Abstract
Purpose:
To examine recent trends in the coronary heart disease (CHD) risk profiles of the population aged 45 to 64 in the United States.
Methods:
Data from the National Health and Nutrition Examination Surveys (NHANES) from 2 time periods (1988–1994 and 2005–2008) are used to estimate the CHD risk functions derived from the Framingham Heart Study. The risk functions take account of levels of blood pressure (systolic and diastolic), total and high-density lipoprotein serum cholesterol, diabetes (doctor diagnosed or based on fasting glucose), and smoking status to estimate the 10-year risk of myocardial infarction or coronary death. We estimate the risk functions by gender, race, and age group (45–54 and 55–64).
Results:
The CHD risk profile of middle-aged adults has improved over time. For example, the mean 10-year risk of heart attack or CHD death among persons 55 to 64 years has declined from 7.1% to 5.2%. Declines are seen among both men and women and among non-Hispanic Blacks and non-Hispanic whites.
Conclusions:
Despite increases in diabetes and obesity, the CHD risk profile of middle-aged adults improved during the period from 1988–1994 to 2005–2008.
Keywords: Aging, Coronary heart disease, Mortality, Risk factors
Many studies have demonstrated improved health and functional ability among recent cohorts of the elderly. Even as the prevalence of some chronic diseases has increased, life expectancy at the oldest ages has risen, and many areas of health have improved [1-4].
Lately, there has been interest in the health and functioning of middle-aged adults—the “baby boomers”—who will soon become eligible for Medicare. Health indicators over the past two decades for the middle-aged population are mixed. For example, overall mortality rates (and heart disease mortality rates) have continued to decline. The prevalence of obesity and diabetes has increased, whereas the percentage with high cholesterol has declined [5-8]. There is some evidence of increased limitations in functional ability, and the decline in the percent reporting fair to poor health seems to have leveled off since the mid 1990s. [5,6,9-12].
In this paper, we focus on trends in the risk of coronary heart disease (CHD) because it is a major contributor to poor health and disability, as well as a common cause of death. The aging of the baby-boom generation is expected to place a major strain on the U.S. health care system and spending, the magnitude of which may depend on whether their rates of cardiovascular disease are lower than preceding cohorts [13-15]. National health surveys have documented a striking increase in the prevalence of obesity and overweight in the U.S. population over the past three decades, although in recent years the increase has leveled off for women. More recently, the prevalence of diabetes has increased for the total population and for certain age groups. Declines in physical activity and diet quality and increased caloric intake have been blamed [5,6,16-22]. This has led to speculation that adverse effects on the overall risk profile of the population may slow or reverse the long-term decline in mortality from CHD and stroke in the near future [23,24]. Many risk factors for cardiovascular disease are interrelated and present apparently inconsistent trends [25]. Because it is difficult to sort out the effect of individual risk factors when examining trends or modeling future health status and health care spending, we calculate a summary measure of cardiovascular risk using a model derived from the Framingham Heart Study [26,27]. This model estimates the 10-year risk of coronary death and/or myocardial infarction. We estimate this risk among the population of middle-aged adults from 1988 to 1994 and from 2005 to 2008.
Data and methods
Data in this study are taken from the National Health and Nutrition Examination Surveys (NHANES). NHANES is designed to monitor the health and nutritional status of the U.S. population. The survey consists of interviews conducted in participants’ homes, standardized physical examinations conducted in specially outfitted mobile examination centers, and laboratory tests utilizing blood and urine specimens provided by participants during the physical examination. NHANES had been conducted intermittently from the early 1960s until 1994. In 1999, NHANES became a continuous survey, fielded on an ongoing basis. Each year of data collection is based on a representative sample covering all ages of the civilian noninstitutionalized population. Since 1999, public-use data files are released in 2-year cycles.
We use data from the NHANES III, conducted from 1988 to 1994, and from the NHANES 2005 to 2008. Response rates for the medical examination component of NHANES from 1988 through 1994 to 2005 through 2008 were between 75% and 78% [5]. Selected subjects were aged 45 to 64 years and completed the morning fasting glucose component of the examination in the mobile examination center. We excluded fewer than 5% of these subjects because of missing values on analytic variables. Data on fasting glucose levels from the 2007 through 2008 NHANES were adjusted to be compatible with earlier years as recommended in the survey documentation [28]. Analyses use the fasting sampling weights and adjust for the complex survey design with Sudaan software [29].
We estimate the 10-year risk of CHD, defined here as myocardial infarction (heart attack) and/or fatal CHD, using mathematical risk functions developed from the Framingham Heart Study. The risk functions are based on the experience of over 5000 persons aged 30 to 74 years who were examined in 1971 through 1974 as part of the Framingham Heart Study. Twelve years of follow-up data were used in proportional hazards models. These results were adjusted to estimate a 10-year risk. The risk functions assign weights, based on the coefficients of the hazards models, to various CHD risk factors. SAS programs to calculate the risk estimates were provided by researchers from the National Heart Lung and Blood Institute of the National Institutes of Health (Personal communication, Mr. Sean Coady, November 14, 2007). The inputs to the risk estimation functions are gender, age, measured total and high-density lipoprotein serum cholesterol levels, measured blood pressure, diabetes status, and self-reported smoking status [26,27]. For this analysis, the definition of diabetes includes any of the following: Physician-diagnosed diabetes, taking diabetic medication including insulin, or having a fasting glucose level greater than or equal to 126 mg/dL. This definition differs slightly from currently accepted classifications, which also take account of levels of hemoglobin A1c [30]. The definition here conforms to the specifications of the risk equations that were developed before the latest revision in diabetes definitions. The risk factors of high blood pressure and high cholesterol are based only on measured levels, whereas the diabetes risk factor includes measured levels of glucose or physician diagnoses or being treated with medication. Coronary heart disease risk estimates were calculated by age group, gender, and race/ethnicity only for those who were not previously diagnosed with a heart attack. The final sample sizes for our analysis were 1862 in 1988 through 1994 and 1563 in 2005 through 2008. Because the Framingham CHD prediction scores have been shown to be poorly calibrated for at least some groups of Hispanics [26], we only show race/ethnicity results separately for non-Hispanic Whites and non-Hispanic Blacks, although Hispanics are included in the overall estimates. Because of the small sample sizes, we combined age groups when we present race differences.
Results
The characteristics of the two study samples are shown in Table 1. Percents are based on weighted data. Some risk factors worsened over the time period, such as the percent obese, whereas others improved (declines in high cholesterol). The estimates of 10-year CHD risk shown in Table 2 are calculated among the study sample respondents who were not previously diagnosed with a heart attack. For all persons aged 45 to 54 years, the 10-year risk of CHD declined by 20% between the two time periods, 23% for men and 14% for women. Among persons aged 55 to 64 years, there was a 26% overall decline in the 10-year risk of CHD. Non-Hispanic Whites and non-Hispanic Blacks showed similar declines in CHD risk over the period.
Table 1.
Demographic and health characteristics of adults aged 45–64 who have not had a heart attack: United States, 1988–1994 and 2005–2008
| NHANES III, 1988–94 (n = 1862) |
NHANES 2005–2008 (n = 1563) |
|||
|---|---|---|---|---|
| % | SE | % | SE | |
| Age groups (yrs) | ||||
| 45–54* | 55.9 | 2.4 | 63.3 | 1.8 |
| 55–64* | 44.1 | 2.4 | 36.7 | 1.8 |
| Male | 46.5 | 1.4 | 48.8 | 1.6 |
| Race/ethnicity | ||||
| Non-Hispanic White | 79.4 | 2.2 | 75.0 | 2.3 |
| Non-Hispanic Black | 8.9 | 0.1 | 10.9 | 1.6 |
| Risk factors | ||||
| Ages 45–54 | ||||
| Diabetes | 8.0 | 1.1 | 10.5 | 0.9 |
| High cholesterol* | 26.1 | 2.5 | 18.5 | 1.8 |
| High blood pressure | 13.8 | 1.6 | 11.8 | 1.2 |
| Current smoker | 28.8 | 2.7 | 25.4 | 2.5 |
| Obese* | 26.0 | 2.4 | 34.9 | 2.2 |
| Ages 55–64 | ||||
| Diabetes | 16.1 | 1.6 | 18.2 | 2.4 |
| High cholesterol* | 37.0 | 1.7 | 20.7 | 2.0 |
| High blood pressure | 23.3 | 1.5 | 20.0 | 2.0 |
| Current smoker | 24.2 | 2.1 | 18.6 | 2.1 |
| Obese* | 30.7 | 2.1 | 41.9 | 2.5 |
Notes: Estimates may differ from other published reports due to differences in sample selection.
The study sample consists of subjects who completed the morning fasting glucose component of the NHANES examination and who were not missing values on analytic variables and who were not previously diagnosed with a heart attack.
Obesity is not part of risk function calculations.
Percents are based on weighted n.
Diabetes is defined as self-reported diabetes or taking diabetes medication or insulin or having a fasting glucose level of ≥126 mg/dL.
High Cholesterol is defined as total cholesterol ≥240 mg/dL.
High blood pressure is defined as having mean measured systolic reading of ≥140 mm Hg or diastolic ≥90 mm Hg.
Current smoking is defined as having smoked ≥100 cigarettes and currently smoking every day or on some days.
Obesity is defined as a body mass index of ≥30 kg/m2.
Estimates across years are significantly different at the P ≤ .05 level.
Table 2.
Mean 10-year CHD risk among persons aged 45–64: United States, 1988–1994 and 2005–2008
| NHANES III, 1988–1994 | NHANES 2005–2008 |
% Change | |||
|---|---|---|---|---|---|
| % | SE | % | SE | ||
| All races/ethnicity | |||||
| Ages 45–54 | |||||
| All* | 4.0 | 0.3 | 3.2 | 0.2 | −19.8 |
| Men* | 6.5 | 0.4 | 5.0 | 0.2 | −22.8 |
| Women | 1.6 | 0.1 | 1.4 | 0.1 | −13.6 |
| Ages 55–64 | |||||
| All* | 7.1 | 0.3 | 5.2 | 0.3 | −26.4 |
| Men* | 11.1 | 0.7 | 8.0 | 0.4 | −28.0 |
| Women* | 4.0 | 0.3 | 2.8 | 0.2 | −30.1 |
| Non-Hispanic White | |||||
| Ages 45–64* | 5.3 | 0.2 | 3.8 | 0.2 | −28.2 |
| Non-Hispanic Black | |||||
| Ages 45–64* | 5.8 | 0.3 | 4.1 | 0.2 | −30.4 |
Note: Risk calculated from Framingham Heart Study Risk Functions as described in Wilson 1998 and D’Agostino 2001.
Risks are estimated only for persons not previously diagnosed with a heart attack.
The sample size for 1988–1994 is 1862 and for 2005–2008 is 1563.
Age groups are collapsed to create stable estimates for race/ethnicity.
Change in risk across time periods is statistically significant at the P ≤ .05 level.
Discussion
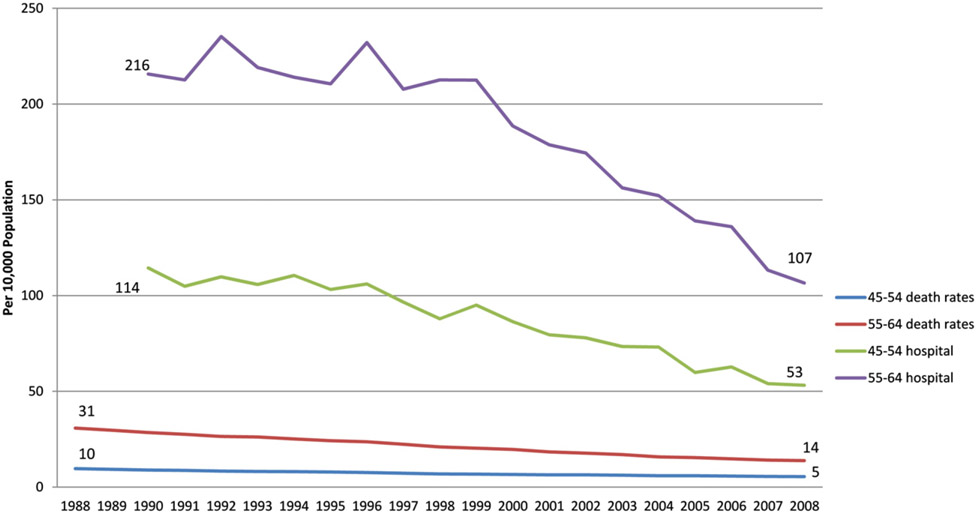
NHANES surveys provide national estimates of coronary risk factors for the civilian, non-institutionalized population of American adults. With these data, we show that the predicted 10-year risk of major coronary events among adults aged 45 to 64 years declined, despite the widely reported increase in the prevalence of overweight, obesity, and diabetes. Data from the National Vital Statistics System and the National Hospital Discharge Survey show that ischemic heart disease mortality and hospitalizations for these age groups also declined in the same period (Fig. 1.) The decline in risk for middle-aged adults is consistent with declines in CHD risk among older age groups. We found a 31% decline in risk for people aged 65 to 74 years during the same time period (data not shown).
Fig. 1.
Deaths and hospital discharges for ischemic heart disease (per 10,000 population), for ages 45 to 64 from 1988 to 2008. Note: Death rates are presented as deaths per 10,000 population. Death rates are for the underlying cause of death, and hospital discharge rates are for the first-listed diagnosis. ICD-CM codes for hospital discharge rates are 410 to 414. The ICD-9 codes for death rates for 1988 to 1998 are 410 to 414 and 429.2. ICD-10 codes for death rates for 1999 through 2008 are I20 to I25. (Source: Centers for Disease Control and Prevention, National Center for Health Statistics, National Hospital Discharge Survey and National Vital Statistics System.)
The present study provides evidence for the ongoing role of declining levels of certain risk factors in the reduction in coronary incidence, severity, and thus mortality. This finding is consistent with previous research, including studies of cardiovascular risk among those with a diabetes diagnosis [31]. It is also consistent with reports that the risk profile among the obese has improved along with a greater prevalence of treatment of risk factors [32,33]. For example, the percent of middle-aged persons with undiagnosed diabetes decreased from 1988 through 1994 to 2003 through 2006 [5,8]. Also, whereas the overall percent with hypertension (defined as elevated blood pressure or taking high blood pressure medication) increased from 1988 through 1994 to later periods, the share with uncontrolled high blood pressure among those with hypertension has declined, suggesting an increase in treatment. The same trend is seen for high cholesterol: From 1988 through 1994 to 2005 through 2008, the percentage of people with measured high serum cholesterol or taking cholesterol-lowering medication increased, whereas the percentage with measured high serum total cholesterol decreased [5,6]. The prevalence of these risk factors in the population has increased at the same time as the treatment of these conditions has also increased.
The smaller and not significant decrease in risk for women aged 45 to 54 compared with men offers some evidence, as other studies have suggested, that declines in CHD risk and mortality seem to be slower for women than men in this age group [3,34]. Patterns of smoking are likely part of the explanation for these results; there have been declines in rates of smoking for both men and women over the past several decades, but the decline among women started later and has not been as steep [5]. It might also be that, because the risk among women of this age is so low, further declines are difficult to achieve.
NHANES provides population-based data on multiple coronary risk factors in nationally representative samples of Americans. However, there are limitations of the present study to consider. The definitions of risk factors required by the Framingham Heart Study risk model are not consistent across the various factors. For example, the levels of blood pressure and serum cholesterol are evaluated regardless of treatment with medication, whereas medication treatment for diabetes by itself is considered a risk factor, irrespective of the measured level of fasting glucose. Some recent studies have questioned the performance of the Framingham risk scores, but these analyses were conducted on an older population than our study [35,36]. Although institutionalized persons are excluded from NHANES surveys, the effect on our analysis is likely minimal because the focus here is on persons aged 45 to 64 years who have a low rate of institutionalization. Also, in this analysis we do not take account of socioeconomic differences, which have been shown to be important in cardiovascular risk [37].
Because the model does not take account of advances in technology and treatment, the risk estimates presented here may underestimate future declines in cardiovascular risk. If improvements in treatment of CHD reduce the risk of death, then risk of CHD (which includes CHD mortality) could be even lower, even if the effects of the risk factors stay the same.
The Framingham Heart Study risk model does not include obesity as an independent variable. Consequently, the effect of obesity is assumed to work through its influence on the various risk factors. Studies addressing the question of whether obesity plays an independent role in cardiovascular risk are not conclusive. Using the longitudinal Framingham Heart Study data, Wilson et al. [38] show an increase in hypertension and cardiovascular sequelae among overweight and obese participants. More recently, other research found that adding waist circumference to the Framingham risk model did not improve its predictive ability for older adults [35]. The sample sizes of the present study do not allow an analysis by BMI subgroup to examine whether trends in CHD risk differ for overweight and obese people compared with healthy weight people.
Although CHD risk has declined as levels of obesity have increased, the role of obesity in future risk of CHD is unknown; future cohorts will be entering mid-life heavier and having lived with higher levels of obesity and diabetes for longer periods of time than current middle-aged cohorts. Although the risk is currently declining, it remains to be seen whether this declining risk will continue as these middle-aged cohorts grow older. Most studies only have data on the current weight of participants. Future models should attempt to take into consideration the changing role of obesity over a lifetime in the calculation of the risk of heart disease.
Acknowledgments
Dr. Paul Sorlie and Mr. Sean Coady of the National Heart, Lung and Blood Institute provided information which facilitated the risk computations. Dr. Richard Gillum, formerly of the National Center for Health Statistics, gave valuable advice in earlier versions of this paper. Nazik Elgaddal of the National Center for Health Statistics provided expert programming assistance.
Footnotes
An earlier version this analysis was presented by Dr. Kramarow as a poster at the 2008 American Public Health Association meeting.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- [1].Freedman VA, Crimmins E, Schoeni RF, Spillman BC, Aykan H, Kramarow E, et al. Resolving inconsistencies in trends in old-age disability: report from a Technical Working Group. Demography 2004;41:417–41. [DOI] [PubMed] [Google Scholar]
- [2].Crimmins EM. Trends in the health of the elderly. Annu Rev Public Health 2004;25:79–98. [DOI] [PubMed] [Google Scholar]
- [3].Kramarow E, Lubitz J, Lentzner H, Gorina Y. Trends in the health of older Americans, 1970-2005. Health Aff 2007;26:1417–25. [DOI] [PubMed] [Google Scholar]
- [4].Federal Interagency Forum on Aging-Related Statistics. Older Americans 2010: key indicators of well-being. Washington, DC: U.S. Government Printing Office; 2010. [Google Scholar]
- [5].National Center for Health Statistics. Health, United States 2010: with special feature on death and dying. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- [6].U.S. Centers for Disease Control and Prevention. National Center for Health Statistics. Health data interactive, www.cdc.gov/nchs/hdi.htm; [accessed April 29, 2011]. [Google Scholar]
- [7].Minino AM, Murphy SL, Xu JQ, Kochanek KD. Deaths: final data for 2008. National Vital Statistics Reports 2011;59(10). [PubMed] [Google Scholar]
- [8].Cowie CC, Rush KF, Byrd-Holt DD, Gregg EW, Ford ES, Geiss LS, et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care 2010;33:562–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lakdawalla DN, Bhattacharya J, Goldman DP. Are the young becoming more disabled? Health Aff 2004;23:168–76. [DOI] [PubMed] [Google Scholar]
- [10].Martin LG, Freedman VA, Schoeni RF, Andreski PM. Health and functioning among baby boomers approaching 60. J Gerontol 2009;64B:369–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Martin LG, Freedman VA, Schoeni RF, Andreski PM. Trends in disability and related chronic conditions among people ages fifty to sixty-four. Health Aff 2010;29:725–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988-1994 and 1999-2004. Am J Public Health 2010;100:100–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Daviglus ML, Liu K, Pirzada A, Yan LL, Garside DB, Greenland P, et al. Cardiovascular risk profile earlier in life and Medicare costs in the last year of life. Arch Intern Med 2005;165:1028–34. [DOI] [PubMed] [Google Scholar]
- [14].Goldman DP, Zheng Y, Girosi F, Michaud PC, Olshansky J, Cutler D, et al. The benefits of risk factor prevention in Americans aged 51 years and older. Am J Public Health 2009;99:2096–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff 2010;29:718–24. [DOI] [PubMed] [Google Scholar]
- [16].Caballero B. The global epidemic of obesity: an overview. Epidemiol Rev 2007;29:1–5. [DOI] [PubMed] [Google Scholar]
- [17].Jeffery RW, Harnack LJ. Evidence implicating eating as a primary driver for the obesity epidemic. Diabetes 2007;56:2673–6. [DOI] [PubMed] [Google Scholar]
- [18].Wang Y, Beydoun MA. The obesity epidemic in the United States–gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28. [DOI] [PubMed] [Google Scholar]
- [19].Wang YC, Colditz GA, Kuntz KM. Forecasting the obesity epidemic in the aging U.S. population. Obesity 2007;15:2855–65. [DOI] [PubMed] [Google Scholar]
- [20].Erlichman J, Kerbey AL, James WP. Physical activity and its impact on health outcomes. Paper 2: prevention of unhealthy weight gain and obesity by physical activity: an analysis of the evidence. Obes Rev 2002;3:273–87. [DOI] [PubMed] [Google Scholar]
- [21].Lee S, Harnack L, Jacobs DR Jr, Steffen LM, Luepker RV, Arnett DK. Trends in diet quality for coronary heart disease prevention between 1980-1982 and 2000-2002: the Minnesota Heart Survey. J Am Diet Assoc 2007;107:213–22. [DOI] [PubMed] [Google Scholar]
- [22].Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. NCHS data brief, no. 82. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- [23].Gillum RF. Secular trends in stroke mortality in African Americans: the role of urbanization, diabetes and obesity. Neuroepidemiology 1997;16:180–4. [DOI] [PubMed] [Google Scholar]
- [24].Declining prevalence of no known major risk factors for heart disease and stroke among adults—United States, 1991-2001. MMWR 2004;53:4–7. [PubMed] [Google Scholar]
- [25].Kim JK, Alley D, Seeman T, Karlamangla A, Crimmins E. Recent changes in cardiovascular risk factors among women and men. J Women’s Health 2006;15:734–46. [DOI] [PubMed] [Google Scholar]
- [26].D’Agostino RB Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA 2001;286:180–7. [DOI] [PubMed] [Google Scholar]
- [27].Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837–47. [DOI] [PubMed] [Google Scholar]
- [28].U.S. Centers for Disease Control and Prevention. www.cdc.gov/nchs/nhanes/nhanes2007-2008/GLU_E.htm; [accessed 14.11.11].
- [29].RTI International. SUDAAN language manual, release 10. Research Triangle Park (NC): RTI International; 2008. [Google Scholar]
- [30].American Diabetes Association. Standards of medical care in diabetes – 2010. Diabetes Care 2010;33(Suppl. 1):S11–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S. Diabetes Care 2011;34:1337–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med 2007;356:2388–98. [DOI] [PubMed] [Google Scholar]
- [33].Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA 2005;293:1868–74. [DOI] [PubMed] [Google Scholar]
- [34].Ezzati M, Friedman AB, Kulkarni S, Murray CJL. The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med 2008;5:557–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Rodondi N, Locatelli I, Aujesky D, Butler J, Vittinghoff E, Simonsick E, et al. Framingham Risk Score and alternatives for prediction of coronary heart disease in older adults. PLoS ONE 2012;7:e34287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].De Ruijter W, Westendorp RGJ, Assendelft WJJ, den Elzen WPJ, de Craen AJM, le Cessie S, et al. Use of Framingham risk score and new biomarkers to predict cardiovascular mortality in older people: population based observational cohort study. BMJ 2009;338:a3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Karmanlanga AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001-2006. Ann Epidemiol 2010;20:617–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Wilson WF, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk. Arch Intern Med 2002;162:1867–72. [DOI] [PubMed] [Google Scholar]