Abstract
Objectives:
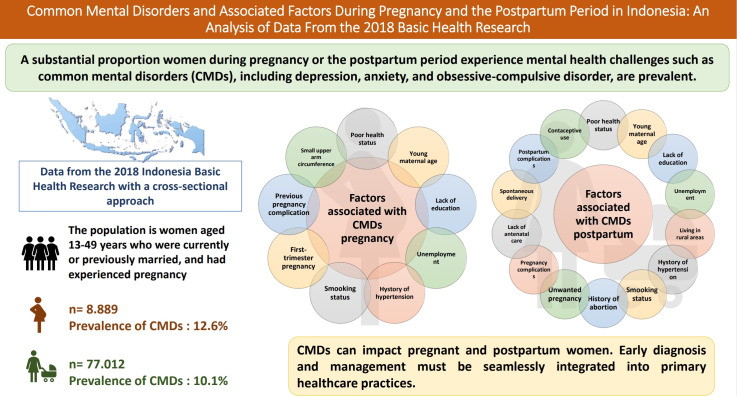
A substantial proportion of women experience mental health challenges during pregnancy or the postpartum period. Common mental disorders (CMDs), including depression, anxiety, and obsessive-compulsive disorder, are prevalent. Identifying causes and associated risk factors is imperative for early intervention and the prevention of mental health issues.
Methods:
This study utilized data from the 2018 Basic Health Research, which was conducted nationwide in Indonesia, using a crosssectional approach. We focused on women aged 13-49 years who were currently or previously married, and had experienced pregnancy, including 8889 pregnant women and 77 012 women who had delivered between January 1, 2013 and August 31, 2018. The Self-Reporting Questionnaire-20 was employed to assess CMDs. Multivariate logistic regression was performed.
Results:
The prevalence of CMDs in pregnant women was 12.6%, while postpartum mothers exhibited a prevalence of 10.1%. Poor health status displayed the strongest impact on CMDs during both pregnancy (adjusted odds ratio [aOR], 12.23; 95% confidence interval [CI], 9.01 to 16.60) and the postpartum period (aOR, 16.72; 95% CI, 14.85 to 18.82). Additional significant factors for both group include young maternal age, lack of education, unemployment, history of hypertension, and smoking status. Among pregnant women, CMDs was also associated with first-trimester pregnancy, previous pregnancy complications, and small upper arm circumference. For postpartum mothers, significant factors include living in rural areas, history of abortion, unwanted pregnancy, pregnancy complications, lack of antenatal care, spontaneous delivery, postpartum complications and contraceptive use.
Conclusions:
CMDs can impact in pregnant and postpartum women. Early diagnosis and management must be seamlessly integrated into primary healthcare practices.
Keywords: Mental disorder, Pregnancy, Postpartum period, Indonesia
GRAPHICAL ABSTRACT
INTRODUCTION
A seminal large-scale study, conducted through structured face-to-face surveys across 29 countries of diverse economic standing, revealed that about 1 in every 2 individuals worldwide will encounter a mental health disorder at some point in their lives [1]. The World Health Organization reports a global prevalence of mental health problems, with approximately 10% of pregnant women and 13% of postnatal mothers affected. In developing countries, these rates are higher at 15.6% during pregnancy and 19.8% in postpartum women [2].
Maternal mental health problems are a major public health concern worldwide, with common mental disorders (CMDs) representing the predominant category of issues during pregnancy and the postpartum period. CMDs include distressing conditions such as anxiety, depression, and unexplained somatic symptoms, which can lead to functional impairment in daily [3,4]. An international systematic review found that in low and lower-middle-income countries, the average prevalence rates of CMDs were 15.6% and 19.8% among pregnant and postpartum women, respectively, across various healthcare settings. Community-based studies have reported even higher rates, with 19.7% of pregnant women and 39.4% of postpartum women experiencing CMDs [5].
A meta-analysis of 102 studies, which included 221 974 participants from 34 countries, revealed a prevalence of anxiety of 15.2% [6]. Pregnant women have demonstrated greater susceptibility to anxiety than postpartum mothers. Depression during pregnancy affects 10% to 15% of individuals and is associated with an elevated risk of postnatal depression. While approximately 70% of new mothers experience the transient “baby blues,” postpartum depression impacts 10% to 20% of postpartum women [7-9]. The reported prevalence of postpartum depression varies widely, ranging from 0.5% to 60.8% globally and differing among studies [10,11]. These discrepancies in prevalence rates may be attributed to differences in population characteristics, methodologies, and measurement instruments.
In Indonesia, a study revealed that the prevalence of depression among pregnant women is 7.9%, with variation across trimesters. At 6 months postpartum, the overall prevalence of depression is 4.0%, with urban areas exhibiting higher rates (5.7%) than rural areas (2.9%) [12,13]. A wide range of multidimensional factors contribute to maternal mental disorders, encompassing physical, psychological, obstetric, pediatric, and socio-demographic domains. These factors include medical and psychological history, physical health conditions, experiences during childbirth, pediatric concerns, and socio-demographic variables [5,14]. Although numerous studies have been conducted in Indonesia, the present research is focused on mental health issues in pregnant and postpartum women as distinct groups. Its objective is to provide clearer insight into the extent of CMDs affecting these women.
Mental health issues during pregnancy and the postpartum period can have cascading effects on maternal and infant well-being. These problems may compromise self-care capacity, nutritional habits, and antenatal care attendance. Adverse outcomes associated with mental health conditions include higher risk of miscarriage, premature birth, and low birth weight, along with elevated rates of cesarean section or instrumental delivery [15,16]. Postnatal mental health issues can further impact mother-infant interactions, potentially negatively impacting parenting abilities and newborn care practices. This can extend to infant feeding practices, possibly leading to malnutrition [17]. The purpose of this study was to determine the prevalence of CMDs and to identify factors associated with these conditions among pregnant and postpartum women in Indonesia.
METHODS
Data Sources
This study involved a secondary analysis of data from the Indonesia Basic Health Survey (RISKESDAS 2018), a national cross-sectional, non-interventional survey overseen by the Ministry of Health. The survey employed a linear systematic and 2-stage sampling approach to cover 34 provinces, including 514 districts/cities, and targeted the entire population of households in Indonesia. In the first stage, probability proportional to size sampling was employed to systematically select census blocks within each urban/rural stratum of each district or city, resulting in a total of 30 000 census blocks. The second stage consisted of systematically choosing 10 households from each of the selected census blocks. Within these households, all members were included in the RISKESDAS sample and interviewed [18], and then the household members who were pregnant and postpartum women were selected as the sample for this study.
Participants
The study population consisted of married or previously married mothers aged 15 years to 49 years, drawn from the RISKESDAS sample. These participants were pregnant or had given birth between January 1, 2013 and August 31, 2018. The subset of pregnant women included 8889 participants, while the group of postnatal mothers comprised 77 012 participants.
Outcome Variables
The primary outcome assessed in this research was the prevalence of CMDs, which were measured using the Self Reporting Questionnaire-20 (SRQ-20). This questionnaire was developed by the World Health Organization and later adapted and translated by Hartono, a researcher at the Research and Development Agency of the Ministry of Health of the Republic of Indonesia, in 1995. The SRQ-20, which has a sensitivity of 88% and a specificity of 81%, is comprised of 20 questions that identify symptoms commonly associated with neurosis. Responses are scored with a 1 for “yes” and a 0 for “no.” The threshold for concern is set at a score of 6, with scores of 6 or higher indicating the presence of a CMD. The SRQ-20 is utilized in a national survey to evaluate emotional and mental disorders experienced in the previous month [19,20].
Independent Variables
We categorized the independent variables into 3 groups: socio-demographics, obstetrics, and health. Socio-demographic variables included the mother’s age (≤19, 20-34, or ≥35 years), education level (no school, elementary school, middle school, high school, or college), employment status (not employed or employed), and residential area (urban or rural). Obstetric variables encompassed gravida (primipara or multipara), pregnancy intention (unwanted, mistimed, or intended), trimester (first, second, or third), parity (0 or ≥1), history of antenatal care (no or yes), history of abortion (yes or no), history of pregnancy complications (yes or no), history of birth complications (yes or no), type of delivery (cesarean or instrumental, spontaneous, or unknown), history of postpartum complications (yes or no), and contraception use (no, yes, or unknown). Health variables included history of hypertension (yes or no), health status (poor, fair, or good), smoking status (yes or no), and midupper arm circumference (MUAC). MUAC measurements below 23.5 cm were considered to place pregnant women at risk of chronic energy deficiency [18]. History of hypertension was based on a diagnosis made by a doctor, while health status was self-assessed by respondents based on their condition over the past month.
Statistical Analysis
The analytical approach included univariate, bivariate, and multivariate analyses. Univariate analysis was used to evaluate the frequency of CMDs symptoms and quantify risk factors within the entire sample. Bivariate analysis, performed using binary logistic regression, was employed to examine the association between each independent variable and the presence of CMDs. Variables that were significant (p<0.05) in the binary regression model were then included in a multiple logistic regression multivariate analysis to establish the most appropriate model, as well as to calculate odds ratios (ORs) for the associations between significant variables. Each OR is presented with a 95% confidence interval (CI). The threshold for statistical significance was set at a 2-sided p-value of less than 0.05 (alpha 5%). All analyses were conducted using SPSS version 22 (IBM Corp., Armonk, NY, USA).
Ethics Statement
The information utilized in this research are secondary data from RISKESDAS 2018, which are publicly accessible. The Ethics Committee of the Indonesian Ministry of Health Center for Health Research and Development (Balitbangkes) approved the RISKESDAS 2018 study (No. LB.02.01/3/KE024/2018).
RESULTS
Table 1 presents the characteristics of the 8889 pregnant respondents and 77 012 postpartum mothers. Among the pregnant women, 12.6% experienced CMDs, a higher proportion than the 10.1% of postpartum mothers. For both pregnant and postpartum women, most were between 20 years and 34 years old, were not employed, and resided in rural areas. Overall, the health conditions of these women were favorable; they tended not to smoke, and most had no history of hypertension. Additionally, most of the pregnant women had a good nutritional status, as evidenced by a MUAC value of ≥23.5 cm. Obstetrically, the pregnant women were generally multiparous and had no history of abortion. Among postpartum mothers, the majority reported having desired their pregnancies; experiencing no complications during pregnancy, childbirth, or the postpartum period; attending antenatal care visits; and using contraception.
Table 1.
Socio-demographic, obstetric and health characteristics of pregnant and postpartum women in Indonesia, 2018
| Characteristics | Pregnancy (n = 8889) | Postpartum (n = 77 012) |
|---|---|---|
| Age (y) | ||
| ≤19 | 574 (6.5) | 1843 (2.4) |
| 20-34 | 6553 (73.7) | 49 658 (64.5) |
| ≥35 | 1762 (19.8) | 25 511 (33.1) |
| Educational level | ||
| No school | 708 (8.0) | 7483 (9.7) |
| Elementary school | 1647 (18.5) | 16 897 (21.9) |
| Middle school | 1990 (22.4) | 18 058 (23.4) |
| High school | 3057 (34.4) | 24 399 (31.7) |
| College | 1487 (16.7) | 10 175 (13.2) |
| Employment status | ||
| Not employed | 5053 (56.8) | 41 462 (53.8) |
| Employed | 3836 (43.2) | 35 550 (46.2) |
| Residential area | ||
| Urban | 3761 (42.3) | 31 305 (40.6) |
| Rural | 5128 (57.7) | 45 707 (59.4) |
| History of hypertension | ||
| Yes | 190 (2.1) | 3145 (4.1) |
| No | 6960 (78.3) | 51 245 (66.6) |
| Unknown | 1739 (19.6) | 22 613 (29.4) |
| Health status | ||
| Poor | 201 (2.3) | 1354 (1.8) |
| Fair | 2752 (31.0) | 22 869 (29.7) |
| Good | 5936 (66.8) | 52 789 (68.5) |
| Smoking status | ||
| Yes | 185 (2.1) | 1707 (2.2) |
| No | 8704 (97.9) | 75 305 (97.8) |
| Gestational period | ||
| First trimester | 2158 (24.3) | N/A |
| Second trimester | 3328 (37.4) | N/A |
| Third trimester | 3404 (38.3) | N/A |
| Gravida | ||
| Primipara | 3405 (38.3) | N/A |
| Multipara | 5484 (61.7) | N/A |
| Parity | ||
| Never | 2121 (23.9) | N/A |
| Ever | 6768 (76.1) | N/A |
| History of abortion | ||
| Yes | 1772 (19.9) | 13 235 (17.2) |
| No | 7117 (80.1) | 63 777 (82.8) |
| Previous pregnancy complications | ||
| Yes | 1163 (13.1) | N/A |
| No | 2421 (27.2) | N/A |
| Data not available | 5305 (59.7) | N/A |
| MUAC (cm) | ||
| <23.5 | 1483 (16.7) | N/A |
| ≥23.5 | 7406 (83.3) | N/A |
| Pregnancy intention | ||
| Unwanted | N/A | 1533 (2.0) |
| Mistimed | N/A | 6059 (7.9) |
| Intended | N/A | 69 420 (90.1) |
| Complications of recently completed pregnancy | ||
| Yes | N/A | 24 357 (31.6) |
| No | N/A | 52 655 (68.4) |
| Antenatal care | ||
| No | N/A | 4113 (5.3) |
| Yes | N/A | 72 899 (94.7) |
| Childbirth complications | ||
| Yes | N/A | 3001 (3.9) |
| No | N/A | 74 011 (96.1) |
| Mode of delivery | ||
| CS or instrumental | N/A | 12 738 (16.5) |
| Spontaneous | N/A | 62 615 (81.3) |
| Data not available | N/A | 1659 (2.2) |
| Postpartum complications | ||
| Yes | N/A | 7921 (10.3) |
| No | N/A | 67 432 (87.5) |
| Data not available | N/A | 1659 (2.2) |
| Contraceptive use | ||
| No | N/A | 22 271 (28.9) |
| Yes | N/A | 53 082 (68.9) |
| Data not available | N/A | 1659 (2.2) |
Values are presented as number (%).
N/A, not applicable; CS, cesarean section; MUAC, mid-upper arm circumference.
Table 2 presents the results of the bivariate analysis for pregnant women, indicating that certain socio-demographic variables were significantly associated with CMDs in this population. These variables included age, education, and employment status. However, residential area was not significantly associated with CMDs. Among health-related variables, significant associations were observed between CMDs and history of hypertension, overall health status, smoking status, and MUAC. Regarding obstetric history, the trimester of pregnancy, history of abortion, and previous pregnancy complications displayed significant correlations with the presence of CMDs. However, in the multivariate logistic regression analysis, abortion history was not significantly associated with CMDs.
Table 2.
Factors associated with CMDs among pregnant women in Indonesia, 2018 (n=8889)
| Variables | CMDs (%) |
cOR (95% CI) | aOR (95% CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Age (y) | ||||
| ≤19 | 17.2 | 82.8 | 1.50 (1.19, 1.88)** | 1.70 (1.29, 2.26)** |
| 20-34 | 12.2 | 87.8 | 1.48 (1.14, 1.91)** | 1.60 (1.25, 2.06)** |
| ≥35 | 12.4 | 87.6 | 1.00 (reference) | 1.00 (reference) |
| Educational level | ||||
| No school | 14.0 | 86.0 | 1.73 (1.31, 2.28)** | 1.35 (1.01, 1.82) |
| Elementary school | 15.7 | 84.3 | 1.20 (0.94, 1.52)** | 1.21 (0.94, 1.56) |
| Middle school | 13.4 | 86.6 | 1.05 (0.82, 1.35)** | 1.06 (0.82, 1.39) |
| High school | 12.0 | 88.0 | 0.87 (0.68, 1.12)** | 0.84 (0.65, 1.10)* |
| College | 8.6 | 91.4 | 1.00 (reference) | 1.00 (reference) |
| Employed status | ||||
| Not employed | 14.4 | 85.6 | 1.50 (1.31, 1.71)** | 1.37 (1.19, 1.58)** |
| Employed | 10.1 | 89.9 | 1.00 (reference) | 1.00 (reference) |
| History of hypertension | ||||
| Yes | 21.6 | 78.4 | 2.59 (1.77, 3.79)** | 1.89 (1.25, 2.86)* |
| No | 13.1 | 86.9 | 1.83 (1.28, 2.60)** | 1.43 (0.97, 2.10)* |
| Unknown | 9.6 | 90.4 | 1.00 (reference) | 1.00 (reference)* |
| Health status | ||||
| Poor | 55.2 | 44.8 | 15.04 (11.20, 20.18)** | 12.23 (9.01, 16.60)** |
| Fair | 20.3 | 79.7 | 4.85 (3.62, 6.51)** | 4.13 (3.05, 5.58)** |
| Good | 7.6 | 92.4 | 1.00 (reference) | 1.00 (reference) |
| Smoking status | ||||
| Yes | 33.0 | 67.0 | 3.56 (2.60, 4.86)** | 2.50 (1.78, 3.51)** |
| No | 12.2 | 87.8 | 1.00 (reference) | 1.00 (reference) |
| Gestational period | ||||
| First trimester | 16.6 | 83.4 | 1.64 (1.40, 1.91)** | 1.36 (1.15, 1.61)* |
| Second trimester | 11.7 | 88.3 | 1.50 (1.29, 1.76)** | 1.24 (1.10, 1.47)* |
| Third trimester | 10.9 | 89.1 | 1.00 (reference) | 1.00 (reference)* |
| History of abortion | ||||
| Yes | 14.6 | 85.4 | 1.24 (1.07, 1.44) | NI |
| No | 12.1 | 87.9 | 1.00 (reference)* | |
| Previous pregnancy complications | ||||
| Yes | 19.8 | 80.2 | 2.40 (1.96, 2.92)** | 2.09 (1.70, 2.58)** |
| No | 12.5 | 87.5 | 1.73 (1.46, 2.40)** | 1.61 (1.35, 1.93)** |
| Data not available | 9.3 | 90.7 | 1.00 (reference) | 1.00 (reference) |
| MUAC (cm) | ||||
| <23.5 | 15.4 | 84.6 | 1.34 (1.14, 1.57)* | 1.21 (1.02, 1.43)* |
| ≥23.5 | 12.0 | 88.0 | 1.00 (reference)* | 1.00 (reference)* |
CMDs, common mental disorders; cOR, crude odds ratio; aOR, adjusted odds ratio; CI, confidence interval; MUAC, mid-upper arm circumference; NI, not included.
p<0.05,
p<0.01.
Pregnant respondents with previous pregnancy complications were around twice as likely to experience CMDs (adjusted odds ratio [aOR], 2.09; 95% CI, 1.70 to 2.58) as those without such a history. Mothers in poor health had approximately 12 times the likelihood of CMDs compared to those in good health (aOR, 12.23; 95% CI, 9.01 to 16.60). Furthermore, pregnant women who smoked were nearly 3 times as likely to experience CMDs than non-smokers (aOR, 2.50; 95% CI, 1.78 to 3.51). Younger age, lack of formal education, lack of employment, history of hypertension, first-trimester pregnancy, and a MUAC of less than 23.5 cm were associated with a greater likelihood of CMDs among pregnant women.
As Table 3 demonstrates, among postpartum women, all socio-demographic, health, and obstetric variables were significantly associated with the presence of CMDs. However, in the multivariate logistic regression analysis, birth complications were not significantly associated with CMDs. Postpartum mothers with poor health status were over 16 times more likely to experience CMDs (aOR, 16.72; 95% CI, 14.85 to 18.82) than those in good health. Mothers with no formal education were nearly 3 times more susceptible to CMDs compared to those with a college education (aOR, 2.64; 95% CI, 2.34 to 2.97). Additionally, women who had experienced pregnancy or postpartum complications, who smoked, who underwent spontaneous delivery, and who used contraception each had around twice the likelihood of experiencing CMDs relative to their respective reference groups.
Table 3.
Factor associated with CMDs among postpartum women in Indonesia, 2018 (n=77 012)
| Variables | CMDs (%) |
cOR (95% CI) | aOR (95%CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Age (y) | ||||
| ≤19 | 12.9 | 87.1 | 1.23 (1.07, 1.42)** | 1.39 (1.19, 1.61)** |
| 20-34 | 9.6 | 90.4 | 1.39 (1.21, 1.60)** | 1.47 (1.26, 1.71)** |
| ≥35 | 10.7 | 89.3 | 1.00 (reference) | 1.00 (reference) |
| Educational level | ||||
| No school | 14.3 | 85.7 | 3.19 (2.86, 3.56)** | 2.64 (2.34, 2.97)** |
| Elementary school | 12.6 | 87.4 | 1.70 (1.57, 1.84)** | 1.63 (1.49, 1.78)** |
| Middle school | 10.4 | 89.6 | 1.45 (1.34, 1.57)** | 1.41 (1.28, 1.53)** |
| High school | 8.9 | 91.1 | 1.16 (1.08, 1.26)** | 1.14 (1.04, 1.24)** |
| College | 5.0 | 95.0 | 1.00 (reference) | 1.00 (reference) |
| Employed status | ||||
| Not employed | 10.7 | 89.3 | 1.16 (1.10, 1.22)* | 1.,06 (1.00, 1.11)* |
| Employed | 9.3 | 90.7 | 1.00 (reference) | 1.00 (reference) |
| Residential area | ||||
| Urban | 9.5 | 90.5 | 0.91 (0.86, 0.95)* | 0.94 (0.89, 0.99)* |
| Rural | 10.4 | 89.6 | 1.00 (reference) | 1.00 (reference) |
| History of hypertension | ||||
| Yes | 18.3 | 81.7 | 2.68 (2.42, 2.97)** | 1.49 (1.33, 1.67)** |
| No | 10.6 | 89.4 | 1.88 (1.71, 2.06)** | 1.21 (1.,09, 1.35)** |
| Unknown | 7.7 | 92.3 | 1.00 (reference) | 1.00 (reference) |
| Health status | ||||
| Poor | 55.3 | 44.7 | 21.76 (19.42, 24.38)** | 16.72 (14.85, 18.82)** |
| Fair | 18.2 | 81.8 | 5.56 (4.97, 6.22)** | 4.80 (4.27, 5.40)** |
| Good | 5.4 | 94.6 | 1.00 (reference) | 1.00 (reference) |
| Smoking status | ||||
| Yes | 24.5 | 75.5 | 3.02 (2.69, 3.38)** | 2.23 (1.97, 2.53)** |
| No | 9.7 | 90.3 | 1.00 (reference) | 1.00 (reference) |
| History of abortion | ||||
| Yes | 12.4 | 87.6 | 1.33 (1.26, 1.41)* | 1.12 (1.04, 1.20)* |
| No | 9.6 | 90.4 | 1.00 (reference) | 1.00 (reference) |
| Pregnancy intention | ||||
| Unwanted | 20.5 | 79.5 | 2.51 (2.21, 2.85)** | 1.72 (1.50, 1.98)** |
| Mistimed | 15.8 | 84.2 | 1.38 (1.20, 1.60)** | 1.18 (1.01, 1.38)** |
| Intended | 9.3 | 90.7 | 1.00 (reference) | 1.00 (reference) |
| Complications of recently completed pregnancy | ||||
| Yes | 15.4 | 84.6 | 2.23 (2.13, 2.34)** | 1.70 (1.61, 1.79)** |
| No | 7.6 | 92.4 | 1.00 (reference) | 1.00 (reference) |
| Antenatal care | ||||
| No | 12.1 | 87.9 | 1.25 (1.13, 1.38)* | 1.13 (1.01, 1.26)* |
| Yes | 10.0 | 90.0 | 1.00 (reference) | 1.00 (reference) |
| Childbirth complications | ||||
| Yes | 11.2 | 88.8 | 1.13 (1.00, 1.27)* | NI |
| No | 10.0 | 90.0 | 1.00 (reference) | |
| Mode of delivery | ||||
| CS or instrumental | 9.1 | 90.9 | 1.00 (reference) | 1.00 (reference) |
| Spontaneous | 10.1 | 89.9 | 1.70 (1.48, 1.93)** | 2.38 (1.99, 2.86)** |
| Data not available | 16.0 | 84.0 | 1.90 (1.64, 2.19)** | 2.80 (2.32, 3.40)** |
| Postpartum complications | ||||
| Yes | 21.7 | 78.3 | 2.97 (2.79, 3.15)** | 2.03 (1.90, 2.17)** |
| No | 16.0 | 84.0 | 1.46 (1.27, 1.68)** | 1.49 (1.25, 1.77)** |
| Data not available | 8.6 | 91.4 | 1.00 (reference) | 1.00 (reference) |
| Contraceptive use | ||||
| No | 9.6 | 90.4 | 1.00 (reference) | 1.00 (reference) |
| Yes | 10.1 | 89.9 | 1.70 (1.49, 1.94)** | 1.93 (1.58, 2.37)** |
| Data not available | 16.0 | 84.0 | 1.78 (1.55, 2.05)** | 1.97 (1.62, 2.41)** |
CMDs, common mental disorders; cOR, crude odds ratio; aOR, adjusted odds ratio; CI, confidence interval; CS, cesarean section; NI, not included.
p<0.05,
p<0.01.
DISCUSSION
In this study, the prevalence of CMDs among pregnant women was 12.6%. This figure is based on respondents answering in the affirmative to 6 or more questions out of 20, which suggests the presence of a CMDs according to the recommended 5/6 cut-off criterion.
This prevalence is low relative to similar studies conducted in Ethiopia (35.8%), Ireland (18.9%), and India (15.3%) [21-23]. The rate of CMDs during pregnancy was 16.6% in the first trimester, 11.7% in the second trimester, and 10.9% in the third trimester, indicating a decreasing trend over time. This aligns with findings from Brazil, which reported CMDs prevalence rates of 36.2% and 24.5% among pregnant women in the second and third trimesters, respectively, within a community population. In contrast, a cohort study in Saudi Arabia involving a hospital population observed an increasing trend in anxiety and depression from early pregnancy to the period before birth [24,25]. These variations suggest that the prevalence of CMDs is influenced by the characteristics of the study population.
In the postpartum group, the prevalence of CMDs was 10.1%, which is lower than the 15% rate found in a hospital-based cross-sectional study in Iran [26]. Furthermore, this figure is less than the prevalence of 17.22% reported in a recent systematic review that included 80 countries and regions [27]. The variation in prevalence across studies may be due to methodological differences, such as study design, setting (hospital vs. community), or sample size, as well as cultural factors and the level of development of the country or region. Additional disparities may result from differences in the measurement instruments used and the cut-off points selected. Notably, the SRQ-20 instrument utilized in this study was originally developed for use in primary healthcare settings [28].
This study identified socio-demographic factors associated with the risk of CMDs in pregnant and postpartum women, including age, education level, and employment status. Pregnant women under the age of 19 years were at a greater risk of developing CMD compared to those 35 years or older. This relationship may be attributed to emotional instability and a lack of preparedness for motherhood. These findings align with research from Iran, which indicates a heightened vulnerability to CMDs among younger pregnant women [26]. Conversely, studies conducted in Ethiopia report that older mothers face a higher risk of CMDs than their younger counterparts, representing conflicting evidence [29,30].
Mothers without formal education and those who were not employed faced notably higher risks of CMDs during pregnancy and the postpartum period. This risk decreased with higher levels of education. More educated mothers tend to engage in healthier behaviors, possess better problem-solving skills, and encounter more opportunities for personal growth. Furthermore, they typically have easier access to information about pregnancy and the postpartum period, which can improve their physical and mental preparedness [21,26]. Research conducted by Tauqeer et al. [31] indicates that homemakers, who balance a variety of responsibilities, may experience mental health challenges due to feelings of reduced self-esteem, self-confidence, and independence.
The prevalence of CMDs among postpartum mothers was generally higher in rural areas than in urban regions, as observed in research by Ginja et al. [32] in Northern England, which underscored the heightened risks of depression and anxiety among rural mothers. Although urban areas are frequently linked with more widespread mental health issues [13], it is important to recognize that rural regions, despite their perceived tranquility, may lack essential resources for physical and mental well-being.
Physical health factors also contribute to the occurrence of CMDs. Mothers who reported being in poor health or had chronic diseases, such as hypertension, were at comparatively high risk of exhibiting CMDs. This aligns with findings from research conducted in European countries and Ethiopia, which highlight the links between physical and mental health. Individuals with poor health or chronic illnesses are more susceptible to psychological stress and may experience heightened feelings of sadness or worry about their well-being [21,30]. Smoking was also correlated with the presence of CMDs. Studies have shown that although nicotine may provide temporary relaxation, it does not effectively alleviate anxiety and tension [31].
Pregnant women are more likely to develop CMDs during the first trimester than in later stages, which may be attributed to hormonal changes that require maternal adjustment [25,30]. Research indicates that women who have undergone abortions may face a higher risk of CMDs, experiencing symptoms such as depression, worry, reduced self-esteem, nightmares, guilt, and regret, all of which can adversely affect mental health during the perinatal period [21,29,30,33]. Mothers who express a lack of desire for pregnancy face an increased risk of CMDs compared to those with planned pregnancies [31]. The physical, hormonal, and psychological changes that occur during pregnancy necessitate careful planning and preparation. Global epidemiological research has shown that unplanned pregnancy is associated with postpartum depression [27].
A study conducted in Ethiopia revealed that pregnant women who do not attend antenatal care face a higher likelihood of experiencing CMDs than those who do participate [31]. Attendance at antenatal care sessions can increase self-esteem, improve maternal and social resilience, and provide knowledge about pregnancy, childbirth, and preparedness for the postpartum period, including aspects of mental health [34]. Additionally, mothers with a MUAC of less than 23.5 cm are at a relatively high risk of CMDs, suggesting a relationship between nutritional deficiencies and depression. In Indonesia, MUAC represents a fairly reliable indicator of the risk of nutritional deficiency [35,36].
Notably, mothers who underwent spontaneous delivery were more likely to experience CMDs than those who gave birth via cesarean section or other procedures. This contrasts with findings from other studies that have linked cesarean delivery with a comparatively high risk of mental health issues [37,38]. The rising prevalence of cesarean deliveries in Indonesia, particularly among the middle and upper economic classes, may contribute to the observed lower risk of CMDs in mothers opting for cesarean sections [39]. Complications during pregnancy or the postpartum period significantly impact the incidence of CMDs. Several studies have indicated that complications such as hyperemesis, infection, hypertension, fetal distress, and premature membrane rupture can lead to prolonged physical health issues that extend into the postpartum period. Poor health often leads to stress due to pain, fatigue, and functional limitations [13,21,29,38].
Contraceptive use has been identified as a potential contributing factor to CMDs. In a cross-sectional study from New York City, hormonal contraceptives were linked to mood swings and aggravated psychiatric symptoms in individuals with histories of mental health issues. Hormonal fluctuations may cause women to experience mood swings or unpredictable emotions, heightening their vulnerability to feelings of anger, sadness, sensitivity, apathy, and potentially depression [40].
This study was limited by its cross-sectional design, which precluded the monitoring of CMDs symptoms throughout the peripartum period and the establishment of causal relationships between variables. Additionally, biological factors that may influence CMDs were not explored. Despite these limitations of this community-based research, its findings are generalizable to the broader population, which is a notable strength.
The prevalence of CMDs in pregnant women in Indonesia exceeds that in postpartum mothers. Socio-demographic, health, and reproductive factors are shared between these groups. Mental health screening for pregnant and postpartum women should consider the associated risk factors and the adverse effects of CMDs on mothers, children, and families. Promotional campaigns for maternal mental health, especially during pregnancy, should emphasize the importance of sustainable antenatal care services.
Acknowledgements
The first author would like to express sincere gratitude to the Indonesia Endowment Fund for Education (LPDP) under the Ministry of Finance of the Republic of Indonesia for the scholarship that supported this research. Additionally, the authors would like to thank the Head of the Health Policy and Development Agency at the Ministry of Health of the Republic of Indonesia for providing the dataset and granting permission for the analysis, representation, and publication of the findings.
Footnotes
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
Funding
None.
Author Contributions
Conceptualization: Ariasih A, Besral, Budiharsana M, Ronoatmodjo S. Data curation: Ariasih A, Besral. Formal analysis: Ariasih A, Besral. Funding acquisition: None. Methodology: Budiharsana M, Ronoatmodjo S, Besral. Project administration: Ariasih A. Visualization: Ariasih A, Besral. Writing – original draft: Ariasih A, Besral. Writing – review & editing: Ariasih A, Besral, Budiharsana M, Ronoatmodjo S.
REFERENCES
- 1.McGrath JJ, Al-Hamzawi A, Alonso J, Altwaijri Y, Andrade LH, Bromet EJ, et al. Age of onset and cumulative risk of mental disorders: a cross-national analysis of population surveys from 29 countries. Lancet Psychiatry. 2023;10(9):668–681. doi: 10.1016/S2215-0366(23)00193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Maternal mental health [cited 2023 Dec 27]. Available from: https://www.who.int/teams/mentalhealth-and-substance-use/promotion-prevention/maternalmental-health.
- 3.Risal A. Common mental disorders. Kathmandu Univ Med J (KUMJ) 2011;9(35):213–217. doi: 10.3126/kumj.v9i3.6308. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Depression and other common mental disorders: global health estimates; 2017 [cited 2023 Dec 29]. Available from: https://www.who.int/publications/i/item/depression-global-health-estimates.
- 5.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139G–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. 2017;210(5):315–323. doi: 10.1192/bjp.bp.116.187179. [DOI] [PubMed] [Google Scholar]
- 7.Fawcett EJ, Fairbrother N, Cox ML, White IR, Fawcett JM. The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate Bayesian meta-analysis. J Clin Psychiatry. 2019;80(4):18r12527. doi: 10.4088/JCP.18r12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fellmeth G, Plugge E, Fazel M, Oo MM, Pimanpanarak M, Phichitpadungtham Y, et al. Prevalence and determinants of perinatal depression among labour migrant and refugee women on the Thai-Myanmar border: a cohort study. BMC Psychiatry. 2020;20(1):168. doi: 10.1186/s12888-020-02572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nurbaeti I, Deoisres W, Hengudomsub P. Postpartum depression in Indonesian mothers: its changes and predicting factors. Pacific Rim Int J Nurs Res. 2018;22(2):93–105. [Google Scholar]
- 10.Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in lowincome and middle-income countries. Lancet Psychiatry. 2016;3(10):973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: a narrative review. J Educ Health Promot. 2017;6:60. doi: 10.4103/jehp.jehp_9_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ariasih RA, Budiharsana M. Prevalence and sociodemographic factors associated with peripartum depression in Indonesia: national basic health research data 2018. J Kesehat Reproduksi. 2023;13(2):141–149. doi: 10.58185/jkr.v13i2.45. [DOI] [Google Scholar]
- 13.Putri AS, Wurisastuti T, Suryaputri IY, Mubasyiroh R. Postpartum depression in young mothers in urban and rural Indonesia. J Prev Med Public Health. 2023;56(3):272–281. doi: 10.3961/jpmph.22.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Insan N, Weke A, Forrest S, Rankin J. Social determinants of antenatal depression and anxiety among women in South Asia: a systematic review & meta-analysis. PLoS One. 2022;17(2):e0263760. doi: 10.1371/journal.pone.0263760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kotlar B, Gerson EM, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 2021;18(1):10. doi: 10.1186/s12978-021-01070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1097/01.aoa.0000744128.44930.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viswasam K, Eslick GD, Starcevic V. Prevalence, onset and course of anxiety disorders during pregnancy: a systematic review and meta analysis. J Affect Disord. 2019;255:27–40. doi: 10.1016/j.jad.2019.05.016. [DOI] [PubMed] [Google Scholar]
- 18.Indonesian Ministry of Health The 2018 Indonesia Basic Health Survey (RISKESDAS): national report. 2019. [cited 2023 Dec 29]. Available from: https://labmandat.litbang.kemkes.go.id/images/download/laporan/RKD/2018/Laporan_Nasional_RKD 2018_FINAL.pdf (Indonesian)
- 19.Idaiani S, Mubasyiroh R, Suryaputri IY, Indrawati L, Dharmayanti I. The validity of the self-reporting questionnaire-20 for symptoms of depression: a sub-analysis of the national health survey in Indonesia. Open Access Maced J Med Sci. 2022;10(E):1676–1682. doi: 10.3889/oamjms.2022.9999. [DOI] [Google Scholar]
- 20.Ganihartono I. Psychiatric morbidity among patients attending the Bangetayu community health centre in Indonesia. Bul Penelit Kesehat. 1996;24(4):42–51. [Google Scholar]
- 21.Woldetsadik AM, Ayele AN, Roba AE, Haile GF, Mubashir K. Prevalence of common mental disorder and associated factors among pregnant women in South-East Ethiopia, 2017: a community based cross-sectional study. Reprod Health. 2019;16(1):173. doi: 10.1186/s12978-019-0834-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mongan D, Lynch J, Hanna D, Shannon C, Hamilton S, Potter C, et al. Prevalence of self-reported mental disorders in pregnancy and associations with adverse neonatal outcomes: a population-based cross-sectional study. BMC Pregnancy Childbirth. 2019;19(1):412. doi: 10.1186/s12884-019-2572-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jha S, Salve HR, Goswami K, Sagar R, Kant S. Prevalence of common mental disorders among pregnant women-evidence from population-based study in rural Haryana, India. J Family Med Prim Care. 2021;10(6):2319–2324. doi: 10.4103/jfmpc.jfmpc_2485_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silva BP, Neves PA, Mazzaia MC, Gabrielloni MC. Common mental disorders and perinatal depressive symptoms: an integrative review. Rev Bras Enferm. 2020;73(Suppl 1):e20190823. doi: 10.1590/0034-7167-2019-0823. [DOI] [PubMed] [Google Scholar]
- 25.Alqahtani AH, Al Khedair K, Al-Jeheiman R, Al-Turki HA, Al Qahtani NH. Anxiety and depression during pregnancy in women attending clinics in a University Hospital in Eastern province of Saudi Arabia: prevalence and associated factors. Int J Womens Health. 2018;10:101–108. doi: 10.2147/IJWH.S153273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barat S, Ghanbarpour A, Mirtabar SM, Kheirkhah F, Basirat Z, Shirafkan H, et al. Psychological distress in pregnancy and postpartum: a cross-sectional study of Babol pregnancy mental health registry. BMC Pregnancy Childbirth. 2023;23(1):793. doi: 10.1186/s12884-023-06024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. 2021;11(1):543. doi: 10.1038/s41398-021-01692-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Organization of mental health services in developing countries Sixteenth report of the WHO Expert Committee on mental health. World Health Organ Tech Rep Ser. 1975;(564):1–41. [PubMed]
- 29.Duko B, Ayano G, Bedaso A. Depression among pregnant women and associated factors in Hawassa city, Ethiopia: an institution-based cross-sectional study. Reprod Health. 2019;16(1):25. doi: 10.1186/s12978-019-0685-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tamiru D, Misgana T, Tariku M, Tesfaye D, Alemu D, Weldesenbet AB, et al. Prevalence and associated factors of common mental disorders among pregnant mothers in rural eastern Ethiopia. Front Psychiatry. 2022;13:843984. doi: 10.3389/fpsyt.2022.843984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tauqeer F, Ceulemans M, Gerbier E, Passier A, Oliver A, Foulon V, et al. Mental health of pregnant and postpartum women during the third wave of the COVID-19 pandemic: a European cross-sectional study. BMJ Open. 2023;13(1):e063391. doi: 10.1136/bmjopen-2022-063391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ginja S, Jackson K, Newham JJ, Henderson EJ, Smart D, Lingam R. Rural-urban differences in the mental health of perinatal women: a UK-based cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):464. doi: 10.1186/s12884-020-03132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pourreza A, Batebi A. Psychological consequences of abortion among the post abortion care seeking women in Tehran. Iran J Psychiatry. 2011;6(1):31–36. [PMC free article] [PubMed] [Google Scholar]
- 34.Dadras O, Nakayama T, Kihara M, Ono-Kihara M, Seyedalinaghi S, Dadras F. The prevalence and associated factors of adverse pregnancy outcomes among Afghan women in Iran; findings from community-based survey. PLoS One. 2021;16(1):e0245007. doi: 10.1371/journal.pone.0245007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Madeghe BA, Kimani VN, Vander Stoep A, Nicodimos S, Kumar M. Postpartum depression and infant feeding practices in a low income urban settlement in Nairobi-Kenya. BMC Res Notes. 2016;9(1):506. doi: 10.1186/s13104-016-2307-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oktavianda YD, Ramadhan S, Mufida T, Mukminin U, Irwinda R. Maternal body mass index (BMI) and mid-upper arm circumference (MUAC) in early pregnancy as predictors of low birth weight infants. Adv Sci Lett. 2018;24(8):6203–6205. doi: 10.1166/asl.2018.12679. [DOI] [Google Scholar]
- 37.Khanum S, Jabeen S, Souza MD, Naz N, Andrade ZB, Nóbrega JF, et al. Mental health of mothers after natural childbirth and cesarean section: a comparative study in Kohat, Khyber Pakhtunkhwa, Pakistan. Texto Contexto Enferm. 2022;31:e20220140. doi: 10.1590/1980-265x-tce-2022-0140en. [DOI] [Google Scholar]
- 38.Swart T, Shandley K, Huynh M, Brown CM, Austin DW, Bhowmik J. Pregnancy complications and their association with postpartum depression symptoms: a retrospective study. Aust J Psychol. 2023;75(1):2247088. doi: 10.1080/00049530.2023.2247088. [DOI] [Google Scholar]
- 39.Pratiwi AM. The phenomenon of caesarean section as a trend. 2015. [cited 2024 Feb 9]. Available from: https://www.jurnalperempuan.org/wacana-feminis/fenomena-operasi-cesar-sebagai-tren (Indonesian)
- 40.Martell S, Marini C, Kondas CA, Deutch AB. Psychological side effects of hormonal contraception: a disconnect between patients and providers. Contracept Reprod Med. 2023;8(1):9. doi: 10.1186/s40834-022-00204-w. [DOI] [PMC free article] [PubMed] [Google Scholar]