Abstract
Background and setting:
From 2015 to 2020, the THRIVE project supported 7 US health departments to improve HIV prevention services for Black or African American (Black) and Hispanic or Latino gay, bisexual, and other men who have sex with men (GBM) and transgender women (TGW).
Methods:
We described services provided in the THRIVE PrEP continuum. Using Poisson regression models, we estimated associations between race or ethnicity and age and PrEP screening, linkage, and prescription. We examined associations between colocation of services and PrEP linkage and prescription for 2 sites.
Results:
THRIVE served 12,972 GBM without HIV; 37% of PrEP-eligible GBM were prescribed PrEP. THRIVE served 1185 TGW without HIV; 45% of PrEP-eligible TGW were prescribed PrEP. Black and Hispanic or Latino GBM were 29% (RR = 0.71, 95% CI: 0.66–0.77) and 19% (RR = 0.81, 95% CI: 0.75–0.87) less likely, respectively, to be prescribed PrEP than White GBM. GBM aged 18–24 years and 55 years or older were 19% (RR = 0.81, 95% CI: 0.75–0.87) and 22% (RR = 0.78, 95% CI: 0.67–0.9) less likely, respectively, to be prescribed PrEP compared with those aged 35–44 years. Colocated services were associated with a 54% (RR = 1.54, 95% CI: 1.44–1.64) and a 31% (RR = 1.31, 95% CI: 1.19–1.43) greater likelihood of PrEP linkage and prescription, respectively, compared with services at different locations.
Conclusions:
THRIVE provided PrEP to higher proportions of PrEP-eligible persons than current national estimates; however, PrEP use disparities persist. Colocation of services may be a useful component of jurisdictional strategies to increase PrEP coverage.
Keywords: HIV prevention, PrEP, men who have sex with men, transgender women, persons of color, health care access
INTRODUCTION
A disproportionate number of new HIV diagnoses occur among Black or African American (Black) and Hispanic or Latino gay, bisexual, or other men who have sex with men (GBM) and transgender women (TGW).1,2 Pre-exposure prophylaxis (PrEP) reduces the risk of acquiring HIV.3 However, disparities in PrEP use persist with larger gaps in PrEP coverage among Black and Hispanic or Latino persons compared with non-Hispanic White persons in the United States.4,5
The Targeted Highly Effective Interventions to Reverse the HIV Epidemic (THRIVE) demonstration project supported 7 health departments to provide comprehensive, culturally competent HIV prevention and care services for Black and Hispanic or Latino GBM and TGW.6 Recipient health departments developed community collaboratives consisting of funded and unfunded partnerships among health departments, community-based organizations (CBOs), behavioral and social services providers, and clinical providers. Applicants for THRIVE funding had to demonstrate high rates of HIV morbidity or mortality. The lessons learned in these communities are particularly valuable for similarly affected jurisdictions and applicable to implementation of the Ending the HIV Epidemic in the US (EHE) initiative, with the goal to substantially reduce HIV incidence nationally.7
THRIVE recipients implemented programs and activities to increase and improve PrEP services in their jurisdictions. Implementation was tailored by recipients to address the needs of their jurisdictions. All sites collected client-level program evaluation data to describe PrEP services including HIV testing, screening for indications for PrEP use, referring to a PrEP provider, linking to PrEP services, and prescribing PrEP. Our objectives were to describe the continuum of PrEP services provided in THRIVE and to evaluate associations among race or ethnicity, age, and colocation of services with PrEP screening, linkage, and prescription.
METHODS
The THRIVE Demonstration Project
THRIVE recipients were chosen from a pool of applicants to a Centers for Disease Control and Prevention (CDC) notice of funding opportunity. To be eligible, jurisdictions had to be (1) a metropolitan statistical area (MSA)/division with >2000 Black and/or Hispanic or Latino GBM living with diagnosed HIV or (2) a state in the fourth quartile for mortality rates as reported in its state progress report and with >1000 Black and/or Hispanic or Latino GBM living with diagnosed HIV in a specified MSA.6 THRIVE activities took place in Birmingham, AL; Baltimore, MD; Washington District of Columbia; New Orleans, LA; Brooklyn, New York City, NY; Philadelphia, PA; and Hampton Roads, VA. New York City, Baltimore, LA, and Virginia departments of health were also recipients of funding through the “Pre-exposure Prophylaxis* Intervention*Data-to-Care-*Evaluation” (PrIDE) project.8 Project activities to increase the use of PrEP among GBM and TGW, especially among Black and Hispanic or Latino persons, were complementary and intertwined to varying degrees in these jurisdictions. Data on service usage reported here reflect those combined PrIDE and THRIVE activities at cofunded sites but are referred to throughout as THRIVE. The THRIVE demonstration project was supported by the US Department of Health and Human Services Minority HIV/AIDS Fund. The CDC determined that the THRIVE evaluation was not research and was exempt from institutional board review.
PrEP Services in THRIVE
THRIVE implementation included community collaboratives, navigation programs, and attention to providing culturally competent services at all sites. Other programs and activities to increase and improve PrEP services varied by site. Other PrEP service activities implemented by 1 or more THRIVE sites included community-wide PrEP provider trainings, social marketing campaigns, learning collaboratives, community listening/focus groups conducted to understand barriers to PrEP, free or discounted PrEP medication, and resources to support PrEP provision. THRIVE funds were not used directly to purchase PrEP medication. PrEP service delivery models varied by project site and implementing agency. Some THRIVE collaborative partners had colocated HIV prevention services (eg, sexually transmitted infection testing and all PrEP services available in 1 location), while others provided a selection of services (eg, HIV testing and PrEP screening only) and referred clients to other agencies or locations for additional services.
THRIVE Data and Definitions
THRIVE recipients collected longitudinal, client-level data according to a standardized cross-site project evaluation plan. Deidentified data were reported to the CDC from 2015 through 2020. A THRIVE client was any person aged 18 years or older who received a THRIVE-funded service. The cross-site evaluation plan defined PrEP screening as assessing potential benefit for PrEP based on CDC PrEP clinical guidelines3; PrEP eligibility as the determination that a person does not have HIV and may benefit from PrEP based on CDC PrEP clinical guidelines; referral to PrEP as the process through which clients receive information about how to access PrEP services; linkage to PrEP as the outcome of the referral of a PrEP-eligible person, as indicated by the person’s attendance at an appointment at a clinical setting that provides PrEP services; and PrEP prescription as provision of a PrEP prescription by a health care provider. We defined colocation of services as having PrEP screening and PrEP prescription services provided at the same location. Age was determined at the time of THRIVE enrollment; age categories were 18–24 years, 25–34 years, 35–44 years, 45–54 years, and 55 years or older. Race and ethnicity were reported by THRIVE clients; categories were non-Hispanic Black, non-Hispanic White, Hispanic or Latino, other race (including non-Hispanic persons who identified as American Indian or Alaskan Native, Asian, Hawaiian or Pacific Islander, multiracial, or another race), and unknown race or ethnicity. THRIVE clients who reported male sex assigned at birth, male sex, and history of male sexual partners were classified as GBM. THRIVE clients who reported male sex assigned at birth and sex as female or TGW were classified as TGW.
Analysis
We determined the number of GBM and TGW without HIV served in THRIVE and the proportions screened for PrEP and eligible for PrEP. Among persons without HIV who were eligible for PrEP, we determined the proportions referred to PrEP services, linked to PrEP services, and prescribed PrEP during the project period. Steps in the PrEP services continuum may have occurred in the same clinical encounter or over a series of encounters. Missing continuum data were categorized as service not received, except where clients who received later events in the continuum (eg, were prescribed PrEP) were imputed to have received earlier steps (eg, PrEP screening).
We described the proportions of persons who received services in the THRIVE PrEP services continuum by race or ethnicity. We estimated relative risk (RR) and 95% confidence intervals (CI) between race or ethnicity and age and the binary outcomes of being screened, linked, and prescribed PrEP using Poisson regression models controlled for study site and fit separately for GBM and TGW THRIVE clients. Evaluation of PrEP screening was among all THRIVE clients without HIV while evaluation of PrEP linkage and prescription were among PrEP-eligible THRIVE clients. Race or ethnicity calculations were adjusted for age; age calculations were adjusted for race or ethnicity. Models controlled for study site as sites differed in baseline capacity, population racial and ethnic distribution, capacity of collaborative partners, and resources outside of THRIVE.
Two THRIVE sites provided data about location of services and included collaborative partners with and without colocated PrEP services. We used a Poisson regression model to evaluate associations between colocation of services and PrEP linkage and prescription. The model was adjusted for age group and race or ethnicity. All data were analyzed using SAS 9.4 (SAS Inc, NC). Although data collection from the fifth year of the project (September 2019 to September 2020) are included in this analysis, services were likely affected by the COVID-19 pandemic. The exact impact of COVID-19 on THRIVE participants was not measured.
RESULTS
Between 2015 and 2020, THRIVE served 38,866 clients without HIV, 12,972 (33%) GBM, and 1185 (3%) TGW. Age, race or ethnicity, and PrEP services for GBM and TGW THRIVE clients without HIV are summarized in Table 1. There were 9098 (70%) and 889 (75%) persons younger than 35 years among GBM and TGW clients, respectively. Among GBM, 2694 (21%) were White, 5743 (44%) Black, 2892 (22%) Hispanic or Latino, and 1643 (13%) other or unknown race or ethnicity. Among TGW, 87 (7%) were White, 585 (49%) Black, 378 (32%) Hispanic or Latina, and 135 (11%) other or unknown race or ethnicity. Among GBM served in THRIVE, 11,817 (91%) were screened for PrEP and 9505 (73%) were eligible for PrEP. Among PrEP-eligible GBM, 8271 (87%) were referred for PrEP, 5112 (54%) were linked to PrEP services, and 3544 (37%) were prescribed PrEP (Table 1). Among TGW served in THRIVE, 829 (70%) were screened for PrEP and 664 (56%) were eligible for PrEP. Among PrEP-eligible TGW, 600 (90%) were referred for PrEP, 367 (55%) were linked to PrEP services, and 299 (45%) were prescribed PrEP. THRIVE provided PrEP services to 9598 Black, Hispanic or Latino GBM, and TGW.
TABLE 1.
Characteristics of Gay, Bisexual, and Other Men Who Have Sex With Men and Transgender Women Without HIV Who Received Services in the THRIVE Demonstration Project, 2015-2020
| GBM* |
TGW† |
|||
|---|---|---|---|---|
| N | % | N | % | |
| TOTAL | 12,972 | 100 | 1185 | 100 |
| Age (yr) | ||||
| 18–24 | 3259 | 25 | 371 | 31 |
| 25–34 | 5839 | 45 | 518 | 44 |
| 35–44 | 2155 | 17 | 194 | 16 |
| 45–54 | 1068 | 8 | 64 | 5 |
| 55 years or older | 651 | 5 | 38 | 3 |
| Race or ethnicity | ||||
| White | 2694 | 21 | 87 | 7 |
| Black | 5743 | 44 | 585 | 49 |
| Hispanic or Latino‡ | 2892 | 22 | 378 | 32 |
| Other or unknown§ | 1643 | 13 | 135 | 11 |
| PrEP services | ||||
| Screened for PrEP‖ | 11,817 | 91 | 829 | 70 |
| Eligible for PrEP‖ | 9505 | 73 | 664 | 56 |
| Referred for PrEP¶ | 8271 | 87 | 600 | 90 |
| Linked to PrEP services¶ | 5112 | 54 | 367 | 55 |
| Prescribed PrEP¶ | 3544 | 37 | 299 | 45 |
Gay, bisexual, and other men who have sex with men.
Transgender women.
Hispanic persons can be of any race.
Other included American Indian/Alaska Native, Asian, Native Hawaiian/other Pacific Islander, multiracial.
Percentage among all GBM or TGW without HIV in THRIVE
Percentage among PrEP-eligible GBM or TGW in THRIVE
Figure 1A shows the percentages of GBM who were screened and eligible for PrEP among all GBM without HIV served in THRIVE and the percentages referred, linked for services, and prescribed PrEP among GBM eligible for PrEP, by race or ethnicity. Figure 1B shows the same metrics for TGW in THRIVE. Among GBM, all races or ethnicities had PrEP screening percentages ≥85%. Percentages eligible for PrEP were similar across all races or ethnicities (range 69%–76%). The percentage of PrEP-eligible GBM referred for PrEP differed by race or ethnicity with 78%, 86%, 92%, and 95% referred among White, Black, Hispanic or Latino, and other or unknown races or ethnicities, respectively. Less than 50% of PrEP-eligible White and Black GBM were linked for PrEP services, while 73% of Hispanic or Latino and 69% of GBM of other or unknown race or ethnicity were linked. Percentages of PrEP-eligible White and Black GBM prescribed PrEP were similar (34% and 32%, respectively), while 51% of Hispanic or Latino and 41% of GBM of other or unknown race or ethnicity were prescribed PrEP. Among TGW, percentages screened for PrEP differed by race or ethnicity with 91%, 81%, 56%, and 47% of White, Black, Hispanic or Latino, and TGW of other or unknown race or ethnicity screened, respectively. Similar percentages of White (67%) and Black (66%) TGW were eligible for PrEP, while only 47% of Hispanic or Latino and 30% of TGW of other or unknown race or ethnicity were eligible. More than 85% (range 87%–95%) of PrEP-eligible TGW were referred for PrEP across all races or ethnicities. Similar percentages of PrEP-eligible White (45%) and Black TGW (50%) were linked for PrEP services, while 70% of Hispanic or Latino and 58% of TGW of other or unknown race or ethnicity were linked. Percentages of PrEP-eligible TGW prescribed PrEP were 29%, 43%, 55%, and 48% among White, Black, Hispanic or Latino, and TGW of other or unknown race or ethnicity, respectively.
FIGURE 1.
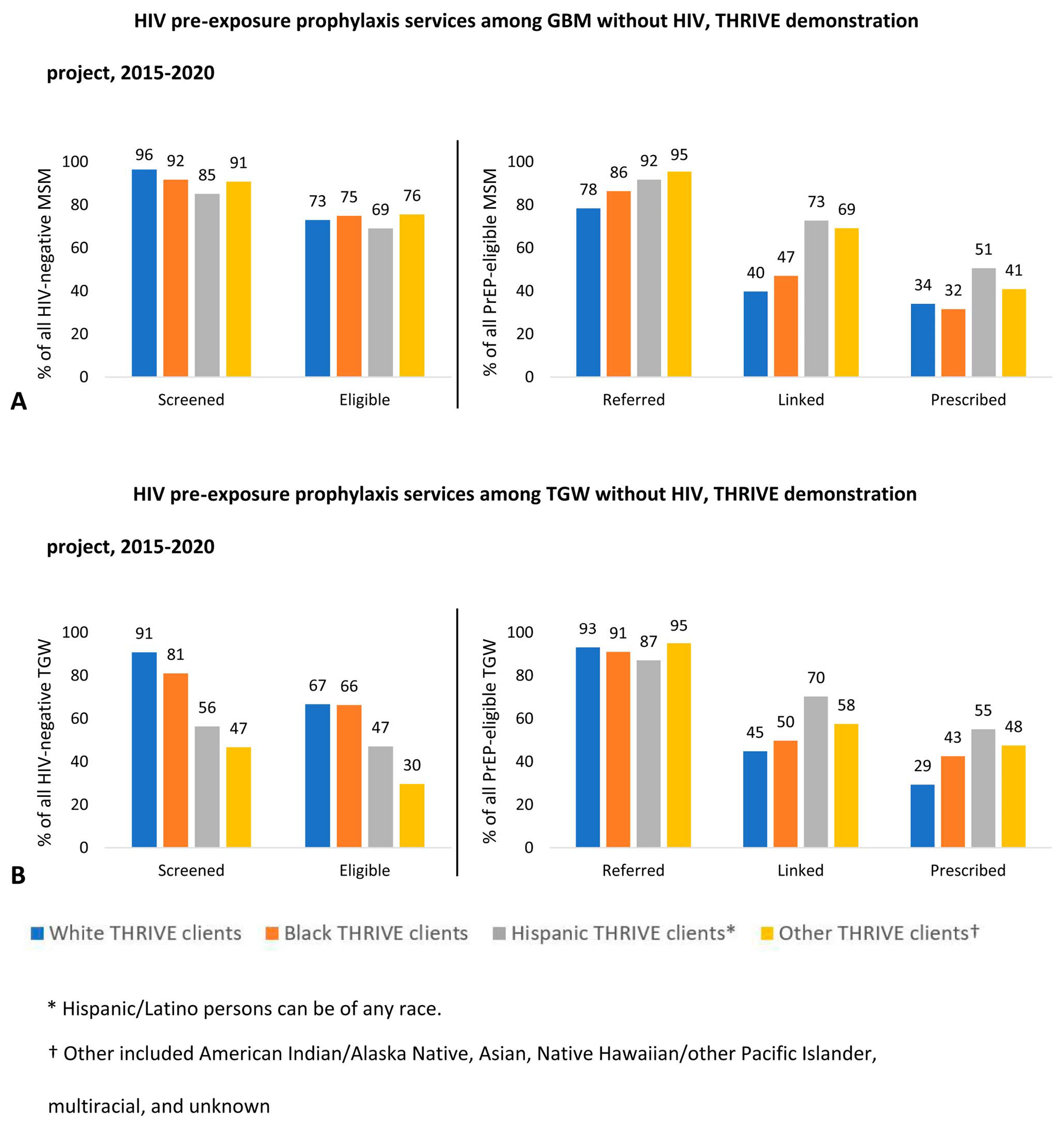
A, HIV pre-exposure prophylaxis services among GBM without HIV, THRIVE demonstration project, 2015–2020. A, Hawaiian/other Pacific Islander, multiracial. B, Adjusted for site and race or ethnicity.
We summarize estimated adjusted risk ratios (aRR) and 95% confidence intervals (95% CI) to evaluate associations between race or ethnicity, age, and PrEP outcomes in Table 2. Among GBM, estimated associations between race or ethnicity and PrEP screening or linkage to a PrEP provider were small and close to the null, indicating no differences in the likelihood of PrEP screening or linkage by race or ethnicity. However, all categories of non-White GBM were found less likely than White GBM to be prescribed PrEP. Black GBM were 29% (RR = 0.71, 95% CI = 0.66–0.77) less likely, Hispanic or Latino GBM were 19% (RR = 0.81, 95% CI: 0.75–0.87) less likely, and GBM of other or unknown race or ethnicity were 30% (RR = 0.7, 95% CI: 0.64–0.77) less likely than White GBM to be prescribed PrEP. Estimated associations between age and PrEP screening or linkage to PrEP provider were small and close to the null, indicating that the likelihood of PrEP screening and linkage did not vary by age group. However, we found that GBM aged 18–24 years and 55 years or older were 19% (RR = 0.81, 95% CI: 0.75–0.87) and 22% (RR = 0.78, 95% CI: 0.67–0.9) less likely, respectively, to be prescribed PrEP compared with those aged 35–44 years. Among TGW, estimated associations between race or ethnicity or age group with PrEP screening, linkage to PrEP provider, or PrEP prescription were small, indicating that likelihood of PrEP screening, linkage, or prescription did not vary by race or ethnicity or age group.
TABLE 2.
Association of PrEP Services With Race or Ethnicity and Age, THRIVE Demonstration Project, 2015-2020
| Screened for PrEP* |
Linked to PrEP† |
Prescribed PrEP† |
|
|---|---|---|---|
| aRR (95% CI)‡ | aRR (95% CI) | aRR (95% CI) | |
| GBM without HIV | |||
| Race or ethnicity§ | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 0.99 (0.97–1.02) | 1.01 (0.99–1.03) | 0.71 (0.66–0.77) |
| Hispanic or Latino ‖ | 0.99 (0.97–1.01) | 0.98 (0.96–1) | 0.81 (0.75–0.87) |
| Other or unknown¶ | 1.03 (1.01–1.06) | 1.02 (1–1.04) | 0.7 (0.64–0.77) |
| Age (yr)# | |||
| 18–24 | 1 (0.98–1.02) | 0.93 (0.9–0.96) | 0.81 (0.75–0.87) |
| 25–34 | 1.01 (0.99–1.03) | 1 (0.99–1.01) | 0.95 (0.9–1.01) |
| 35–44 | Reference | Reference | Reference |
| 45–54 | 1 (0.97–1.04) | 1 (0.97–1.02) | 0.92 (0.84–1.02) |
| 55 years or older | 0.98 (0.95–1.02) | 0.95 (0.9–1.01) | 0.78 (0.67–0.9) |
| TGW without HIV | |||
| Race or ethnicity§ | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 1 (0.84–1.20) | 0.97 (0.8–1.17) | 1.13 (0.8–1.6) |
| Hispanic or Latino ‖ | 1.02 (0.83–1.24) | 0.97 (0.79–1.18) | 1.06 (0.74–1.54) |
| Other or unknown¶ | 0.88 (0.65–1.18) | 1.09 (0.73–1.64) | 1.46 (0.8–2.68) |
| Age (yr)# | |||
| 18–24 | 0.99 (0.87–1.13) | 1.01 (0.88–1.16) | 0.98 (0.79–1.22) |
| 25–34 | 0.99 (0.86–1.13) | 1 (0.9–1.11) | 1.02 (0.85–1.22) |
| 35–44 | Reference | Reference | Reference |
| 45–54 | 0.99 (0.76–1.29) | 1.02 (0.88–1.19) | 1.02 (0.76–1.37) |
| 55 years or older | 0.94 (0.68–1.31) | 1.07 (0.81–1.41) | 1.27 (0.83–1.94) |
Among THRIVE clients without HIV
Among PrEP-eligible THRIVE clients.
Adjusted risk ratios (95% confidence intervals) estimated using Poisson regression.
Adjusted for site and age.
Hispanic/Latino persons can be of any race.
Other included American Indian/Alaska Native, Asian, Native Hawaiian/other Pacific Islander, multiracial.
Adjusted for site and race or ethnicity.
Bolded text indicates results where the 95% confidence interval does not include zero.
In Table 3, we summarize our analysis of the association between colocation of services and PrEP linkage and prescription for GBM and TGW without HIV at 2 THRIVE sites. We found colocated services were associated with a 54% greater likelihood of linkage to PrEP providers (RR = 1.54, 95% CI: 1.44–1.64, P <0.01) and 31% greater likelihood of PrEP prescription (RR = 1.31, 95% CI: 1.19–1.43, P <0.01) compared with collaborative partners where services were not colocated.
TABLE 3.
Association Between Colocation and PrEP Services Among PrEP-Eligible GBM and TGW in Two Sites With Different Service Location Models, THRIVE Demonstration Project, 2015-2020
| N PrEP-Eligible | n event | % Event | aRR* | 95% CI | P | |||
|---|---|---|---|---|---|---|---|---|
| Linked to PrEP provider | Colocated | 3439 | 3350 | 97.4 | 1.54 | 1.44 | 1.64 | <0.01 |
| Not colocated | 499 | 308 | 61.7 | Ref | ||||
| Prescribed PrEP | Colocated | 3439 | 2118 | 61.6 | 1.31 | 1.19 | 1.45 | <0.01 |
| Not colocated | 499 | 236 | 47.3 | Ref |
Adjusted risk ratio, adjusted for age and race or ethnicity, estimated using Poisson regression.
Colocation was defined as PrEP screening and PrEP prescription available at the same location.
DISCUSSION
In the THRIVE demonstration project, PrEP services were provided to more than 9500 Black and Hispanic or Latino GBM and TGW, populations who have historically lower rates of PrEP use compared with other populations.4,5,9 Six of the 7 THRIVE sites are EHE-funded phase 1 jurisdictions.8 THRIVE laid important groundwork for the ongoing work in the EHE initiative to reduce HIV incidence at least 90% by 2030 through diagnosis, prevention, treatment, and outbreak response.10
Most THRIVE clients were screened for PrEP, and there were no notable disparities in screening by age or race or ethnicity. Notable proportions of Black and Hispanic or Latino GBM and TGW who were eligible for PrEP received PrEP prescriptions, ranging from 32% to 55%. The EHE PrEP coverage indicator is the estimated percentage of individuals with indications for PrEP who have been prescribed PrEP. In 2020, 28% of US men with PrEP indications were prescribed PrEP; the EHE goal is 50% PrEP coverage by 2025.11 The proportions of PrEP-eligible Black and Hispanic or Latino GBM and TGW prescribed PrEP in THRIVE exceeded current national estimates of PrEP coverage.
THRIVE results suggest that focused efforts to improve PrEP services for Black and Hispanic or Latino GBM and TGW can increase PrEP coverage. Demonstration project data limit the ability to evaluate separate project components, and THRIVE implementation was tailored to each site’s needs and context. However, key THRIVE components that were defined by the project and implemented across all sites included establishment of community collaboratives, navigation programs, and attention to providing culturally competent services. THRIVE community collaboratives included organizations with established outreach among the priority populations. Most THRIVE collaborative members reported that their collaboratives represented the diversity of their communities and that those collaboratives were successful in implementing HIV prevention services for Black and Hispanic or Latino GBM and TGW.12 THRIVE’s community collaboratives may have contributed to the project’s success in reaching the priority communities by creating connections among CBOs, behavioral and social services providers, clinical providers, and health departments. A recent analysis of National HIV Surveillance System data for THRIVE sites and comparator sites found that the THRIVE community collaborative model was associated with decreased HIV diagnoses among Black and Hispanic or Latino MSM.13 Navigation services, also implemented by all THRIVE sites, may have contributed to THRIVE’s success by guiding THRIVE clients through the steps of the PrEP services continuum. This is supported by another analysis of THRIVE data which found that navigation was highly effective for linkage to PrEP.14 Providing culturally competent services, including through partnerships with organizations with established connections to the priority populations, may have contributed to THRIVE’s success by helping to reduce barriers to care for some individuals. An analysis of THRIVE data related to services provided to Hispanic or Latino persons found that Spanish language, culturally competent PrEP clinical services were associated with increased likelihood of PrEP linkage and prescription.15
Although the proportions of PrEP-eligible Black and Hispanic or Latino GBM and TGW prescribed PrEP in THRIVE exceeded national estimates, we found that Black and Hispanic or Latino GBM THRIVE clients eligible for PrEP were less likely to be prescribed PrEP compared with White GBM persons served in THRIVE, after controlling for site and age. We also found that younger GBM persons were less likely to be linked to or prescribed PrEP compared with GBM persons aged 35–44 years, after controlling for site and race or ethnicity. These findings are consistent with national reports of PrEP coverage that continue to show disparities in PrEP provision by race or ethnicity and age.16 We found these disparities in PrEP prescription despite finding no differences in the likelihood of PrEP linkage by race or ethnicity and age, suggesting a gap between PrEP linkage and actual prescription. Possible barriers to PrEP prescription after linkage to PrEP services include personal factors (eg, lack of interest in taking PrEP), health care provider factors (eg, limitations in PrEP clinical knowledge and attitudes/perceptions related to prescribing PrEP), and financial barriers (eg, cost of PrEP).17,18 THRIVE occurred before the statement by the Departments of Labor, Health, and Human Services, and the Treasury was made clarifying that insurance plans should cover without cost sharing any preventive services (including PrEP) recommended by the United States Preventive Services Task Force.19 PrEP medication access programs were available during THRIVE, but some sites reported that assisting clients to navigate these programs takes time that represents another PrEP access challenge.20 Increasing equity in PrEP coverage long term requires continued efforts to address barriers at all levels. Important strategies include enhancing provider education and organizational practices that influence PrEP prescribing and addressing barriers such as medical mistrust, stigma, and racism at the individual, network, health care, and structural levels.21–23
Colocation of services is one strategy to improve HIV prevention and care outcomes. In THRIVE, colocated services were associated with higher likelihoods of PrEP linkage and prescription compared with receiving services at different locations. Persons who were screened for PrEP at one location and were referred to another location for their PrEP appointment may have faced challenges such as the need to schedule in a separate system and a different time, arrange transportation to another location, and deal with delay before the possibility of obtaining a PrEP prescription. Having PrEP services available in one location avoids these challenges and simplifies the process of obtaining a PrEP prescription. Colocation of services is likely to improve efficiency of administering and navigating PrEP programs compared with services separated by location and provider. Other PrEP programs have similarly found improved outcomes with colocated services.24,25 These findings are also consistent with the broader literature demonstrating effectiveness of comprehensive service models in provision of syringe services and HIV treatment.26–29
This analysis of program evaluation data has some limitations. We may have underestimated services in the PrEP services continuum, including PrEP prescriptions, if THRIVE clients received services by providers outside of the THRIVE collaboratives. The likelihood that THRIVE clients may have received PrEP services outside of the collaborative varied by site because availability of resources and breadth of the collaborative differed by jurisdiction. For many THRIVE sites, there were limited PrEP services available outside of THRIVE. We were unable to describe barriers to receipt of PrEP services as these data were not included in THRIVE’s cross-site evaluation. A comprehensive PrEP continuum includes additional steps, including awareness of HIV risk and PrEP awareness, initiation, adherence, and persistence.30 These data were not included in THRIVE’s evaluation plan. Our results are particularly pertinent to other US jurisdictions with high rates of HIV morbidity or mortality because these were eligibility criteria for THRIVE. Those criteria may limit generalizability of these results to less-affected jurisdictions. Finally, THRIVE HIV prevention services were likely affected by the COVID-19 pandemic in 2020, with reduced service provision and data collection in all jurisdictions. The extent and effect of the pandemic on PrEP services in THRIVE jurisdictions were not measured in this project.
The THRIVE demonstration project successfully supported implementation of comprehensive HIV prevention services for Black and Hispanic or Latino GBM and TGW. Key THRIVE components including community collaborative models, culturally competent services, and PrEP navigation may have contributed to reaching large numbers of Black and Hispanic or Latino GBM and TGW. In THRIVE, higher proportions of PrEP-eligible persons received PrEP than current national estimates of PrEP coverage; however, disparities in PrEP prescriptions by race or ethnicity and age were observed. Additional barriers must be overcome to achieve equity in PrEP use, including overcoming stigma at multiple levels, building understanding and trust in health care systems and biomedical interventions, and addressing the social and structural factors that affect a person’s access to and use of HIV preventive services.21,22 Colocation of PrEP services increased the likelihood of PrEP linkage and prescription in THRIVE. Colocation of integrated HIV testing and PrEP education, screening, and clinical services may be a useful component of jurisdictions’ strategy for increasing PrEP coverage.
ACKNOWLEDGMENTS
The authors acknowledge the THRIVE project team for their contributions to this work, including Madison Albright, Robert A. Bonacci, Darnell Barrington, Genevieve Barrow, Mary Beth Cox, Kate Drezner, Zoe Edelstein, Anthony James, Jacky M. Jennings, Robert Jones, Anne Kimball, Michael Kharfen, Eric Mayes, Kenneth Pettigrew, Jerris L. Raiford, Erika Sugimori, and Benjamin Tsoi.
Minority HIV/AIDS Fund (PS15-1509).
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Updated); vol.31. Infographic. Atlanta, GA: Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2020. Accessed Sept 13 2021. [Google Scholar]
- 2.Becasen JS, Denard CL, Mullins MM, et al. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006-2017. Am J Public Health, 2019; 109:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update: A Clinical Practice Guideline. Atlanta, GA: US Department of Health and Human Services, CDC; 2018. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed Sept 13 2021. [Google Scholar]
- 4.Kanny D, Jeffries WLIV, Chapin-Bardales J, et al. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. MMWR Morb Mortal Wkly Rep., 2019; 68:801–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang YlA, Zhu W, Smith DK, et al. HIV preexposure prophylaxis, by race and ethnicity — United States, 2014–2016. MMWR Morb Mortal Wkly Rep., 2018; 67:1147–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. About THRIVE. Atlanta, GA: Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/hiv/research/thrive/about.html. Last reviewed: Nov 13 2019. Accessed Sept 21 2021. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Ending the HIV Epidemic: A Plan for America. 2020. Atlanta, GA: Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/endhiv/index.html. Accessed Sept 21 2021. [Google Scholar]
- 8.Mulatu MS, Carter JW, Flores SA, et al. Expanding PrEP Services for Men Who Have Sex with Men and Transgender Persons through Health Department Programs: Key Processes and Outcomes from Project PrIDE, 2015-2019. Public Health Reports, 2022; 138:31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sevelius JM, Poteat T, Luhur WE, et al. HIV testing and PrEP use in a national probability sample of sexually active transgender people in the United States. JAIDS J Acquired Immune Deficiency Syndromes, 2020; 84: 437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fauci AS, Redfield RR, Sigounas G, et al. Ending the HIV epidemic: a plan for the United States. JAMA. 2019; 321:844–845. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Core indicators for monitoring the Ending the HIV Epidemic initiative (preliminary data): national HIV Surveillance System data reported through June 2021; and preexposure prophylaxis (PrEP) data reported through March 2021. HIV Surveill Data Tables 2021; 2:18. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance-data-tables/vol-2-no-5/cdc-hiv-surveillance-tables-vol-2-no-5.pdf. Published October 2021. Accessed Apr 1 2022. [Google Scholar]
- 12.Tanner MR, Iqbal K, Dominguez KL, et al. Key factors for successful implementation of HIV prevention services by THRIVE community collaboratives. Public Health Rep., 137, 2021; 310, 316, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iqbal K, Dong X, Zhu W, et al. Decreased HIV diagnosis rates among Black and Hispanic or Latino MSM in U.S. jurisdictions supported by the THRIVE demonstration project, 2014-2019. Clin Infect Dis. 2022. Sep 17;ciac774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimball AA, Zhu W, Tanner MR, et al. The Effect of Navigation on Linkage to a PrEP Provider Among PrEP-Eligible Men Who Have Sex with Men Enrolled in THRIVE — United States, 2015–2020. AIDS Behav. 2022. doi: 10.1007/s10461-022-03931-y. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Bonacci RA, Tanner MR, Zhu W, et al. HIV Prevention Services for Hispanic/Latino Men Who Have Sex with Men and Transgender Women in THRIVE, 2015–2020. 2022. Manuscript submitted for Publication. [Google Scholar]
- 16.Centers for Disease Control and Prevention. Core indicators for monitoring the Ending the HIV Epidemic initiative (early release): National HIV Surveillance System data reported through December 2020; and preexposure prophylaxis (PrEP) data reported through September 2020. HIV Surveill Data Tables 2021; 2:41. https://www.cdc.gov/hiv/pdf/library/reports/surveillance-data-tables/vol-1-no-1/cdc-hiv-surveillance-tables-vol-1-no-1.pdf. Published March 2021. Accessed Sept 12 2021. [Google Scholar]
- 17.Mayer KH, Agwu A, Malebranche D. Barriers to the wider use of preexposure prophylaxis in the United States: a narrative review. Adv Ther. 2020;37:1778–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hart-Cooper GD, Allen I, Irwin CE, et al. Adolescent health providers’ willingness to prescribe pre-exposure prophylaxis (PrEP) to youth at risk of HIV infection in the United States. J Adolesc Health, 2018; 63:242–244. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Department of Labor. Employee Benefits Security Administration. Frequently asked questions: affordable care act implementation, Part 47. Available at: https://www.dol.gov/sites/dolgov/files/EBSA/about-ebsa/our-activities/resource-center/faqs/aca-part-47.pdf. Jul 19 2021. Accessed: Mar 3 2022.
- 20.U.S. Department of health and human services. Ready, set, PreP. Available at: https://readysetprep.hiv.gov/#how-to-enroll. Accessed Mar 3 2022.
- 21.Mizuno Y, Gelaude DJ, Crepaz N, et al. Healthcare Providers’ Views on Clinic Infrastructure and Practice Models that May Facilitate HIV Preexposure Prophylaxis (PrEP) Prescribing: A Qualitative Metasynthesis. Health Promot Pract, 2022; 23:999–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bonacci RA, Smith DK, Ojikutu BO. Toward greater pre-exposure prophylaxis equity: increasing provision and uptake for Black and Hispanic/Latino individuals in the U.S. Am J Prev Med., 2021; 61: S60–S72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanner MR, Miele P, Carter W, et al. Preexposure prophylaxis for prevention of HIV acquisition among adolescents: clinical considerations, 2020. MMWR Recomm Rep., 2020; 69:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frank L, Starzyk E, Hoxworth T, et al. HIV PrEP Implementation: a multi-level systems approach. Eval Program Plann., 2022; 90:101966. [DOI] [PubMed] [Google Scholar]
- 25.Roche SD, Odoyo J, Irungu E, et al. A one-stop shop model for improved efficiency of pre-exposure prophylaxis delivery in public clinics in western Kenya: a mixed methods implementation science study. J Int AIDS Soc. 2021; 24:e25845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mizuno Y, Higa DH, Leighton CA, et al. Is co-location of services with HIV care associated with improved HIV care outcomes? A systematic review. AIDS Care, 2019; 31:1323–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dasgupta S, Tie Y, Beer L, et al. Unmet needs for ancillary care services are associated with HIV clinical outcomes among adults with diagnosed HIV. AIDS Care. 2022; 34:606–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roth AM, Tran NK, Felsher M, et al. Integrating HIV preexposure prophylaxis with community-based syringe services for women who inject drugs: results from the project SHE demonstration study. JAIDS J Acquired Immune Deficiency Syndromes, 2021; 86:e61–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dasgupta S, Broz D, Tanner M, et al. Changes in reported injection behaviors following the public health response to an HIV outbreak among people who inject drugs: Indiana, . AIDS Behav. 2019;23:3257–3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, et al. Defining the HIV pre-exposure prophylaxis care continuum. AIDS, 2017; 31:731–734. [DOI] [PMC free article] [PubMed] [Google Scholar]


