to the point of vomiting. However, there were also many individuals who struggled with normal chewing and swallowing. Caregivers reported many individuals had a “steam shovel effect” in which “before she has fully chewed it and swallowed it, she’s already got the next bite in there” (Caregiver 23). This caused 2 caregivers to have to perform the Heimlich maneuver on the children because of choking. Additionally, many caregivers implemented external controls to help correct these behaviors (see theme #4).
Frustration channeled through meltdowns and aggression (15/21; 71.4%)
Previous data demonstrate that individuals with SMS experience an inability to control emotions and a deficit in executive function and emotional regulation.15,16 Because of this, most individuals had meltdowns when food was not given to them or offered in the way they desired. For some, meltdowns were only in relation to unhealthy food items, “like the ice cream or…candy bars or something like that we don’t even put at the house….She would get physical with those kind of things…It’s a fight. It’s a struggle” (Caregiver 20). For others, aggression was aimed at specific people, as one mother said, “Well, it depends on who it is. Me, she’ll charge at me. Sometimes she’ll…hit me just trying to grab at it” (Caregiver 5).
Unbreakable habits from failure to thrive treatment (6/21; 28.6%)
Six individuals with SMS had failure to thrive early in life. The treatment for failure to thrive typically consists of letting children eat almost any food they are willing to, adding calories to foods with additives, such as butter, peanut butter, or sour cream, and sometimes allowing kids to graze throughout the day to try to increase their caloric intake. Thus, several caregivers noticed that as their children switched from failure to thrive to normal weight and then approached or exceeded obesity, it was difficult to switch gears and focus on healthy eating and reduced portions. One mother stated that her greatest wish is that “I would have had a better understanding of the food and how it plays so much in their lives now, that I wish I would have developed a better diet for her [early in life]” (Caregiver 19).
Sensory issues affect food choices (3/21;14.3%)
Although many individuals with SMS had specific food preferences and cravings (discussed more under theme #2), some individuals had limited diets stemming directly from difficulties with texture or sensory issues resulting from their underlying syndrome. One caregiver of a 9-year old said, “He has quite a lot of oral issues that he can’t eat – He doesn’t eat regular foods” (Caregiver 22), whereas another of a 7-year old said “she’s very, very limited – Sorry, I’ve got a baby – as to like what she likes to try” (Caregiver 17).
Organizing theme #2: Need for personalized strategies
The food-related behaviors exhibited by individuals with SMS were diverse, requiring a plethora of different strategies. These strategies included very individualized solutions, as well as the importance of keeping to routines, communicating with individuals, and avoiding situations in which specific reactions were more likely to occur. Caregivers (N = 21, 87.5%) representing all 21 individuals with SMS contributed to this theme.
Unique behaviors require unique strategies (17/21; 81.0%)
Caregivers had unique and diverse experiences negating any common approach that worked for the majority of individuals with SMS. Although some individuals with SMS had symptoms consisting of classic hyperphagia, an intense drive to eat all food, many more families struggled with specific food preferences/cravings or behaviors. In fact, some individuals with SMS did not eat large meals at all but wanted to graze constantly throughout the day. Other families noted that large amounts of food were only for highly desired foods. One caregiver said, “He still only wants way more if it’s pasta or bread or dessert” (Caregiver 12). However, bananas and milk were surprisingly common foods that individuals with SMS would overeat. One caregiver noted that they have “drag-out fights because of bananas” (Caregiver 3), whereas another noted “she had drank a half-gallon of milk. Just chugged it right out of the carton” (Caregiver 15). Others sought out condiments, including ketchup, mayonnaise, and hollandaise sauce. Interestingly, limiting access to condiments required very personalized strategies. For instance, Caregiver 11 stated, “hollandaise sauce is one of those things that goes in my pocketbook and not the cabinet, because he’ll make the whole thing and eat the whole thing.” On the other hand, one individual was obsessed with salad dressings; therefore, the family would put a drop of 8 different salad dressings on their child’s salad. Some individuals with SMS dislike spicy foods, which allowed one family to redirect their child to a different food but required another family to carefully avoid offering spicy foods to minimize outbursts.
Keeping to routines (12/21; 57.1%)
Structure and routine are an integral part of the lives of many with SMS. Most individuals had a schedule they adhered to and as one caregiver stated, “She’s on the dot, if you don’t give, it’s – You’ll know about it” (Caregiver 2). Keeping to a routine was important both to increase well-being and to prevent meltdowns. Because individuals with SMS often obsessed about new food items, with the “new thing [asked for] every day” (Caregiver 9), structure and routine were found to be necessary in many families. Some families felt that anything that “throws [routines] off, causes a lot more anxiety for her and thus, makes her more upset and kind of have meltdowns surrounding food” (Caregiver 17). Interestingly, although behaviors around food were altered with changes in routine, families did not note any increase in the amount of food eaten in these situations.
Need for communication (12/21; 57.1%)
Individuals with SMS have very concrete thinking. Some individuals responded well to discussions about cause and effect. One caregiver noted, “And I have to tell her, if you take too big of a bite, you could choke and you could end up having to go to the hospital, give her all of the explanation as to why, and she’ll do fine the rest of that meal” (Caregiver 4). Sometimes, the cause-and-effect discussions were linked to reminding them of past experiences. Individuals also responded well to redirection, although Caregiver 5 stated, “You’ve got to get her right at the beginning.” Although an individual may accept the redirection without a meltdown, this did not equate to the conversation being ended. One caregiver noted that, because her child had no concept of time, after being told lunchtime was an hour away, “maybe 10 minutes later, she’ll be back…and we could go through this, you know, a dozen times” (Caregiver 21). Many individuals also did well when future plans were communicated to them about routines and events. Although some families were able to talk about future meals without incident, several families noted that they could not talk about what was going to be served at the next meal. Discussion of the next meal would often provoke “arguing with me in the kitchen for the next 2 hours about what she didn’t want” (Caregiver 9).
Situationally specific reactions (11/21; 52.4%)
Negative behaviors with food often were tied to specific situations in individuals with SMS. For example, although seeing a soda may not cause a problem, “if it’s in her hand…it’s a losing battle” (Caregiver 5). Some individuals had more negative behaviors or increase in meltdowns after eating unhealthy foods. Interestingly, one family treated their child with a McDonald’s meal before going to a horseback riding session. However, their aide eventually asked them, “Can you stop with the McDonald’s meal? Because her behavior is worse always after horseback riding day” (Caregiver 3). For some individuals, anxiety around new situations, such as going to a restaurant with an unfamiliar waiter or a party at work, increased meltdowns surrounding food, and others noted that their children would seek food when upset.
Organizing theme #3: Controlling food experiences
Individuals with SMS expressed strong opinions to exert their autonomy, displayed a significant degree of ownership with both their own and other’s food, and were very sensitive to any perceived iniquities. Contributing to this theme were 22 caregivers (91.7%), representing 20 (95.2%) of the individuals with SMS.
Exerting autonomy (18/21; 85.7%)
A very common theme was that individuals with SMS wanted control over their food and environment. One parent noted, “That’s why for us I think it’s a control thing. That’s one thing that she has a say or she knows that she has an opinion on like what she gets to eat or how much of it or when she gets to eat. She has control in that aspect of her life” (Caregiver 4). This need for control was manifested by many individuals as always being “focused on the next meal. Like it’s breakfast and she’s like ‘What are we having for dinner tonight?’” (Caregiver 7). The need to know what the next meal included was often an attempt to insert their opinion for what the next food offering would be. Additionally, there were also strong demands or avoidance of certain types of foods. For example, Caregiver 22 noted, “If I buy the no name fish crackers and they’re the penguin crackers, that causes an issue. He knows if it’s a different brand.”
Strong sense of ownership regarding food (16/21; 76.2%)
The majority of individuals with SMS displayed behaviors consistent with believing they were entitled to any food around them. As Caregiver 19 noted, “she thinks that anything in the house…it’s hers.” To that end, when people in the home threw away food or finished the last of a food item, individuals often got upset. Stealing food from within the home, as well as from strangers was observed in many individuals with SMS. Some would walk up to strangers to take food. Although some individuals manifested ownership through eating “the entire package of 16 slices of cheese” (Caregiver 24), others would just “ask for [a cookie] and then it will just sit beside him…He just wants to know that it’s there” (Caregiver 22). One caregiver noted that her daughter’s sense of ownership over food caused problems with siblings, “[if] her baby sister….comes near her food, she will hit at her” (Caregiver 17).
Perceived fairness (12/21; 57.1%)
Individuals with SMS had distorted concepts of fairness and were often hyperfocused on others obeying “the rules.” Individuals wanted their portions to be the same as everyone else, regardless of their age. Caregiver 24 stated, “he looked at whatever the adult was having next to him, and he thought it should be the same.” This sense of fairness sometimes disregarded past events—“So even if she ate hers earlier, and her brother’s just now eating his, she wants another because he’s having his now” (Caregiver 17). This need for fairness also caused a problem with siblings, as one caregiver noted, “If he finds out my daughter had birthday cake at school, he might just go hit her because he’s angry that he didn’t get birthday cake that day” (Caregiver 6). Another caregiver noted, “It has to be fair. Like if there’s a little bit smidge of icing more on his sister’s, he can have a fit and then just like completely melt down” (Caregiver 11).
Organizing theme #4: Need for parents to orchestrate life
Because of the struggles individuals with SMS had surrounding food, they required significant intervention from their parents to create boundaries both within and outside of the home to help them rein in their food intake, with 22 caregivers (91.7%) contributing to this theme, representing 20 (95.2%) of the individuals with SMS.
Parents act as gatekeepers (19/21; 90.5%)
Monitoring and controlling food intake was a significant part of the lives of caregivers of individuals with SMS. One caregiver said, “You have to kind of monitor what they eat or else they won’t stop” (Caregiver 2). Locking up food or hiding food was felt to be necessary by parents to control their child’s food intake. Fourteen families had locked refrigerators or pantries or blocked their child’s access to the kitchen, whereas 6 families hid or locked away specific food items. However, some individuals with SMS also needed direct supervision around any food opportunities. Caregiver 9 advised, “Don’t ever let them eat without somebody around. A little bit of advice.” Although sleeping controls at night were not explicitly investigated, caregivers mentioned that 52.3% of individuals with SMS were locked in their rooms at night, both for their safety and to prevent them from foraging for food when others were asleep. Additionally, parents controlled the types of food inside the home, as one caregiver noted, “there’s a lot of things we just don’t purchase and keep in our home” (Caregiver 4).
Parents feel judged and responsible (13/21; 61.9%)
Given the pervasive problems with food and, for many, subsequent problems with obesity, it is not surprising that caregivers felt both responsible for the outcomes, as well as judged by others. A few caregivers noted specifically that they felt strongly about being an example for their kids and not eating unhealthy foods in front of them. One caregiver noted that after learning more about SMS, “we were like ‘Oh, so we’re actually doing harm by not locking things up’” (Caregiver 24). Caregivers wished they “would have had a better understanding of …how [food] plays so much in their lives now…[to] have developed a better diet for her [in the past]” (Caregiver 19). However, it is also notable that parents felt “embarrassed for them” (Caregiver 3) because of their behaviors and messiness.
Parents control outside the home environments (12/21; 57.1%)
Given that individuals with SMS spend a significant amount of time outside of their home, there was a need for caregivers to engage with their extended family, school, work, and/or group home environments to help set appropriate boundaries to limit food intake and decrease negative behaviors. One family “[had] to talk to her bosses, too, and [ask them to not] allow her to go and just by $5 worth of sodas or something” (Caregiver 20). However, Caregiver 13 noted that “it requires a lot of obedience from a lot of people because there’s so many aides, teachers. There are so many hands in the pot.” Additionally, not all environments were supportive of beneficial boundaries for individuals with SMS because “her diagnosis isn’t defined like a Prader-Willi’s. So because she’s an adult now, it’s considered a right’s restriction, and we aren’t allowed to limit what she eats or what, where, you know how much [she eats]” (Caregiver 16).
Catalyzing family conflict and stress (10/21; 47.6%)
Likely unknowingly, several individuals with SMS were catalysts for family conflict and parental stress. One interesting outcome was that several families noted they were unable to have family meals that included the individual with SMS. Caregiver 17 stated, “Well, it sounds like all of us have stopped doing family meals, just how I feel, because of the negative emotions that go with it.” The other major negative finding noted was conflict between siblings with the individual with SMS related to food. As noted previously, individuals with SMS may hit or get angry with their siblings when there is a perceived inequity of food or if they feel their food is threatened. Some of the behavioral and motor development difficulties individuals with SMS experience can also increase parental stress, causing one caregiver to state, “I’ve just given up because otherwise I’m going to be that crazy mom who’s just always mad all the time” (Caregiver 18).
Organizing theme #5: Surprising resourcefulness
Individuals with SMS showed a wide variety of strategies to gain access to food. These included manipulating situations, taking advantage of lapses in parental vigilance, and using crafty solutions. Twenty caregivers (83.3%) contributing to this theme, representing 18 (85.7%) of the individuals with SMS.
Manipulating situations (16/21; 76.2%)
Many caregivers noted that individuals with SMS were able to manipulate situations to their advantage to obtain food. Outbursts and even self-injurious behaviors were felt to be manipulative to some extent because many parents noted these were worse out in public than at home. Caregiver 17 stated, “I think she has been manipulating me with her meltdowns. Like she knows that, you know, in certain situations, to avoid a meltdown, I will give in in certain ways.” Several individuals also tried to get food for good or bad days. One caregiver noted, “My daughter, same. She’ll ask, ‘Can we go to Starbucks? Because I’m having a bad day’” (Caregiver 5). There were also several instances of individuals with SMS being able to get strangers to buy or give them food. Caregiver 16 noted, “She’s gotten in trouble for going with her day program to McDonald’s and getting in line even though she doesn’t have money and ordering. And then when her food arrives, she gets the person standing next to her to pay for it.”
Awareness of lapses in parental vigilance (12/21; 57.1%)
Although it was noted previously that many families hid or locked away food, individuals with SMS were often able to determine when there were opportunities to get around these safeguards. Individuals with SMS, similar to other kids, show different behaviors depending on who is nearby. As one caregiver noted, “I don’t really have that many problems with her at the house. But that’s also because her dad’s usually around” (Caregiver 2). Individuals with SMS were noted to “get to the kitchen on his own” (Caregiver 22) or seek out food when parents were not around, eg, at work. At a parent support group conference, one SMS individual was “all excited when we were finished, and she said ‘somebody left a can of Coke. I drank a can of Coke’” (Caregiver 8).
Crafty solutions (10/21; 47.6%)
Individuals with SMS showed amazing abilities to create unique solutions to gain access to food. Families hid keys to locks in various locations (with pens, inside a crockpot, for example), but the individuals with SMS were always able to find them. One child had even “taken the key off of the keychain and taken it to the hardware store to make a copy” (Caregiver 11). Another individual “went around to the back door, went out to the side yard, was able to go get into the garage, through the garage, into the laundry room, into the pantry area” (Caregiver 13). Another individual took “Thanksgiving pies from the freezer at night, …put them in the cabinet, [and would] just go by and grab a handful, and nobody knew that was going on” (Caregiver 8).
Discussion
Overall, the general findings of behaviors in this study are similar to those described by a consensus group for individuals with hyperphagia (which included hyperphagia, temper outbursts, anxiety, obsessive compulsive behaviors, rigidity, and social cognition).17 However, this study indicates that individuals with SMS struggle with food-related behaviors in interesting and specific ways. A pictograph representing the frequency of word occurrences in our interviews (Supplemental Table 1) is displayed in Figure 2, emphasizing the impact of food in this population (with “food,” “eat,” and “more” occurring very frequently). Also interesting is the frequency of the words “time” and “try,” underlining the effects of time on behaviors, as well as the variety of behaviors attempted by individuals with SMS and the strategies tried by their caregivers. Although food is a controlling factor in most of their lives, many individuals struggled with specific foods or situations, not overeating all foods at all times. From classic dessert foods, such as ice cream, to seemingly innocuous foods, such as hollandaise sauce, specific foods can set off very disruptive behaviors. The underlying aspects of the syndrome, which include sensory issues, concrete thinking and obsessive natures, abnormal appetite regulation, and dysregulated circadian rhythms, manifested in food-related behaviors, causing disruptions of mealtimes and hyperfixation on food. However, these fixations may change over time based on television or internet commercials they saw or experiences outside of the home. Thus, these fixations were unique to the individuals in large part. Last, this study showed that individuals with SMS are masters at obtaining their goals when given the opportunity, requiring significant vigilance by parents and stressing the importance of communication and strategizing with school/work/extended family to limit food consumption across all environments.
Figure 2. Word cloud representation of caregiver quotes.
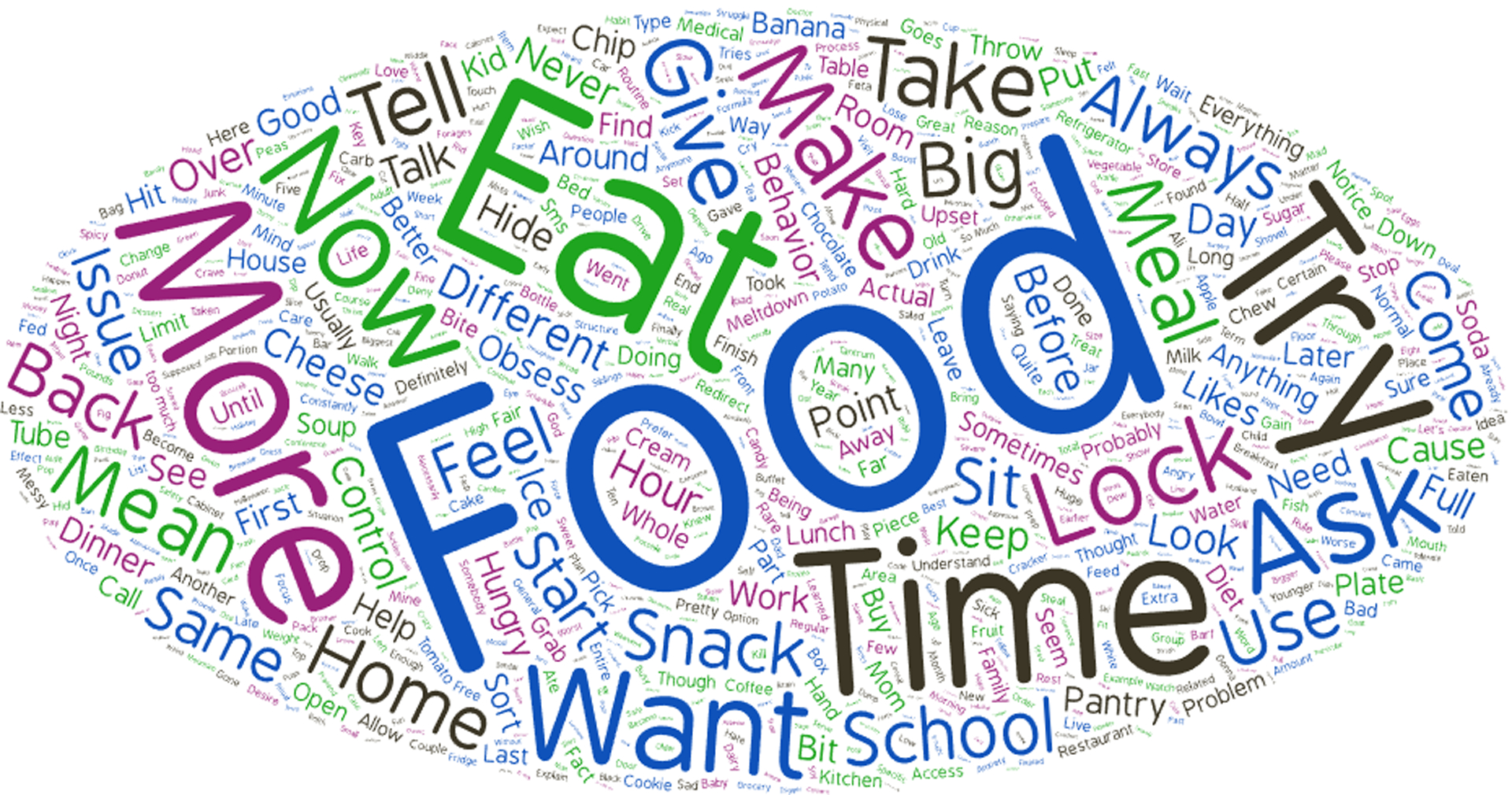
All words from caregiver quotes aligning with our thematic analysis are depicted. Font size correlates with word frequency, with larger font sizes indicating higher-frequency words.
The seeking of specific foods as opposed to all foods may explain the discrepancies we previously observed between the high percentage of parents who locked food away with lowered impaired satiety scores on the Food-Related Problems Questionnaire (FRPQ) in individuals with SMS compared with PWS.4 First, several parents in this study noted they only lock away specific foods, not all foods. Because the FRPQ asks, “Is it necessary to lock food away to stop the person from taking food,” it does not capture if this is global access or specific access to foods. Second, questions related to impaired satiety include, “After a normal size meal, how often will the person say they still feel hungry” and “If given the opportunity, does the person ever eat more than a standard sized meal.” Answering these questions for an individual who only overeats specific foods may not capture individuals who overeat large amounts of foods outside of meal times or only overeat certain foods (if parents do not offer those foods). Thus, performing research using the FRPQ likely needs to be tailored to the SMS population to better capture the behaviors seen in individuals with SMS.
Many parents wished they knew more about how important food would become later in life to set up earlier guardrails. Interestingly, one-quarter of the individuals with SMS had experienced failure to thrive early on, and then the caregivers struggled to change habits as their child began to gain excess weight. Although the literature is sparse, evidence in PWS shows that frequent monitoring of weight and length/height is helpful to catch a rise in weight for height ratio before an onset of food-seeking behaviors.18 Whether these phases hold true for SMS is unknown. Regardless, future research to help parents treat failure to thrive in a manner that is easier to modify as weight gain occurs is clearly needed. However, caregivers were also clear that regardless of failure to thrive, early education on nutrition and food-related behaviors would have been beneficial. Those caregivers who received earlier diagnoses and implemented healthier nutrition early in life felt their children did not struggle with limited portions and options compared with individuals who were diagnosed later. Thus, early nutrition education is likely beneficial for all families with a child with SMS.
Although we did not explicitly ask about caregiver burden in this study, these results show a need for high parental involvement in all aspects of an individual’s life, further supporting previous studies indicating a high caregiver burden in this population.7,19,20 A previously published study in parents of children with early onset obesity11 and a study of caregivers of individuals with PWS21 both show that obesity in children can cause high caregiver burden. Given the high food-seeking behaviors and need for constant vigilance in this population, understanding how treatments affect caregiver burden would be important information to best assess quality of life outcomes and efficacy of treatment.
Understanding what influences behaviors in SMS is likely important to accurately capture the extent of food-related problems in this population. Interestingly, no one in this study felt that changes in routine or sleep changes increased food intake in general, although they did note that nonfood-related behaviors may change. However, they did note that individuals with SMS would use emotional states as a manipulation to get specific types of food. Previous work has shown that behavioral problems correlate with sleep disruption in individuals with SMS.22 No one in this study specifically mentioned sleep as a reason for changes in food-related behaviors, which was a specific prompt in the open-ended questions. However, we did not explicitly gather information on the sleep patterns or sleep aids (eg, tasimelteon) in these subjects. Without prompting, over half of individuals mentioned that they used external controls to keep their child safe at night; therefore, the effect of disrupted sleep on food intake is likely masked because of these strategies. Thus, it is unknown if this group had better treatment of their sleep disruption than reported in previously published studies or if the families just had better coping and management of the sleep behaviors because of extensive experience over the years.
Overall, this study shows that most individuals with SMS are controlled by their obsessions with food and will seek food regardless of harms that may occur (as evidenced by episodes of choking, overeating, and disruption to relationships around them). A key takeaway from this study is that strategies to help individuals with SMS curb weight gain will likely need to be both multifactorial and individualized. The constant obsession with food for many of them is in part driven by hunger but also by obsession, a need for autonomy, and a need for fairness, which are unlikely to be corrected with a purely anorexic drug. Additionally, dietary strategies, such as smaller portions or using individually portioned snacks, may work well for some but be completely ineffective for others. Thus, the medical community must uncover the unique behaviors in each individual to provide effective treatments for the individuals with SMS. Uncovering these unique behaviors is crucial to support caregivers to enhance compliance, monitor outcomes, and to ensure that the comprehensive personalized approach contributes to the improving both health and quality of life for the individual and their family. Additionally, these unique behaviors likely necessitate instruments tailored for the SMS population to truly track changes in behaviors over time in therapeutic trials.
Supplementary Material
Funding
This work was supported by the NIH (R21HD106345-01A1) to Drs Elsea and Sisley.
Conflict of Interest
Stephanie Sisley’s work has been funded by the NIH, USDA, Rhythm Pharmaceuticals, and Eli Lilly and Company. Stephanie Sisley has received speaking and consulting fees from Rhythm Pharmaceuticals. Sarah H. Elsea has research funding from the NIH, PTC Therapeutics, Speragen, Inc, and PRISMS, Inc. PRISMS, Inc supports the SMS Patient Registry, which is housed at Baylor College of Medicine. All other authors declare no conflicts of interest.
Footnotes
Ethics Declaration
This study was approved by the Baylor College of Medicine Institutional Review Board. Verbal informed consent was obtained from subjects.
Additional Information
The online version of this article (https://doi.org/10.1016/j.gimo.2024.101857) contains supplemental material, which is available to authorized users.
Data Availability
Because of the potential loss of confidentiality, we will make data summaries and codebooks available upon request to Stephanie Sisley (sisley@bcm.edu).
References
- 1.Elsea SH, Williams SR. Smith-Magenis syndrome: haploinsufficiency of RAI1 results in altered gene regulation in neurological and metabolic pathways. Expert Rev Mol Med. 2011;13:e14. 10.1017/S1462399411001827 [DOI] [PubMed] [Google Scholar]
- 2.Chen L, Mullegama SV, Alaimo JT, Elsea SH. Smith-Magenis syndrome and its circadian influence on development, behavior, and obesity – own experience. Dev Period Med. 2015;19(2):149–156. [PubMed] [Google Scholar]
- 3.Edelman EA, Girirajan S, Finucane B, et al. Gender, genotype, and phenotype differences in Smith-Magenis syndrome: a meta-analysis of 105 cases. Clin Genet. 2007;71(6):540–550. 10.1111/j.1399-0004.2007.00815.x [DOI] [PubMed] [Google Scholar]
- 4.Alaimo JT, Barton LV, Mullegama SV, Wills RD, Foster RH, Elsea SH. Individuals with Smith-Magenis syndrome display profound neurodevelopmental behavioral deficiencies and exhibit food-related behaviors equivalent to Prader-Willi syndrome. Res Dev Disabil. 2015;47:27–38. 10.1016/j.ridd.2015.08.011 [DOI] [PubMed] [Google Scholar]
- 5.Greenberg F, Lewis RA, Potocki L, et al. Multi-disciplinary clinical study of Smith-Magenis syndrome (deletion 17p11.2). Am J Med Genet. 1996;62(3):247–254. [DOI] [PubMed] [Google Scholar]
- 6.Burns B, Schmidt K, Williams SR, Kim S, Girirajan S, Elsea SH. Rai1 haploinsufficiency causes reduced Bdnf expression resulting in hyperphagia, obesity and altered fat distribution in mice and humans with no evidence of metabolic syndrome. Hum Mol Genet. 2010;19(20):4026–4042. 10.1093/hmg/ddq317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gandhi AA, Wilson TA, Sisley S, Elsea SH, Foster RH. Relationships between food-related behaviors, obesity, and medication use in individuals with Smith-Magenis syndrome. Res Dev Disabil. 2022;127: 104257. 10.1016/j.ridd.2022.104257 [DOI] [PubMed] [Google Scholar]
- 8.Fehnel SE, Brown TM, Nelson L, et al. Development of the hyperphagia questionnaire for use in Prader-Willi syndrome clinical trials. Value in Health. 2015;18(3):A25. 10.1016/j.jval.2015.03.154 [DOI] [Google Scholar]
- 9.Dykens EM, Maxwell MA, Pantino E, Kossler R, Roof E. Assessment of hyperphagia in Prader-Willi syndrome. Obesity (Silver Spring). 2007;15(7):1816–1826. 10.1038/oby.2007.216 [DOI] [PubMed] [Google Scholar]
- 10.Control CfD, Prevention. The Social-Ecological Model: A Framework for Prevention. 2015. Accessed June 25, 2024. https://mncasa.org/tools/the-social-ecological-model/
- 11.Bryant K, Sandhu J, Nguyen J, Asonye E, Thompson D, Sisley S. Isolation in a sea of “experts”: identifying the parental struggles caring for children with early-onset obesity. Child Obes. 2023;19(6):408–416. 10.1089/chi.2022.0089 [DOI] [PubMed] [Google Scholar]
- 12.DeMello AS, Acorda DE, Thompson D, et al. Growing up after adolescent bariatric surgery. Clin Nurs Res. 2023;32(1):115–125. 10.1177/10547738221120338 [DOI] [PubMed] [Google Scholar]
- 13.Baek WS, Elsea SH. Smith-Magenis syndrome treated with ramelteon and amphetamine-dextroamphetamine: case report and review of the literature. J Genet Disord Genet Rep. 2016;5:4. 10.4172/2327-5790.1000145 [DOI] [Google Scholar]
- 14.Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. 10.1177/160940690600500107 [DOI] [Google Scholar]
- 15.Wilde L, Oliver C. Brief report: contrasting profiles of everyday executive functioning in Smith-Magenis syndrome and Down syndrome. J Autism Dev Disord. 2017;47(8):2602–2609. 10.1007/s10803-017-3140-2 [DOI] [PubMed] [Google Scholar]
- 16.Smith AC, Gropman AL. Smith-Magenis syndrome. In: Carey JC, Cassidy SB, Battaglia A, Viskochil D, eds. Cassidy Allanson’s Management of Genetic Syndromes. John Wiley & Sons; 2021:863–893. [Google Scholar]
- 17.Schwartz L, Caixàs A, Dimitropoulos A, et al. Behavioral features in Prader-Willi syndrome (PWS): consensus paper from the International PWS Clinical Trial Consortium. J Neurodev Disord. 2021;13(1):25. 10.1186/s11689-021-09373-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller JL, Lynn CH, Driscoll DC, et al. Nutritional phases in Prader-Willi syndrome. Am J Med Genet A. 2011;155A(5):1040–1049. 10.1002/ajmg.a.33951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foster RH, Kozachek S, Stern M, Elsea SH. Caring for the caregivers: an investigation of factors related to well-being among parents caring for a child with Smith-Magenis syndrome. J Genet Couns. 2010;19(2):187–198. 10.1007/s10897-009-9273-5 [DOI] [PubMed] [Google Scholar]
- 20.Agar G, Bissell S, Wilde L, et al. Caregivers’ experience of sleep management in Smith-Magenis syndrome: a mixed-methods study. Orphanet J Rare Dis. 2022;17(1):35. 10.1186/s13023-021-02159-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kayadjanian N, Schwartz L, Farrar E, Comtois KA, Strong TV. High levels of caregiver burden in Prader-Willi syndrome. PLoS One. 2018;13(3):e0194655. 10.1371/journal.pone.0194655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garayzábal E, Hidalgo I, Miranda De Souza ALD, da Silva NC, Giacheti CM, Pinato L. Sleep disturbances and behavior in Smith-Magenis syndrome. Res Dev Disabil. 2022;128:104286. 10.1016/j.ridd.2022.104286 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Because of the potential loss of confidentiality, we will make data summaries and codebooks available upon request to Stephanie Sisley (sisley@bcm.edu).


