Abstract
Background.
Neurosyphilis, a complication of syphilis, can occur at any stage of infection. Measuring the prevalence of neurosyphilis is challenging, and there are limited data on the prevalence of neurologic or ocular symptoms among patients with syphilis. We sought to describe the prevalence of neurologic and/or ocular symptoms among early syphilis (ES) cases and the clinical management of symptomatic cases enrolled in the STD Surveillance Network (SSuN) Neuro/Ocular Syphilis Surveillance project.
Methods.
Persons diagnosed with ES were selected for interviews based on current health department protocols in 5 participating SSuN jurisdictions from November 2016 through October 2017. All interviewed ES cases were screened for self-reported neurologic and/or ocular symptoms. Additional clinical information on diagnostic testing and treatment for cases concerning for neurosyphilis/ocular syphilis was obtained from providers.
Results.
Among 9123 patients with ES who were interviewed, 151 (1.7%; 95% confidence interval [CI], 1.4%–1.9%) reported ≥ 1 neurologic or ocular symptom. Of the 53 (35%) who underwent lumbar puncture, 22 (42%) had documented abnormal cerebrospinal fluid, of which 21 (95%) were treated for neurosyphilis/ocular syphilis. Among the remaining 98 symptomatic patients with no documented lumbar puncture (65%), 12 (12%) were treated for and/or clinically diagnosed with neurosyphilis/ocular syphilis.
Conclusions.
We observed a low prevalence of self-reported neurologic and/or ocular symptoms in interviewed ES cases. Approximately one-third of ES cases who self-reported symptoms underwent further recommended diagnostic evaluation. Understanding barriers to appropriate clinical evaluation is important to ensuring appropriate management of patients with possible neurologic and/or ocular manifestations of syphilis.
Keywords: neurosyphilis, ocular syphilis, early syphilis, complicated syphilis, prevalence
Neurosyphilis, an infection of the central nervous system by Treponema pallidum, is a rare but serious complication of syphilis that can result in debilitating sequelae. Ocular syphilis (eg, syphilitic uveitis, iritis, neuroretinitis, and optic neuritis) can be associated with neurosyphilis. Given the absence of a gold standard diagnostic modality, neurosyphilis or ocular syphilis is often a clinical diagnosis that relies on the interpretation of multiple tests, including cerebrospinal fluid (CSF) analysis [1]. Transient CSF abnormalities can be seen in a significant proportion of patients with early syphilis (ES) without neurological symptoms [2-4]. However, it is unclear if CSF laboratory abnormalities in the absence of neurologic symptoms predict future neurological sequelae. There are no data to suggest that therapy beyond a single intramuscular 2.4 million unit dose of benzathine penicillin G for ES improves long-term outcomes. Per Centers for Disease Control and Prevention (CDC) guidelines, persons who have syphilis and symptoms or signs suggesting neurologic disease (eg, cognitive dysfunction, motor or sensory deficits, auditory symptoms, cranial nerve palsies, and symptoms or signs of meningitis or stroke) or ophthalmic disease should undergo evaluation that includes analysis of CSF, obtained by performing a lumbar puncture (LP), ocular slit-lamp ophthalmologic examination, and otologic examination [1]. The CDC recommends that all patients with neurosyphilis and/or ocular syphilis be treated with intravenous aqueous penicillin G for 10–14 days to achieve adequate drug levels in the CSF [1].
Rates of primary and secondary syphilis (stages that reflect recent infection) have increased in the United States (US) since 2001, with concerns that an increase in adverse outcomes would follow. Recently, several large US urban areas have reported increases in neurosyphilis, including clusters of ocular syphilis [5, 6]. However, population-based data on the burden of neurosyphilis and ocular syphilis have been limited. Syphilis, including neurological involvement, is a nationally notifiable condition in the US with case reports provided to the CDC [7]. During 2009–2015, the proportion of ES cases, which include primary, secondary, or early latent syphilis cases, with identified neurosyphilis varied, but overall remained low at 1.8% [8]. However, case report data likely underestimate the true burden of neurosyphilis. Prior to 1 January 2018, the surveillance case definition for neurosyphilis or neurologic manifestations required documentation of abnormal CSF results [9]. Therefore, case reports underestimate burden if providers do not routinely screen patients for neurologic or ocular symptoms and perform LPs on symptomatic patients and will be biased toward patients most likely to be screened and/or undergo LP, such as persons infected with human immunodeficiency virus (HIV) [10, 11]. Additionally, the completeness of case report data is influenced by health department protocols, which may vary in terms of how syphilis cases are followed up to determine if a case might meet the neurosyphilis surveillance case definition. Furthermore, prior to 2018, case report data lacked specificity on the type of neurological manifestations with cases unable to be reported as having ocular or otic manifestations. Finally, it is unknown among representative populations what proportion of patients undergo LP, what proportion of these have abnormal CSF findings, and what proportion are treated with a CDC-recommended regimen for neurosyphilis and/or ocular syphilis.
The STD Surveillance Network (SSuN) Enhanced Neuro/Ocular Syphilis Surveillance project was established in 2016 to address significant gaps in the surveillance of ES cases with neurologic and/or ocular manifestations. Our primary objective was to describe the prevalence of self-reported neurologic and/or ocular symptoms among reported ES cases in participating SSuN jurisdictions with a secondary objective of describing the clinical management of symptomatic cases identified through the project.
METHODS
Study Population
The SSuN is a sentinel surveillance network that aims to improve the capacity of national, state, and local sexually transmitted disease (STD) programs to detect, monitor, and respond rapidly to trends in STDs. Five SSuN jurisdictions participated in the Enhanced Neuro/Ocular Syphilis Surveillance Project: Florida Department of Health, Multnomah County (Oregon) Health Department, New York City Department of Health and Mental Hygiene (NYC), Philadelphia Department of Public Health, and Washington State Department of Health. Per the project protocol, the prioritization of STD disease investigation, including patient interviews to facilitate partner services, for ES cases was based on local health department protocols. All jurisdictions investigated ES cases to ensure treatment and, with the exception of NYC, prioritized all reported ES cases for additional disease investigation activities that included data collection on presence of neuro/ocular symptoms (described below). NYC conducted data collection on ES cases prioritized for investigation that met specific risk criteria (Supplementary Text) and then selected a 10% random sample from all ES cases that would otherwise not have been prioritized for investigation. We included all ES cases reported between 1 November 2016 and 31 October 2017 that were prioritized for and received STD disease investigation within the participating jurisdictions.
Data Collection Procedures
Demographic, behavioral, clinical, and laboratory data are routinely collected during health department investigation of ES cases, including data from provider case reports, provider follow-up, and patient follow-up. To enhance routine surveillance, a standardized neurosyphilis and ocular syphilis data collection tool was incorporated into existing local investigation protocols. The tool included questions to be asked during patient interviews regarding patient-reported neurologic and/or ocular symptoms and having an LP as part of their ES clinical management (collected via patient questionnaire), as well as collection of clinical data from provider case reporting and follow-up.
For interviewed ES cases that met the criteria of (1) self-reported neurologic and/or ocular symptoms (eg, to disease intervention specialists), (2) documented treatment with a CDC-recommended antibiotic regimen for neurosyphilis and/or ocular syphilis, or (3) documented CSF testing, medical provider(s) involved in the ES case clinical management were contacted by health department staff for additional clinical information (collected via provider questionnaire).
During this follow-up, standardized information was gathered from medical provider(s) including diagnostic testing performed (eg, LP, ophthalmologic exam), laboratory test results (eg, CSF results), prescribed type and duration of antibiotic treatment, and whether the patient received a clinical diagnosis of neurosyphilis or ocular syphilis. Questionnaires were completed by providers or information was abstracted from medical charts by public health staff.
Presence of Self-reported Neurologic and/or Ocular Symptoms
An ES case with self-reported neurologic and/or ocular symptoms was defined as a patient reported with ES who received enhanced neurosyphilis screening as part of STD investigation and self-reported the presence of at least 1 of the following neurologic and/or ocular symptoms within the past 60 days: hearing change, hearing loss, tinnitus, headaches, altered mental status, stroke-like symptoms, eye pain, blurry vision, red eye, vision changes, flashing lights, floaters, vision loss, or “other neurologic and/or ocular symptoms.”
Diagnostic and Clinical Management Outcomes
Lumbar Puncture
Lumbar puncture completion was defined as either (1) the patient self-reported performance of LP as part of their syphilis care, (2) medical provider(s) documented LP performance in the provider questionnaire, or (3) there was documentation of CSF results (Venereal Disease Research Laboratory [VDRL] test, leukocyte, protein, and/or fluorescent treponemal antibody absorption test [FTA-ABS]) on the provider questionnaire.
Abnormal CSF
Abnormal CSF was defined as CSF results obtained from the provider questionnaire that met 1 of the following criteria: (1) reactive VDRL; (2) leukocyte count > 5 cells/μL in HIV-seronegative persons or > 20 cells/μL in HIV-seropositive persons; or (3) protein > 45 mg/dL and reactive CSF FTA-ABS testing [12, 13].
Treatment
Treatment for neurosyphilis or ocular syphilis was determined by documentation of treatment with an antimicrobial regimen recommended by the CDC for neurosyphilis and/or ocular syphilis [1] in the patient or provider questionnaire.
Clinical Diagnosis
Clinical diagnosis of neurosyphilis or ocular syphilis was defined as an interviewed ES case with a clinical diagnosis of neurosyphilis and/or ocular syphilis diagnosis designated on the provider questionnaire.
Ophthalmologic Examination
Ophthalmologic examination completion was defined as an interviewed ES case with performance of ophthalmologic examination designated on the provider questionnaire. An abnormal ophthalmologic examination was defined as having ≥ 1 of the following results indicated on the provider questionnaire: uveitis, scleritis/keratitis, retinitis/chorioretinitis, optic neuritis/neuropathy, or retinal detachment.
Data Analysis
We calculated the prevalence of ES cases with at least ≥ 1 self-reported neurologic or ocular symptom, referred to as “symptomatic ES cases,” with binominal confidence intervals (CIs) and determined the frequencies of specific neurologic or ocular symptoms.
We evaluated the diagnostic and clinical management outcomes in a clinical cascade for symptomatic ES cases by determining the proportion of symptomatic ES cases that underwent LP, followed by the proportion of symptomatic ES cases that underwent an LP with abnormal CSF results, the proportion of cases with abnormal CSF results treated with a CDC-recommended regimen for neurosyphilis and/or ocular syphilis, and the proportion of treated cases that had documentation of a clinical diagnosis of neurosyphilis and/or ocular syphilis. For ES cases that reported ≥ 1 ocular symptom, we calculated the proportion that had an LP and/or an ophthalmologic examination performed and, of those who underwent an ophthalmologic examination, the proportion that had abnormal ophthalmologic findings. Analyses were conducted using SAS version 9.4 soft-ware (SAS Institute, Cary, North Carolina). Data were collected as sentinel surveillance activities and were considered exempt from CDC human subjects review.
RESULTS
Study Population Characteristics
Overall, 13 071 ES cases were reported across the 5 participating jurisdictions between 1 November 2016 and 31 October 2017; 9123 (70%) were interviewed and received enhanced neurosyphilis screening (Table 1). Among interviewed ES cases, 87% were from jurisdictions in the East (Florida, NYC, and Philadelphia), the majority identified as male gender (85%) and as men who have sex with men (MSM) (82%), and almost half (43%) were known to be HIV infected.
Table 1.
Demographic, Behavioral, and Clinical Risk Factors of Reported Interviewed Early Syphilis Cases—STD Surveillance Networka, October 2016—November 2017
| Characteristic | All Interviewed Cases (N = 9123) | Cases Self-reporting ≥ 1 Neurologic or Ocular Symptom (n = 151) |
|---|---|---|
| No. (Column %) | No. (Column %) | |
| Jurisdiction by geographic region | ||
| East | 7950 (87) | 59 (39) |
| Florida | 4405 (48) | 19 (13) |
| New York City | 2715 (30) | 23 (15) |
| Philadelphia | 830 (9) | 17 (11) |
| West | 1173 (13) | 92 (61) |
| Multnomah County, Oregon | 201 (2) | 24 (16) |
| Washington State | 972 (11) | 68 (45) |
| Gender | ||
| Male | 7798 (85) | 136 (90) |
| Female | 1031 (11) | 13 (9) |
| Transgender male to female | 38 (0.4) | 0 (0) |
| Transgender female to male | 3 (0.03) | 0 (0) |
| Transgender unspecified | 10 (0.1) | 0 (0) |
| Unknown | 243 (2.7) | 2 (1) |
| Age group, y | ||
| 18–24 | 3633 (40) | 43 (28) |
| 25–34 | 3519 (39) | 57 (38) |
| 35–44 | 1872 (21) | 51 (34) |
| ≥ 45 | 0 (0) | 0 (0) |
| Missing | 99 (1) | 0 (0) |
| Race/ethnicity | ||
| AIAN/Asian/NHOPI | 216 (2) | 2 (1) |
| Black | 2915 (32) | 26 (17) |
| White | 2643 (29) | 84 (56) |
| Multiple races | 373 (4) | 7 (5) |
| Hispanic | 2509 (28) | 27 (18) |
| Refused | 467 (5) | 5 (3) |
| Gender and gender of sex partners | ||
| Women | 1112 (12) | 12 (8) |
| Men who have sex with women only | 325 (4) | 7 (5) |
| Men who have sex with men | 7459 (82) | 129 (85) |
| Missing | 227 (2) | 3 (2) |
| HIV status | ||
| Negative (tested negative at syphilis diagnosis) | 1957 (21) | 50 (33) |
| Positive (known positive or tested positive at syphilis diagnosis) | 3901 (43) | 73 (48) |
| Unknown | 3265 (36) | 28 (19) |
| Syphilis stage | ||
| Primary | 1355 (15) | 9 (6) |
| Secondary | 3123 (34) | 74 (49) |
| Early latent | 4645 (51) | 68 (45) |
| Highest RPR titer recorded | ||
| 1:1–1:8 | 1575 (17) | 13 (9) |
| 1:16–1:64 | 4243 (47) | 53 (35) |
| 1:128–1:512 | 2805 (31) | 72 (48) |
| ≥ 1:1024 | 192 (2) | 8 (5) |
| Unknown | 308 (3) | 5 (3) |
Abbreviations: AIAN, American Indian/Alaska Native; HIV, human immunodeficiency virus; NHOPI, Native Hawaiian, other Pacific Islander; RPR, rapid plasma reagin.
Five STD Surveillance Network jurisdictions participated in the enhanced surveillance project.
Prevalence and Frequency of Neurologic and/or Ocular Symptoms
Among 9123 ES cases screened for neurologic and/or ocular symptoms, 151 (1.7%; 95% CI, 1.4%–1.9%) reported ≥ 1 neurologic or ocular symptom (Table 1). Among symptomatic ES cases, 36% (n = 54) reported neurologic symptom(s) only, 34% (n = 51) reported ocular symptom(s) only, and 30% (n = 46) reported having both neurologic and ocular symptoms. Among symptomatic ES cases, 61% were from jurisdictions in the West (Washington State, Multnomah County) despite ES cases in the West accounting for only 13% of all interviewed ES cases. Most symptomatic ES cases identified as male (90%), were MSM (85%), and almost half (48%) were known to be HIV infected. Among all symptomatic ES cases, blurry vision (30%), headaches (39%), vision changes (22%), and tinnitus (21%) were the most commonly reported symptoms; 19% (n = 29) reported serious, debilitating symptoms such as vision loss, hearing loss, and/or stroke-like symptoms (Table 2).
Table 2.
Frequency of Self-reported Symptoms in Interviewed Early Syphilis Cases Self-reporting ≥ 1 Neurologic or Ocular Symptom—STD Surveillance Networka, October 2016–November 2017 (n = 151)
| Self-reported Symptoms | No. (%) |
|---|---|
| Ocular symptoms in past 60 db | |
| Blurry vision | 46 (30) |
| Vision changes | 33 (22) |
| Floaters | 22 (15) |
| Vision loss | 14 (9) |
| Red eye | 15 (10) |
| Eye pain | 12 (8) |
| Flashing lights | 15 (10) |
| Other (eg, photophobia) | 23 (15) |
| Neurologic symptoms in past 60 db | |
| Headaches | 58 (39) |
| Tinnitus (ringing in ears) | 32 (21) |
| Hearing change | 26 (17) |
| Hearing loss | 11 (7) |
| Altered mental status | 7 (5) |
| Other (eg, unsteadiness, dizziness, decreased memory) | 23 (15) |
| Stroke-like symptoms | 4 (3) |
Five STD Surveillance Network jurisdictions participated in the enhanced surveillance project.
Symptoms are not mutually exclusive.
Diagnostic and Clinical Management Outcomes
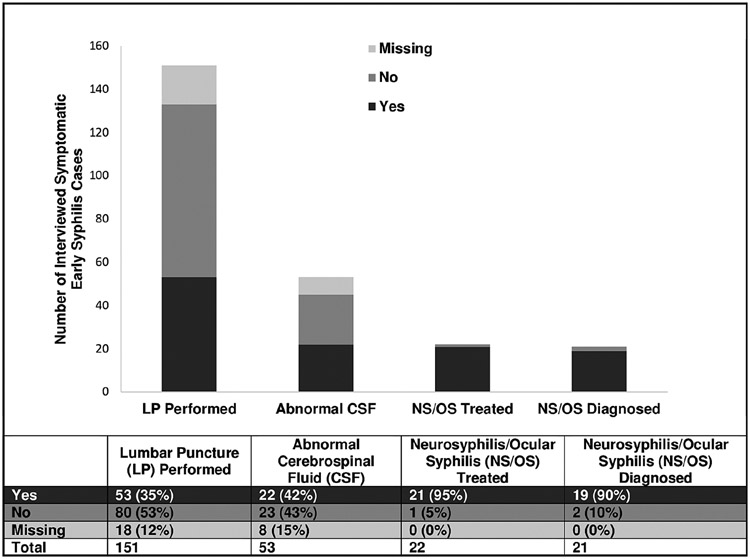
Thirty-five percent of symptomatic ES cases (n = 151) underwent an LP (Figure 1). Among 98 symptomatic ES cases without documentation of LP performance, only 12% (n = 12) reported isolated headache. Among those who underwent an LP (n = 53), 42% had documentation of abnormal CSF results. Among those with abnormal CSF (n = 22), 95% were treated for neurosyphilis or ocular syphilis with a regimen recommended by the CDC. Of the 98 symptomatic patients with no documented LP, 12% (n = 12) were treated for and/or clinically diagnosed with neurosyphilis or ocular syphilis.
Figure 1.
Clinical management of early syphilis cases self-reporting ≥ 1 neurologic or ocular symptom, STD Surveillance Network (SSuN), November 2016–October 2017 (n = 151). The bar graph and corresponding table demonstrate the diagnostic and clinical management outcomes among interviewed symptomatic early syphilis cases within the 5 SSuN jurisdictions participating in the enhanced Neuro/Ocular Syphilis Surveillance Project and include the following: the proportion that had lumbar puncture (LP) performed, the proportion that had documentation of abnormal cerebrospinal fluid (CSF) results (among those who underwent an LP), the proportion that were treated for neurosyphilis (NS) or ocular syphilis (OS) with a regimen recommended by the Centers for Disease Control and Prevention (among those with abnormal CSF), and the proportion that were given a clinical diagnosis of NS and/or OS (among those treated). Abnormal CSF consistent with NS/OS was defined as the presence of 1 of the following criteria: (1) reactive Venereal Disease Research Laboratory test; (2) leukocyte count > 5 cells/μL in human immunodeficiency virus (HIV)–seronegative persons or > 20 cells/μL in HIV-seropositive persons; or (3) protein > 45 mg/dL and reactive CSF fluorescent treponemal antibody absorption test.
Among the 97 ES cases that reported ≥ 1 ocular symptom, 33% (n = 32) had documentation of ophthalmologic examination, of which 44% (n = 14) had abnormal findings. Abnormal ophthalmologic examination findings in patients self-reporting ocular symptom(s) included uveitis (79% [n = 11]), optic neuritis (21% [n = 3]), and retinitis (14% [n = 2]). Of the 51 ES cases that only reported ocular symptoms, 37% (n = 19) had an LP performed, of which 53% (n = 10) had abnormal CSF results. Among the 32 ES cases that reported only ocular symptoms but did not undergo an LP, only 28% (n = 9) had documentation of an ophthalmologic examination performed.
DISCUSSION
Overall, the prevalence of ES cases reporting neurologic and/or ocular symptoms in 5 jurisdictions participating in a sentinel surveillance project was low. However, only one-third of symptomatic ES cases had documentation of an LP, and almost half of those with an LP performed had documentation of abnormal CSF. The majority of symptomatic cases with abnormal CSF were diagnosed and treated for neurosyphilis and/or ocular syphilis. The relatively small proportion of patients reporting neurologic and/or ocular symptoms suggests that incorporation of neurologic and ocular symptom screening into routine STD disease investigations was feasible across the 5 participating jurisdictions.
Our low prevalence estimate (1.7%; 95% CI, 1.4%–1.9%) of self-reported neurologic and/or ocular symptoms is consistent with prior population-based studies in the post-penicillin era, which have reported prevalence of possible or confirmed symptomatic neurosyphilis ranging from 0.5% to 7.9% [8, 14-17]. Prior studies have also reported similar demographics and neurologic and/or ocular symptoms among reported syphilis cases including vision changes/disturbances, headaches, tinnitus, hearing loss, and photophobia [15-18]. While neurologic and/or ocular syphilis are considered rare complications, syphilis rates in the US are increasing. As syphilis becomes more common, we would expect an increased number of persons presenting with complications of syphilis. In our analysis, nearly 20% of those with neurologic and/or ocular symptoms reported serious, debilitating manifestations such as hearing loss, vision loss, or stroke-like symptoms (0.32% of all investigated ES cases). If this proportion were applied to all reported ES cases in the US in 2018 (73 602) [19], 235 individuals could potentially face these devastating sequelae of syphilis.
Notably, the proportion of symptomatic ES cases varied by geographic region. Most symptomatic ES cases were reported by jurisdictions in the West and, specifically, Washington State, which is consistent with prior neurosyphilis and/or ocular syphilis prevalence estimates [16, 17]. Data from 8 US jurisdictions from 2014 to 2015 revealed increases in suspected ocular syphilis cases within 5 jurisdictions, with Washington State reporting the highest prevalence of suspected ocular cases in 2015 (3.9%) [17]. In another study, multiple strains of T. pallidum were identified in patients with ocular syphilis, suggesting that the apparent increases in ocular syphilis were not attributed to a single oculotropic strain [20]. While it is possible that there are currently differences in circulating strains, it is also likely that differential ascertainment of symptoms by jurisdiction could explain the geographic variation. Symptom ascertainment was already part of routine investigations in Seattle, Washington, prior to this enhanced activity and it is likely that investigators were more experienced in obtaining information about neurologic and/or ocular symptoms from patients and providers. Additionally, there was a health advisory around the ocular syphilis cluster in Seattle [21], which may have resulted in community members being more willing to provide symptom information.
Per CDC guidelines, CSF examination should be performed on ES cases if there is clinical evidence of neurologic involvement and in all instances of ocular syphilis [1]; however, only 35% of symptomatic ES cases reporting neurologic and/or ocular symptoms in our study had an LP performed. In an analysis of 49 symptomatic HIV-infected MSM in 4 US cities in 2002–2004, all had LPs performed and most received intravenous penicillin [15], which may reflect adherence to older guidelines that recommended heightened awareness for performing LPs in HIV-infected patients with syphilis [22]. More recent data from 8 jurisdictions revealed that LPs were performed in less than half of 388 suspected ocular syphilis cases; only 60% of patients with suspected ocular syphilis received recommended intravenous penicillin [17]. It is possible that in our study, some symptoms reported by ES cases were attributable to a nonsyphilis morbidity for which an LP was not indicated. However, among the symptomatic ES cases in our study that did not undergo LP, 12% were treated for and/or clinically diagnosed with neurosyphilis or ocular syphilis, suggesting that barriers to LP may exist despite clinicians’ high clinical suspicion for neurosyphilis and/or ocular syphilis.
Barriers to having an LP performed likely exist at multiple levels. On the patient level, a patient with ES may report neurologic and/or ocular symptoms to disease intervention specialists and be referred for follow-up care, but may not discuss symptoms with their provider or may not consent to an LP. On the clinic level, the provider may not be able to perform LPs (based on provider comfort level and feasibility within certain clinical settings) and may rely on referrals to specialists (eg, neurology, infectious diseases) to have an LP performed. However, the referral process can also be limited by geographic distance, availability, and patient barriers to attending follow-up appointments. Challenges with or the absence of specialist referral processes may also impact ability to have ophthalmologic examinations performed on patients with suspected ocular syphilis; in our study, only 33% of ES cases self-reporting ≥ 1 ocular symptom had documentation of an ophthalmologic examination performed. Additional clinical management challenges may include interpretation of CSF results and ensuring appropriate treatment. Reassuringly, 95% of symptomatic ES cases with abnormal CSF in our study were treated for neurosyphilis or ocular syphilis with a CDC-recommended regimen.
The CDC recommends that complex STDs or STD-related conditions, including neurosyphilis and ocular syphilis, should be managed in consultation with or through referral to a specialist [1, 23]; however, our study suggests that there may exist gaps in patients receiving these services. To ensure timely evaluation and treatment of patients with suspected neurosyphilis or ocular syphilis, as indicated, healthcare facilities that provide STD care should proactively establish partnerships and referral processes with local community healthcare providers that have specialized training or experience in diagnosing, treating, and providing follow-up for patients with neurosyphilis or ocular syphilis. Local providers with which to partner may include infectious disease clinicians, ophthalmologists, neurologists, otolaryngologists, and other specialists. Services can be provided in different sites within a multispecialty practice or hospital system [23] and include providers at different facility types, such as local emergency departments where a patient with suspected neurosyphilis or ocular syphilis may be referred for urgent evaluation and treatment.
Our study was subject to several limitations. First, we only collected data on reported ES cases. Although ES case investigations involved actively screening patients for symptoms, it was still inherently passive surveillance as investigations were based on persons already diagnosed with syphilis. Since undiagnosed infections are not investigated, we were unable to estimate the true prevalence of neurologic and/or ocular symptoms among persons with early syphilis. Second, project protocols were designed around existing local health department protocols, and there was variation in project implementation across participating jurisdictions. Existing partner services practices may have varied by mode of interview (telephone vs in person), type of interviewer, and prioritization of ES cases for interview. For example, NYC prioritized ES cases for investigation based on specific risk criteria, such that investigations were targeted to include cases that may have had higher prevalence of neurologic and/or ocular symptoms. However, a sensitivity analysis was performed in which NYC data were removed and all findings were similar. For collection of enhanced data for this project, depending on burden of disease and staffing, some jurisdictions mailed provider questionnaires to clinics for completion vs calling providers and/or performing medical records reviews. Third, we are not able to determine the reasons for geographic differences in prevalence of self-reported neurologic and/or ocular symptoms; future studies with additional data collection on provider and health department practices may shed light on this. Finally, as there were only 5 jurisdictions included, our findings may not be generalizable.
Overall, we found that routine neurosyphilis and ocular syphilis symptom screening for all ES cases as part of STD disease investigations is feasible. Additionally, our findings illustrate the need for interventions, such as provider education, training, and clinic protocols or referral processes to ensure timely patient follow-up, including LPs and ophthalmologic examinations. To address the limitations of current surveillance, in January 2018, the CDC began collecting data on ocular, otic, and late clinical manifestations (in addition to neurologic manifestations) for all reported syphilis cases. Additionally, a new category, “possible” neurologic manifestations, was added to allow reporting of cases that are symptomatic but do not receive an LP. The methodology documented in this enhanced surveillance project could be adopted by other jurisdictions to facilitate collection of these valuable clinical data and to better monitor for adverse outcomes related to syphilitic infections.
Acknowledgments.
This article was written on behalf of the STD Surveillance Network (SSuN) collaborators, the disease intervention specialists, and other public health staff who contributed to the data collection, management, and implementation of this project. The authors thank Jim Braxton, LaZetta Grier, Jonathan Downs, Alyssa Piraino, Cathy Bradley, Ellen Klingler, Brian Toro, Preeti Patel, Lenore Asbel, and James J. Williams, as well as the patients and providers who contributed data to this project.
Financial support.
This work was supported by the CDC (grant number PS13-1306), through which the SSuN was established.
Footnotes
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1.Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015; 64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 2.Lukehart SA, Hook EW 3rd, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med 1988; 109:855–62. [DOI] [PubMed] [Google Scholar]
- 3.Rolfs RT, Joesoef MR, Hendershot EF, et al. A randomized trial of enhanced therapy for early syphilis in patients with and without human immunodeficiency virus infection. The Syphilis and HIV Study Group. N Engl J Med 1997; 337:307–14. [DOI] [PubMed] [Google Scholar]
- 4.Merritt HH, Adams AR, Solomon HC. Neurosyphilis. New York: Oxford, 1946. [Google Scholar]
- 5.Woolston S, Cohen SE, Fanfair RN, Lewis SC, Marra CM, Golden MR. A cluster of ocular syphilis cases—Seattle, Washington, and San Francisco, California, 2014–2015. MMWR Morb Mortal Wkly Rep 2015; 64:1150–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Clinical advisory: ocular syphilis in the United States. Available at: http://www.cdc.gov/std/syphilis/clinicaladvisoryos2015.htm. Accessed 4 February 2020.
- 7.Centers for Disease Control and Prevention. National Notifiable Diseases Surveillance System: case definitions. Available at: http://wwwn.cdc.gov/nndss/script/casedefDefault.aspx. Accessed 31 May 2019.
- 8.de Voux A, Kidd S, Torrone EA. Reported cases of neurosyphilis among early syphilis cases—United States, 2009 to 2015. Sex Transm Dis 2018; 45:39–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. STD surveillance case definitions. Available at: http://www.cdc.gov/std/stats10/app-casedef.htm. Accessed 4 February 2020.
- 10.Marra CM, Maxwell CL, Smith SL, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis 2004; 189:369–76. [DOI] [PubMed] [Google Scholar]
- 11.Libois A, De Wit S, Poll B, et al. HIV and syphilis: when to perform a lumbar puncture. Sex Transm Dis 2007; 34:141–4. [DOI] [PubMed] [Google Scholar]
- 12.Marra CM, Maxwell CL, Tantalo L, et al. Normalization of cerebrospinal fluid abnormalities after neurosyphilis therapy: does HIV status matter? Clin Infect Dis 2004; 38:1001–6. [DOI] [PubMed] [Google Scholar]
- 13.Marra CM, Maxwell CL, Tantalo LC, Sahi SK, Lukehart SA. Normalization of serum rapid plasma reagin titer predicts normalization of cerebrospinal fluid and clinical abnormalities after treatment of neurosyphilis. Clin Infect Dis 2008; 47:893–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taylor MM, Aynalem G, Olea LM, He P, Smith LV, Kerndt PR. A consequence of the syphilis epidemic among men who have sex with men (MSM): neurosyphilis in Los Angeles, 2001–2004. Sex Transm Dis 2008; 35:430–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Symptomatic early neurosyphilis among HIV-positive men who have sex with men—four cities, United States, January 2002–June 2004. MMWR Morb Mortal Wkly Rep 2007; 56:625–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Dombrowski JC, Pedersen R, Marra CM, Kerani RP, Golden MR. Prevalence estimates of complicated syphilis. Sex Transm Dis 2015; 42:702–4. [DOI] [PubMed] [Google Scholar]
- 17.Oliver SE, Aubin M, Atwell L, et al. Ocular syphilis—eight jurisdictions, United States, 2014–2015. MMWR Morb Mortal Wkly Rep 2016; 65:1185–8. [DOI] [PubMed] [Google Scholar]
- 18.Davis AP, Stern J, Tantalo L, et al. How well do neurologic symptoms identify individuals with neurosyphilis? Clin Infect Dis 2018; 66:363–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2018. Available at: https://www.cdc.gov/std/stats. Accessed 4 February 2020.
- 20.Oliver S, Sahi SK, Tantalo LC, et al. Molecular typing of Treponema pallidum in ocular syphilis. Sex Transm Dis 2016; 43:524–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Public Health–Seattle & King County. 2015 ocular syphilis advisory: ocular syphilis in King County. Available at: https://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/~/media/depts/health/communicable-diseases/documents/hivstd/ocular-syphilis-advisory.ashx. Accessed 4 February 2020.
- 22.Workowski KA, Levine WC. Selected topics from the Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines 2002. HIV Clin Trials 2002; 3:421–33. [DOI] [PubMed] [Google Scholar]
- 23.Barrow RY, Ahmed F, Bolan GA, Workowski KA. Recommendations for providing quality sexually transmitted diseases clinical services, 2020. MMWR Recomm Rep 2020; 68:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]