Inequalities in optimal blood pressure (BP) control and air pollution exposure are 2 interconnected public health challenges that disproportionately affect racial and ethnic minority groups across the United States. Black and Hispanic individuals are also more likely to have higher BP than their white counterparts,1 which may promote significant disparities in cardiovascular diseases. Racial and ethnic minority groups are more likely to be exposed to higher levels of particulate matter air pollution (including particles ≤2.5 μm, PM2.5), which has been directly linked to BP elevation.2,3 We have recently shown that excess BP associated with PM2.5 levels (“excess BP”) exceeding World Health Organization (WHO) Air Quality Guidelines (AQG) of 5 μg/m3 (annual exposure) varies significantly throughout the world.4 Here, we sought to investigate the racial differences in excess BP across the United States.
We calculated PM2.5 exceeding the WHO AQG by setting guideline annual PM2.5 threshold for all census block groups at the WHO AQG of 5 μg/m3. We derived the annual average PM2.5 from validated integrated model combining satellite, chemical transport models, and ground monitor data using the most recent data from 2018 (available at 1 × 1 km resolution). The results from 2 published meta-analyses were used to calculate an estimated range of excess systolic BP based on known relationships between observational studies of PM2.5 exposure and BP elevations (0.06 mm Hg per 1 μg/m3 increase in PM2.5)2 and randomized trials of air filtration reduction of PM2.5 (3.9 mm Hg reduction per 20.9 μg/m3 reduction in PM2.5 with an imputed 0.19 mm Hg per 1 μg/m3 reduction in PM2.5).3 We used the census data to identify the population composition and the proportion of self-identified non-Hispanic White (NHW), non-Hispanic Black (NHB), Asian, and Hispanic individuals. The Social Vulnerability Index (SVI), a composite measure with higher scores indicating lower socioeconomic position, was assigned at the census tract level for the year 2018. We then calculated the weighted systolic BP by SVI, race, and ethnicity for the entire United States. Institutional review board approval was not required due to the nature of datasets, which are publicly available.
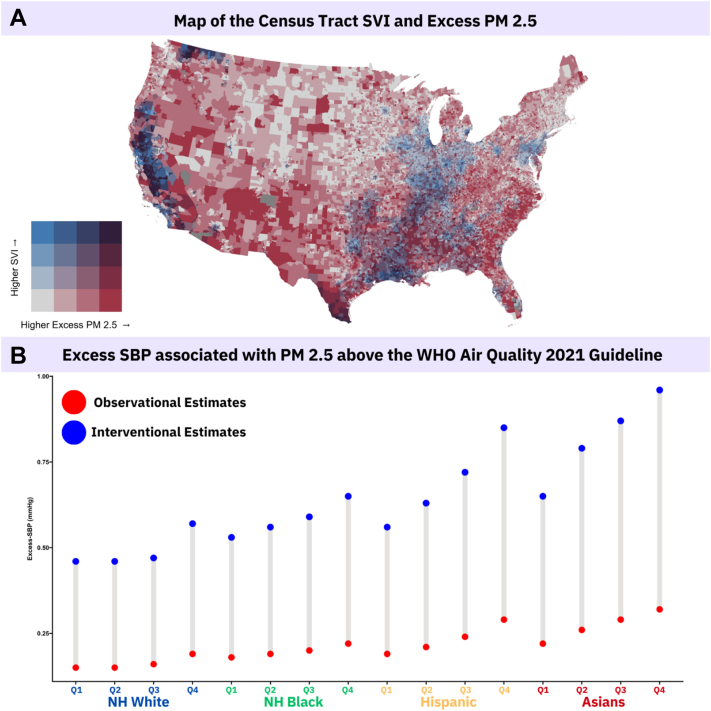
A total of 322,424,487 individuals were included with a mean PM2.5 of 7.94 μg/m3. Most individuals (95.5%) had PM2.5 exposure equal to or higher than 5 μg/m3 (97.1% of Hispanics, 94.2% of NHW, and 99.5% of NHB individuals). The weighted average of excess systolic BP (observational [lowest] to interventional [highest] estimates) was 0.19 to 0.56 mm Hg overall, 0.16 to 0.47 mm Hg for NHW, 0.20 to 0.61 mm Hg for NHB, 0.27 to 0.80 mm Hg for Asians, and 0.25 to 0.75 mm Hg for Hispanic individuals. People with higher SVI had higher excess systolic BP (Figure 1) across all racial and ethnic minority groups. The group with the highest excess BP were Asian individuals in the 4th quartile of SVI (0.32-0.96 mm Hg), while the lowest group was NHW living in the lowest quartile of SVI (0.15-0.46 mm Hg).
Figure 1.
Social Vulnerability Index and Excess Blood Pressure Associated With PM2.5 Exceeding WHO Annual Standards
(A) Map of the census tract-level SVI and excess PM2.5. (B) Estimated excess systolic blood pressure (mm Hg) associated with annual PM2.5 exposures exceeding the revised 2021 World Health Organization air quality guidelines (PM2.5 ≥5 μg/m3) using estimates from interventional studies (top) and observational studies (bottom), by race and ethnicity and social vulnerability. NH = non-Hispanic; SVI = social vulnerability index.
We demonstrate significant differences in excess BP associated with PM2.5 throughout the United States, varying with race, ethnicity, and socioeconomic position. There was a 2-fold increase in excess BP from the lowest group to the highest group. While the absolute excess in systolic BP is small, even small increases in systolic BP and its pervasive impact translate into a substantial cardiovascular impact, especially in racial and ethnic minority groups. Although race and ethnicity have little biological substrate, these disparities in excess BP likely stem from complex social determinants of health and built-environment interactions, which may ultimately increase vulnerability to negative health outcomes. Our findings further highlight the importance of accelerating the clean energy transition, which may help reduce air pollution levels from a BP control perspective and therefore impact atherosclerotic cardiovascular disease events. The benefits of targeted personal-level interventions (eg, portable air cleaners) for high-risk patients, especially those at the intersection of social vulnerability and high air pollution merits further study.5 Addressing air pollution exposure may be a critical step in reducing health disparities and improving health outcomes among racial and ethnic minority groups in the United States.
Footnotes
This work was supported by the National Institutes of Health grants P50 MD017351-01 and 1R35ES031702-01A1. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Aggarwal R., Chiu N., Wadhera R.K., et al. Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the United States, 2013 to 2018. Hypertension. 2021;78:1719–1726. doi: 10.1161/HYPERTENSIONAHA.121.17570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Niu Z., Duan Z., Yu H., et al. Association between long-term exposure to ambient particulate matter and blood pressure, hypertension: an updated systematic review and meta-analysis. Int J Environ Health Res. 2023;33:268–283. doi: 10.1080/09603123.2021.2022106. [DOI] [PubMed] [Google Scholar]
- 3.Walzer D., Gordon T., Thorpe L., et al. Effects of home particulate air filtration on blood pressure: a systematic review. Hypertension. 2020;76:44–50. doi: 10.1161/HYPERTENSIONAHA.119.14456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brook R.D., Motairek I., Rajagopalan S., Al-Kindi S. Excess global blood pressure associated with fine particulate matter air pollution levels exceeding World Health Organization guidelines. J Am Heart Assoc. 2023;12 doi: 10.1161/JAHA.122.029206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rajagopalan S., Brauer M., Bhatnagar A., et al. American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Stroke Council. Personal-Level Protective Actions against particulate matter air pollution exposure: a Scientific Statement from the American Heart Association. Circulation. 2020;142:e411–e431. doi: 10.1161/CIR.0000000000000931. [DOI] [PubMed] [Google Scholar]